Infection control at nursing homes during the COVID-19 pandemic
Nursing homes have had better routines, training of personnel, and access to testing and PPE during the coronavirus pandemic than the picture painted in the media.
Background: Frail elderly people with multimorbidity are particularly susceptible to and at greater risk than younger people of becoming seriously ill and dying from COVID-19. All health and care institutions are required to have an infection control programme that gives written guidelines for general infection control measures and for examination, treatment and care of patients. Most residents of Norwegian nursing homes are frail, susceptible to illness and have multiple morbidities. Media reports indicate that institutions of this kind have a shortage of personal protective equipment (PPE). Hard numbers are not available on the extent or severity of this shortage. It has also been reported that insufficient training and inadequate routines have caused major challenges in institutions where infection has occurred.
Objective: We wanted to chart how ward managers in nursing homes assess their ability to handle infection control, as well as their access to PPE, testing of personnel and patients, infection control routines, and competency of the personnel. We also wanted to compare wards with and without cases of COVID-19 infection.
Method: We developed our own electronic questionnaire that we gave to ward managers in nursing homes and conducted a cross-sectional study with a descriptive, explorative design.
Results: A total of 82 nursing homes agreed to participate in the study, and we received responses from 93 ward managers. Access to PPE, the use of equipment, and training are better than the picture painted in the media. A number of wards faced challenges in terms of compliance with infection control rules, such as maintaining a physical distance, spot-disinfection, and personnel that work in multiple locations. There were only a few differences between wards with infection and wards without infection.
Conclusion: Norwegian nursing homes are generally doing a good job with infection control, but there is nonetheless room for improvement. Training of personnel in crucial areas of health care such as infection control should be made mandatory and not be left up to the initiative of the individual employee. With regard to the staffing situation, there are still challenges related to the shortage of registered nurses and the reliance on part-time top-up jobs that cause many care workers to work in multiple locations. This may result in a greater risk of infection during the current epidemic and in future epidemics.
Frail elderly people with multimorbidity are particularly susceptible to and at greater risk than younger people of becoming seriously ill and dying from COVID-19 (1–3), and we must take measures to limit the spread of infection, especially among vulnerable individuals (4).
All health and care institutions are required to have an infection control programme that gives written guidelines for general infection control measures and for examination, treatment and care of patients (5).
There must also be a system for monitoring infections at institutions and guidelines for detecting and restricting outbreaks of infection. The system must be designed to ensure that infections can be quickly discovered and identified, and it must be clear who has the medical and organisational responsibility for the infection control measures (5).
Research on COVID-19
A literature review of studies up to March 2020 showed that the course of illness in people over 70 years of age develops more rapidly than in other age groups (2). Nursing home residents have a higher mortality rate from COVID-19 than elderly people who live at home (1, 6).
Most residents of Norwegian nursing homes are frail, susceptible to illness and have multiple morbidities (7). Norwegian health authorities recommend that as a general rule, patients living in nursing homes, and who become ill with COVID-19, should be treated in the nursing home rather than being hospitalised (8).
In Norway, the average age of those who die from COVID-19 is 83 years old (9), and 60 per cent of them had been living in a nursing home or another municipal health and care institution (9). Media reports indicate that institutions of this kind have a shortage of personal protective equipment (PPE) (10).
However, hard numbers are not available on the extent or severity of this shortage. It has also been reported that insufficient training and inadequate routines have caused major challenges in institutions where infection has occurred (11).
We have not found scientific publications or other systematic descriptions of the situation that substantiate or negate these reports.
Status review of Norwegian nursing homes
During the week of 23–27 March 2020, the Norwegian National Advisory Unit on Ageing and Health (Ageing and Health), in cooperation with the Norwegian Directorate of Health, conducted a review of Norwegian nursing homes. Those who responded worked primarily in clinical positions on nursing home wards, such as registered nurses, healthcare workers and doctors.
They were asked the following questions: ‘What kind of challenges are you facing in your workplace as a result of the coronavirus outbreak? What are the consequences for the patients, their family members and the personnel? What measures have been implemented?’
