Translation and cultural adaptation of the Attentional Function Index (AFI)
Involving a user and a professional translator may be appropriate when an instrument is translated and adapted to another culture.
Background: The incidence of cancer among older adults is rapidly increasing, and as a result of treatment cancer patients may be subject to cognitive changes. Many cancer survivors experience reduced attention and concentration, as well as poorer memory. The Attentional Function Index (AFI) is an instrument developed in the USA to assess cognitive processes.
Purpose: To describe the translation and pilot testing of the Norwegian version of AFI.
Method: Three researchers with knowledge of psychology, nursing and cancer, one psychologist with specialist knowledge of cognitive instruments, and a user representative, constituted the expert group in translation and cultural adaptation of the instrument. An accredited translator participated actively in the work. In the pilot testing of the Norwegian version persons ³ 60 years were recruited using “snowball sampling”. A total of 114 persons between 60–90 years were recruited for the testing, and twelve of these were specifically asked to comment on the instrument.
Results: The expert group members provided feedback based on their competence. The user representative wanted a simple and understandable, non-offensive language, and the translator provided linguistic comments. Fifteen persons commented particularly on question 11 “Keeping yourself from saying or doing things you did not want to say or do”.
Conclusion: The inclusion of users and a translator in the translation process can improve the validation. We recommend that the process be made available for future users of translated instruments.
Cancer incidence is rapidly increasing, and it is assumed that approximately 40 000 people will be affected by cancer by 2030. Two-thirds of these will be older than 60 years (1). Elderly patients may be at an elevated risk of changes to their cognitive function when undergoing treatment for cancer (2).
Changes in cognitive function have been shown to constitute a significant problem for many cancer survivors (3). Cognitive changes after cancer treatment manifest themselves as reduced attention, reduced concentration and poorer short-term and long-term memory. In addition, problems may arise with regard to verbal or visual learning, as well as problems in executive and planning functions (4).
Assessing cognitive function is especially important for cancer patients, prior to, during and after the treatment. The patients must go through a treatment sequence where they need to relate to a number of health service agencies (5). It can be argued that cancer treatment may have a negative effect on cognitive function in both the short and long term.
Furthermore, the treatment may have a negative effect on social relationships, education and work, as well as on quality of life (4). A review article (6) revealed that clinicians need better knowledge to be able to recommend interventions to address the cognitive changes that cancer survivors experience. One way to obtain this information is to measure the patient’s own perception of his or her cognitive function.
Attentional Function Index
Attentional Function Index(AFI) is an instrument developed by professor Bernadine Cimprich in the USA for use on cancer patients. The objective of the instrument is to assess the patients’ self-reported ability to focus on activities of daily living that require fundamental cognitive processes (5, 7).
The AFI measures the patient’s ability to stay focused, short-term memory and higher-level executive functions. Executive functions are cognitive processes that enable a person to generate ideas, initiate actions, adapt to new or unfamiliar situations, sort sensory impressions, concentrate, persevere, show cognitive flexibility, relate to multiple cognitive processes at the same time, and suppress undesired responses (8, 9).
Originally, AFI included 16 questions (7, 10), later reduced to 13 based on the results of a factor analysis (5). The questionnaires are primarily used for patients with breast cancer (10–13), but also in samples of persons with other cancer diagnoses (14, 15). AFI is used for both genders and various age groups of adult cancer patients before, during and after the treatment. Cronbach’s alpha for both questionnaires is > 0.90 (10–15) with high test-retest reliability (16).
COSMIN
‘COnsensus-based Standards for the Selection of Health Measurement Instruments’ (COSMIN) includes recommendations for terminology, taxonomy and methodology in studies concerning self-reporting questionnaires and their measurement properties. According to these recommendations, inter-cultural validity is described as a small element of the total validity of the instrument in question (17).
Similarly, COSMIN makes few references to the translation procedure for an instrument (18). In our study, we emphasise the cultural adaptation in the translation of the instrument and have therefore not undertaken any testing of its psychometric properties.
Objective of the study
AFI assesses cancer patients’ own perception of their cognitive functioning in daily life and is thus relevant for studies that highlight this function. We therefore wished to apply a systematic and thorough approach to the translation process.
