How public health nurses use sources of knowledge
Public health nurses consider themselves to be adept at finding and assessing national guidelines, but feel less proficient at assessing research-based knowledge.
Background: Public health nursing is constantly evolving; the profession must adjust to new focus areas, new professional demands, new tasks and more responsibilities.
Objectives: The study’s objectives were to identify 1) the sources of knowledge that public health nurses use in practice, 2) what skills enable public health nurses to find and assess research and national guidelines, 3) what barriers public health nurses encounter as they endeavour to find and assess research and national guidelines, and 4) influences that impact on their skills in assessing research-based knowledge.
Method: This is a cross-sectional study which involved 708 public health nurses completing an online questionnaire. We used statistical analyses to investigate their use of sources of knowledge and the factors that may influence their skills in assessing research-based knowledge.
Results: National guidelines, knowledge acquired while training as a public health nurse, personal experience and guidelines issued by local authorities were the most commonly used sources of knowledge. The most significant barriers reported were a shortage of time to find research, and the challenge of understanding articles written in English. The public health nurses considered that they were generally adept at finding and assessing national guidelines, but that they were less proficient at assessing research-based knowledge. The odds were significantly greater that public health nurses with a Master’s degree, and public health nurses in full-time employment, would consider themselves adept at assessing research.
Conclusion: National guidelines constitute the source of knowledge most frequently used by public health nurses. In order to implement evidence-based professional practice, public health nurses must be proficient at assessing the recommendations set out in national guidelines in combination with other sources of knowledge. A future national competence and development centre for services provided at community and school health care centres may come to play an important role in implementing national guidelines and safeguarding the quality of procedures issued by local authorities.
The general population’s access to research is ever-increasing. Public health nurses and other nurses must therefore be prepared to answer questions and to discuss findings from research. In line with the requirements for safety and high standards, the objective set out in the consultation draft of the new national professional guidelines for community and school health care centres is to offer health promotional and preventive services (1).
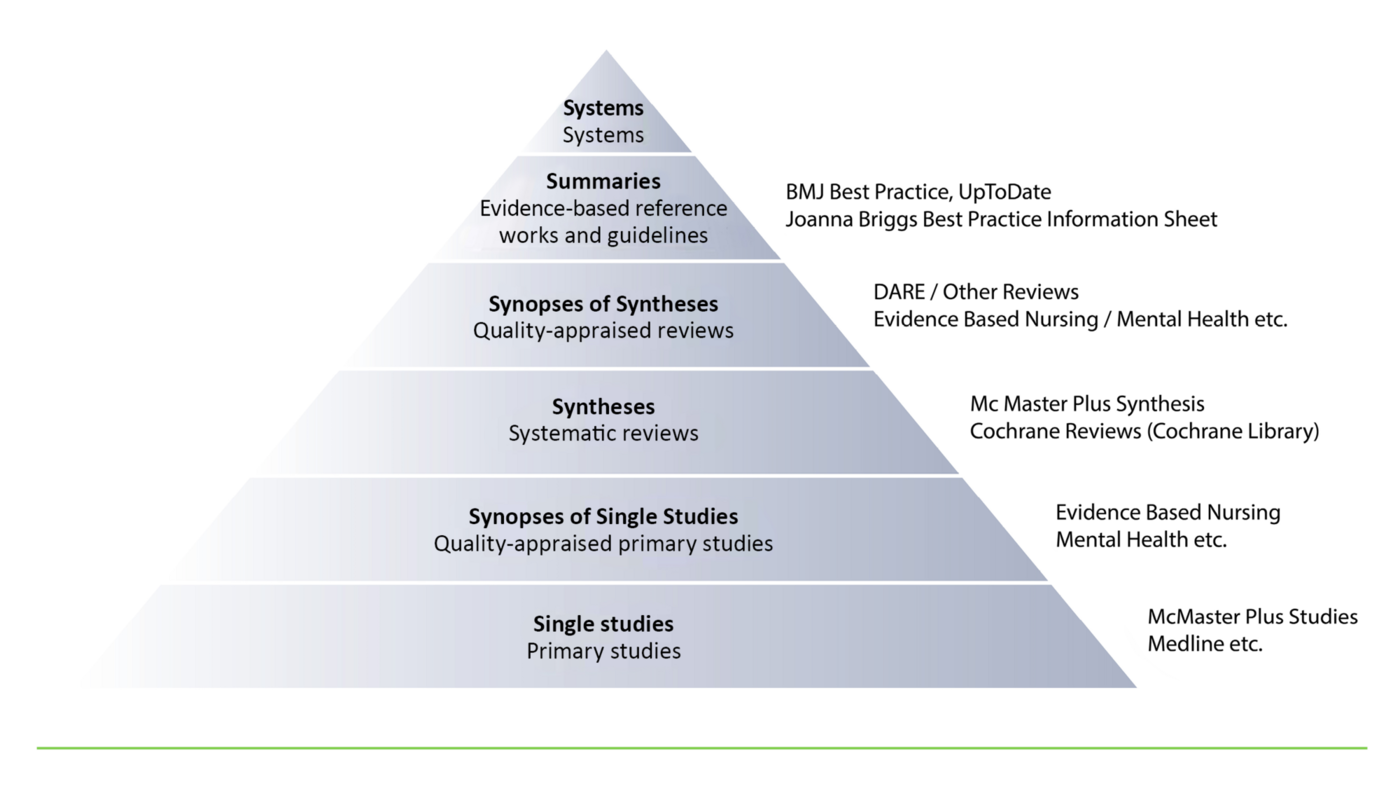
Evidence-based practice involves making decisions in a professional capacity based on a combination of systematically obtained research-based knowledge, evidence-based knowledge and the patient’s wishes and needs in the given situation (2–4). It is an important principle in evidence-based practice to search for research summaries and evidence-based reference works and guidelines before looking for single studies (5), as shown by the 6S pyramid (see figure 1).
Earlier studies
A Norwegian study conducted among nurses in the municipal health service (6) showed that the most frequently used sources of knowledge were personal experience, the experience of colleagues, knowledge acquired while training as a nurse, the patient’s wishes, and health legislation. Research findings were rarely used.
Some nurses read articles published in the Sykepleien Forskning nursing research journal, but this knowledge was never used as a basis for clinical decision-making. The nurses also reported limited understanding of the importance of updating their professional knowledge.
