Oslo’s child health service during the COVID-19 pandemic – the experiences of first-time mothers
Mothers who engaged with the ‘New families’ home visit programme, had more frequent contact with child health centres. But more than a third of all the mothers reported that they had received inadequate information from public authorities about the child health centre’s services.
Background: The child health service comes into contact with virtually all parents and children in their first year of life and until they start school. The service plays a key role in providing parents with guidance, support and reassurance. In addition to the standard child health service programme, Oslo local authority has introduced a home visit programme, ‘New families’, to provide extra support for first-time parents. In spring 2020, the Norwegian Directorate of Health introduced temporary national guidelines for child health centres, as a consequence of COVID-19. This entailed a severe cut-back to the programme of child health services.
Objective: The study’s objective was to survey the experience of first-time mothers with child health centre service provision during the COVID-19 pandemic. We also wanted to investigate whether the experiences of first-time mothers who engaged with the ‘New families’ home visit programme, differed from those who did not.
Method: This was a cross-sectional study and data were collected through the Nettskjema online survey platform. Descriptive analyses were conducted in SPSS. The study recruited mothers who participate in the ‘New families’ research project.
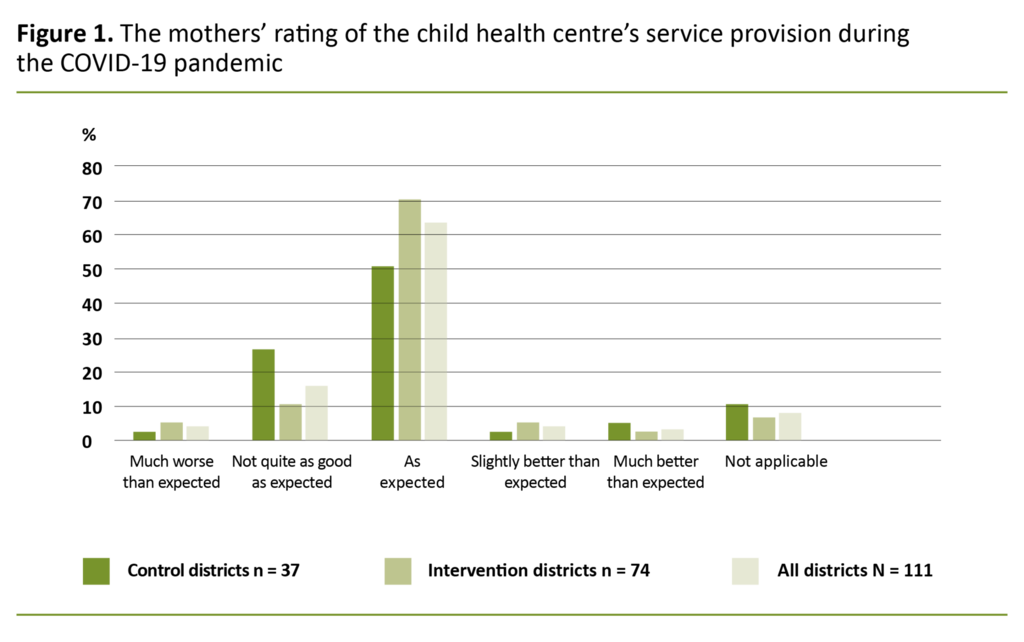
Results: The response rate was 62 per cent (111 mothers). Seventy-eight mothers (70 per cent) had been in touch with a child health centre in one or more ways, and four (4 per cent) had been unable to get in touch with a public health nurse when the need arose. In areas where the home visit programme had been introduced (the intervention districts), a larger proportion of mothers had been in touch with a child health centre (p = 0.028). The mothers who had been in telephone contact, reported that this did not work as well as earlier in-person consultations at a child health centre (n = 17 / 63 per cent) or that it worked equally well (n = 5 / 19 per cent). The majority of the mothers (n = 71 / 64 per cent) had found that services provided by the child health centre met their expectations.
Conclusion: A large proportion of the mothers had been in touch with a child health centre during the period. Out of these, a significantly greater number lived in the intervention districts than in the control districts. More than a third of the mothers reported that they had received inadequate information about changes to services in the period. While the mothers preferred the standard service provision, they appeared to adjust to the changes and the services provided.
