COVID-19: Initiation of breastfeeding during a global pandemic
The infection control measures may have impacted negatively on the breastfeeding assistance provided for first-time mothers in postnatal facilities. There was also a greater reliance on breast-milk substitutes than normal.
Background: Breastfeeding and breast-milk benefit the health of mothers and their infants in a number of ways. For women to be able to master breastfeeding, it is important that they receive support from their partners, and that the healthcare facility has a structured and positive approach to breastfeeding. The Mother-Baby Friendly Initiative provides a quality standard for postnatal services in Norway. The infection control measures that were introduced by the government during the coronavirus pandemic may have affected the breastfeeding assistance provided postnatally.
Objective: The objective was to describe the breastfeeding assistance made available to first-time mothers during the period of strictest infection control measures in the coronavirus pandemic, and how the breastfeeding worked out.
Method: We conducted a descriptive cross-sectional study using an online questionnaire developed specifically for this study. We recruited the women via social media.
Results: We included a total of 821 women in our analyses. Half the sample felt they had received good assistance with breastfeeding. The surveyed women had received little information and guidance compared to the level expected of a baby-friendly ward. The partner’s presence did not influence the level of information imparted to the women. Those who spent more than two days in a postnatal facility, received more information and guidance. Almost half the sample gave their babies a breast-milk substitute while in the postnatal facility. This is a larger percentage than what is reflected in Norwegian surveys of infant feeding. Approximately 70 per cent of the surveyed women were exclusively breastfeeding two weeks after giving birth.
Conclusion: It appears that the infection control measures may have impacted negatively on the breastfeeding assistance provided for first-time mothers in postnatal facilities. We have also identified greater reliance on breast-milk substitutes, which may have meant that fewer women were exclusively breastfeeding, and that the duration of the breastfeeding period was reduced. In this study, the proportion of women who were exclusively breastfeeding at two weeks postpartum was lower than in other surveys, yet the study cannot conclude that this was caused by the infection control measures. Research is required to help us understand how the infection control measures affected the longer-term breastfeeding outcomes for these women.
There is wide agreement in medical circles that breastfeeding and breast-milk are important for the health of infants and their mothers (1–3). The World Health Organization (WHO) recommends exclusive breastfeeding of infants during the first six months, after which breastfeeding should continue alongside solids until the child is two years of age or older (4).
Breastfeeding is a physiological process influenced by hormonal changes during pregnancy and postpartum, and it involves skills that need to be learnt. Breastfeeding success is closely linked to the mother’s motivation and confidence in her own ability to breastfeed. In turn, these factors are influenced by attitudes and knowledge in society, among the woman’s family and at the healthcare facility she attends (5). The support and assistance received will influence the duration and extent of her breastfeeding efforts (6).
Her partner can influence the initiation of breastfeeding and the duration of the breastfeeding period by providing practical assistance, encourage breastfeeding and being alert to the woman’s needs. When the woman and her partner cooperate over the breastfeeding, the woman will gain greater control of the breastfeeding outcomes and greater confidence in her own ability to breastfeed (7).
Healthcare facilities have a unique role to play in promoting breastfeeding, as this is where women tend to spend the first days with their new-born child. The guidelines for postnatal care therefore recommend that mothers are not discharged from the postnatal facility before breastfeeding is well established or the offer of assistance from the municipal healthcare service is considered sufficient (8). Studies show that if mother and baby go home early, this does not have an adverse effect on breastfeeding as long as the woman is offered at least one home visit (9).
The Mother-Baby Friendly Initiative
The global Mother-Baby Friendly Initiative was launched by WHO and UNICEF in 1989 in order to promote breastfeeding (10). The initiative was introduced in Norway in 1993 and currently constitutes the benchmark standard for facilities that provide maternity and postnatal services, in compliance with recommendations issued by the Norwegian Directorate of Health (8, 11).
The Mother-Baby Friendly Initiative comprises the ‘Ten Steps to Successful Breastfeeding’ (Appendix 1), which must be adopted before healthcare facilities can refer to themselves as Baby-Friendly (12). The steps are intended to promote breastfeeding and facilities must meet the standards for information and guidance. Several studies have found that the Mother-Baby Friendly Initiative increases the proportion of women who breastfeed (13, 14).
Infection control measures in connection with COVID-19
In January 2020, a new coronavirus was discovered in China, and this quickly spread to other parts of the world. On 12 March 2020, WHO declared the outbreak a pandemic. Norwegian authorities introduced extensive and invasive infection control measures in society in general and in healthcare facilities specifically (15).