A study conducted by Austvoll-Dahlgren and Helseth among public health nurses investigated barriers and facilitators to the use of research in consultations about childhood vaccinations. They also investigated what sources of knowledge are most frequently used (7). These were found to be national guidelines and other information issued by the Norwegian Institute of Public Health.
The public health nurses commented that research formed an important basis for making good decisions in practice. Research also provided a good base from which to meet the demands of parents, and to develop professionally. Nevertheless, the public health nurses were reluctant to search for research articles. They did not see it as their role to seek out knowledge on their own initiative; rather, they saw their responsibility and role to be one of trusting the information and guidelines issued by public authorities.
One review article showed that nurses working in the primary and specialist health services encountered known barriers such as a shortage of time, knowledge and skills to find and assess research articles (8). This review article included studies about the implementation of evidence-based practice from several countries.
The study’s objective
There are many international and several Norwegian studies that survey how nurses in the specialist health service utilise sources of knowledge (9–12). Fewer studies have been conducted among nurses in the primary health service, but there is a growing body of research in this field as well (6, 13, 14). No earlier studies have surveyed how Norwegian public health nurses use sources of knowledge in general.
If we know how public health nurses use sources of knowledge, this may influence the way that evidence-based practice is taught at public health nursing courses. It may also give us knowledge about the demand for refresher courses within the field of practice. It is important that public health nurses work from evidence. There is a need to look closer into what sources of knowledge public health nurses use as a basis for their professional decision-making.
The study’s objectives were to identify 1) the sources of knowledge that public health nurses use in practice, 2) what skills enable public health nurses to find and assess research and national guidelines, 3) what barriers public health nurses encounter as they endeavour to find and assess research and national guidelines, and 4) influences that impact on their skills in assessing research-based knowledge.
Method
Sample and data collection
In this cross-sectional study, we wished to survey the population of professionally active public health nurses practising in Norway. According to Statistics Norway, a total of 4 368 public health nurses were in work in 2014 (15). This study’s sample was recruited among the members of the NNO Professional interest group of public health nurses (LaH) who had registered an email address.
The LaH provided information about the survey in a newsletter distributed to 3 130 email addresses. The study was carried out in the period between 26 October 2015 and 5 December 2015. Two reminders were issued.
Translation and adaptation of the questionnaire
We wanted to investigate whether an instrument already existed that could be used for the purpose of this survey. Consequently, we searched for studies that utilised questionnaires associated with the appraisal of evidence-based practice (14, 16–18). To restrict our search further, we only considered questionnaires that had already been translated into Norwegian, and which had been used for studies carried out in Norway (9, 10, 17, 19–21).
The ‘Developing Evidence-Based Practice Questionnaire’ (DEBP) (18) turned out to be the one best suited to our study. This had been translated into Norwegian in accordance with the World Health Organisation’s translation procedure (10, 19). Its Norwegian translator, Anne Dalheim, has granted us permission to use the Norwegian version of the questionnaire.
We needed to adapt the questionnaire to suit the public health nurses’ work situation. Consequently, we left out all questions that were clearly aimed at nurses in hospitals. These questions referred to patient information, conferring with doctors, and new treatments and medication.
Furthermore, we changed certain questions to make them appropriate for public health nursing. For example, ‘my personal experience of nursing patients over time’ was changed to ‘my personal experience of public health nursing over time’.
We also added some questions for the purposes of our adapted version. These questions referred to sources of knowledge such as guidance, cross-disciplinary cooperation, placements and service user feedback. Moreover, we left out a section of the original questionnaire that dealt with the implementation of practice changes, because the study’s objective was not to look at changing practices.
The questionnaire
The adapted questionnaire was tested in a pilot study at a health care centre that employs ten public health nurses. We removed question no. 2 concerning ‘my intuitive sense of what appears to be the right thing to do for the service user or the family’ because the public health nurses interpreted this question in different ways.
We also omitted question number 4 concerning ‘what has worked for me for a long time’. The public health nurses felt it was difficult to distinguish this question from number 3: ‘the way I have always been doing it’, which we retained. Reliability testing shows that the adapted instrument’s internal consistency is good (Cronbach’s α = 0.87) (22).
The questionnaire had one introductory question: ‘Are you currently working as a public health nurse?’ Those who replied no to this question were excluded from the survey. There were 40 compulsory questions that were graded on a five-point Likert scale. The last question was open-ended: ‘Do you have anything to add?’ This provided an opportunity to respond by way of free text comment. We stated that it would take approximately eight to ten minutes to complete the questionnaire.
The questionnaire was divided into four sections. Section one asked what sources of knowledge the public health nurses were using in their work. Section two asked the public health nurses how they assessed their own skills in finding, assessing and using various sources of knowledge. Section three asked what barriers the public health nurses encountered when they endeavoured to find and assess research articles and national guidelines.
Section three of the original DEBP questionnaire concerned the nurses’ skills in finding, assessing and using various sources of knowledge. This was moved forward and became part two. The last section of our questionnaire surveyed the demographic variables.
Ethical considerations
The study was reported to and approved by the Norwegian Centre for Research Data, formerly Norwegian Social Science Data Services We secured anonymity by distributing the questionnaire by email via Questback. Participation was voluntary, and we informed the participants that by completing the survey, they gave their consent to taking part in the study.
