From hospitals to nursing homes – the consequences of the Care Coordination Reform
Following the Care Coordination Reform, more frail elderly patients have died after discharge from hospitals to nursing homes and more have been discharged to return home.
Background: The coordination reform was introduced in January 2012 to ensure sustainability of health and care services. The transfer of responsibility for treatment from the specialist to the primary health service formed a central pillar of the reform. This study compares the situation before and after the introduction of the coordination reform for frail elderly patients being transferred from hospitals to nursing homes, related to: 1) deaths, and 2) age, sex, days of hospitalization and discharge destination.
Objective: Investigate possible differences in the population of patients transferred from hospitals to nursing homes before and after the introduction of the Care Coordination Reform.
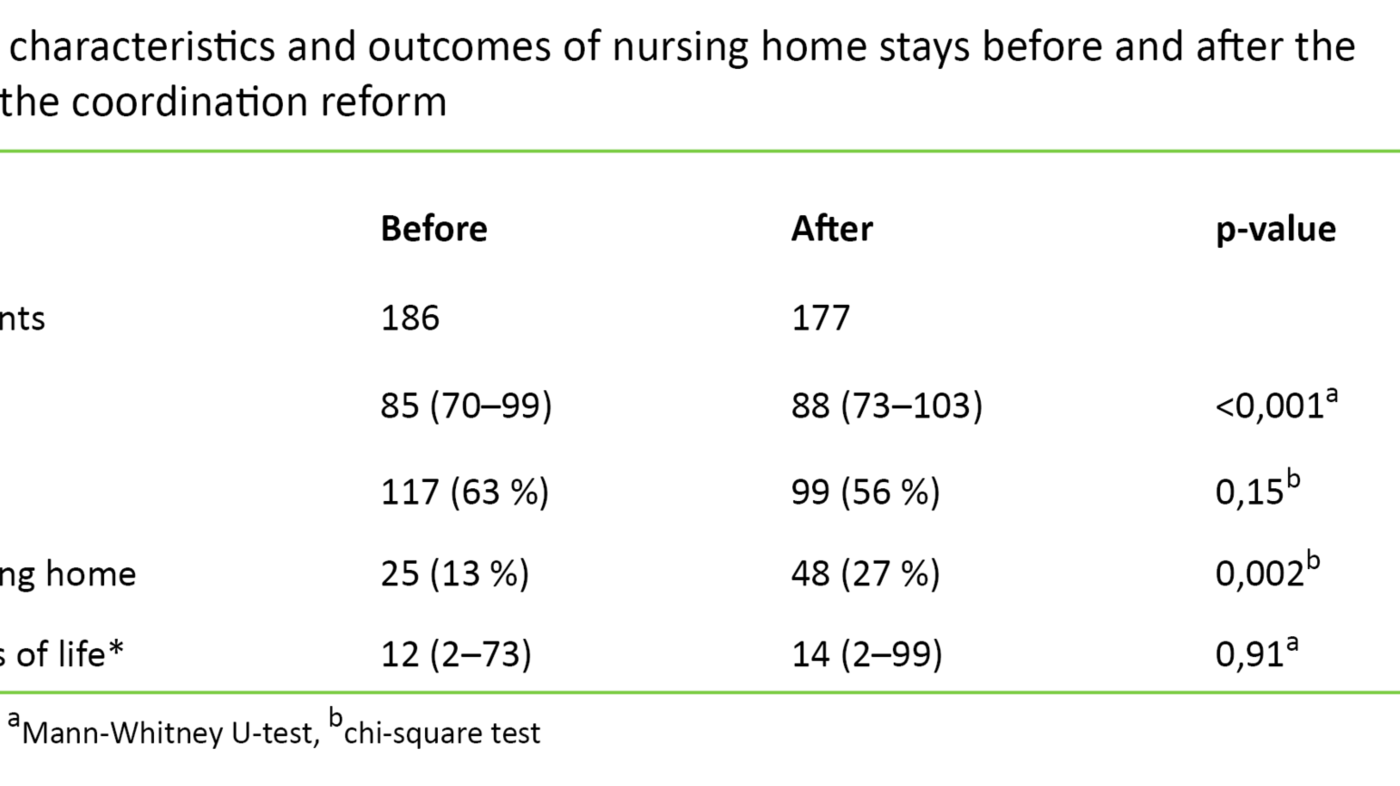
Method: The data were retrieved from a 35-bed short-term ward at one nursing home, where the procedures and staffing were unchanged in the period before and after the reform. Information on the patients' age, sex, days in the nursing home, discharge destination and death in the nursing home was retrospectively collected for 186 patients aged ≥ 70 years for the period before the introduction of the coordination reform, and for 177 patients after the introduction of the coordination reform.