The recommendation for childbirth and postnatal services was that partners should only be present during the active delivery stage and for two hours thereafter (16). This meant that all postnatal facilities were asked to bar the presence of partners.
Another recommendation was to reduce the length of stay in postnatal facilities, preferably to less than 48 hours (17). For many first-time mothers, this was a shorter period than normal, and breastfeeding could not be expected to be fully established at this early stage (18).
Furthermore, the Norwegian Directorate of Health recommended the introduction of a number of infection control measures on the wards, which brought increased focus on disinfection, isolation and changes to daily routines (16). These changes may have increased staff workloads, which in turn may have affected the time they had available to spend with each individual woman.
Pandemics represent an ever-present risk, and the situation may well occur again in the future. Can we learn something that we can use if this happens again? It is therefore important to find out if the changes made to ward practices affected the women’s initiation of breastfeeding. This knowledge will enable us to improve current practices.
The objective of the study
We wanted to investigate the outcomes of the breastfeeding assistance provided by postnatal facilities during the period of strictest infection control. The study aimed to describe the breastfeeding assistance that first-time mothers received during the period of strictest coronavirus infection control, and how the breastfeeding initiation worked out.
Method
This was a quantitative cross-sectional study involving a survey conducted using an online questionnaire.
Sample
The study population were first-time mothers who had given birth in Norway between 12 March and 12 May 2020. We excluded women whose children had spent time in neonatal intensive care units, and women who had not delivered to term. This was because these children may have had different nutritional needs than healthy full-term infants.
Data collection
We collected data by means of the University of Oslo’s (UiO) Nettskjema online questionnaire service. We found no pre-existing questionnaire suitable for our purposes. Our questionnaire was therefore specially designed for this survey.
In drafting the questionnaire, we drew inspiration from a questionnaire about breastfeeding guidance and breastfeeding problems (18). The Mother-Baby Friendly Initiative is the quality standard adopted by most hospitals, so we chose to formulate our questions along the lines of the ‘Ten Steps to Successful Breastfeeding’. We received input from the Norwegian National Advisory Unit on Breastfeeding in this process. In order to ensure that all questions were easy to understand and relevant, and that exhaustive response options were provided, we conducted a pilot test among women who met the inclusion criteria in part or in full. Their feedback resulted in additional explanatory text for some questions and additional response options for others.
The questions in the questionnaire (Appendix 2, in Norwegian) were structured chronologically from delivery to returning home from the postnatal facility. The women were asked between 27 and 38 questions, as some of them were filter questions. Response options varied between Likert scales, single-answer and multiple choice.
Because we wanted to collect information from our respondents while the infection control measures were still in place, we endeavoured to distribute the questionnaires as quickly as possible. We therefore found it useful to recruit a convenience sample, which means choosing respondents based on their availability (19).
We wanted as many respondents as possible to enable generalisation of findings and therefore recruited participants through Facebook. According to Ipsos, Facebook is used by approximately 90 per cent of women between 18 and 39 years of age, and 82 per cent use the platform on a daily basis (20).
We posted the questionnaire in Facebook groups directed at mothers, including ‘Mammaklubb for bra damer’ (mummy club for cool ladies) with more than 19 000 members and ‘Ammehjelpsgruppen’ (the breastfeeding assistance group), with more than 32 000 members. We also shared the questionnaire on Facebook. The questionnaire was available online between 26 May and 26 June 2020.
Analysis
We analysed the data using IBM SPSS Statistics version 27. We wanted to survey the breastfeeding assistance that first-time mothers had received in postnatal facilities during the period of strictest infection control. We therefore chose to use descriptive statistics with frequency tables and cross-tabulations that we considered to adequately describe our research question.
The study involved only categorical data and results were presented in numbers and percentages. We used chi-square tests in cross-tabulations to test the differences between groups, and we set the significance level to 0.05. There were multiple response options for questions related to the guidance that the women received.
In order to analyse these responses, we designed a ‘Multiple response set’ in SPSS. Each response was coded into dichotomous variables (had the women received the specific item of guidance, yes or no), which were then grouped in a set.
We used frequency analyses to see how many respondents had received specific items of guidance, and cross-tabulations to identify differences with respect to length of stay in the postnatal facility and whether the partner was present.
