Safety measures for medication in nursing homes
New reforms and time-consuming tasks such as cleaning, preparing food and poor ICT solutions mean that nurses give less priority to safety measures in connection with medication management.
Background: Medication errors are among the most common adverse events in the health and care services. The Norwegian Coordination Reform entails that nursing homes now have increased responsibility for medical treatment and no longer merely have responsibility for nursing care. Adverse events in health care have a great potential for improvement and can be prevented by implementing safety interventions.
Purpose: To explore how safety measures function with a view to preventing the use of incorrect medication and adverse drug treatment in nursing homes.
Method: Qualitative design involving focus group interviews with nurses and student nurses, and a study of student nurses’ learning logs. The data collection started parallel with the introduction of the Norwegian Coordination Reform, and was conducted over a three year period. Data analysis was carried out by coding and categorising meaning.
Results: Nurses and student nurses perceived that safety procedures were often impracticable due to shortage of time. There was also little correlation between tasks, staffing and medication competence. There was little focus on systematic competence building, and training in handling medication was not taken sufficiently seriously.
Conclusion: This study has shown that safety measures do not function adequately, and that there is an increasing need for personnel with relevant pharmaceutical expertise in nursing homes. An important question is how nursing competence can be utilised to improve patient safety in respect of medication.
Medication errors are among the most common adverse events in the health and care services. The need for greater efforts to ensure patient safety has been documented in national guidelines (1, 2, 3) and in the Official Norwegian Report 2015:11 (4). This highlights the considerable need to develop systems and cultures in order to learn from errors. Furthermore, managers must be more aware of risk and must ensure that internal controls are performed in fulfilment of the municipality’s duty to do so (5).
In 2011, the Ministry of Health and Care Services launched the national patient safety campaign ‘In Safe Hands 24/7’ as a national programme in which correct use of medication in nursing homes is one of the prioritised areas (2). This programme is carried forward in 2014–2018. The Coordination Reform entails that nursing homes have greater responsibility for treatment and not only responsibility for nursing and care. Care for patients in a nursing home is demanding and requires that the nurses have wide-ranging competence (6). Because nursing home residents use many medications at the same time, this increases the risk of interactions between drugs, side effects and incorrect medication (7).
The need to develop medication competence
In order to prevent medication errors, a variety of safety measures are often implemented, for example training, and control of the prepared drugs by two members of staff. Nevertheless, a report from the Norwegian Board of Health Supervision in 2010 reveals serious deficiencies in medication management in 51 out of 67 nursing homes that were investigated (8). Pressure of time, poor coordination between work tasks, staffing and competence as well as inadequate training are common, while following the introduction of the Coordination Reform, the complexity of nursing tasks has grown (9). Despite this, a survey showed that tasks such as cleaning and preparing food as well as poor ICT solutions stole time and attention from the care of patients (10).
The nurses state that they need better knowledge of pharmacology and age-related physiological changes (11). Alteren (12) found that student nurses lacked knowledge and experience of handling medication. Another study (13) showed that by assuming responsibility for a nursing home ward, third-year students gained experience of handling medication. Brenden et al. found that although the working environment in nursing homes provided a solid basis for learning, there was a lack of formal structures to enhance competence (14).
Need for better guidelines
International studies show that medication errors represent a considerable problem (15–18). However, we must question how effective current systems are in dealing with non-conformance, particularly in terms of whether error reporting systems and organisational measures promote learning and improvement (19). Research has revealed that there are conspicuous organisational barriers in the case of adverse events (16, 20). Interruptions when preparing medicines, a lack of knowledge and few opportunities to follow up the effects and side effects are factors that influence medication error (18, 20).
A survey of four American nursing homes on limiting medication error showed that the reporting systems were difficult to access. There was no information about medication error reporting forms and the follow-up of reported non-conformances was poor (21). Guidelines and standard procedures that could reduce incorrect use of medication often did not exist in nursing homes (22). An international study found that lack of time and training as well as a punitive culture were reasons for the failure of health personnel to report medication error. The study also showed that a culture of learning and fairness helped to increase reporting (17).