Results: We found that the number of patients who died in the nursing home after hospitalization doubled (27% versus 13%, p <0.002) following the introduction of the coordination reform. Compared with the situation before the reform, patients admitted after the reform were older (median 88 years (range 73–103) versus 85 years (range 70–99), p <0.001). Fewer patients were transferred to a different nursing home (21% versus 45%, p < 0.001), and more were discharged to their own home (47% versus 36%, p = 0.04).
Conclusion: Our results show that patients transferred from hospitals to nursing homes after the introduction of the coordination reform were older. Moreover, more patients died during short-term stays in nursing homes after being transferred from hospitals. There is reason to assume that these results have consequences for the needs for competence and staffing in nursing homes.
To better meet the health challenges of the future, many industrialised countries have implemented health reforms during the last decade (1). The challenges have been described as including insufficient coordination of the health services, little focus on prevention and an expected growth in the number of elderly people with chronic illness and need for assistance (1). This is reflected in the Care Coordination Reform, which was introduced in Norway in 2012, with the goal of improving public health and sustainably improving the health and care services (2).
In line with the health reforms in the Nordic countries, the Norwegian coordination reform has been concerned with relocating the responsibility for treatment to places closer to the patient’s home (1). This implies that a larger proportion of the health services will be transferred to municipal health providers, thus to slow down the growth in the use of hospital services. According to Grimsmo and Magnussen (1), the Norwegian coordination reform is distinctive in having been implemented in the specialist and primary health services separately.
One of the instruments in the Norwegian coordination reform has been to establish collaboration agreements between the municipalities and the health enterprises. According to the evaluation of the coordination reform undertaken by the Research Council of Norway (3), the reform has had a limited impact on the way in which the municipal health services perceive this collaboration. The collaboration is described as asymmetrical, since the hospital doctors are authorised to decide when a patient is ready for discharge without having to involve the medical competence in the municipality to any appreciable extent in this decision (3).
Shorter hospitalisation periods after the reform
The fee paid by the municipalities for patients who are deemed to be ready for discharge from hospital is a further key instrument in the Norwegian reform. During the first year after the reform, some hospitals reported a reduction of up to 96 per cent in the number of excess hospitalisation days of patients who were ready for discharge (4). According to the investigation made by the Office of the Auditor General of resource utilisation and quality in the health services after the introduction of the coordination reform (5), more than 80 per cent of the patients who were registered as ready for discharge nationwide in 2014 were received by the municipality on the day when the discharge was announced. Hospitalisation times for the oldest patients have also been reduced.
At the geriatric emergency department of Diakonhjemmet Hospital, the reduction in hospitalisation time after the introduction of the coordination reform was associated with an increase in readmissions in the same period (7). According to the evaluation report for the coordination reform, this is not linked to an increase in readmissions, but an increase in admissions during the same period in which a reduction in hospitalisation periods had been observed (3). Coordination statistics from the Directorate of Health confirm that there is a correlation between shorter hospitalisation periods and readmissions (8). There is a greater risk of readmission among patients who are transferred to the municipality on the same day that the discharge is notified, when compared to patients who remain in hospital beyond this time (8). A large-scale Swedish study found a correlation between shorter hospitalisation periods and reduced survival after discharge among elderly patients with femoral neck fractures (9).