Ethical considerations
The Norwegian Centre for Research Data considered there was no need to notify them or Regional Committees for Medical and Health Research Ethics (REK) of the study, because our plans were for an anonymous survey via the University of Oslo’s Nettskjema platform.
To ensure that all respondents would remain unidentifiable, we included no free-text fields, and all background information was provided as categorical data and kept to a minimum. Participants were considered to give their consent to taking part in the study by submitting the questionnaire.
Results
A total of 882 women responded to the survey. Based on our exclusion criteria, we removed 61 of them from the dataset, leaving 821 who were included in our analyses. In total, 79.5 per cent of the women were between 25 and 35 years of age.
There were respondents from all Norwegian counties (see Table 1), and most of them came from counties with large birthing facilities and a high population density. The majority of the women gave birth on a delivery ward or in a maternity clinic (94.3 per cent), and the proportion who delivered by caesarean section was 15.8 per cent.
One in five women (19.9 per cent) reported that their partner had been present throughout their stay in the postnatal facility. Half the sample had spent less than 48 hours in the facility.
Perception of breastfeeding assistance received in the postnatal facility
We asked the women about the extent to which they felt they had been given assistance with their breastfeeding queries while in the postnatal facility (see Table 2). Those whose partners were present, felt that they had received more support than those whose partners were not present. The women who spent less time in the maternity unit, received less support than those who spent longer.
There were significant differences between counties in terms of breastfeeding assistance. The county of Møre og Romsdal provided assistance to the largest proportion of women (66.7 per cent), while Oslo’s score was the lowest in this respect (40.7 per cent).
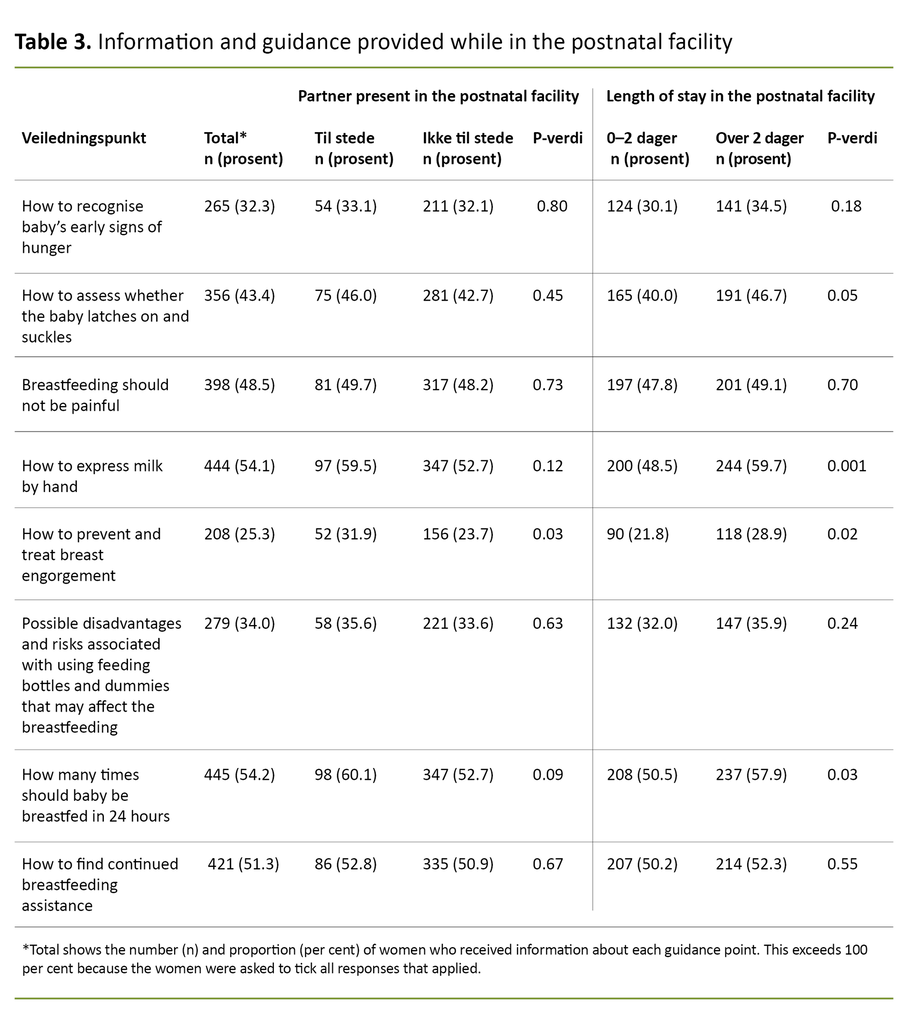
Guidance received in the postnatal facility
Table 3 shows the degree to which the women received information that reflected the ‘Ten Steps to Successful Breastfeeding’. The figures show that the women generally received little guidance. Most of them were told ‘How often to breastfeed’ (54.2 per cent).