Data analysis
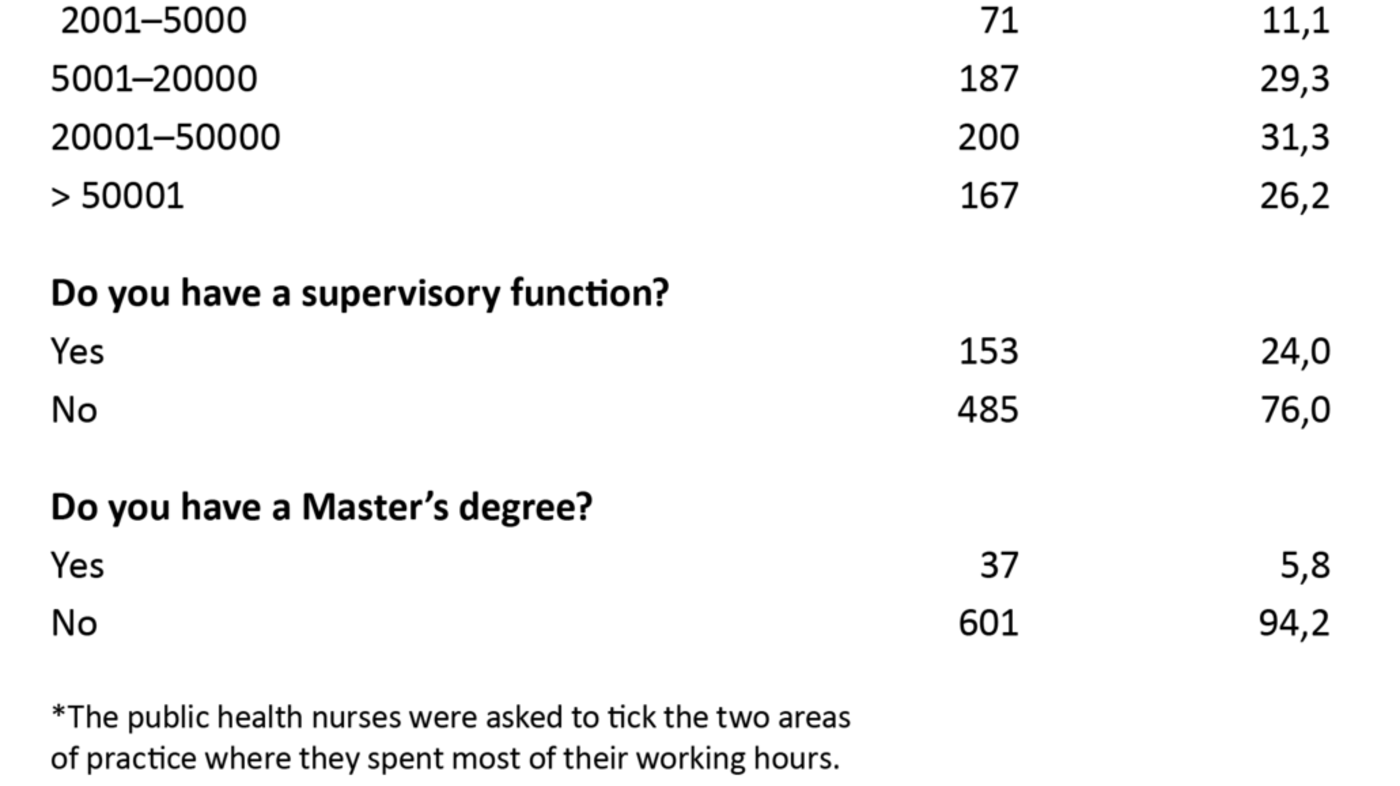
We used descriptive statistics to describe the sample and to get an indication of the frequency distribution of all categorical variables (see table 1). Logistic regression analysis was used to investigate the factors that might influence the public health nurses’ opinion of their own skills in assessing research-based knowledge.
We had reason to believe that working conditions might differ with the municipalities’ population size, so this was controlled for in the logistic regression model (23). The significance level was set to 0.05 in all analyses. The statistics software SPSS for Mac, version 23 was used for the analysis of all responses except the free text comments. These were subjected to content analysis (24).
Results
Of the 3 130 registered public health nurses, 708 completed the questionnaire, which gives a response rate of 22.6 per cent. We excluded 70 of them from the study because they answered no to the introductory question of whether they were currently working as a public health nurse. Of the public health nurses who completed the full questionnaire, 638 were included.
Two thirds of the included public health nurses were aged between 41 and 60, and over half of them had been working as public health nurses for between six and twenty years. Approximately one quarter indicated that they had a supervisory function, and almost six percent responded that they held a Master’s degree (see table 1). The content analysis led us to divide the free text responses into three main themes: time, competence and attitudes.
The sources of knowledge used by public health nurses
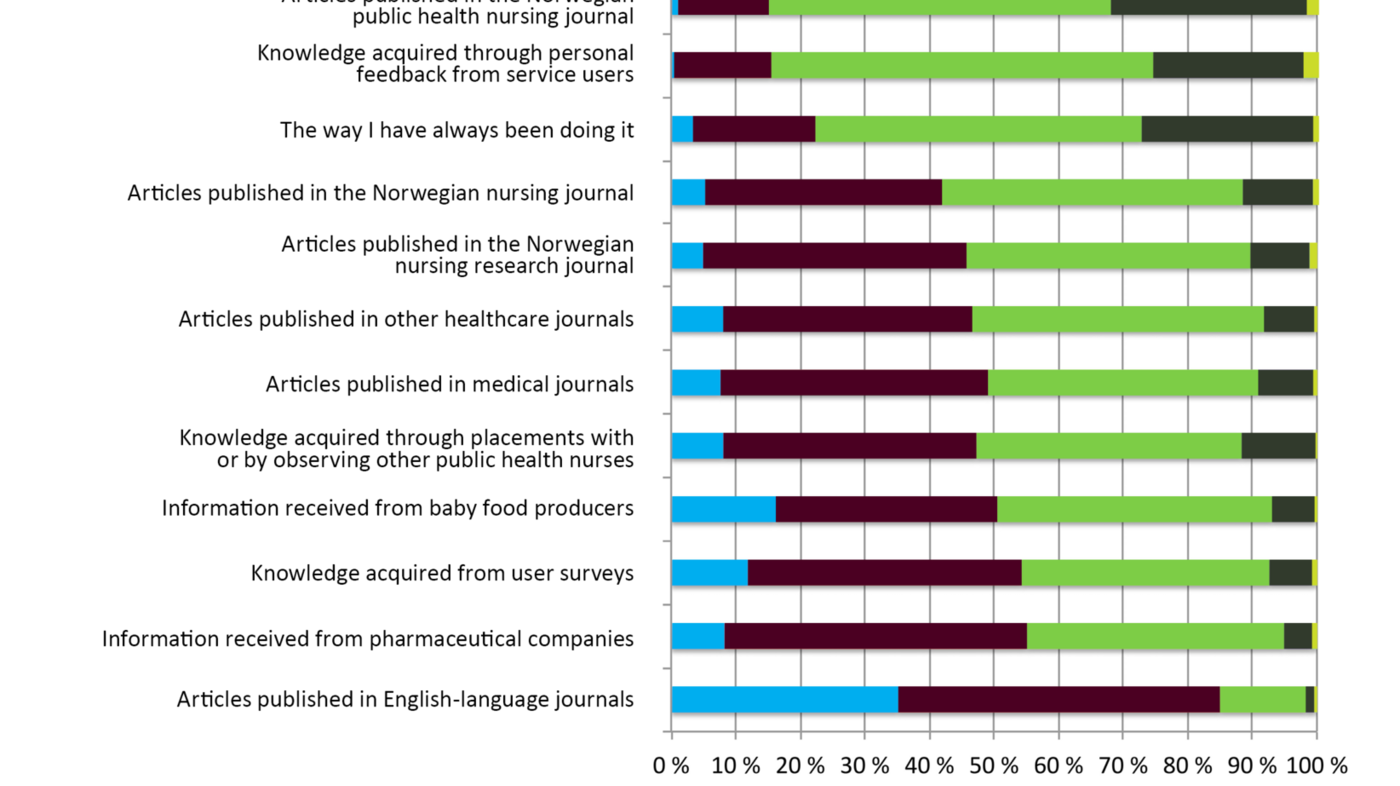
The public health nurses’ ranking of their sources of knowledge showed that the four most frequently used sources were national plans and guidelines, knowledge acquired while training as a public health nurse, personal experience, and guidelines and procedures issued by their local authorities. Other commonly used sources of knowledge included external courses and internal medical meetings, as well as knowledge shared among public health nursing colleagues.