Flaws in patient transfer
Because of the shorter hospitalisation periods for the oldest patients, we can see an increase in the number of patients being transferred to nursing homes (8). This increase has not resulted in a significant increase in nursing home beds (5). However, more widespread use of double rooms and corridor patients has been registered (10), as well as an increase in short-term stays at the cost of permanent places in nursing homes (11). The transfer of responsibility for treatment from the hospitals to the municipalities entails that the patients being transferred suffer from more serious, complex and treatment-intensive conditions, when compared to the situation before the introduction of the coordination reform (10, 11). Thus, the nursing homes have been charged with more specialised care and treatment, with a concurrent need for more competence. However, the municipalities have not upgraded their competencies to any great extent since the introduction of the coordination reform (5). The nursing homes report having unfulfilled needs for competence and increased time constraints after the coordination reform (9).
When seriously ill patients needing treatment are to be transferred to health services at another level, collaboration between the service levels is essential. Measures including collaboration agreements between the municipalities and the health enterprises have been introduced to reinforce the coordination between the service levels. The municipalities nevertheless report that the collaboration associated with transfer of patients has been weakened since the introduction of the reform (10). This was confirmed by a nationwide inspection, which identified deficiencies in the flow of information when patients were transferred between hospitals and municipalities (5).
We wished to obtain more knowledge about the consequences of the coordination reform for frail elderly patients who are transferred from hospitals to nursing homes. We therefore compared the incidence of deaths, age, sex, hospitalisation days and discharge destination before and after the reform.
Material and method
We undertook a retrospective study in one of the nursing homes in Bergen municipality by retrieving data for the periods from May 2009 to December 2011 and March 2012 to May 2014, i.e. before and after the introduction of the coordination reform respectively (2). The study was undertaken in a 35-bed short-term ward. This ward received patients who could not be discharged to their own homes after emergency hospitalisation. The objectives of their stay in the ward were:
- to complete medical treatment and care that had been initiated in the hospital, and
- to identify care needs and the possibilities for transfer to their own homes.
Through this period (2009–2014), the ward has followed the same procedures, with unchanged staffing. When our study was initiated in 2013, all the patients included had either been discharged from the nursing home or were deceased.
Patients
We included all patients ≥ 70 years who were transferred from Haukeland University Hospital or Haraldsplass Diaconal Hospital to the short-term ward at the nursing home during the period in question. We collected patient characteristics, such as age, sex, hospitalisation days, discharge destination and death, from the municipal patient administration system.
Statistics
We analysed the data with the aid of descriptive statistics. The data were not normally distributed, and we used the Mann-Whitney U-test to compare continuous data and the chi-square test to compare categorical data between two groups. The data were analysed with the aid of the statistics package SPSS, version 20 for Windows.
Ethics
The study was approved by the Regional Committee for Medical and Health Research Ethics (REK Western Norway), which also granted exemption from the requirement for patient consent.
Results
We included a total of 363 patients with a median age of 86 years (range: 70 to 103 years), whereof 59 per cent were women. The patients who were admitted after the introduction of the coordination reform were significantly older (p < 0.001), and more than twice as many died in the nursing home (p = 0.002) (Table 1).