Only 25.3 per cent of the women received information about ‘How to prevent/treat breast engorgement pains’. On this point, there was a significant difference between women who had their partners present and those who had not.
The length of stay in hospital had some influence. Among the women who spent between zero and two days, a lower proportion had received information about ‘How to express milk by hand’, ‘How to prevent/treat breast engorgement’ and ‘How often to breastfeed’.
Breast-milk substitutes
Among the women in the survey, 46.3 per cent responded that their babies received a breast-milk substitute in the first three days of life. Breast-milk substitutes were used just as frequently at birth centres (42.6 per cent) as in maternity clinics and maternity units (46.5 per cent).
More women who spent over two days in the postnatal facility gave their baby a breast-milk substitute (30.8 per cent compared to 61.9 per cent) (not in the table).
Breastfeeding status two weeks after delivery
We asked the women how their breastfeeding was going two weeks after they had given birth (see Figure 1), and 92 per cent of them were still breastfeeding. Among these, 72 per cent were exclusively breastfeeding. Women whose partners had been present reported the same breastfeeding status as women whose partners were not present.
Among the women who spent more than two days in the postnatal facility (63.8 per cent), a lower proportion was exclusively breastfeeding compared to those who spent 0–2 days in the facility (79.4 per cent) (the data are not given in the tables).
Discussion
The study results show that the infection control measures introduced at postnatal facilities are likely to have had a negative effect on first-time mothers’ perception of breastfeeding assistance received during their stay in the postnatal facility. Women who had their partner present were more satisfied with the assistance they received.
Breastfeeding guidance was found to be wanting when compared to expectations of a Mother-Baby Friendly facility. There was greater reliance on breast-milk substitutes, and fewer women were exclusively breastfeeding after two weeks compared to the results of earlier surveys.
The pandemic changed the working day
There were differences between counties with respect to the amount of help the women felt they had received. This may have been because it was left up to the individual care facility to draw up local procedures for how to enforce the recommended measures for infection control (16).
Also, there may well be differences in culture between units. One study found that the mothers’ sense of support increased when the midwife had a positive attitude to breastfeeding (21). The redistribution of resources that took place during the pandemic may have adversely affected the midwives’ attention and attitude to aspects of care such as breastfeeding.
The coronavirus pandemic has changed the working day at postnatal facilities in that staff spend time and resources on infection control measures. An increased workload and associated frustrations can have left less time available for staff to provide breastfeeding assistance, which is often a time-consuming task. Women are likely to have noticed this capacity reduction, as reflected in news stories and feature articles published in the daily press (22, 23).
Women who spent less than 48 hours in the postnatal facility, felt that they received less help.
Among the women who had their partner present, a larger proportion felt supported while in the postnatal facility. This may be because the women included the support received from their partners when answering the question.
If the healthcare personnel had less time available to spend with the women during the coronavirus pandemic, and their partner was not present, this is likely to have affected the women’s experience of support and assistance received.
Women who spent less than 48 hours in the postnatal facility, felt that they received less help. This is unfortunate, because women who go home early need significant guidance to be able to handle the challenges of breastfeeding on their own (9). When their time in the facility is reduced, the breastfeeding assistance provided should be adjusted accordingly.
Insufficient information and guidance
It is surprising that the women received little information and guidance. The guidance points are tools intended to make sure that women receive appropriate information while in a postnatal facility (11).
Most such facilities in Norway are accredited as Mother-Baby Friendly because they have been found to provide information about most of the guidance points to at least 80 per cent of women. We must therefore assume that the figures revealed in this study are significantly lower than normal (11).
The partner’s presence affected only one item of guidance. Length of stay in the facility had a greater impact. For instance, a lower proportion of the women who returned home early received information about milk pains.
Because milk pains normally occur two to four days after delivery (18), it is worrying that so few had received such information when discharged after two days and left to manage on their own.
Nor had sufficient guidance in accordance with the Mother-Baby Friendly standard been provided to women who stayed for longer than recommended in the facility during the coronavirus pandemic, so we can assume that a greater workload and changes to resource allocations will have played a part.