Virtually all children (98.8 per cent) and their parents are seen by the child health service in their first year of life and until they start school (1). This public health service, provided by local authorities, plays a key role in providing parents with guidance, support and reassurance through home visits, in-person consultations at child health centres, telephone consultations, group sessions and drop-in services (2).
Due to COVID-19, the Norwegian Directorate of Health introduced temporary national guidelines for the provision of child health services on 13 March 2020. These guidelines entailed severe cut-backs to the services provided by child health centres (3).
Child health centres were instructed to prioritise neonates, the child vaccination programme and six-week medical check-ups with a doctor in attendance, but were asked to reduce their other activities and avoid making home visits so far as possible. As from mid-April, the Directorate of Health recommended that the services be reinstated, but home visits and group sessions should be replaced by individual consultations at the child health centres (4).
In the middle of May, the Directorate of Health further recommended that normal activities should be maintained or reinstated (5). Oslo’s district councils were recommended to follow the guidelines issued by the Directorate of Health.
Programme developed for first-time mothers
Oslo local authority has developed (6) a programme designed to provide support for new parents, boost their coping skills and reassure them in their parenting role while also promoting a healthy family lifestyle (7). The programme is called ‘New families’ (NF) and relies on repeat home visits.
NF is additional to the statutory services made available by child health centres (2) and the programme is offered universally to all first-time parents. The first home visit is offered during pregnancy, around week 28, and is intended to build a relationship between the family and the public health nurse prior to delivery. NF then offers home visits according to the family’s needs until the child has reached two years of age.
The aim is for families to be seen by the same public health nurse who visits their home whenever they attend consultations at the child health centre. An ongoing research project is studying the effectiveness of and experience with the NF home visit programme (8). Due to COVID-19, the frequency of home visits under the NF programme was reduced.
COVID-19 brought changes to child health centre service provisions
Becoming a parent for the first time is considered to be one of the greatest upheavals in a person’s life. Access to knowledge and support is highlighted as key to coping with the new parent role (9, 10). The COVID-19 infection control measures changed not only the services offered by child health centres, but also the everyday lives of many.
International studies show that the uncertainty caused by COVID-19 has been a heavy burden for many (11), and there has been a rise in the number of mothers with symptoms of depression and anxiety during the pandemic (12, 13).
Pre-pandemic studies also show that quarantining can have a psychological impact, such as stress, depression, insomnia and irritability, and that inadequate public information about control measures and the purpose of quarantining can be seen as stress factors (14).
Nationally, there was a considerable drop in in-person consultations at child health centres in March and April 2020. In-person consultations were generally replaced by telephone and video consultations, and parents of young children increasingly made contact with voluntary organisations, telephone help lines and live chat services during the coronavirus period. The child health centres’ reduced capacity was caused by infection control measures, reassignment of municipal staff to other tasks, quarantining and illness (15).
The study’s objective
This study surveyed the experience of first-time mothers with child health service provision during the COVID-19 pandemic. We also wanted to investigate whether the experiences of first-time mothers who engaged with the NF home visit programme differed from those who did not.
Method
We conducted a cross-sectional study in the period 18 May 2020 to 7 June 2020 in order to survey the experiences of first-time mothers with Oslo’s child health centres during the coronavirus pandemic. Invitations to take part were sent by text message to mothers who participate in the ongoing research project ‘New families’ (8), a prospective non-randomised controlled study that is examining the effectiveness of the NF home visit programme. In total, 111 of 178 mothers responded (62 per cent) to the invitation. We issued two reminders, which increased the response rate.
The mothers were residents of five different parts of Oslo, three areas where the NF home visit programme had been introduced by the child health service (intervention districts), and two areas where NF had yet to be introduced (control districts).
The project group developed a digital questionnaire for the collection of quantitative data. Completing the questionnaire took approximately 15 minutes. It consisted of 31 questions about the child’s age, the family’s infection status and inclusion in any COVID-19 risk group, home visits/telephone consultations/child health centre consultations, number of consultations, reason for consultations, quality of consultations, contact with the regular public health nurse, expectations of the child health centre’s services, use of other support services, concerns regarding the pandemic, general information about COVID-19 and information about the child health centre’s services.
We used categorical and numeric values and a Likert scale with three or five alternatives. One question invited a free-text response if the mothers wanted to add anything that had affected their situation during the pandemic. Some questions were conditional, so that the respondent would not have to answer further questions if the topic was not relevant to them.