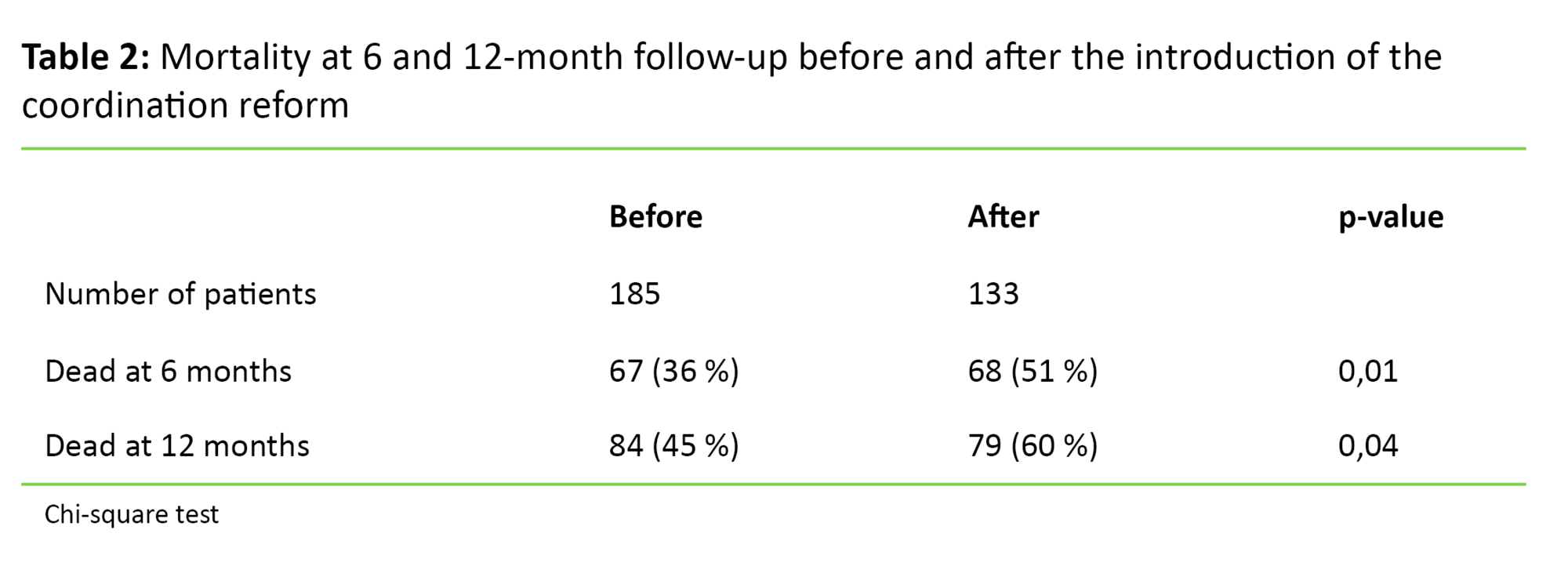
Mortality increased after the introduction of the coordination reform, at six as well as twelve months (p = 0.04 and p = 0.01 respectively) (Table 2).
Fewer patients were transferred to a long-term place in another nursing home (p = 0.001), while a higher proportion of patients were discharged to their homes (p = 0.04). There was no significant difference (p = 0.91) in the number of days the patients remained alive prior to and after the coordination reform (Table 1).
Discussion
This study shows that patients who were transferred from a hospital to a nursing home after the introduction of the coordination reform were older than those transferred before the reform. In addition, a larger proportion of the patients died in the nursing home (Tables 1 and 2). As far as we are aware, this study is the first to have retrieved information on age and death in this patient population.
Unfortunately, we have no variables that may explain the increased mortality that we have found. Despite an increase in survival in hospitals from 2010 to 2014 (12), we have limited information on the correlation between changes in the frequencies of deaths in hospitals and nursing homes. The most likely explanation, which has also been emphasised in previous studies (10, 11), is that the patients who were transferred to nursing homes after the coordination reform suffered from more serious, complex and treatment-intensive conditions than those who were admitted before the reform. Moreover, the patients admitted after the reform were older. The number of diagnoses has been shown to contribute to increased mortality among residents in nursing homes (13, 14).
Weakening of service levels
We found that the number of patients who died in nursing homes doubled after the introduction of the coordination reform (from 13 per cent to 27 per cent; p = 0.002). Nursing, care and treatment of extremely ill and dying patients are especially challenging, in terms of both competence and resources. According to the National Action Plan’s guidelines for palliative cancer care (15), the palliative pathway is characterised by a complex clinical picture with acute conditions such as complications and organ failure, and an increasing need for care. Those who follow up this patient group emphasise close follow-up with appropriate information to the patients and their next of kin (15). Studies show that sufficient time and competence with regard to palliative care as well as communication with the patients and their next of kin are essential for the provision of good end-of-life care (16–19).