More extensive use of breast-milk substitutes
We found that approximately half the study sample had given their babies a breast-milk substitute while in the postnatal facility. This is a significant increase compared to the infant feeding surveys of 2013 and 2020 (24, 25).
In these surveys, 25 and 29 per cent respectively answered that they had given their baby a breast-milk substitute in the first week of life (24, 25). According to ‘Ten Steps to Successful Breastfeeding’, breast-milk substitutes should never be given unless medically indicated.
In our study, only 53.1 per cent of infants were exclusively breastfed.
In order to be accredited as a Mother-Baby Friendly facility, the hospital must be able to report exclusive breastfeeding while in the facility for at least 80 per cent of full-term babies (12). In our study, only 53.1 per cent of infants were exclusively breastfed, which demonstrates that the Mother-Baby Friendly standard was not achieved for these women during the pandemic.
Our results do not tell us if there was a medical reason for the increased reliance on breast-milk substitutes, but the volume involved suggests that in general, there was no such indication. This is supported by the fact that in our study, the use of breast-milk substitutes was just as high at birth centres as in maternity units and clinics.
Only healthy mothers and infants are routed to birth centres, so no medical indication for a breast-milk substitute would therefore be expected (26). It may be the case that breast-milk substitutes were given because the postnatal facilities were busy during the pandemic. ‘Ten Steps to Successful Breastfeeding’ specifies that a lack of resources is not a sufficiently good reason to give a breast-milk substitute (12).
Breastfeeding status two weeks after delivery
National infant feeding surveys undertaken in 2013 and 2020 show that the proportion of women who exclusively breastfed their babies after two weeks, was 84 and 85 per cent respectively (24, 25). By comparison, the exclusive breastfeeding proportion in our study was considerably lower (71.6 per cent).
Unlike our sample, the women who responded to the infant feeding surveys included both primiparous and multiparous women. This may have been one reason for the difference.
A woman’s partner plays an important part in establishing the breastfeeding (7, 27). Nevertheless, our study found no significant difference between the women whose partners were present and those whose partners were not present with respect to breastfeeding status at two weeks postpartum. Only a small group of women were allowed to have their partner present (19.9 per cent).
We can assume that the partners who were allowed to be present, had their freedom of activity restricted due to infection control measures.
We can assume that the partners who were allowed to be present, had their freedom of activity restricted due to infection control measures. This may have affected their opportunity to provide respite and make things easier, which is an important part of the partners’ support function. This may have affected the impact of their presence (7).
It was a surprising finding that women who spent a short time in the facility were more likely to exclusively breastfeed, despite the fact that they reported having received less guidance than the women who spent longer in the facility. This may be associated with the fact that there was a greater reliance on breast-milk substitutes among those who stayed for longer. This factor is known to influence exclusive breastfeeding (28).
We must take account of the fact that those who stayed for longer, may have had medical issues that gave rise to breastfeeding challenges.
Strengths and weaknesses of the study
The fact that the study used a convenience sample can have affected the transferability of its findings. This data collection method means that we cannot tell how many women could have taken part, and who opted not to respond. The high number of respondents is a strength.
In Norway, approximately 3800 (29) first-time mothers give birth in any two-month period, so our response rate is around 23 per cent. The respondents are similar to the general birthing population in terms of measured background variables.
Among the women in our study, 79.5 per cent were between 25 and 35 years of age. The average age of first-time mothers in Norway in 2019 was 29.7 years (29). The proportion of women who delivered by caesarean section (15.8 per cent), is similar to the caesarean section prevalence in the Norwegian birthing population (15.9 per cent) (29).
Recruitment took place via social media.
Recruitment took place via social media. Despite the fact that the majority of the population makes use of such media, we must assume that we failed to reach parts of the population. Additionally, the various Facebook groups that we chose to use as vehicles of recruitment, may have affected the sample and can potentially have produced a biased sample.
In an effort to counteract any such bias, we asked a number of different groups to share the questionnaire, which they did. Studies show that recruitment via Facebook can provide representative samples that match traditional data collection methods (30).
Any cross-sectional study runs the risk of potential memory bias (19). However, this study was conducted soon after the events we were asking about and the risk that respondents may have failed to remember will therefore be small.
It is a weakness of the study that the questionnaire that we used had not been validated. We therefore spent considerable time on formulating the questionnaire, taking heed of input from the Norwegian National Advisory Unit on Breastfeeding and conducting a pilot test.