The Norwegian public health nursing journal was the most commonly read literature, while other journals were less popular. Articles published in English-language journals represented the least frequently used source of knowledge (see figure 2)..
Skills and barriers
The public health nurses reported that they were generally proficient or expert at finding and assessing national guidelines. Fewer reported that they were proficient or expert at finding and assessing research-based knowledge.
They indicated that the greatest barrier to finding research articles was a shortage of time (see figure 3). Similarly, it was also apparent from the questionnaire’s free text comments that insufficient time was a barrier to finding research. Another major barrier was the language used in articles published in English, which they found difficult to understand. Furthermore, the public health nurses did not feel confident in their ability to appraise the quality of research articles.
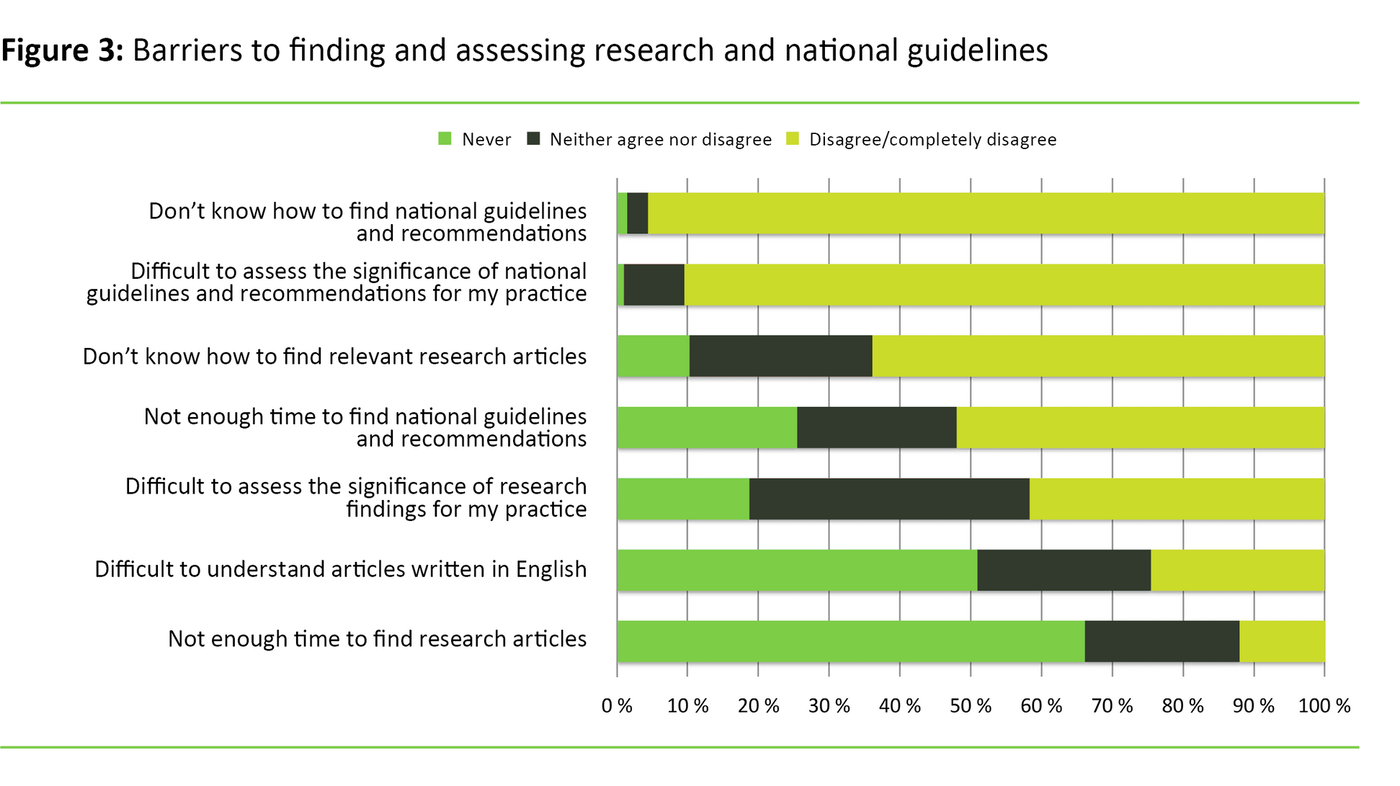
Shortage of time was an insignificant problem with respect to seeking out national guidelines and recommendations. Less than five per cent of the public health nurses indicated that they were in complete agreement or in agreement with a statement that it was difficult to find national guidelines and recommendations. Only ten per cent indicated that they were in complete agreement or in agreement with a statement that it was difficult to assess the significance of guidelines for their own practice.