To provide seriously ill and terminal patients with appropriate follow-up and care, planning of the transfer of treatment responsibility to another service level is essential. It is therefore a source of concern when nurses in the municipal health services report that the collaboration between the service levels has weakened when it comes to discharge planning in the specialist health services since the introduction of the coordination reform (10). Moreover, it is problematic that medical competence in the municipality is rarely involved in assessments and decisions regarding the transfer of treatment responsibility from the specialist health services.
Weaknesses of the study
One weakness of our study is that we have no data regarding any possible differences in terminal care between nursing homes and hospitals. Nor do we have any data on how the patients or their next of kin perceive the transfer to a nursing home at this stage of life. We are therefore unable to draw any conclusions as to where terminal care can best be provided to this group of patients. When departing from life or losing someone close, security, predictability and a perception of support and competence are essential factors. Whether this can be best ensured close to the patient’s home or where the specialist competence is highest, depends on several factors that are not elucidated in this study. Further research should focus on the treatment needs of patients admitted to nursing homes since the coordination reform. There is a need for knowledge on how patients and their next of kin perceive a transfer from a hospital to a nursing home at this stage of life. User experience is a key element in optimising service provision.
Our results are generated by a small retrospective study undertaken in a single nursing home, and we have no information on morbidity. This is a weakness of this study. It would consequently be interesting to compare our figures with equivalent figures from other short-term wards from the same period and area. No such figures are available, however.
A less favourable situation for the elderly and frail
The results show that fewer patients were transferred to long-term places in other nursing homes, and that a higher proportion of the patients were discharged to their homes (Table 3). Other studies also conclude that a higher number of frail, elderly people are discharged from hospitals to nursing homes. This transfer entails an increase in short-term and rehabilitation places at the cost of permanent places in nursing homes (10).
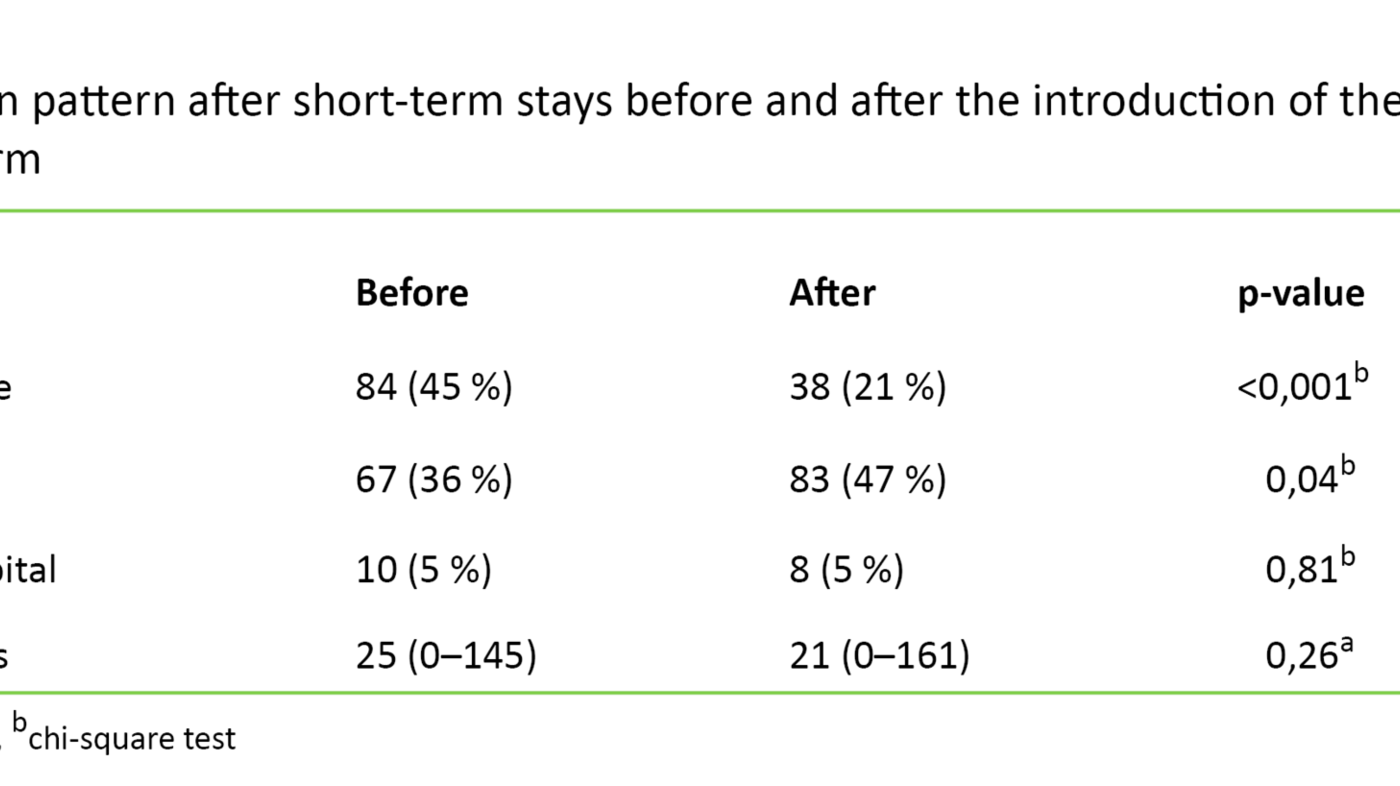