The questionnaire was posted on the University of Oslo’s online Nettskjema platform and is available here. The questions referred to the period from the introduction of COVID-19 restrictions on 13 March 2020 until the day of completing the questionnaire.
Analyses
We analysed the data material using SPSS (16). We undertook frequency analyses for the entire sample of mothers and analysed the sample’s distribution between intervention and control districts. We conducted a chi square test to find the relationship between categorical variables.
Free-text responses from thirteen mothers did not provide a basis for qualitative analysis. We will highlight the free-text responses where we consider this to aid the overall interpretation of the results.
Ethics
The mothers received a link to an electronic information letter by text message. The letter provided information about data anonymisation, the opportunity to withdraw from the study and to have all collected information deleted. The participants gave their consent to taking part by completing the questionnaire. Response data from the Nettskjema survey were linked to the mother’s ID code in the ‘New families’ research project and stored directly in Services for Sensitive Data (17).
The NF research project has received advance approval by the Regional Committees for Medical and Health Research Ethics (REK) (reference number 2018/1378 REK south-east D), and was reported to the Norwegian Centre for Research Data (NSD) (project number 735207). The project is being conducted in compliance with research ethical guidelines (18). We submitted alteration notifications for the COVID-19 survey to REK and NSD.
Results
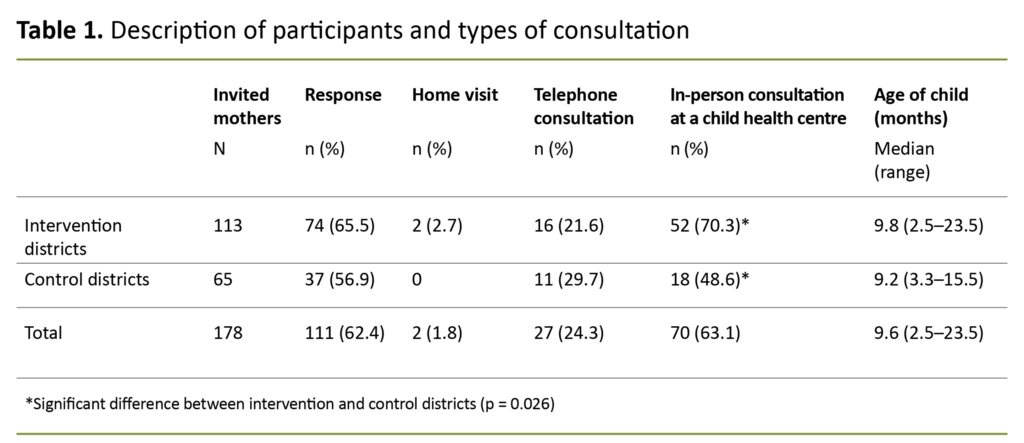
The survey had a response rate of 62 per cent – 111 mothers – unevenly distributed between intervention and control districts. The age of the children ranged from 2.5 to 23.5 months (table 1).
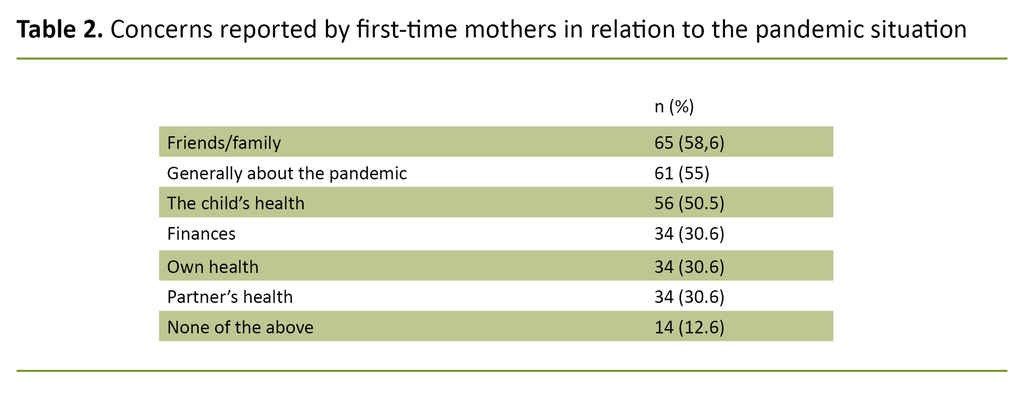
None of the mothers or anyone in their households had been diagnosed with COVID-19 or hospitalised with COVID-19. Twenty-three mothers (21 per cent) or people in their households had quarantined, of whom 11 (15 per cent) were from the intervention districts and 12 (32 per cent) from the control districts. Eight mothers (7 per cent) or people in their households were in a COVID-19 risk group. No mothers gave an affirmative answer to both questions. The mothers reported several concerns in relation to the pandemic situation (table 2).