This status review revealed that healthcare personnel were worried about the challenges of complying with the infection control rules, access to PPE, effective routines and competency of the personnel (unpublished memorandum).
It was also brought to light that it could be difficult to get personnel with COVID-19 symptoms tested. One month later, Norway saw a significant increase in the number of patients with COVID-19.
Objective of the study
Given the situation, we wanted to conduct a study that would chart how ward managers in nursing homes assess their ability to handle infection control, how ready access they have to PPE, whether they have routines for testing personnel and patients, whether they have routines for infection control, and how they ensure the personnel have the necessary competency.
We assumed that it would be easier to uncover how infection control measures functioned in wards that had cases of COVID-19 infection. We therefore wanted to compare wards with and without infection.
Method
Questionnaire
We designed a questionnaire based on three sources: 1) government guidelines on infection control in connection with the coronavirus crisis (12), 2) concerns about the situation of infection control that had been reported in the media, and 3) a less extensive survey of the coronavirus situation in nursing homes conducted by the Ageing and Health Unit.
First we defined important thematic areas (13–15), and then we identified sub-themes, before formulating the final draft questions. The themes included managing the risk of infection, access to PPE, testing, access to diagnostic and treatment equipment, infection control routines, and information and training.
The questionnaire consisted of 28 yes/no questions and 17 questions with the following response options: ‘very seldom or never’, ‘quite seldom’, ‘occasionally’, ‘quite often’, ‘very often or always’.
In addition, each theme had a field for comments and further explanation. We also registered the type of ward and the county in which the ward was located.
The questionnaire was piloted in two nursing home wards in order to assess its relevance, clarity and ease of understanding, as well as the length of time it took to complete. No changes were made in the form after the piloting. The two forms are included as part of the overall data.
Sample and implementation
The target group was managers of nursing home wards. The term ‘ward’ is defined as an independent administrative unit with its own manager. Some wards consisted of multiple units such as suites of rooms or groups of staff with the same manager.
First we contacted the head of the institution by email, then by telephone. We asked for permission to contact the ward managers to obtain information about the situation regarding infection control on the wards.
The ward managers could choose between answering questions in a structured interview on the telephone or receiving the questions as a Questback survey by email. We did not create a list with links to the responses. Questback was a general link that did not allow for tracking those who had responded.
Six employees from the Ageing and Health Unit were charged with collecting the data from a sample of nursing homes. The first and second authors performed some of the data collection as well.
We took a strategic sample of nursing homes from small, medium and large municipalities in all of the counties in Norway. To ensure that we included wards that had experience with COVID-19 patients, we also included nursing homes that were known to have or have had cases of infection.
Recruitment and data collection were conducted in the period of 22–30 April 2020.
Analysis
We used descriptive statistics with a description of numbers and percentages. We highlight some of the free-text responses when it seems appropriate for a complete understanding. Wards that had or had had infection were compared with wards without infection.
We performed Chi-square tests and Fisher’s exact tests to test the statistical certainty of any differences between the wards with and without infection.
We tested yes/no questions directly and dichotomised questions with the response options of ‘very seldom or never’, ‘quite seldom’, ‘occasionally’, ‘quite often’, ‘very often or always’. The responses ‘quite often’ and ‘very often or always’ were given a value of 1, and the remaining three responses were given a value of 0.
The tables show the distribution of all the response options, while the statistical tests were performed on the dichotomised values.
Ethical considerations
This study investigates health services, not the circumstances of individual patients or employees, and therefore, it was not submitted to the Regional Committees for Medical and Health Research Ethics (REK). Information was provided anonymously, and as such, the study does not come under the purview of the Data Protection Officer either.
Results
We contacted 89 nursing homes. At two nursing homes we were not able to contact the right person, one nursing home declined to participate without giving a reason, and four declined to take part because of excessive workloads, primarily due to the coronavirus.
Altogether 82 nursing homes with 93 wards participated in the study. There were a maximum of two wards from the same nursing home.