We wished to include users in this process in order to ensure cultural adaptation to Norwegian conditions. Cimprich gave permission to translate the questionnaire. In consultation with Cimprich we chose to translate the 16-question version, in order to be able to test the factor structures of the two different versions of the questionnaire.
This article thus has two objectives:
- to provide an account of the translation of AFI into Norwegian
- to present results from testing of AFI among people older than 60 years
Method
Translation procedure
To translate and assess the content of the instrument we used the first three steps in the protocol from the World Health Organization (WHO) (19): translation, expert panel and back-translation.
Five experts with a broad range of competence in cognitive processes and development of instruments were involved in the translation procedure and assessment of the validity of the content. The expert group included one user representative, three researchers with specialist competence in psychology, nursing and cancer, and a psychologist with specialist competence in cognitive instruments.
These professionals possess wide-ranging research experience, including previous experience from Norwegian translations of instruments developed in the USA. They all possess level C English skills, advanced user (20), and many of them have sound understanding of American culture. In the translation procedure – back-translation into English – an authorised translator participated actively.
The English-language version of the AFI (Appendix 1) was translated into Norwegian by the first author. The expert group discussed and commented on this version as well as a previous Norwegian version of the AFI (21). We assessed the extent to which the English and Norwegian texts were conceptually, technically and linguistically equivalent, consistent with the selected recommendations (19, 22).
The expert group agreed on a preliminary translation. The questionnaire was then translated into English by the professional translator, who had no previous knowledge of the instrument (19) and sent to Cimprich, the author of the AFI, for a statement.
The first author communicated the feedback from Cimprich to the translator. The first author and the translator thoroughly assessed the comments to the questions from Cimprich, in terms of language as well as culture. The comments were returned to the instrument developer, who assessed this input. Finally, we convened the expert panel to approve the Norwegian version.
Pilot testing
For purposes of quality assurance of the translation with potential users of AFI, we undertook a pilot test to examine whether the translated questionnaire functioned well for persons older than 60 years. Polit and Young (23) recommend undertaking such a pilot test before the instrument is trialled with the target group. In the period from December 2015 to March 2016 we recruited men and women using the ‘snowball sampling’ method (24, 25).
These persons could then refer us to further informants. Five of the co-authors contacted a person older than 60 years in their network, who in turn recruited participants in their network. Snowball sampling can be used when informants cannot be easily identified.
All these persons responded to the questionnaire, and the respondents noted their own gender and age. We requested twelve selected persons, three persons from two of the groups and two persons from three of the groups, to provide written feedback, noting whether some of the questions were hard to understand, hard to answer or unacceptable and intrusive.
We deliberately chose not to test the translation on cancer patients, since this would have imposed an unnecessary burden on them. We wished to produce the best possible translation before testing the questionnaire on elderly cancer patients.
The AFI instrument
The AFI includes twelve questions on activities that require varying degrees of cognitive function associated with defining goals, planning and performing activities of daily living. The questionnaire also includes questions on goal attainment. In addition, the questionnaire includes four questions that measure subjective perception of attention deficit (5, 7).
The answers are crossed off on a numerical rating scale (NRS) (0–10), on which higher scores indicate better functioning. Questions 13 to 16 are reversed, so that lower scores indicate better functioning. Total scores are calculated as an average of the points scored on each item, where higher scores indicate better functioning and less attention deficit (11).
Data analysis
We analysed the data with the aid of IBM SPSS Statistics, Version 24. We used descriptive statistics, analysing demographic data and each of the AFI questions using frequency analyses, averages and standard deviations.
Ethics
Participation in the study was voluntary, and all participants provided an indirect informed consent by submitting the completed questionnaire and any supplementary comments to the form. All respondents remained anonymous. The participants noted only their gender and age. The response forms have been shredded, but the computer file will be stored for five years as recommended by the Regional Committees for Medical and Health Research Ethics (REK).