The majority of the mothers reported that they had received general information about COVID-19 that made them feel that they and their family were safe.
The majority of the mothers (n = 102 / 92 per cent) reported that they had received general information about COVID-19 that made them feel that they and their family were safe.
Contact with child health centres during the COVID-19 pandemic
Seventy-eight mothers (70 per cent) had been in touch with a child health centre on one or more occasions. In the intervention districts, 57 mothers (77 per cent) had been in touch with a child health centre, compared to 21 (57 per cent) in the control districts (p = 0.028). Table 1 shows how many times each of the three different forms of contact with the child health service had been used by the mothers: home visit, telephone contact and in-person child health centre consultations.
Telephone consultations
Twenty-seven mothers had experience of a telephone consultation (table 1). The most frequent reason for a telephone consultation was that the mother had requested an appointment (n = 15 / 56 per cent). Other reasons included replacement appointments for an in-person child health centre consultation (n = 6 / 22 per cent), the public health nurse got in touch to ask how the family was doing (n = 5 / 19 per cent), and cancellation of appointments (n = 4 / 15 per cent).
The majority of the mothers who had been in telephone contact reported that to a great or very great extent they had been addressed in a polite and respectful manner (n = 26 / 96 per cent), that the public health nurse welcomed their questions (n = 24 / 89 per cent) and that the public health nurse cared for them and their child (n = 23 / 85 per cent).
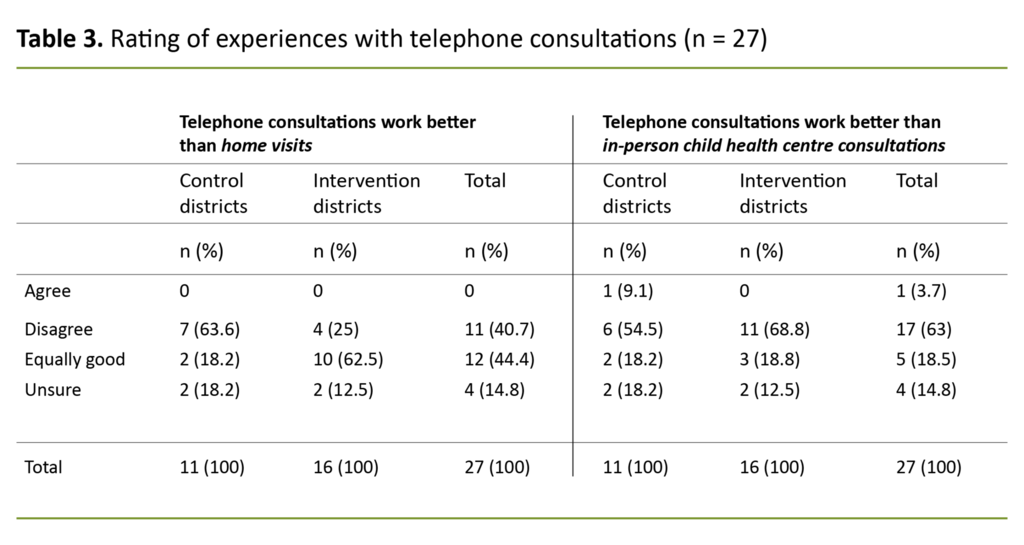
The mothers came to trust the public health nurse’s professional expertise (n = 23 / 85 per cent), and felt that they had benefited from the telephone consultation (n = 21 / 78 per cent). There were no major differences between the districts. Table 3 shows how the mothers rated telephone consultations compared to earlier home visits and in-person child health centre consultations.