All the Norwegian counties are represented. The most participants were from Viken county (16 wards) and the fewest from Troms and Finnmark counties (three wards). A total of 16 wards (17.2 per cent) had or had had cases of infection.
These wards were divided among six counties. The forms had seven comment fields, and 71 ward managers wrote responses in at least one of the comment fields.
Risk of infection
Three questions dealt with restrictions on personnel’s options to work in multiple locations (Table 1), and three involved the potential to maintain a physical distance between personnel and patients and among patients (Table 2).
Of the wards with infection, eight of them (50 per cent) had introduced a ban on working both at other institutions and in home care services. Seven of these had also prohibited personnel from working on other wards at the same institution.
Of the eight wards that said they had introduced a ban on working in other places, two wards stated that they nonetheless had personnel working at other institutions or in home care services.
A significantly larger percentage of the wards without infection reported that they ‘quite often’ or ‘very often or always’ had situations in which maintaining the recommended distance between the care worker and the patients was impossible.
It could be especially challenging to comply with infection control rules for residents with dementia.
When asked whether the residents’ behaviour led to cleaning challenges, most wards with infection responded that they ‘quite often’ or ‘very often or always’ had challenges in this area (Table 2).
In their free-text comments, many ward managers wrote that they tried to not let their personnel work in different locations or on different wards, but that this could be difficult to implement because many employees worked very limited hours and registered nurses are often responsible for several wards.
Several of them wrote that it was impossible to maintain the recommended distance between care worker and residents, especially in personal hygiene care situations. It could be especially challenging to comply with infection control rules for residents with dementia. One ward manager explained that they had established set groups of residents at mealtime.
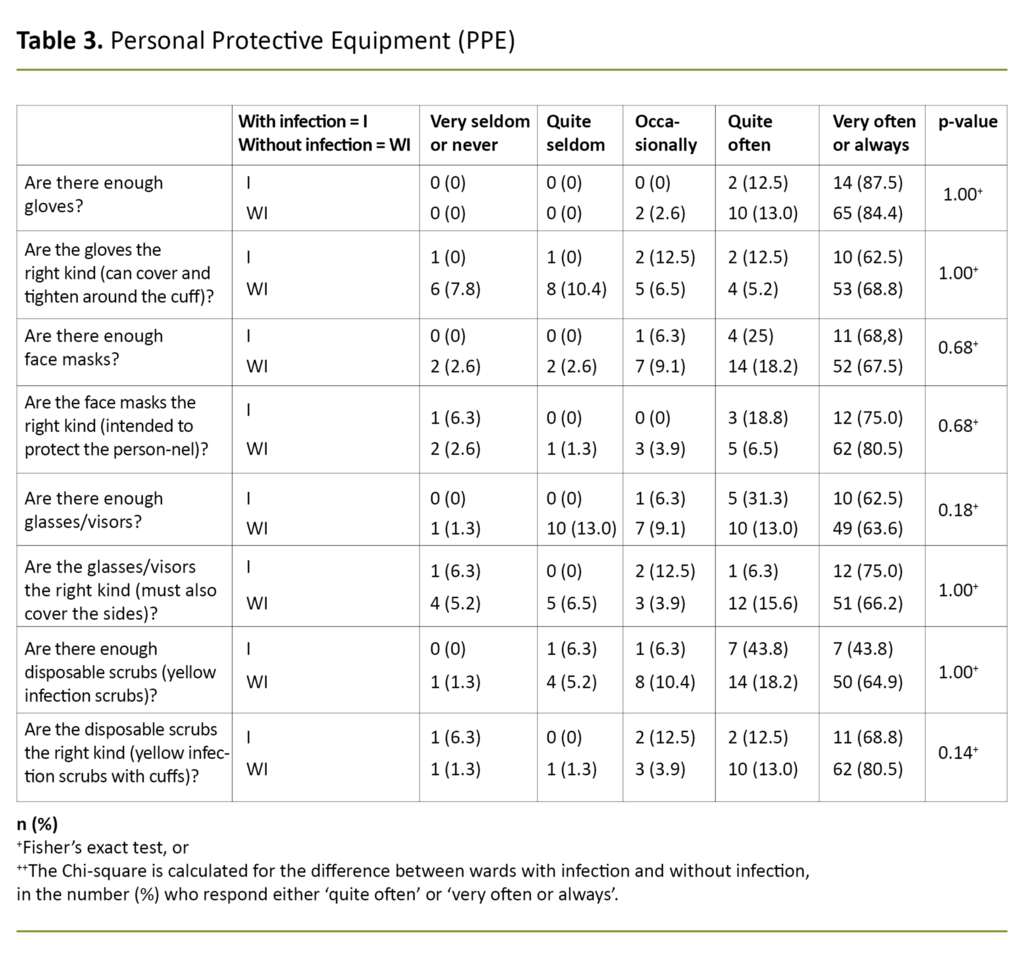
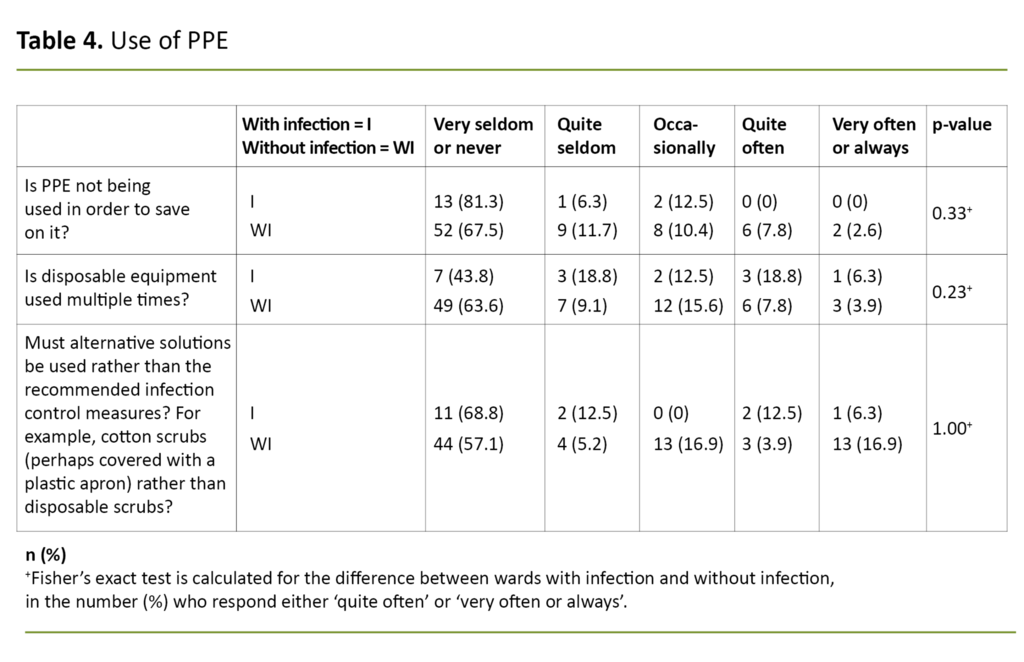
PPE
We asked 13 questions about access to and use of PPE, four questions about whether the nursing home had adequate PPE, and four questions about whether they had the right kind of equipment for the situation (Table 3).
Of the wards without infection, 63 of 77 (81.8 per cent) said that they could easily acquire PPE when they needed it, while 15 of 16 wards with infection (93.8 per cent) gave the same response.
More wards with infection (75 per cent) than those without infection (46.8 per cent) kept PPE in locked storage, but there was no difference in the availability of equipment, regardless of whether or not it was locked up.
Face masks were reused several times when there were no documented cases of infection.
We asked three questions about the use of PPE (Table 4). In their free-text comments, respondents referred to uncertainty about and a shortage of equipment in an early phase (three to four weeks prior to this study), but they said that they had sufficient PPE now (in the last week of April 2020).