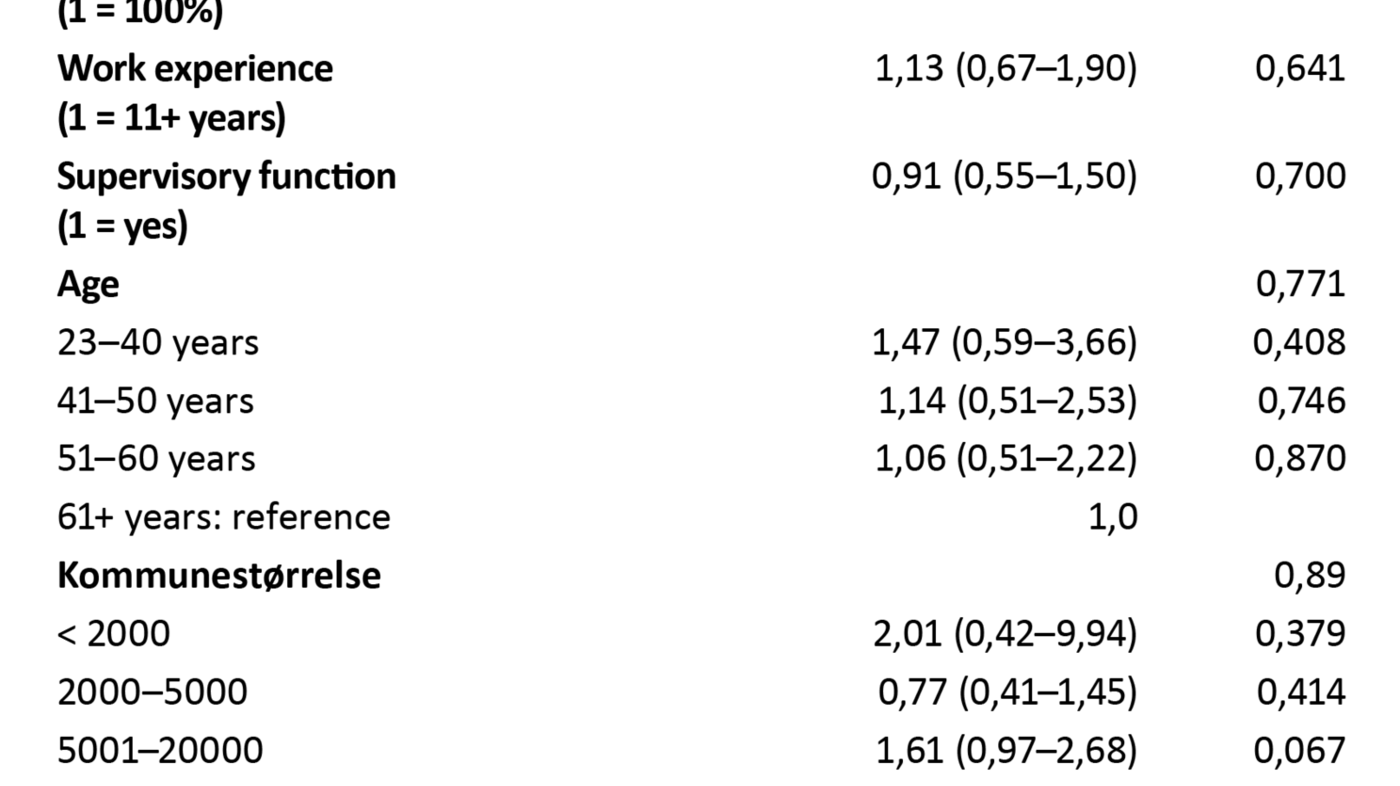
Having controlled for age, work experience, full-time equivalent ratio, municipality population size, and supervisory function, we found that two factors significantly influenced the public health nurses’ opinion of their own skills in assessing research. Compared with the public health nurses without a Master’s degree, the odds were more than 3.5 times greater (OR 3.72, p = 0.033) that public health nurses who hold a Master’s degree will assess themselves as being fairly good, proficient or expert at assessing research.
Compared with public health nurses in part-time employment, the odds were 1.5 times greater (OR 1.49, p = 0.045) that public health nurses in a full-time job will consider themselves to be fairly good, proficient or expert at assessing research (see table 2).
Free text responses
Time
The public health nurses feel that their day-to-day work regime allows far too little time for them to read and look up research articles and other professional literature: ‘That’s something I have to do at home, to keep updated.’ They report that due to great work pressure, it is often down to chance whether they are able to keep updated.
Competence
The public health nurses feel they receive little management support for attending courses and completing specialty training programmes, and that such professional development is never rewarded in the form of increased pay or new tasks. In their view, holding a Master’s degree is important for being able to understand and apply evidence: ‘I have attended several refresher courses since I first trained as a public health nurse, so have kept professionally updated. It is sad that there is little local recognition of our professional competencies.’
Attitudes
The public health nurses believe that research-based knowledge should be given a greater focus in practice: ‘There are far too many personal views, and a prevailing attitude that ʻwe have always done thingsʼ [this way].’ They feel that professional development comes a long way down on the list of priorities, and that practices and attitudes differ with respect to keeping updated.
Discussion
This study shows that national guidelines constitute the most frequently used source of knowledge among public health nurses. The greatest barriers to finding and assessing research include shortage of time, difficulties in understanding articles published in English and a lack of confidence in appraising the quality of research. Holding a Master’s degree, and full-time employment, are factors that significantly impact on the public health nurses’ assessment of their own competence to appraise research.
Sources of knowledge
In recent years, numerous new guidelines have been issued for public health nurses to absorb and comply with. Such guidelines are therefore becoming an increasingly important source of knowledge for public health nurses (25–29). National guidelines are professionally normative; any non-compliance will have to be based on good reasons, even if health care personnel need to use their professional discretion in making the assessment (1).
More than 90 per cent of the public health nurses in our study report that they frequently or always use national recommendations and guidelines as a source of knowledge in practice. This finding matches the findings of a study conducted in 2012 on how public health nurses use sources of knowledge in relation to paediatric vaccinations (7).
Criticism against guidelines
There are both positive and negative sides to having increasing numbers of national guidelines. There is little research and knowledge concerning the impact of ever more national guidelines on the professional practice of public health nurses. Many argue that the simplest way that public health nurses can base their practice on relevant and updated research, is to comply with national guidelines. On the other hand, the criticism levelled at the guidelines is often aimed at their tendency to oversimplify the treatment of patients.