In-person consultation at a child health centre
There was a significant difference between the intervention districts and the control districts with respect to the number of in-person consultations at child health centres (table 1). The reason for these consultations included ordinary vaccination appointments with a doctor and a public health nurse. Seven mothers had attended additional consultations. Of the mothers who had attended a consultation in person at a child health centre, 65 (93 per cent) reported that they felt the consultation was safe in terms of infection control, four (6 per cent) reported that they had not felt safe, and one (1.4 per cent) reported that the question was not applicable.
Contact with a public health nurse
A total of 44 (40 per cent) of the mothers reported that they had been able to get in touch with a public health nurse when the need arose. Four (4 per cent) had been unable to get in touch, and 63 (57 per cent) reported that the question was not applicable. Out of the mothers who had been able to get in touch with a public health nurse (n = 44), 29 (66 per cent) responded that they had talked to their regular public health nurse.
A total of 44 of the mothers reported that they had been able to get in touch with a public health nurse when the need arose.
A small proportion of the mothers (n = 14 / 13 per cent) had avoided contacting the public health nurse with questions or challenges. The reasons they gave were that their questions were not sufficiently important, they worried about the infection situation, and they did not want to burden the public health nurse.
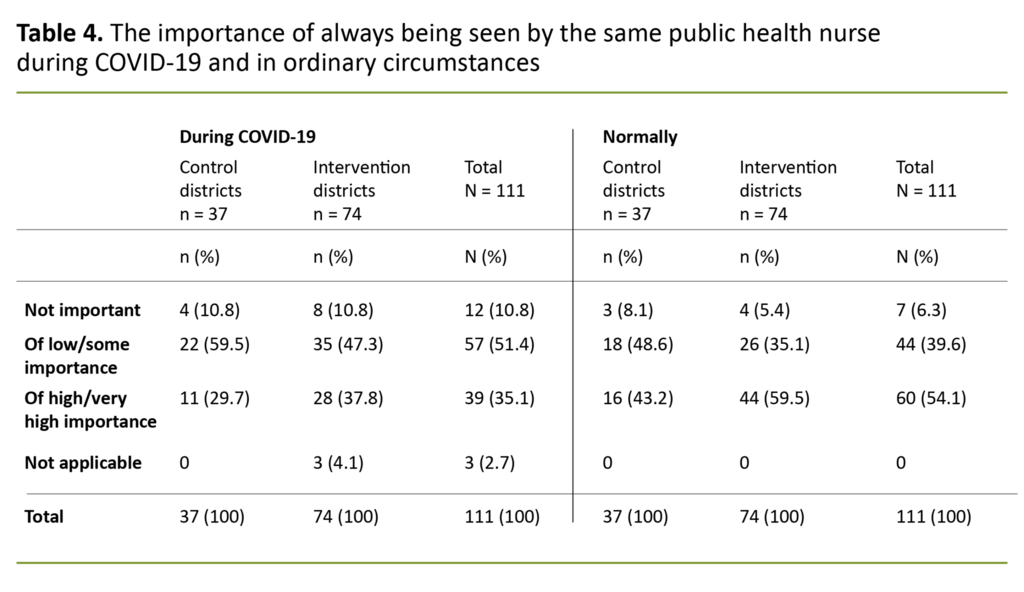
The mothers’ rated their need to see their regular public health nurse differently during COVID-19 compared to during ordinary circumstances (table 4).
Rating the child health centre’s services
A total of 69 (62 per cent) of the mothers reported that they had received adequate information about the child health centre’s services during the pandemic. Of these, 20 (54 per cent) lived in the control districts while 49 (66 per cent) lived in the intervention districts.
The majority of the mothers reported that the child health centre’s services had met their expectations during the pandemic (figure 1). Five mothers reported that they had made use of other support services in the period in question, like live chat services, telephone help lines, online forums and family guidance centres.
Free text
Thirteen mothers submitted free-text responses. These answers concerned their home situation and the child health centre’s service provision. Comments related to changes at work or in their social life, as well as job-related challenges and a strain on relationships when faced with having to balance working from home with looking after children at home. They missed social settings like postnatal groups, open days at the child health centre and access to important information.
Discussion
More than a quarter of the families had been directly affected by COVID-19 in that they had quarantined or found themselves in a high-risk group. Earlier studies have shown that quarantining can have a mental health impact in the form of stress, symptoms of depression, insomnia and irritability (14).