Results
The expert group’s proposed translation
The expert group met to discuss the two versions of AFI. The members of the expert group each provided their feedback based on their respective competencies. Each question was discussed with a view to its applicability. The input provided by the user representative was critical, especially in her pointing out the importance of using a simple and easily understandable language that would cause no offence to the target group.
The translation of the scale in the English version is a case in point. In the English version, the end point of the scale is ‘extremely well’. In Norwegian, the equivalent is an uncommon phrase, especially when assessing cognitive function in a group that may perceive this as difficult. The user proposed to reformulate the end point to ‘svært godt’ (‘very well’), i.e. a deviation from a direct translation that would have been ‘ekstremt godt’ (‘extremely well’)
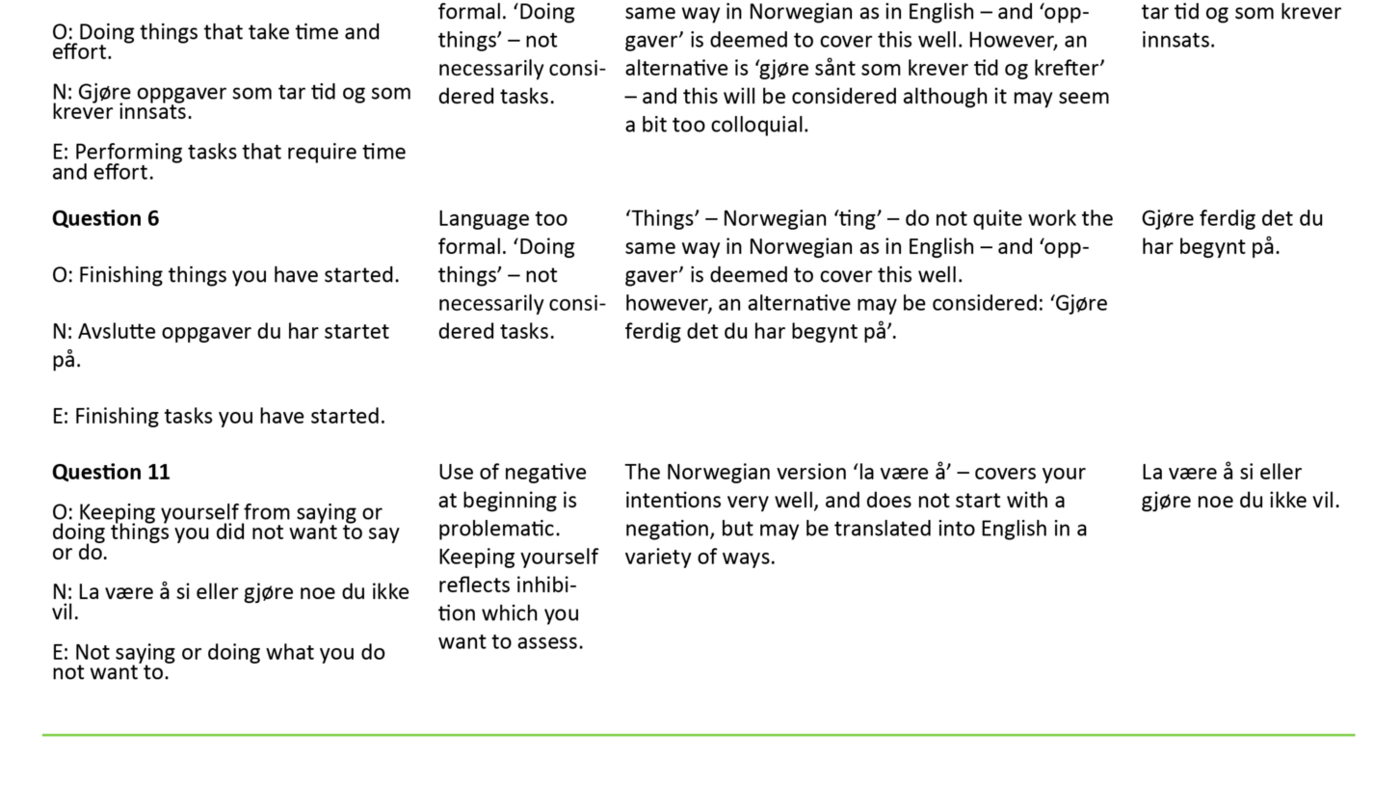
The specific contribution from the psychologist to this process concerned the translation of the conceptual content of questions 7, ‘Keeping your mind on what you are doing’, and 11, ‘Keeping yourself from saying or doing things you did not want to say or do’. The expert panel reviewed all questions, identified ambiguities in the proposed translations and discussed them until a consensus was reached.