Criticism is also directed at their failure to accommodate the context and the patients’ multimorbidity since guidelines often deal with a single disease or an isolated condition (30, 31). There is no research that examines the degree to which this criticism affects public health nurses and their compliance with the guidelines.
Similarly, our study tells us nothing about the public health nurses’ day-to-day practical compliance with the guidelines. It appears, however, that the guidelines are increasingly influencing the public health nurses’ working day since they report on their frequent use.
The study that looked at facilitators and barriers to the use of research by public health nurses in consultations about paediatric vaccinations (7) may suggest that the public health nurses feel their responsibility is to comply with national guidelines rather than to seek out research on their own initiative.
National guidelines are based on research summaries, which make them more reliable than single studies as a basis for professional decision-making. Public health nurses should nevertheless be able to explain their actions in a better way than by simply referring to the fact that ‘this is the recommendation of the national guidelines’. One particular problem is that several of the guidelines were issued a number of years ago and have never been updated to reflect more recent research.
National guidelines are more important to public health nurses than to other nurses
Approximately 50 per cent of the public health nurses who took part in our study reported that they often or always use the guidelines and procedures issued by their local authority as a source of knowledge. Studies conducted among nurses in the primary health service rate national guidelines as an infrequently used source of knowledge, while municipal or hospital procedures are frequently used (6, 10).
Public health nurses are required to relate directly to recommendations provided by national guidelines more frequently than other nurses in the primary health service. The study’s finding that national guidelines constitute a more important source of knowledge for public health nurses than for other primary health nurses without a specialty, is therefore not unexpected.
No utilisation of research findings
In line with earlier research among nurses (6, 32, 33), our study shows that the public health nurses who completed the questionnaire rarely make direct use of research findings in their practice. This may be a cause for concern. It may be particularly challenging to transfer or ‘translate’ research findings into the context of preventive healthcare. For example, it is not unusual that programmes or initiatives whose effectiveness has been documented, fail to have the expected effect when implemented in a different context or population (34).
A method or intervention that has proved to be effective in one population will not necessarily have the same effect in a different context. In order to answer whether the intervention is effective, it is always necessary to assess not only the intervention, but also the relationship between the intervention and its context (35). There is therefore reason to assume that public health nurses need the skills to assess research. They also need to know how research can be implemented in different contexts.
Barriers and skills
Our study shows that the greatest barrier to the use of research is shortage of time. This result matches findings from earlier studies (8, 10, 14, 20, 36). The public health nurses expand on this shortage of time in their free text comments. Almost 40 per cent of them also report that they agree or fully agree with a statement that it is difficult to assess the significance of research findings for their own practice, which matches the findings of other studies (10, 13, 14).
The majority of the public health nurses found it difficult to understand articles published in English, a problem which has also been reported in other countries where English is not the native tongue (37). This language barrier restricts the public health nurses’ opportunity to obtain and assess new evidence. Their free text comments also explain that while they focus on professional development and research, time is a restricting factor.
However, this finding does not coincide with the study that demonstrated limited understanding among other primary health care nurses of the importance of updating their professional knowledge (6). Our result may be explained by the fact that all public health nurses have specialty training, which may well influence their views on professional development.
A Master’s degree is significant
Compared with public health nurses without a Master’s degree, the odds were more than 3.5 times greater that public health nurses who hold a Master’s degree will consider themselves as being fairly good, proficient or expert at assessing research. There has been much debate about the general need for a Master’s degree programme. Arguments have been put forward both for and against the trend of introducing ever more postgraduate specialty training programmes for nurses (38–40).
Nurses agree that evidence-based practice is useful to clinical work, but they lack the skills to implement such practices (41). Like other studies, our study supports the view that public health nurses with a Master’s degree will be better equipped to assess research findings (36, 42).
The odds were 1.5 times greater that public health nurses in a full-time job will consider themselves to be fairly good, proficient or expert at assessing research-based knowledge. Other studies also show that the full-time equivalent ratio impacts on the implementation of evidence-based practice (43). It is reasonable to assume that fewer working hours result in correspondingly fewer opportunities to read up on research and other professional literature or to attend courses and medical meetings during working hours.
Implications
In order to implement evidence-based work practices, the public health nurses need to be adept at assessing multiple sources of knowledge rather than solely referring to national guidelines and local procedures. This study tells us nothing about the ways that public health nurses use the various sources of knowledge. Further research is therefore required in this area.
The training
The study’s findings should impact on the teaching of evidence-based practice at public health nursing courses in order to build confidence in newly qualified public health nurses that they are able to access different sources of knowledge. Local authorities and university colleges should also consider introducing refresher courses for public health nurses in evidence-based practice and sources of knowledge.
The local authorities
Public health nursing is a widely scoped profession, and public health nurses work independently, which may suggest that the training programme for public health nursing should be at postgraduate level. It is also important that local authorities utilise the competence of public health nurses with a Master’s degree to develop the area’s service provision.
There is currently no body that holds an overarching responsibility for implementing national guidelines and safeguarding the quality of procedures issued by local authorities. Work has been on-going for some time to establish a national competence and development centre for services provided at community and school health centres (44–46). The Professional interest group of public health nurses (LaH) also recognises that there is a great demand for such a centre and has pushed for its establishment. This work should be intensified and may play an important role in achieving the objective of introducing evidence-based practice in the public health nursing service (47).
Strengths and weaknesses
A total of 3 130 public health nurses were invited to take part in the survey. Of these, 708 completed the questionnaire. This gives a response rate of 22.6 per cent, which matches that of other comparable studies (48). In 2014, a total of 4 368 public health nurses were working in Norway.
This study was able to obtain responses from 16.2 per cent of the entire population (15). The fact that we chose to recruit via LaH, may have introduced a bias in the sample. However, we have no data that might verify whether public health nurses outside the LaH are significantly different to those who are members of the LaH. Consequently, it is difficult to assess whether the findings are representative of the public health nurses who did not take part in the survey. Nevertheless, we hold the opinion that the results of the study provide a general indication of conditions within the service.
One of our study’s limitations, however, is that we have only established what the public health nurses report that they do, not what they are actually doing in practice. Neither can the study establish possible causes and effects; it can only describe associations between variables.
The modifications made to the original UKBP questionnaire proved to be so comprehensive that the results of this study cannot readily be compared with the results of studies that have employed the original English or Norwegian version of the questionnaire.