Most of the mothers in this study had one or more concerns in relation to friends, family, the child’s health or a general worry related to the pandemic. The uncertainty surrounding COVID-19 has been a burden to many (11), and symptoms of anxiety and depression have increased among mothers in this period (12, 13).
Virtually all mothers in our study reported that they had received adequate information about COVID-19 to feel that they and their families were safe. Earlier research has shown that inadequate public information about measures imposed and the purpose of quarantining may be felt as stressors (14).
A survey undertaken by the Research Council of Norway in April 2020 (19), shows that 77 per cent of the population understood the information provided about coronavirus infection. This figure may indicate that Norwegian health authorities have helped to reduce potential stressors for the mothers in the study by issuing comprehensible and adequate information.
Fewer child health centre consultations during the pandemic
Many of the mothers had had some form of contact with a child health centre in the relevant period. A few reported that they had been unable to get in touch with a public health nurse when the need arose. The proportion of contacts is similar to that found in national statistics, which show a decline in the number of child health centre consultations in the period March to April 2020.
The decline was greatest for children over 18 months of age, amounting to more than 90 per cent. Consultations for children under 18 months also fell, except for the check-ups at six weeks, three and ten months, all of which were at normal levels (15). Voluntary organisations, telephone help lines and live chat services have reported a greater number of calls during the coronavirus period, including from the parents of young children (15). In our study, a very small proportion reported that they had made use of other support services. Based on this result, and despite the service cut-backs (3) and potential re-assignment of public health nurses to infection control work, it may appear that Oslo’s standard child health centre programme remained available to service users.
Compared to respondents in the control districts, respondents in the intervention districts reported having had significantly more contact with child health centres and having attended more ordinary consultations there.
Compared to respondents in the control districts, respondents in the intervention districts reported having had significantly more contact with child health centres and having attended more ordinary consultations there. The study does not reveal the reason why, but it is possible that random factors may have contributed to this difference, like the age range of children in each district compared to the recommended age at check-up consultations, or the district councils’ respective use of resources, for instance by reassigning child health centre staff to infection control initiatives.
In-person child health centre consultations were better than telephone consultations
The majority of mothers who had been in telephone contact with a child health centre had found that in-person consultations are a better form of contact than telephone consultations. The mothers nevertheless rated the telephone consultation as a positive experience. International studies confirm that parents prefer physical consultations to digital alternatives or telephone contact (12).
When it comes to home visits, however, a large proportion of the mothers in the intervention districts reported that telephone consultations worked just as well as the earlier home visits, as opposed to the mothers in the control districts who reported that home visits were a better alternative. Universal intervention programmes involving home visits help to develop a stronger relationship of trust between mothers and public health nurses (20). Everyone who took part in the study had previously received a home visit by a public health nurse from the local child health centre. The home visit programme introduced in the intervention districts may have boosted the mothers’ trust in the public health nurse, and may have made them more at ease with using the telephone for consultations.
The mothers in the intervention districts reported a greater need always to see the same public health nurse than the mothers in the control districts, which may suggest a strengthened relationship of trust between the mothers in the intervention districts and the public health nurses.
Inadequate information about services
More than a third of the mothers reported that they had received inadequate information about the child health centre’s services during the COVID-19 pandemic. This applied to a slightly larger proportion of the mothers in the control districts. The child health centres had been advised to provide information about services and restrictions that would apply in this period and to convey this information via a variety of channels (4).
Some mothers in the study had been looking for more information about services offered by child health centres, and about the changes to the way they operated. A national report on child health centres (15) refers to fewer questions than usual from service users during the coronavirus pandemic, although the opening hours for telephone enquiries and consultations were generally affected only to a minor degree. This report suggests that the fall in the number of enquiries may be because service users wished not to or dared not attend appointments, and that they may have assumed the service to be closed.
A small proportion of the mothers in our study reported that they for different reasons had avoided contacting a public health nurse with questions and challenges. This may mean that the mothers had not received adequate information from the child health centre to enable them to make use of the services available, but there may also be other reasons which we have been unable to identify through this survey.
Most had found the service provision to meet their expectations
Nevertheless, the majority of the mothers reported that the child health centre’s services in the relevant period had met their expectations, with a greater proportion of mothers in the intervention districts rating the services as in accordance with their expectations compared to the mothers in the control districts.