Translation from Norwegian into English with the approval of the instrument developer
All questions were subsequently translated back into English by the authorised translator and sent to Cimprich. They contained some deviations from the original English version, and the instrument developer gave comments to the back-translation. After a discussion between the first author and the translator, we responded to the instrument developer’s comments. This communication continued until Cimprich approved the questionnaire, as did the expert panel. Examples of the process are shown in Table 1.
Pilot testing
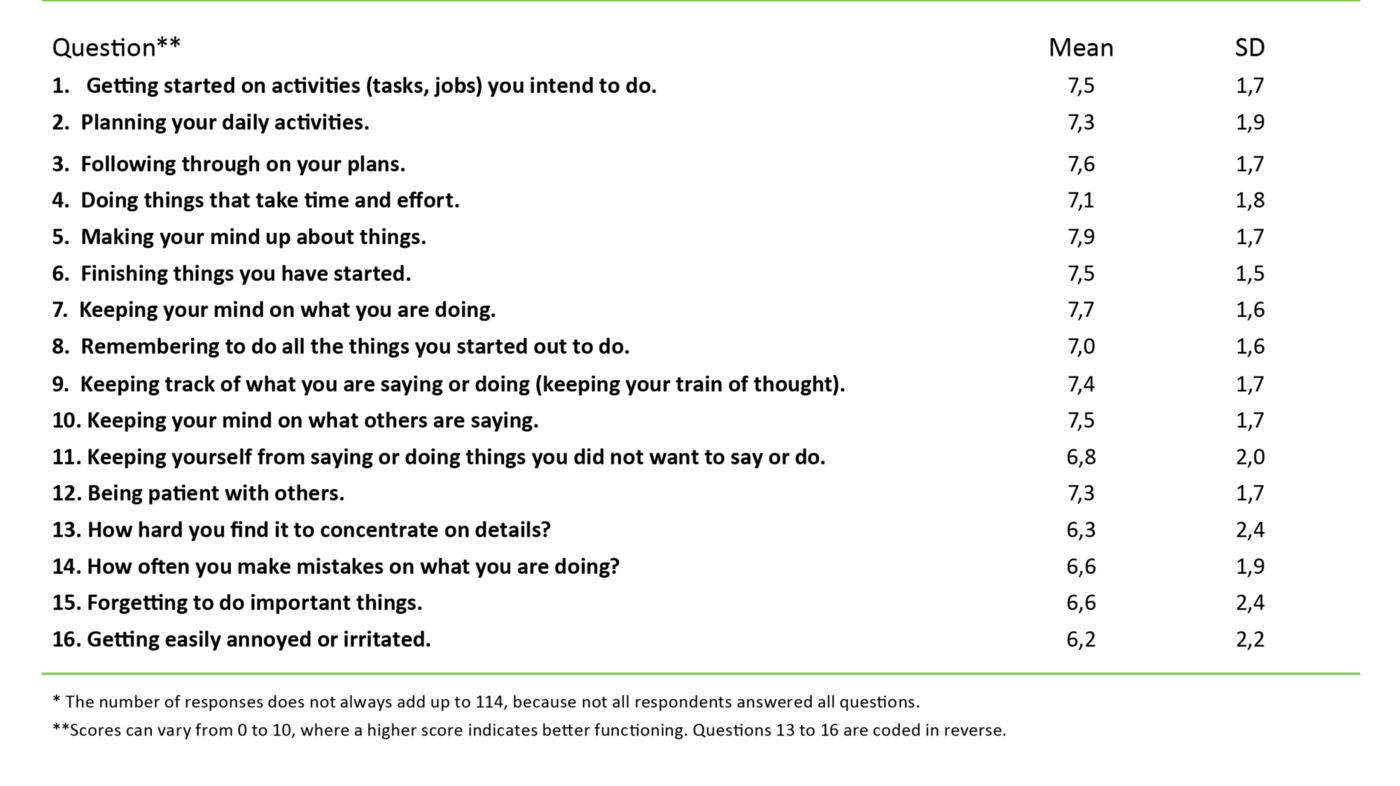
The sample included 114 persons; 42 men and 72 women. Their age varied from 60 to 90 years, with an average age of 71 years, standard deviation (SD) 7. Averages and SDs for each of the questions in AFI are shown in Table 2.