We chose descriptive statistics and bivariate analyses, which in our opinion are appropriate choices that suit the objective of the study. Any interpretation of the results must take account of the simple analytic approach.
Conclusion
We have found that the breastfeeding assistance that first-time mothers received during the coronavirus pandemic did not meet the Mother-Baby Friendly standard. Since most hospitals have been accredited to this standard, we can assume that the infection control measures impacted negatively on the assistance they received. Only half the sample felt that they received good breastfeeding support in the postnatal facility.
Breast-milk substitutes were administered more widely and insufficient information and guidance were provided. We know that this affects the number of women who exclusively breastfeed, and the duration of their breastfeeding. The proportion of women who were exclusively breastfeeding two weeks after delivery, was lower in our study than in other studies.
Because our sample included only first-time mothers, we cannot conclude that the infection control measures are the definitive cause of this low proportion.
This study looked at breastfeeding in the two-week period after birth. In order to understand the full consequences of the infection control measures, it will be necessary to study breastfeeding progression in the longer term.
References
1. Victora CG, Bahl R, Barros AJD, França GVA, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. The Lancet. 2016;387(10017):475–90. DOI: 10.1016/s0140-6736(15)01024-7
2. Chowdhury R, Sinha B, Sankar MJ, Taneja S, Bhandari N, Rollins N, et al. Breastfeeding and maternal health outcomes: a systematic review and meta-analysis. Acta Paediatrica. 2015;104(S467):96–113. DOI: 10.1111/apa.13102
3. Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, et al. Breastfeeding and maternal and infant health outcomes in developed countries. 2007. Evidence Report Technology Assessments nr. 153. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4781366/ (downloaded 10.05.2020).
4. Verdens helseorganisasjon. Global strategy for infant and young child feeding. Genève: Verdens helseorganisasjon; 2003. Available at: https://apps.who.int/iris/bitstream/handle/10665/42590/9241562218.pdf?sequence=1. (downloaded 02.05.2020).
5. Rollins NC, Bhandari N, Hajeebhoy N, Horton S, Lutter CK, Martines JC, et al. Why invest, and what it will take to improve breastfeeding practices? The Lancet. 2016;387(10017):491–504. DOI: 10.1016/s0140-6736(15)01044-2
6. McFadden A, Gavine A, Renfrew MJ, Wade A, Buchanan P, Taylor JL, et al. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database of Systematic Reviews. 2017(2). DOI: 10.1002/14651858.CD001141.pub5
7. Davidson EL, Ollerton RL. Partner behaviours improving breastfeeding outcomes: an integrative review. Women and Birth. 2020;33(1):e15–e23. DOI: 10.1016/j.wombi.2019.05.010
8. Helsedirektoratet. Nytt liv og trygg barseltid for familien: Nasjonal faglig retningslinje for barselomsorgen. Oslo: Helsedirektoratet; 2014.
9. Brown S, Small R, Argus B, Davis PG, Krastev A. Early postnatal discharge from hospital for healthy mothers and term infants. Cochrane Database of Systematic Reviews. 2002(3). DOI: 10.1002/14651858.CD002958
10. Verdens helseorganisasjon. Guideline: protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services. Genève: Verdens helseorganisasjon; 2017. Available at: https://www.who.int/publications-detail/9789241550086 (downloaded 02.05.2020).
11. Nasjonal kompetansetjeneste for amming. Mor-barn-vennlig standard (MBV) 2019. Available at: https://oslo-universitetssykehus.no/fag-og-forskning/nasjonale-og-regionale-tjenester/nasjonal-kompetansetjeneste-for-amming-nka/mor-barn-vennlig-standard-mbv (downloaded 02.05.2020).
12. Nasjonal kompetansetjeneste for amming. Mor-barn-vennlig standard (MBV). Ti trinn for vellykket amming. Oslo; 2018.
13. Pérez‐Escamilla R, Martinez JL, Segura‐Pérez S. Impact of the baby‐friendly hospital initiative on breastfeeding and child health outcomes: a systematic review. Maternal & Child Nutrition. 2016;12(3):402–17. DOI: 10.1111/mcn.12294
14. Beake S, Pellowe C, Dykes F, Schmied V, Bick D. A systematic review of structured compared with non-structured breastfeeding programmes to support the initiation and duration of exclusive and any breastfeeding in acute and primary health care settings. Maternal & Child Nutrition. 2012;8(2):141–61. DOI: 10.11124/jbisrir-2011-121
15. Folkehelseinstituttet. Fakta om covid-19-utbruddet. Oslo: Folkehelseinstituttet; 2020. Available at: https://www.fhi.no/nettpub/coronavirus/fakta-og-kunnskap-om-covid-19/fakta-om-covid-19-utbruddet/?term=&h=1 (downloaded 30.03.2020).