The mothers’ expectations of the child health centre’s services can be linked to the centres’ dissemination of information during the relevant period as well as national infection control restrictions imposed on the service (4). The mothers reported that they ordinarily would have a greater need always to see the same public health nurse than during the pandemic, which may suggest that a large proportion of the mothers adjusted to the child health centres’ service alterations.
Nearly all of the mothers felt safe thanks to the infection control measures.
The free-text responses revealed that those who found the services to be somewhat or much poorer than expected, put this down to poor organisation, short consultations that provided little scope for conversation, a sense of poor follow-up and an unfamiliar public health nurse.
Nearly all of the mothers felt safe thanks to the infection control measures. This suggests that child health centres have succeeded in organising and adapting their operations to provide reassuring levels of infection control (4, 5, 21). Nevertheless, a small proportion reported that they felt unsafe, and the free-text responses revealed the reasons as being a sense that there were too many people in the waiting room at the same time, and different days for consultations with doctors and public health nurses.
Differences between intervention districts and control districts
The results show differences between the intervention districts and the control districts, but the sample would have had to be larger to allow us to investigate further differences. The control group consisted of 37 mothers while the intervention group consisted of 74 mothers. This amounts to a relatively large difference in group size, which would produce low statistical strength and make it difficult to use univariate statistical methods.
This weakness is particularly relevant for analyses of sample subgroups, like mothers who had been in touch with a child health centre by telephone (n = 27) and analyses with variables with multiple response categories, such as the need always to see the same public health nurse during the pandemic.
Results with no statistically significant differences between intervention districts and control districts have nevertheless been presented in the article because they represent a trend among respondents and may be of use to later research.
The cross-sectional survey was available for three weeks. Responses could be provided from a time perspective of up to 2.5 months, from the introduction of coronavirus measures in March until the mothers completed the questionnaire, a period during which a number of temporary national guidelines (3–5) were in place.
The study design does not permit a comparison of the services that families received from child health centres in the relevant period with the services that families should have received from child health centres under the temporary guidelines.
The study results are descriptive and are valid for first-time mothers in the selected districts during the period in question. The results cannot be generalised but may provide an impression of mothers’ contact with and experience of child health centres during a period of major service upheaval, and this may be transferrable to similar situations.
Conclusion
Despite changes to service provisions during the COVID-19 pandemic, a large proportion of the mothers had been in touch with a child health centre. The service users appear to have adapted to the changes, both in terms of the type of consultations they were offered and which public health nurse they engaged with. However, their preference was for the child health centre’s standard service provision.
Many mothers are of the opinion that they received inadequate information about the changes to services offered by child health centres. According to the results, there tended to be differences between the intervention districts and the control districts. The mothers in the intervention districts had more contact with child health centres during the COVID-19 period.
References
1. Statistisk sentralbyrå. Kommunehelsetenesta [Internet]. Oslo: Statistisk sentralbyrå [updated 16. June 2020, cited 7. September 2020]. Available at: https://www.ssb.no/helse/statistikker/helsetjko/aar
2. Helsedirektoratet. Nasjonal faglig retningslinje for det helsefremmende og forebyggende arbeidet i helsestasjon, skolehelsetjeneste og helsestasjon for ungdom. Oslo: Helsedirektoratet; 2017. Available at: https://www.helsedirektoratet.no/retningslinjer/helsestasjons-og-skolehelsetjenesten (downloaded 07.09.2020).
3. Helsedirektoratet. Helsestasjon, svangerskapsomsorg og skolehelsetjeneste. I: Koronavirus – beslutninger og anbefalinger. Oslo: Helsedirektoratet; 2020 (downloaded 19.03.2020).
4. Helsedirektoratet. Helsestasjon, svangerskapsomsorg og skolehelsetjeneste. I: Koronavirus – beslutninger og anbefalinger. Oslo: Helsedirektoratet; 2020 (downloaded 17.04.2020).
5. Helsedirektoratet. Helsestasjon, svangerskapsomsorg og skolehelsetjeneste. I: Koronavirus – beslutninger og anbefalinger. Oslo: Helsedirektoratet; 2020 (downloaded 15.05.2020).