There is reason to assume that frail elderly patients who are discharged from nursing homes to their own homes constitute a group with a high risk of multiple readmissions. Our argument for this assertion is a general increase in readmissions after the introduction of the coordination reform (8), specifically in the patient population in acute geriatrics (7). Since the coordination reform, there has been a small increase in the number of readmissions from nursing homes to hospitals.
It remains to be seen what role the establishment of municipal emergency day-care units (KAD units) may have for this patient population. The scheme was introduced in the period from 2012 to 2016. Bergen municipality established the scheme in 2016, after the completion of our study. So far, there are indications that very few patients are admitted from nursing homes, while close to 18 per cent of the patients who pass through these units are transferred to nursing homes within a few days (21).
Conclusion
Our results show that patients who have been transferred from hospitals to nursing homes since the coordination reform tend to be older and have shorter survival when compared to the situation before the introduction of the reform. The nursing homes may thus face a higher throughput of patients as well as challenges related to less clarified patient issues when it comes to active treatment versus terminal care.
There is reason to assume that these factors entail consequences for the competence and staffing needs in nursing homes in order to achieve the coordination reform’s objective of sustainably improving public health and the health and care services. To cope with the new situation after the introduction of the coordination reform, the staffing in nursing homes ought to be reviewed in light of their tasks and competence needs. Further research should focus on the treatment needs of patients who have been admitted to nursing homes after the coordination reform.
References
1. Grimsmo A, Magnussen J. Norsk samhandlingsreform i et internasjonalt perspektiv. 2015.
2. Helse- og omsorgsdepartementet. Samhandlingsreformen: Rett behandling – på rett sted – til rett tid. Oslo. 2009.
3. Norges forskningsråd. Evaluering av samhandlingsreformen. Sluttrapport fra styringsgruppen for forskningsbasert følgeevaluering av samhandlingsreformen (EVASAM). 2016.
4. Otterstad HK, Birkestrand T. Samhandlingsreformen. Færre overliggere i sykehus. Sykepleien 2014;102(2):49–51. Available at: https://sykepleien.no/forskning/2014/02/faerre-overliggere-i-sykehus. (Downloaded 06.02.2017).
5. Riksrevisjonen. Riksrevisjonens undersøkelse av ressursutnyttelse og kvalitet i helsetjenesten etter innføringen av samhandlingsreformen. Dokument 3:5 (2015–2016). Oslo: Helse- og omsorgsdepartementet. 2016.