Conclusion
This study shows that national guidelines constitute the source of knowledge most frequently used by public health nurses. Public health nurses who hold a Master’s degree, and public health nurses in full-time employment, feel that they are better at assessing research-based knowledge than public health nurses without a Master’s degree, or who are in less than full-time employment.
The field of practice should consider how these resources may be better utilised. The educational institutions should also reflect on how they teach evidence-based practice and offer refresher courses for public health nurses. The establishment of a national competence and development centre for services provided at community and school health care centres will potentially have a considerable impact on the use of evidence-based practice and knowledge development in the public health nursing service.
I would like to thank Anne Dalheim for allowing me to use the Norwegian translation of the questionnaire entitled ‘Developing Evidence-Based Practice Questionnaire’ (DEBP).
References
1. Helsedirektoratet. Nasjonal faglig retningslinje for det helsefremmende og forebyggende arbeidet i helsestasjon, skolehelsetjeneste og helsestasjon for ungdom – høringsversjon. Helsedirektoratet; 2016.
2. Nortvedt MW, Jamtvedt G, Graverholt B, Nordheim LV, Reinar LM. Jobb kunnskapsbasert! En arbeidsbok. Oslo: Akribe; 2012.
3. Nasjonalt kunnskapssenter for helsetjenesten. Kunnskapsbasert praksis 2016. Available at: http://www.kunnskapssenteret.no/kunnskapsbasert-helsetjeneste(downloaded 30.10.2017).
4. Sosial- og helsedirektoratet. Kommunenes helsefremmende og forebyggende arbeid i helsestasjons- og skolehelsetjenesten.: Veileder til forskrift av 3. april 2003 nr. 450. Sosial- og helsedirektoratet; 2004. Available at: https://helsedirektoratet.no/Documents/Helsestasjon%20og%20skolehelsetjeneste/Kommunens-helsefremmende-og-forebyggende-arbeid-i-helsestasjons-og-skolehelsetjenesten.pdf(downloaded 21.11.2017).
5. DiCenso A, Bayley L, Haynes RB. Accessing pre-appraised evidence: fine-tuning the 5S model into a 6S model. Evidence Based Nursing 2009;12(4):99–101.
6. Berland A, Gundersen D, Bentsen SB. Evidence-based practice in primary care – An explorative study of nurse practitioners in Norway. Nurse Education in Practice 2012;12(6):361–5.
7. Austvoll-Dahlgren A, Helseth S. Public health nurses’ barriers and facilitators to the use of research in consultations about childhood vaccinations. Scandinavian Journal of Caring Sciences 2012;26(2):271–8.
8. Mallion J, Brooke J. Community-and hospital-based nurses’ implementation of evidence-based practice: are there any differences? British Journal of Community Nursing 2016;21(3):148–54.
9. Stokke K, Olsen NR, Espehaug B, Nortvedt MW. Evidence based practice beliefs and implementation among nurses: a cross-sectional study. BMC Nursing 2014;13(1):8.
10. Dalheim A, Harthug S, Nilsen RM, Nortvedt MW. Factors influencing the development of evidence-based practice among nurses: a self-report survey. BMC Health Services Research 2012;12:367.
11. Maaskant JM, Knops AM, Ubbink DT, Vermeulen H. Evidence-based practice: A survey among pediatric nurses and pediatricians. Journal of Pediatric Nursing 2013;28(2):150–7.
12. Renolen Å, Hjälmhult E. Nurses experience of using scientific knowledge in clinical practice: a grounded theory study. Scandinavian Journal of Caring Sciences 2015;29(4):633–41.
13. Patelarou AE, Patelarou E, Brokalaki H, Dafermos V, Thiel L, Melas CD et al. Current evidence on the attitudes, knowledge and perceptions of nurses regarding evidence-based practice implementation in European community settings: a systematic review. Journal of Community Health Nursing 2013;30(4):230–44.
14. Nilsson Kajermo K, Alinaghizadeh H, Falk U, Wändell P, Törnkvist L. Psychometric evaluation of a questionnaire and primary healthcare nurses' attitudes towards research and use of research findings. Scandinavian Journal of Caring Sciences 2014;28(1):173–85.
15. Statistisk sentralbyrå. Helse- og sosialpersonell, 2014, 4. kvartal 2014. Available at: http://www.ssb.no/arbeid-og-lonn/statistikker/hesospers/aar/2015-06-12?fane=tabell&sort=nummer&tabell=229477(downloaded 15.08.2016).
16. Leung K, Trevena L, Waters D. Systematic review of instruments for measuring nurses' knowledge, skills and attitudes for evidence-based practice. Journal of Advanced Nursing 2014;70(10):2181–95.
17. Upton D, Upton P. Development of an evidence-based practice questionnaire for nurses. Journal of Advanced Nursing 2006;53(4):454–8.
18. Gerrish K, Ashworth P, Lacey A, Bailey J, Cooke J, Kendall S et al. Factors influencing the development of evidence-based practice: a research tool. Journal of Advanced Nursing 2007;57(3):328–38.
19. Dalheim A. Faktorer som influerer på implementering av kunnskapsbasert praksis (Master's thesis): Bergen: Høgskolen i Bergen; 2011.
20. Hommelstad J, Ruland CM. Norwegian nurses' perceived barriers and facilitators to research use. AORN Journal 2004;79(3):621–34.
21. Svarthaug LA. Kunnskapsbasert praksis blant anestesisykepleiere i et norsk helseforetak. Gjøvik (Master's thesis): Høgskolen i Gjøvik; 2012.
22. Polit DF, Beck CT. Nursing Research: Generating and assessing evidence for nursing practice. 10. ed. Philadelphia: Wolters Kluwer; 2017.
23. Waldum-Grevbo KS, Haugland T. En kartlegging av helsesøsterbemanningen i skolehelsetjenesten. Sykepleien Forskning 2015;10(4):352–60. Available at: https://sykepleien.no/forskning/2015/11/en-kartlegging-av-helsesosterbemanningen-i-skolehelsetjenesten(downloaded 30.10.2017).
24. Ryghaug M. Å bringe tekster i tale – mulige metodiske innfallsvinkler til tekstanalyse i statsvitenskap. Norsk statsvitenskapelig tidsskrift 2002;4:303–27.