16. Helseaktuelt. Min koronahverdag: Jordmor Mai-Britt i beredskap på Ringerike sykehus. Helseaktuelt 26.03.2020. Oslo: Helsedirektoratet; 2020. Available at: https://medium.com/helseaktuelt/min-koronahverdag-jordmor-mai-britt-i-beredskap-p%C3%A5-ringerike-sykehus-273e1dddd3fd (downloaded 10.05.2021).
17. Oslo universitetssykehus. Fødeavdelingen. Viktig informasjon om koronasituasjonen ved Føde- og barselseksjonene ved OUS. Oslo: Oslo universitetssykehus. Available at: https://oslo-universitetssykehus.no/avdelinger/kvinneklinikken/fodeavdelingen#viktig-informasjon-om-koronasituasjonen-ved-fode--og-barselseksjonene-pa-ous (downloaded 10.05.2021).
18. Tufte E. Norske kvinners ammeproblemer [Master's Thesis]. Nordic School of Public Health; 2005.
19. Ringdal K. Enhet og mangfold: Samfunnsvitenskapelig forskning og kvantitativ metode. 4th ed. Bergen: Fagbokforlaget; 2018.
20. Ipsos. Sosiale medier tracker Q2’20 2020. Available at: https://www.ipsos.com/sites/default/files/ct/publication/documents/2020-07/ipsos_some_2._kvartal_2020.pdf (downloaded 05.05.2020).
21. Ekström AC, Thorstensson S. Nurses and midwives professional support increases with improved attitudes; Design and effects of a longitudinal randomized controlled process-oriented intervention. BMC Pregnancy Childbirth. 2015;15:275.
22. Thomassen AL. Å bli mor under en pandemi. Dagsavisen. 02.09.2020. Available at: https://www.dagsavisen.no/debatt/a-bli-mor-under-en-pandemi-1.1766957 (downloaded 02.09.2020).
23. Solheim M. Fødsel under pandemi: Marlene (25) føler ho blei frårøva den største opplevinga i livet. NRK. 09.10.2020. Available at: https://www.nrk.no/trondelag/fodsel-under-pandemi_-marlene-_25_-foler-ho-blei-frarova-den-storste-opplevinga-i-livet-1.15167440 (downloaded 09.10.2020).
24. Helsedirektoratet. Amming og spedbarns kosthold. Landsomfattende undersøkelse 2013. Oslo: Helsedirektoratet; 2014.
25. Folkehelseinstituttet. Spedkost 3. Landsomfattende undersøkelse av kostholdet blant spedbarn i Norge, 6 måneder. Oslo: Folkehelseinstituttet; 2020.
26. St.meld. nr. 12 (2008–2009). En gledelig begivenhet. Om en sammenhengende svangerskaps-, fødsels- og barselomsorg. Oslo: Helse- og omsorgsdepartementet; 2008.
27. Hunter T, Cattelona G. Breastfeeding initiation and duration in first-time mothers; Exploring the impact of father involvement in the early post-partum period. Health Promot Perspect. 2014;4(2):132–6.
28. Häggkvist A-P, Brantsæter AL, Grjibovski AM, Helsing E, Meltzer HM, Haugen M. Prevalence of breast-feeding in the Norwegian Mother and Child Cohort Study and health service-related correlates of cessation of full breast-feeding. Public Health Nutrition. 2010;13(12):2076–86. DOI: 10.1017/s1368980010001771
29. Folkehelseinstituttet. Medisinsk fødselsregister. Oslo: Folkehelseinstituttet; 2019. Available at: http://statistikkbank.fhi.no/mfr/ (downloaded 02.10.2020).
30. Thornton L, Batterham PJ, Fassnacht DB, Kay-Lambkin F, Calear AL, Hunt S. Recruiting for health, medical or psychosocial research using Facebook: systematic review. Internet Interventions. 2016;4:72–81. DOI: 10.1016/j.invent.2016.02.001



































Comments