Patient safety in nursing homes
In order to analyse patient safety, we have employed Donabedian’s framework with its concepts of structure, process and result (23, 24). Procedures, guidelines and training are safety measures that are encompassed in the structural aspect of patient safety. According to Hjort (25), errors in the health service are mainly the result of systems errors such as time pressure, lack of guidelines, poor routines and the working environment. The systems approach entails analysing underlying causes and establishing systems that detect adverse events before they have serious consequences (26). Improvement based on learning from adverse events can be studied using Argyris and Schön’s concepts of single loop and double loop learning. While single loop learning involves adjusting behaviour within the same mind-set, double loop learning questions the basic perceptions underlying actions (27).
Good safety provided that the work on preparing medications is not interrupted.
Patient safety in terms of medication is an area that has not been adequately researched in Norwegian nursing homes. The purpose of this study is to shed light on how different safety measures function with regard to preventing medication errors. Safety measures are understood as interventions at the structural and processual level ensuring correct handling of medicines.
Method
The study has a qualitative design with focus group interviews as the main method of data collection. The focus group interview is a quick and non-resource-intensive method that can provide an insight into how nurses think and act to safeguard patient safety, and thus gives a deeper understanding of medication use in nursing homes. Using targeted group discussions, the participants can exchange perceptions and experiences (28). Individual learning logs are included as additional data. Learning logs are a tool used in programmes of professional study, and students use them to log their experiences of their clinical practice (29).
We started collecting data by means of focus group interviews with nurses in 2012, the same year as the Coordination Reform was initiated. With the implementation of the reform, students, teachers and the field of practice paid considerable attention to challenges associated with handling medication. This was particularly the case in a teaching project at Sør-Trøndelag University College, in which third-year students assumed responsibility for a nursing home ward in order to undergo training in professional management and the transition process from student to nurse (13). According to Morgan (28), there should be a sufficiently large number of focus groups to provide adequate data to shed light on the research question. We acquired data on the Coordination Reform’s impact on medication in nursing homes over time by including the students who assumed responsibility for the nursing home ward in the data collected. We conducted therefore two focus group interviews with students in 2013 and 2014 in addition to collecting the learning logs.
Sample
All informants received information in writing about voluntary participation, and we obtained written consent. The Norwegian Centre for Research Data approved the project. We obtained permission to conduct the study at two nursing homes. One was a large urban nursing home with over 100 places distributed among three large wards. The other was situated in a rural municipality and had approximately 60 places distributed among five small wards. The focus groups of nurses and a social educator were randomly made up of the staff on duty the day we carried out the interviews and who had the same formal competence in handling medication. We wanted to ensure that factors related to position levels did not affect the interaction (30).
Hereinafter, we will refer to the special educator as part of the group of nurses for reasons of anonymity. The seniority of the participants varied from 6 months to 24 years of practice. We carried out two focus group interviews at the large nursing home and one at the small nursing home, and two focus group interviews with students at the same nursing homes. The focus group material incorporates the experiences of 16 nurses and 13 student nurses. The learning logs also come from the same nursing homes in addition to a third nursing home that took part in the teaching project. Altogether 18 out of 69 learning logs included the handling of medication as a self-chosen topic.
Data collection
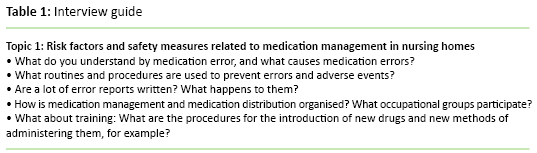
We compiled an interview guide using Donabedian’s triad as a theoretical framework, based on a previous hospital project (23, 31). The interview guide had three main themes:
- Risk factors and safety measures
- Cooperation with others
- Reactions to medication errors, risk perception and risk assessment
This article is limited to structural factors with special focus on safety measures (table 1). The article’s first and second authors conducted the interviews, which were recorded on tape and transcribed.
Data analysis
A previous data collection conducted at a hospital in connection with a related topic of research used the same methods and a similar interview guide, and resulted in relevant data generation. In the nursing home project, some of the discussions were limited and were more akin to a group interview (30). When we compared the data, the nursing home interviews provided considerable information about structural factors, but less information about relational conditions and culture. The content of the learning logs varied. Some gave detailed information about the handling of medication while others contained more superficial descriptions.