Several respondents noted that they did not have any cases of COVID-19 infection yet and that they were concerned about having enough PPE if the infection came to their nursing home. In the beginning, some used alternative equipment that had not been approved, but most stated that they had adequate equipment at the time of the survey.
Some reported that it was difficult to obtain appropriate PPE, such as face masks, visors and gloves with long cuffs. When a COVID-19 infection was confirmed, they did not save on PPE, but they did use alternative equipment when assisting residents with personal care. Face masks were reused several times when there were no documented cases of infection.
Testing and medical equipment
With regard to testing of both personnel and patients, 90 of the wards (96.8 per cent) reported that they had clear-cut routines, and 85 of the wards (91.4 per cent) stated that violations of testing routines for personnel had occurred ‘quite seldom’ or ‘very seldom or never’.
This was also the case for patients in 89 of the wards (95.7 per cent). Altogether 82 wards (88.2 per cent) stated that they had enough testing equipment ‘very often or always’.
All except two wards had pulse oximeters, and all except one ward had oxygen equipment. Eight wards (8.6 per cent) did not have equipment to administer oxygen to several patients at once, and 24 wards (25.8 per cent) had only one pulse oximeter.
Routines
All the wards except one responded that the local authority had established special routines for infection control in connection with the coronavirus, and 83 wards (89.2 per cent) said that they had established special routines for this same purpose on the ward.
A total of 49 wards (52.7 per cent) had designated individuals (or functions) on each shift with responsibility for ensuring that the routines were being followed. Regarding the questions about routines, there was no difference between the wards with and without infection.
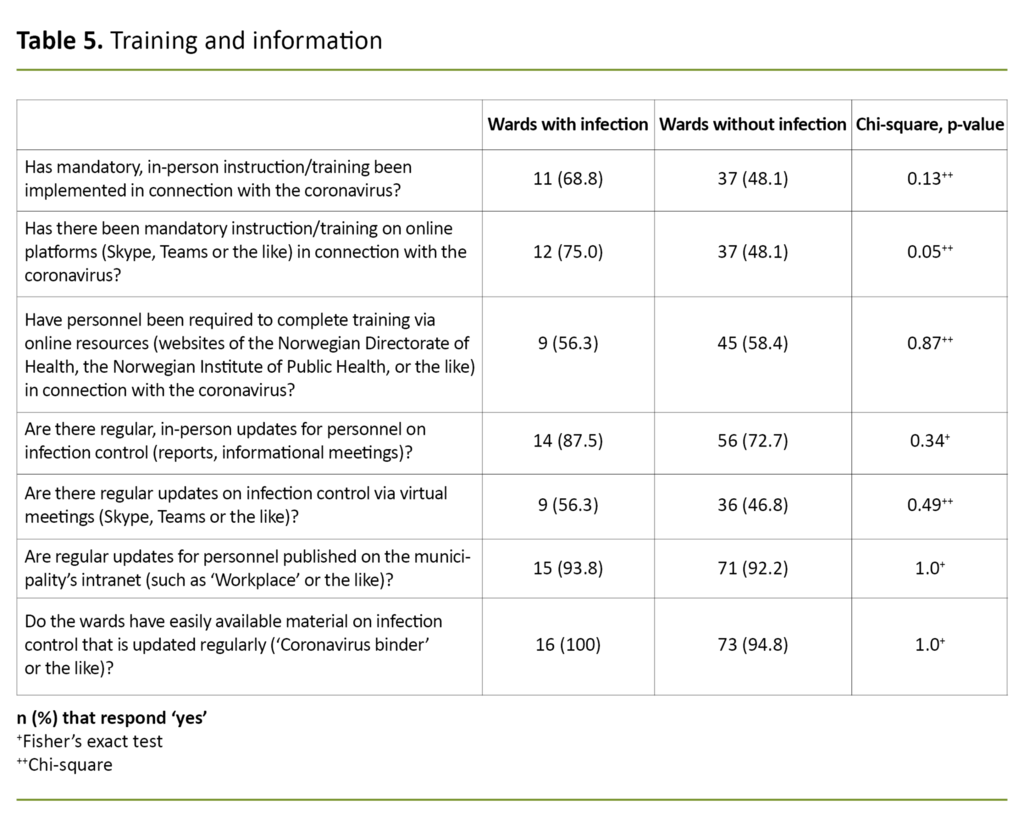
Knowledge, information and training
We asked eight questions about information and training. Altogether 74 wards (80 per cent) responded that they had one or more kinds of mandatory training on infection control in connection with the coronavirus (responded ‘yes’ to at least one of the three questions in Table 5).