6. Hermansen Å, Grødem AS. Reformeffekt: Redusert liggetid blant de eldste. Sykepleien Forskning 2015;10(1):24–32. Available at: https://sykepleien.no/forskning/2015/02/redusert-liggetid-blant-de-eldste. (Downloaded 06.02.2017).
7. Ranhoff A, Alaburic S, Engstad T, Mensen L, Svendsen T. Readmissions after discharge from an acute geriatric unit; an analysis of probable causes. European Geriatric Medicine (EUGMS) September 2014; Rotterdam, Nederland, 2014. p. S207 – S8. Available at: http://www.em-consulte.com/en/article/927637. (Downloaded 12.02.2017).
8. Helsedirektoratet. Samhandlingsstatistikk 2013–14. Oslo. 2015.
9. Nordström P, Gustafson Y, Michaëlsson K, Nordström A. Length of hospital stay after hipp fracture and short term risk of death after discharge: a total cohort study in Sweden. BMJ 2015.
10. Gautun H, Syse A. Samhandlingsreformen. Hvordan tar de kommunale helse -og omsorgstjenestene i mot det økte antallet pasienter som skrives ut fra sykehusene? NOVA. 2013.
11. Abelsen B, Gaski M, Nødland SI, Stephansen A. Samhandlingsreformens konsekvenser for det kommunale pleie- og omsorgstilbudet. International Research Institute of Stavanger. 2014. Available at: http://www.ks.no/globalassets/vedlegg-til-hvert-fagomrader/helse-og-velferd/samhandlingsreformen/forskning-og-evaluering/iris-2014-382-samhandlingsreformens-konsekvenser.pdf. (Downloaded 12.02.2017).
12. Lindman AS, Kristoffersen DT, Hansen TM, Tomic O, Helgeland J. Kvalitetsindikatoren 30-dagers overlevelse etter innleggelse i norske sykehus – resultater for året 2014. Oslo: Kunnskapssenteret for helsetjenesten i Folkehelseinstituttet. 2015.
13. Drageset J, Eide GE, Ranhoff AH. Mortality in nursing home residents without cognitive impairment and its relation to self-reported health-related quality of life, sociodemographic factors, illness variables and cancer diagnosis: a 5-year follow-up study. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. 2012.
14. Barca ML, Engedal K, Laks J, Selbaek G. A 12 months follow-up study of depression among nursing-home patients in Norway. Journal of Affective Disorders 2010;120(1–3):141–8.
15. Helsedirektoratet. Nasjonalt handlingsprogram med retningslinjer for palliasjon i kreftomsorgen. Oslo. 2010.
16. Dreyer A, Forde R, Nortvedt P. Autonomy at the end of life: life-prolonging treatment in nursing homes—relatives’ role in the decision-making process. Journal of Medical Ethics 2009;35(11):672–7.
17. Davies E, Higginson I. Better palliative care for older people. WHO. 2004.
18. Wille I-L, Nyrønning S. Omsorg og behandling ved livets slutt i sykehjem. Geriatrisk Sykepleie 2012;3.
19. Husebø B, Husebø S. Sykehjemmene som arena for terminal omsorg – hvordan gjør vi det i praksis? Tidsskr Nor Lægeforen 2005;125(1352):4.
20. Lovdata. Lov om kommunale helse- og omsorgstjenester m.m. 24.06.2011 [helse- og omsorgstjenesteloven]. Available at: https://lovdata.no/dokument/NL/lov/2011-06-24-30. (Downloaded 06.02.2017).
21. Skinner MS. Øyeblikkelig hjelp døgnopphold. Oppsummering av kunnskap og erfaringer fra de første fire årene med kommunalt øyeblikkelig hjelp døgnopphold. Rapportserie nr. 13. Gjøvik: Senter for Omsorgsforskning. 2015. Available at: https://brage.bibsys.no/xmlui/bitstream/id/398536/rapport_13_2015_web.pdf. (Downloaded 06.02.2017).










Comments