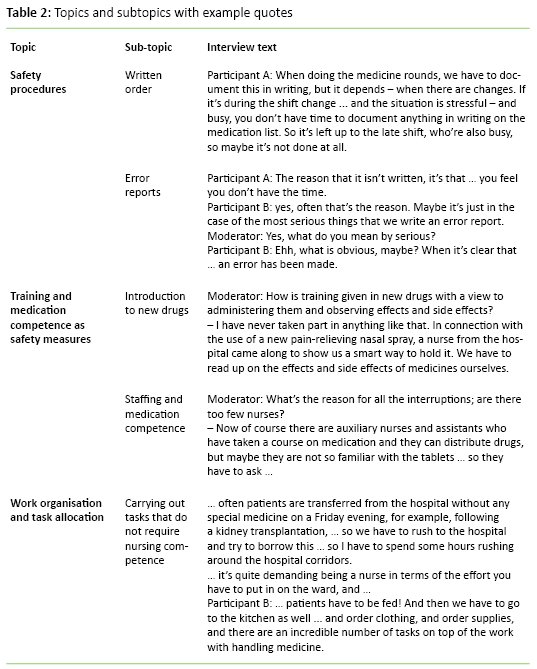
In five focus groups, the participants discussed the same topic guided by questions in a semi-structured interview guide. In the analysis of the discussion, key topics largely paralleled the topics in the interview guide. The first and second authors reviewed and discussed the interview texts before analysing them using Kvale’s method of coding and categorising meaning (32). By coding pieces of text, the general topics of discussion emerged. Categorisation took place by further condensing the data material through unifying several codes under one topic (see table 2). Those interviewed are regarded as informants or witnesses who provide reliable information (32). The learning logs are treated as individual interview data. They were coded and categorised in the same way as the focus group interviews, and supplemented the data material.
Ethical reflections and discussion of methods
We complied with the Helsinki Declaration’s guidelines on anonymity and confidentiality. Since information about medication error may be sensitive, it was vital to be aware of ethical aspects in connection with the project (32). When researching patient safety, a conflict of interests may arise. On the one hand, confidentiality must be safeguarded and a relationship of trust with the interviewees upheld. On the other hand, it is incumbent on us to warn of any risk to patient safety or treatment that is not professionally sound (32, 33). The interviews did not give rise to any such ethical dilemmas.
Several nursing homes in the region were asked to participate but only two of them found it possible to allow several nurses to leave the ward at the same time to participate in an interview. This restricted the breadth of the data. The students who took part assumed responsibility for a nursing home ward for two weeks. They had the same functional area as the nurses, apart from the handling of drugs, which was always checked by a nurse. The students had less experience than the nurses but their strength was their critical external gaze and their attention to theory. When we read through the body of material, it emerged that the nurses and students had similar experiences. For this reason, the data analysis does not distinguish between the nurses’ and the students’ experiences. Both groups are defined as health personnel, and in light of the principle of responsible conduct, prior learning and work experience is decisive for what tasks they can perform in connection with the handling of medication (33).
Results
Experiences of how safety measures functioned with regard to medication management in nursing homes were divided into three main topics (table 2):
- Safety procedures
- Training and medication competence as safety measures
- Organisation of work and allocation of tasks
Incomplete safety procedures
Verification by two members of staff was a well-established safety procedure. Two nurses checked the selection or preparation of medicines. If only one nurse was on duty, a practitioner (for example, a care worker or a nursing assistant) could help to check. The medicines were placed in a pill dispenser one week in advance, and were most often distributed by a nursing assistant. Two nurses mixed the drugs used in the infusion pump, but only one changed the pump. The informants said that after a near-accident, the staff had discussed whether there should also be two present when changing the pump.
At one of the nursing homes, there was a computer-controlled medicine cabinet with inbuilt control of the withdrawal and selection of medication. Secure practice relied on there being no interruptions to the work on preparing the medication. It was pointed out that the cabinet was too cramped, it was difficult to get a full overview and it quickly became very untidy.
Time pressure and interruptions characterised work on managing medication.
Written regulations on medication management were well implemented. However, according to the informants, there were many examples of non-compliance with the safety procedures. Due to time pressures, sometimes they skipped a step in the documentation routine. For example, they might forget to sign for the medicines administered, or they might sign for medicines that had not been handed out. A detailed example of a forgotten signing-off of a blood-thinning drug was described in a learning log. In the evenings or at the weekends, the dispensing of medicine often took place by telephone. Sometimes it took a long time to get the doctor’s signature, or it might be forgotten. A nurse also gave an example where a patient was given the wrong type of antibiotics because no information was noted about the patient’s allergy to this type of antibiotics.