25. Helsedirektoratet. Nasjonale faglige retningslinjer for veiing og måling i helsestasjons- og skolehelsetjenesten. Oslo: Helsedirektoratet; 2010. Available at: https://helsedirektoratet.no/retningslinjer/nasjonal-faglig-retningslinje-for-veiing-og-maling-i-helsestasjons-og-skolehelsetjenesten(downloaded 21.11.2017).
26. Helsedirektoratet. Nasjonale faglige retningslinjer for primærhelsetjenesten. Forebygging og behandling av overvekt og fedme hos barn og unge. Oslo: Helsedirektoratet; 2010. Available at: https://helsedirektoratet.no/retningslinjer/nasjonal-faglig-retningslinje-for-forebygging-utredning-og-behandling-av-overvekt-og-fedme-hos-barn-og-unge(downloaded 21.11.2017).
27. Helsedirektoratet. Nasjonal faglig retningslinje for barselomsorgen. Nytt liv og trygg barseltid for familien. Helsedirektoratet; 2014. Available at: https://helsedirektoratet.no/retningslinjer/nasjonal-faglig-retningslinje-for-barselomsorgen-nytt-liv-og-trygg-barseltid-for-familien(downloaded 21.11.2017).
28. Sosial- og helsedirektoratet. Faglige retningslinjer for oppfølging av for tidlig fødte barn. Oslo: Sosial- og helsedirektoratet; 2007. Available at: https://helsedirektoratet.no/retningslinjer/nasjonal-faglig-retningslinje-for-oppfolging-av-for-tidlig-fodte-barn(downloaded 21.11.2017).
29. Sosial- og helsedirektoratet. Retningslinjer for undersøkelse av syn, hørsel og språk hos barn. Oslo: Sosial- og helsedirektoratet; 2006. Available at: https://helsedirektoratet.no/retningslinjer/nasjonal-faglig-retningslinje-for-undersokelse-av-syn-horsel-og-sprak-hos-barn- (downloaded 21.11.2017).
30. Alanen S, Kaila M, Välimäki M. Attitudes toward guidelines in Finnish primary care nursing: a questionnaire survey. Worldviews on Evidence-Based Nursing 2009;6(4):229–36.
31. Brean A. Et kaos. Tidsskrift for Den norske legeforening 2016;136(8):687.
32. Boström AM, Kajermo KN, Nordström G, Wallin L. Registered nurses’ use of research findings in the care of older people. Journal of Clinical Nursing 2009;18(10):1430–41.
33. Estabrooks CA, Rutakumwa W, O’Leary KA, Profetto-McGrath J, Milner M, Levers MJ et al. Sources of practice knowledge among nurses. Qualitative Health Research 2005;15(4):460–76.
34. Rychetnik L, Bauman A, Laws R, King L, Rissel C, Nutbeam D et al. Translating research for evidence-based public health: key concepts and future directions. Journal of Epidemiology and Community Health 2012;66(12):1187–92.
35. Kemm J. The limitations of ʻevidence-basedʼ public health. Journal of Evaluation in Clinical Practice 2006;12(3):319–24.
36. Baird L, Miller T. Factors influencing evidence-based practice for community nurses. Br J Community Nurs 2015;20(5):233–42.
37. Khammarnia M, Haj Mohammadi M, Amani Z, Rezaeian S, Setoodehzadeh F. Barriers to implementation of evidence based practice in Zahedan teaching hospitals, Iran, 2014. Nursing research and practice 2015. Available at: https://www.hindawi.com/journals/nrp/2015/357140/(downloaded 21.11.2017).
38. Torgersen AI. Mastersyke blant sykepleiere. Sykepleien 2015;103(1):75. Tilgjengelig fra: https://sykepleien.no/meninger/innspill/2015/01/mastersyke-et-sykepleiefenomen(nedlastet 30.10.2017).
39. Lerdal A. Vi trenger funksjonsorienterte mastergrader. Sykepleien 2014;102 (06):103. Tilgjengelig fra: https://sykepleien.no/2014/06/vi-trenger-funksjonsorienterte-mastergrader(nedlastet 30.10.2017).
40. Skogsaas B. Praksisveilederes refleksjoner om akademisering av spesialutdanningene. Sykepleien Forskning 2016;11(1):56–64. Tilgjengelig fra: https://sykepleien.no/forskning/2016/02/praksisveilederes-refleksjoner-om-akademisering-av-spesialutdanningene(nedlastet 30.10.2017).
41. Skela-Savič B, Hvalič-Touzery S, Pesjak K. Professional values and competencies as explanatory factors for the use of evidence-based practice in nursing. Journal of Advanced Nursing 2017;73(3):1910–23.
42. Cotterill-Walker SM. Where is the evidence that master's level nursing education makes a difference to patient care? A literature review. Nurse Education Today. 2012;32(1):57–64.
43. Hellier S, Cline T. Factors that affect nurse practitioners’ implementation of evidence-based practice. Journal of the American Association of Nurse Practitioners 2016;28(11):612–21.
44. Glavin K. Utkast til plan for nasjonalt kompetanse/utviklingssenter for helsefremmende og forebyggende arbeid rettet mot barn og unge. Oslo: Høyskolen Diakonova; 2005.
45. Hertzberg A, Haug H. Evaluering av utviklingssenter for Helsestasjons- og skolehelsetjenesten. Oslo: HUS, HeSo; november 2004.
46. Glavin K, Bild H, Hønningstad G, Brevik S, JacobsenS, Petersen K. Forsknings- og utviklingssenter for helsestasjons- og skolehelsetjenesten, foreløpig utkast til prosjektbeskrivelse. Oslo: IRHUS; 1998.
47. Landsgruppen av helsesøstre NSF. Nasjonalt kompetanse- og utviklingssenter for helsestasjons- og skolehelsetjenesten.: En idé og planskisse fra en prosjektgruppe i regi av Landsgruppen av helsesøstre NSF. 2009. Tilgjengelig fra: https://www.nsf.no/Content/254457/NASJONALT%20kompetansesenter%20%20Presentasjon%20(2).pdf(nedlastet 21.11.2017).
48. Sarna L, Bialous SA, Wells M, Kotlerman J, Wewers ME, Froelicher ES. Frequency of nurses’ smoking cessation interventions: report from a national survey. Journal of Clinical Nursing 2009;18(14):2066–77.










Comments