The remaining 19 wards reported that they made arrangements so that their employees could view the training material published on the websites of the Norwegian Institute of Public Health and the Norwegian Directorate of Health.
Other
Altogether 78 wards (84.8 per cent) responded that the local authority had established a municipal ‘coronavirus department’, and 38 wards (41.3 per cent) had made physical or building-related changes in connection with the coronavirus.
There was no difference in how wards with and without infection responded to these two questions. Fifteen wards (93.8 per cent) with infection reported that they had made changes to shift patterns or had redistributed personnel, while 34 wards without infection (44.7 per cent, p-value < 0.01) stated that they had made changes to shift patterns or had redistributed personnel.
Discussion
This study shows that access to PPE, use of equipment, and training are better than the impression we had prior to the survey.
There were only a few differences between wards with infection and wards without infection.
A number of wards faced challenges in terms of compliance with infection control rules, such as maintaining a physical distance, spot-disinfection, and disallowing personnel from working in multiple locations. There were only a few differences between wards with infection and wards without infection.
Wards with infection allowed personnel to work in multiple locations
We expected that wards with infection in particular would have prevented personnel from working in other locations. It is surprising that half of these wards had personnel working in other locations and that only a little more than half of the wards had introduced restrictions against this.
Except for prohibiting employees from working on other wards at the same institution, the wards with infection were no different from those without infection. To be able to cover all shifts, many wards rely on personnel who work relatively short hours.
Studies show that those who work in these kinds of top-up jobs are often ‘forced’ to work in several different places to earn a normal income (16). In addition, it came to light that registered nurses often have responsibility for several wards, which creates challenges for preventing and controlling infection. It has also been argued that personnel who work on several different wards contribute directly to transmission of the virus (17).
A review conducted by Stockholm County of its 227 elderly nursing home residents revealed that the more employees who came in contact with the patients, the greater the danger was of the residents becoming infected with the virus (18, 19). Having a permanent, stable staff who do not work in other locations is perhaps the most important improvement that can be made to control infection.
Difficult to maintain a physical distance
A total of 55 wards (59.1 per cent) stated that it was ‘quite often’ or ‘very often or always’ difficult for patients to maintain a physical distance between them. The comments show that individuals with dementia who do not understand the situation present the greatest challenge.
Because more than 80 per cent of nursing home residents have dementia, the institutions must be especially mindful of this and try to find good solutions. The solution with set groups, as one ward described, would perhaps be practical to implement and make it possible to limit the infection to one group only.
Eighty wards (87 per cent) (Table 2) stated that it was ‘quite often’ or ‘very often or always’ impossible to maintain a physical distance between care workers and residents in all situations. The finding that 87 per cent of wards were usually not able to comply with the government’s distancing recommendation is to be expected given that most patients need physical assistance.
When a safe distance cannot be maintained, basic infection control routines must be followed, and PPE must be used in some situations as well (12).
The comments indicate that in situations like these, the personnel reused equipment and used alternative equipment. They used the same face mask for an entire shift and wore cotton scrubs in cases where they previously had used disposable scrubs.
Many had PPE
As Table 3 shows, a large majority of the ward managers responded that they had access to compliant PPE. The comments show that this had not been the case the entire time, but that the situation had improved.
In nursing homes without infection, respondents expressed concern that the equipment they had would not last long if they had an outbreak of the virus. However, as regards reported shortages of PPE, there was no distinction between the percentage of responses received from wards with infection and wards without infection.
A large majority of the wards had clear-cut routines for when a person should be tested.