A lack of case histories and non-conformance with procedures
The informants spoke of many episodes where case histories were lacking, or an outdated case history accompanied the patient when he/she was discharged from hospital. The last-mentioned incident was discovered when the nursing home ward received the new case history in the post some days later. If the nursing home asked the hospital about a missing case history, they might be told to use the list of medications, but as one nurse said, ‘That’s just a mess because it’s written by hand, so you don’t understand a thing.’ Such inaccuracies may result in deficient or incorrect treatment of patients. Nor did the nursing documentation and the case history always correspond. Considerable time was wasted in calling the hospital to try to obtain the case history or calling the doctor who had written it.
A topic addressed in several learning logs was non-conformance with procedures by failing to administer medicine at the correct time, or forgetting to do so at all. Nurses in several focus groups related that they were often too busy to write error reports. Time pressure and a shortage of nurses meant that they had to prioritise nursing tasks that involved giving immediate help. They also gave lower priority to writing error reports because they felt it was a waste of time. One nurse said ‘One summer I wrote all the error reports I possibly could (not only those related to medication) to map how much time I required to do this properly. Sometimes I was there one or two hours longer than the ordinary day shift on a completely voluntary basis and without being paid overtime for it.’
Another nurse claimed that only serious and obvious errors were documented. Even though it did not take long to describe the event, answering the point ‘Suggested improvements’ was time-consuming. The error reports were reviewed on a weekly basis in all nursing home wards but practice differed regarding feedback to the staff.
Training and medication competence as safety measures
The informants said that they were constantly being introduced to new drugs, generic drugs and new ways of administering them. Even experienced doctors expressed the view that there was a huge number of new things. Two manufacturers might produce the same drug but under different names. A less experienced nurse could easily select the wrong drug. Although the chemist published lists of all generic drugs, nurses did not always have time to consult the list. In answer to questions about training related to new drugs, new methods of administration and observation of the effects and side effects, one group answered as follows:
‘I have never taken part in anything like that (training in new medications).’
‘In connection with the use of a new pain-relieving nasal spray, a nurse from the hospital came along to show us a smart way to hold it. We have to read up on the effects and side effects of medicines ourselves.’ Several of the others nodded in agreement, saying things like:
‘… and we learn from each other…’
‘… so we read the package information leaflet …’
‘We have a duty to keep updated at all times.’
The informants stated that training in medication management was ‘ad hoc’ and poorly organised. The training consisted of information sheets, package information leaflets, the app of the Norwegian Pharmaceutical Products Compendium on private mobile phones, self-study and exchange of experience. No one had been offered any training by the pharmaceutical companies.
Work organisation and allocation of tasks
The organisation of work and allocation of tasks among health personnel in connection with handling medication was part of the safety measures. Patients were prescribed medication by various actors such as their GP, the nursing home physician and doctors from various hospital departments. At the nursing homes, there were doctor’s visits once a week (twice a week in some short stay wards) with a routine review of medicines. At one of the nursing homes, the doctors had a strong focus on unnecessary medication.
At the other nursing home, in contrast, both the nurses and the doctors paid less attention to polypharmacy. A group of student nurses discussed how easy it was to resort to laxatives and tranquillisers to save time instead of focusing on diet and activity. One student nurse wrote a detailed learning log about a patient who appeared to be considerably overmedicated with analgesics and psycho-pharmaceuticals. The patient was very overweight, and the side effects of several of the medications included drowsiness, an increased need for sleep and weight increase. The patient was hospitalised for reasons of mobilisation, but sat in the lounge and slept the whole day. The student attempted several times to take this up during the pre-visit consultation, but to no avail since it was said to be non-acute. Two more learning logs also dealt with patients who were overmedicated.
There was a lack of systematic competence building.
In the short stay wards, the patients on occasion administered their medicines themselves, often without having the necessary overview. One nurse said ‘They come along with a whole box filled with medicines that they’ve collected and saved up for several years. They ask if they have to use it, because no one has told them to stop.’ If attempts were made to gradually reduce their medication, family members might protest because they wanted active treatment for their loved ones. One of the nursing homes arranged scheduled meetings with family members twice a year, opening for a discussion of medication regimes.
In all nursing home wards, nurses usually prepared the medication, but they were often administered by a nursing assistant who had undergone a six to twelve-hour course of internal training. Each shift had few nurses on duty. Several of the interviews and learning logs provided examples showing that considerable time was spent on tidying, washing and serving food – tasks that do not require nursing competence. Many simultaneous, complicated nursing tasks gave the nurses little opportunity to work in a concentrated manner without interruption. At one of the nursing homes, medication selection was allocated to different days of the week in order to shield the nurses who handled medication.