6. Leirbakk MJ, Torper J, Engebretsen E, Opsahl JN, Zeanah P, Magnus JH. Formative research in the development of a salutogenic early intervention home visiting program integrated in public child health service in a multiethnic population in Norway. BMC Health Services Research 2018;18:741.
7. Oslo kommune. Nye familier – en god start varer livet ut. Opplæringsmanual. Oslo: Oslo kommune; 2018.
8. ClinicalTrials.gov [internett]. NCT04162626. New Families – Innovation and development of the child health services in Oslo 14.11.2019 [updated 27. May 2020, cited 17. December 2020]. Bethesda, Maryland: U.S. National Library of Medicine. Available at: https://clinicaltrials.gov/ct2/results?cond=New+Families&term=&cntry=NO&state=&city=&dist
9. Entsieh AA, Hallström IK. First-time parents’ prenatal needs for early parenthood preparation – A systematic review and meta-synthesis of qualitative literature. Midwifery. 2016;39:1–11.
10. Ahlborg T, Berg S, Lindvig J. Sense of coherence in first-time parents: a longitudinal study. Scandinavian Journal of Public Health. 2013;41:623–9.
11. Brown SM, Doom JR, Lechuga-Pena S, Watamura SE, Koppels T. Stress and parenting during the global COVID-19 pandemic. Child Abuse & Neglect. 2020;110(pt 2):104699.
12. Best Beginnings, Home-Start UK, The Parent-Infant Foundation. Babies in lockdown: listening to parents to build back better. Storbritannia: Best Beginnings, Home-Start UK, The Parent-Infant Foundation; 2020. Available at: https://parentinfantfoundation.org.uk/our-work/campaigning/babies-in-lockdown/#fullreport (downloaded 07.09.2020).
13. Davenport MH, Meyer S, Meah VL, Strynadka MC, Khurana R. Moms are not OK: COVID-19 and maternal mental health. Front. Glob. Women’s Health. 19.06.2020.
14. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet. 2020;395(10227):912–20.
15. Barne-, ungdoms- og familiedirektoratet. Utsatte barn og unges tjenestetilbud under covid-19-pandemien. Oslo: Barne-, ungdoms- og familiedirektoratet; 2020. Statusrapport 1. Available at: https://bufdir.no/globalassets/global/nbbf/bufdir/utsatte_barn_og_unges_tjenestetilbud_under_covid19_pandemien_statusrapport_1-konvertert.pdf (downloaded 01.09.2020).
16. IBM Corporation. IBM SPSS Statistics for Windows, versjon 26.0. Armonk, New York: IBM Corporation; 2019.
17. Universitetet i Oslo. Tjeneste for sensitive data (TSD) [Internet]. Oslo: Universitetet i Oslo [cited 20.03.2021]. Available at: https://www.uio.no/tjenester/it/forskning/sensitiv/
18. Lov 20. juni 2008 nr. 44 om medisinsk og helsefaglig forskning (helseforskningsloven). Available at: https://lovdata.no/dokument/NL/lov/2008-06-20-44 (downloaded 01.09.2020).
19. Forskningsrådet. Befolkningens tillit til og syn på forskning. Rapportnr. 20100423. Oslo: Forskningsrådet; 2020. Available at: https://www.forskningsradet.no/contentassets/96ad9ee96f7a460cada4501ad0b3502d/pm-rapport-befolkningens-tillit-til-forskning---april-2020.pdf (downloaded 07.09.2020).
20. Aston M, Price S, Etowa J, Vukic A, Young L, Hart C, et al. The power of relationships: exploring how public health nurses support mothers and families during postpartum home visits. Journal of Family Nursing. 2015;21(1):11–34.
21. Folkehelseinstituttet. Råd til helsestasjons- og skolehelsetjenesten ved covid-19 (koronasykdom). Veiledning for smittevern i helsestasjons- og skolehelsetjenesten, inkludert ved vaksinasjon [Internet]. Oslo: Folkehelseinstituttet; 12. May 2020 [updated 12. May 2020, cited 7. September 2020]. Available at: https://www.fhi.no/nettpub/coronavirus/helsepersonell/helsestasjons--og-skolehelsetjenesten/
Table 1, 3, 4 and figure 1 have been updated due to terminology changes (from «communities» to «districts») and different wording in the answers taken from the survey.
































Comments