Before the study, reports indicated that personnel and patients in nursing homes were not always being tested, even though the criteria called for this (20).
The figures in our study show that a large majority of the wards had clear-cut routines for when a person should be tested and that these routines were generally followed. This finding indicates that testing has improved.
No clear-cut responsibility for infection control
All the wards stated that the local authority had adopted special routines for infection control. Some wards did not have their own routines, but instead followed common routines introduced for the whole nursing home or municipality.
In our view, the fact that only 49 of 93 wards stated that they have designated employees (or functions) on each shift with responsibility for ensuring routines are followed shows that many wards have not clarified who is responsible for infection control on the individual shifts and that this may mean infection control is inadequate.
Although four of five wards had one or more kinds of mandatory training, 19 wards (17.0 per cent) had left the responsibility for staying informed about infection control up to the individual employee.
Although arrangements were made for employees to watch the training videos from the Norwegian Institute for Public Health, we believe it is unfortunate that not everyone was ensured the necessary infection control training.
Strengths and weaknesses of the study
This study has not investigated the actual infection control preparedness through observation, but is based on responses from ward managers at nursing homes.
This may introduce information bias because managers do not necessarily have detailed information about how infection control preparedness is being experienced by those who work most closely with the patients.
Moreover, there is a risk that ward managers, who of course have the highest administrative responsibility in the wards, including for adequate infection control preparedness, may describe the situation in positive terms to protect their own reputations.
The survey encompasses a moderate number of nursing homes that were not randomly selected. This limits the study’s generalisability somewhat, although the response rate is high.
Four nursing homes with major challenges from coronavirus infection in their wards chose not to participate in the study. Nevertheless, 16 of the 93 wards that responded to the survey had or had had patients with COVID-19 infection.
In several instances, two wards from the same nursing home responded to the survey. Since all the responses were anonymous, we had no opportunity to identify the responses that came from different wards in the same nursing home.
We did not account for this factor in the analyses, which may have resulted in less variation between responses than if only one ward from each nursing home had responded.
Conclusion
This study shows that the situation regarding routines, training of personnel, and access to PPE at Norwegian nursing homes is better than the picture painted in the media.
During the time from the first case of infection in Norway and up to the end of April 2020, much has presumably fallen into place with regard to PPE, testing of personnel and residents, routines and training. However, there is room for improvement.
With regard to the staffing situation, there are still challenges related to the shortage of registered nurses and the reliance on part-time top-up jobs that cause many care workers to work in multiple locations. This may result in a greater risk of infection during the current epidemic and in future epidemics.
Measures to reduce employees’ need to work in several different institutions should be a part of normal operations. In addition, the question of how residents who cannot comply with infection control measures can live together as usual, without constituting a risk for an entire nursing home, should be explored.
Training of personnel in crucial areas of health care such as infection control should be made mandatory and not be left up to the initiative of the individual employee.
We believe that the findings from this study are important in the future planning of infection control measures at nursing homes – for municipal leaders, institution directors and ward managers.
References
1. McMichael TM, Currie DW, Clark S, Pogosjans S, Kay M, Schwartz NG, et al. Epidemiology of Covid-19 in a long-term care facility in King County, Washington. The New England Journal of Medicine. 2020;382:2005–11. DOI: 10.1056/NEJMoa2005412
2. Wang L, Wang Y, Ye D, Liu Q. Review of the 2019 novel coronavirus (SARS-CoV-2) based on current evidence. International Journal of Antimicrobial Agents. 2020:105948. DOI: 10.1016/j.ijantimicag.2020.105948
3. Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with Acute Respiratory Distress Syndrome and death in patients with Coronavirus Disease 2019 pneumonia in Wuhan, China. JAMA Internal Medicine. 13.03.2020. DOI: 10.1001/jamainternmed.2020.0994
4. Fonn M. Korona: Unngå å bli syk, bruk smittevernutstyr riktig. Sykepleien. 11.03.2020. Available at: https://sykepleien.no/2020/03/korona-unnga-bli-syk-bruk-smittevernutstyr-riktig (downloaded 15.05.2020).