Discussion
This study has revealed that documentation as a safety procedure was a risk factor because it was unreliable. Weaknesses in patient record systems have previously been documented at 56 Norwegian nursing homes (8). Another study shows that errors in medication information was one of the most common adverse events when patients are transferred between different levels of the health service (34). Nor do error reports function satisfactorily as safety measures. The nursing homes employ error reports, double-checking and documentation when there is enough time, but the participants described many situations when time pressure made it impossible to follow safety procedures. This finding concurs with international research (17, 21, 22) and shows that there is a long way to go to fulfil the principles of double loop learning (27). This study is also in line with Lipsky (35), who as early as 1980 described how ‘street-level bureaucrats’ were forced ‘to take short cuts’ in situations with difficult priorities.
Descriptions of inaccurate documentation and a lack of error reports recurred during the data collection period of almost three years. This indicates a failure to improve safety measures, which in turn indicates poor follow-up of internal control (5). The responsible manager has the formal responsibility for medication management and risk assessment (36). A 2015 survey also described time pressure as the reason that the writing of error reports was not given priority, and that error reporting systems seldom resulted in improvements (37). This is a grave situation since the Coordination Reform entails greater and more complex medication being administered by the primary health service (3, 9).
If safety procedures that cannot be realised in practice are retained, this can undermine staff’s understanding of the importance of routines for patient safety. Exact documentation of prescribed drugs is essential to prevent medication errors. Since substantial resources are used both for documentation and error reports, we need further research to evaluate the use of resources in order to improve patient safety in the nursing home.
Must build up competence systematically
Our study showed that time pressure and interruptions characterised work on medication management, while at the same time considerable time was spent on tasks that did not require nursing skills. Other surveys and studies also point this out (10, 18, 38), which can be interpreted as indicating that training and the development of medication competence is not being taken sufficiently seriously. Brenden et al. showed that updating knowledge in nursing homes was carried out informally with a lack of formal management strategies to map competence and competence enhancement (14). This finding confirms that there is a lack of systematic competence building. The attending doctor is responsible for medication management but is reliant on nurses’ reports on observations of the effects and side effects. Such reports require that the nurses have time to write them and professional knowledge (7).
The study presents examples in which student nurses point to procedural errors and overmedication. This indicates that the nurses have competence that can be exploited in improving the medication regime in nursing homes, so that competence building can be in line with the principles of double loop learning (27). Further research is necessary to examine why nurses give less priority to safety measures that can improve patient safety, and instead are carrying out tasks with considerably lower risk and need for competence such as serving food, tidying and cleaning.
Professional identity must be enhanced and the nurse’s role shielded from tasks that do not require nursing skills.
The Coordination Reform entails that the municipality has a much greater degree of responsibility for treatment and no longer merely has responsibility for nursing and care. This change increases the need to build up medication competence systematically. When new health reforms are introduced, there is little assessment of what the consequence will be for patient safety (39). Our study indicated that an overly high risk is associated with medication management in nursing homes. Nurses are present twenty-four hours a day in nursing home wards and represent a professional group with formal medication competence.
This study has shed light on the great need that nurses and student nurses have for medication competence, but implies that there must be realistic framework conditions to apply and develop such competence. In addition, the study shows that patients possibly need training. A high rate of polypharmacy has been revealed as being an underlying cause of falls in connection with patients hospitalised in the specialist health service (40). If patients and their family members have better information and knowledge about drugs, this can reduce unnecessary medication use.
Implications for education and practice
The education of nurses must emphasise organisational competence in order to increase understanding of the correlation between safety measures and patient safety (24–26, 41). Professional identity must be boosted, and the role of the nurse shielded from tasks that do not require nursing competence (6). Internal control in nursing homes must be improved. Nursing home management must pay more attention to risk in connection with medication use and make provision for systematic training and development of medication competence, which must take place in relation to double loop learning, including reflection and time to assess underlying causes (27). Management must also facilitate training for patients and family members.
The survey is based on experiences from a limited number of nursing home wards, and must be interpreted with care to avoid generalisation. However, the results correlate well with Norwegian and international studies on patient safety, medication use and competence needs in nursing homes (6, 8, 11, 15, 16, 18, 20–22).
Conclusion
The results of this study describe safety procedures that are not always feasible or reliable in practice. The training was deficient and there was poor correlation between medication competence, work tasks and staffing.
The Coordination Reform has resulted in greater and more complex medication use in nursing homes, increasing the need for a systematic enhancement of medication competence. The results of this study concur with several similar studies and therefore raise the question of why nursing competence is not better utilised to ensure patient safety. Considerable resources are used on structural measures such as documentation and error reports without this having the optimal impact. Further research should be carried out on how increased nursing staff levels and the development of medication competence can improve patient safety in nursing homes.
References
1. Meld. St. 10. God kvalitet – trygge tjenester. Kvalitet og pasientsikkerhet i helse- og omsorgstjenesten. Oslo: Helse- og omsorgsdepartementet. 2013.
2. Meld. St. 11. Kvalitet og pasientsikkerhet 2013. Oslo: Helse- og omsorgsdepartementet. 2014–2015.
3. Meld. St. 26. Fremtidens primærhelsetjeneste – nærhet og helhet. Oslo: Helse- og omsorgsdepartementet. 2014–2015.
4. NOU 2015:11. Med åpne kort. Forebygging og oppfølging av alvorlige hendelser i helse- og omsorgstjenesten. Oslo: Helse- og omsorgsdepartementet. 2015.
5. Helse- og omsorgsdepartementet. Forskrift om internkontroll i helse- og omsorgstjenesten. 1. januar 2003 (Internkontrollforskriften). Available at: https://lovdata.no/dokument/SF/forskrift/2002-12-20-1731 (Downloaded 23.10.15).
6. Bing-Jonsson PC, Bjørk IT, Hofoss D, Kirkevoll M, Foss C. Competence in advanced older people nursing: development of «Nursing older people – competence evaluation tool». International Journal of Older People Nursing 2015; 10:59–72.
7. Kirkevold M, Brodtkorb K, Ranhoff AH. Geriatrisk sykepleie. God omsorg til den gamle pasienten. 2 utgave. Oslo: Gyldendal Akademisk. 2014.
8. Helsetilsynet. Sårbare pasienter – utrygg tilrettelegging. Funn ved tilsyn med legemiddelbehandling i sjukeheimar 2008–2010. Report from Helsetilsynet 7/2010. Oslo: Helsetilsynet. 2010.
9. Gautun H, Syse A. Samhandlingsreformen. Nova-report no. 8/2013. Oslo: Norsk Institutt for forskning, oppvekst, velferd og aldring. 2013.
10. Hofstad E. Sluttet i protest. Tidstyvene gjorde at jeg sa opp på sykehjemmet. Oslo: Sykepleien 2014;12:24–31. Available at: https://sykepleien.no/reportasje/2014/10/sluttet-i-protest(Downloaded 17.11.2016).
11. Wannebo W, Sagmo L. Stort behov for mer kunnskap om legemidler blant sykepleiere i sykehjem. Sykepleien Forskning 2013;8(1):26–34. Available at: https://sykepleien.no/forskning/2013/01/stort-behov-mer-kunnskap-om-legemidler-blant-sykepleiere-i-sykehjem(Downloaded 17.11.2016).
12. Alteren J. Å lære legemiddelhåndtering i sykehjem. Sykepleiestudentenes utfordringer. Vård i Norden 2012;32(4):34–8.
13. Blekken L, Medby AO, Forbord T. Læringsutbytte i sykepleiefaglig ledelse etter praksis der sykepleierstudenter overtok ansvaret for en avdeling. Sykepleien Forskning 2013;4(8):344–52. Available at: https://sykepleien.no/forskning/2013/11/laeringsutbytte-i-sykepleiefaglig-ledelse-etter-praksis-der-sykepleierstudenter(Downloaded 17.11.2016).
14. Brenden TK, Storhei AJ, Grov EK, Ytrehus S. Kompetanseutvikling i sykehjem – ansattes perspektiv. Nordisk Tidsskrift for Helseforskning 2011;7(1):61–75.
15. Lane SJ, Trover JL, Dienemann JA, Laditka SB, Blanchette CM. Effects of skilled nursing facility structure and process factors on medical errors during nursing home admission. Health Care Management Review 2014; 39(4):340–51.