5. Forskrift 17.06.2005 nr. 610 om smittevern i helse- og omsorgstjenesten. Available at: https://lovdata.no/dokument/SF/forskrift/2005-06-17-610 (downloaded 15.05.2020).
6. Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;323(18):1775–6. DOI: 10.1001/jama.2020.4683
7. Jorgensen LB, Thorleifsson BM, Selbaek G, Saltyte Benth J, Helvik AS. Physical diagnoses in nursing home residents – is dementia or severity of dementia of importance? BMC Geriatrics. 2018;18(1):254.
8. Helsedirektoraret. Koronavirus – beslutninger og anbefalinger. Oslo: Helsedirektoratet; 2020. Available at: https://www.helsedirektoratet.no/veiledere/koronavirus/kommunehelsetjenesten-og-tannhelsetjenesten/sykehjem?malgruppe=undefined (downloaded 12.05.2020).
9. Folkehelseinstituttet. COVID-19 – Dagsrapport – torsdag 23. april 2020. Oslo: Folkehelseinstituttet; 2020. Available at: https://www.fhi.no/contentassets/e110607a67df46cbba8e30a443264a73/vedlegg/tidligere-dagsrapporter/2020.04.23-dagsrapport-covid-19.pdf (downloaded 24.04.2020).
10. Muladal A, Engen T. KS slår alarm: Alvorlig mangel på smittevernutstyr. VG. 21.04.2020. april.
11. Wallum S. Mener det er omfattende systemsvikt ved flere sykehjem. Adresseavisen. 20.04.2020.
12. Folkehelseinstituttet. Råd til sykehjem og andre heldøgnsplasser under covid-19-pandemien. Oslo: Folkehelseinstituttet; 2020. Available at: https://www.fhi.no/nettpub/coronavirus/helsepersonell/sykehjem-og-smittevern-mot-covid-19/?term=&h=1 (downloaded 13.05.2020).
13. Boynton PM, Greenhalgh T. Selecting, designing, and developing your questionnaire. BMJ. 2004;328(7451):13125.
14. Haraldsen G. Spørreskjemametodikk: etter kokebokmetoden. Oslo: Ad Notam Gyldendal; 1999.
15. Wärneryd B. Att fråga – om frågekonstruktion vid intervjuundersökningar och postenkäter. Örebro: Statistiska Centralbyrån; 1993.
16. Amble N. Forsøk og erfaringer med arbeidstidsordninger som reduserer uønsket deltid i turnus – en oppsummering. Oslo: Arbeidsforskningsinstituttet; 2008. Report no. 4/08.
17. Fagbladet/NTB. Fagforbundet mener deltidsstillinger på sykehjem kan ha forsterket koronakrisen: Fagbladet. 31.03.2020. Available at: https://fagbladet.no/nyheter/fagforbundet-mener-deltidsstillinger-pa-sykehjem-kan-ha-forsterket-koronakrisen-6.91.692087.ddb050a0b6 (downloaded 12.05.2020).
18. Wikén J, Salihu D, Velizelos A. SVT granskar: Så tog sig coronaviruset in på Sveriges äldreboenden. Stockholm: SVT. 10.05.2020. Available at: https://www.svt.se/nyheter/inrikes/svt-granskar-sa-tog-sig-coronaviruset-in-pa-sveriges-aldreboenden (downloaded 13.05.2020).
19. Region Stockholm. Kunskaper från enkät ska minska smittspridning på äldreboenden Stockholm: Region Stockholm; 04.05.2020. Available at: https://www.sll.se/nyheter-stockholms-lans-landsting/2020/05/kunskaper-fran-enkat-ska-minska-smittspridning-pa-aldreboenden/ (downloaded 10.06.2020).
20. Aas O, Dommerud T. Sykehjem i fem kommuner skiller seg ut. Her har over 40 prosent av alle koronadødsfallene skjedd. Aftenposten. 23.04.2020.

































Comments