16. Lim RHM, Anderson JE, Buckle PW. Work domain analysis for understanding medication safety in care homes in England: an exploratory study. Ergonomics 2016; 59(1):15–26.
17. Holmstrom A, Airaksinen M, Weiss M, Wuliji T, Chan X, Laaksonen R. National and local medication error reporting systems. A survey of practices in 16 countries. Journal of Patient Safety 2012; 8(4):165–76.
18. Dilles T, Elseviers MM, van Rompaey B, van Bortel LM, Vander Stichele RR. Barriers for nurses to safe medication management in nursing homes. Health Policy and Systems. 2011; 43(2):165–76.
19. Stavropoulou C, Doherty C, Tosey P. How effective are incident-reporting systems for improving patient safety? A systematic literature review. The Milbank Quarterly 2015; 93(4):826–66.
20. Barber ND, Alldred DP, Raynor DK, Dickinson R, Garfield S et al. Care homes’ use of medicines study: Prevalence, causes and potential harm of medication errors in care homes for older people. Quality and Safety in Health Care 2009;18:341–6.
21. Handler SM, Perera S, Olshansky EF, Studenski SA, Nace DA, Fridsma DB, Hanlon JT. Identifying modifiable barriers to medication error reporting in the nursing home setting. Journal of the American Medical Directors Association 2007;8(9):568–74.
22. Barnes L, Cheek J, Nation RL, Gilbert A, Paradiso L, Ballantyne A. Making sure the residents get their tablets: medication administration in care administration in care homes for older people. Journal of Advanced Nursing 2006;56(2):190–9.
23. Donabedian A. The definition of quality and approaches to its assessment. Michigan: Health Administration Press. 1980.
24. Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, Hundt AS, Hoonakker P, Holden R, Ayse PG. Human factors system approach to healthcare quality and patient safety. Applied Ergonomics 2014;45:14–25.
25. Hjort PF. Uheldige hendelser i helsetjenesten. Oslo: Sosial- og helsedirektoratet. 2004.
26. Aase K. Pasientsikkerhet. Teori og praksis. 2. ed. Oslo: Universitetsforlaget. 2015.
27. Argyris C, Schön, D. Organizational learning II. Michigan: Addison-Wesley Publishing Company. 1996.
28. Morgan DL. Focus groups as qualitative research. 2. ed. California: Thousand Oaks Sage Publications. 1997.
29. Klemp T. Med praksisloggen som vandrestav. En kvalitativ studie av lærerstudenters læringsprosess. (Doctoral dissertation). Trondheim: NTNU. 2012.
30. Halkier B. Fokusgrupper. Oslo: Gyldendal Norsk Forlag. 2010
31. Storli M. Feilmedisinering i sykehus – organisasjonskulturens påvirkning. Vård i Norden 2008;3(28):19–23.
32. Kvale S. Det kvalitative forskningsintervju. Oslo: Ad Notam Gyldendal. 1997.
33. Molven O. Sykepleie og jus, 4. ed. Oslo: Gyldendal. 2012
34. Mesteig M, Hellebostad J, Sletvold O, Rosstad T, Saltvedt I. Unwanted incidents during transition of geriatric patients from hospital to home: a prospective observational study. BMC Health Services Research 2010;10:1.
35. Lipsky M. Street-level bureaucracy. Dilemmas of the individual in public service. New York: Russel Sage Foundation. 1980.
36. Helsedirektoratet. Legemiddelhåndtering for virksomheter og helsepersonell som yter helsehjelp. Oslo: Helsedirektoratet. 2008.
37. Flatgård I. Avvik stoppes og avvises. «Det er bukken som passer havresekken». Oslo, Sykepleien 2015;3:32–8.
38. Allen D. Re-reading nursing and re-writing practice: towards an empirically based reformulation of the nursing mandate. Nursing Inquiry 2004;11(4):271–83.
39. Aase K. Pasientsikkerhet. Teori og praksis i helsevesenet. Oslo: Universitetsforlaget: 2010.
40. Fylkesmannen i Møre og Romsdal, Nord-Trøndelag, Sør-Trøndelag. Fallprosjekt i Helseregion Midt-Norge, Samlerapport etter Pilotstudien 2010, Journalstudien 2011, Kommunestudien 2012.
41. Orvik A. Organisatorisk kompetanse. Innføring i profesjonskunnskap og klinisk ledelse. Oslo: Cappelen Damm Akademisk. 2015.










Comments