The average scores varied from 6.2 (SD 2.2) for question 16 ‘Getting easily annoyed or irritated’ to 7.9 (SD 1.7) for question 5 ‘Making your mind up about things’. Questions 13, 15 and 16 had an SD of 2.4, 2.4 and 2.2 respectively. For questions 1, 3 and 12 there was one missing score, for question 6 there were two and for question 11 there were eight.
The respondents’ feedback regarding their comprehension of the questions
In addition to those twelve who were requested to provide supplementary comments to the instrument, another six people provided comments to the questionnaire on their own initiative. Fifteen of these eighteen respondents commented on question 11 ‘La være å si eller gjøre noe du ikke vil’ (‘Keeping yourself from saying or doing things you did not want to say or do’). The comments varied in content; some wrote that the question was hard to understand, and that it was ambiguous.
Others noted that it was difficult to answer, because the question asks about two different things. Some simply entered one or more question marks on this item. Similar comments on asking about two things were also entered for questions 8 ‘Huske å gjøre alle de tingene du har begynt på’ (‘Remembering to do all the things you started out to do’) and 9 ‘Holde orden på hva du sier eller gjør’ (‘Keeping track of what you are saying or doing (keeping your train of thought’)).
Many of those who were asked to comment also provided suggestions for changes to the questions. For question 8 ‘Huske å gjøre alle de tingene du har begynt på’ they suggested changing the two last words from ‘begynt på’ (started out to do’) to ‘tenkt å gjøre’ (‘thought of doing’). They also suggested changing question 7 ‘Være konsentrert om det du holder på med’ (‘Keeping your mind on what you are doing’) to ‘Lar du deg lett distrahere/forstyrre?’ (‘Do you let yourself be easily distracted/disturbed?’).
Two respondents commented that the scoring of the last four questions was reversed. One noted that this scoring could confound someone who answered quickly, while another remarked: ‘Is this in itself a test of attention?’
Discussion
This study shows that it might be appropriate to make all steps in a translation procedure available to future users of an instrument. The work of the expert panel and the composition of the group highlight the fact that differences in background experience were crucial to clarify the choices that were made before a consensus was reached. A procedure of this type may be essential to ensure the validity of an instrument.
Without a complete presentation of each part, providing justification for all the choices made and the need for any changes called for, will be difficult. Many articles on validation describe the translation procedure only in terms of the type of procedure used (26–28). According to Johnson, it is difficult to assess the translation of questionnaires without having a description of the cultural adaptation available (29).
A review of 13 articles on validation of the Edmonton Symptom Assessment System (ESAS) reports that only a single study was concerned with translation as a challenge in the validation process (30).
Multiple versions are not uncommon
It is not uncommon to find multiple Norwegian-language versions of the same questionnaire. For example, Bergh and collaborators show that a total of 40 different versions of ESAS are found in Norway (31). The researchers assessed their differences in terms of content, wording, end points and scale formats for this instrument.
The review showed major variations in the heading, introduction, time frame for the assessment, the symptoms included, sequence and wording, adjectives on the numerical scale and the format of the response scales in the ESAS instrument. We do not know why as many as 40 different versions exist, and we have no knowledge as to whether they represent improvements on previous versions or have been produced because researchers have been unaware of the existing versions.
In Denmark, Boel and collaborators have described what they see as problematic due to the availability of numerous versions of ESAS (32). They highlight the importance of describing the translation process and adapting the questionnaire to the culture within which it will be used. They discuss, for example, whether there is a difference between being ‘sløv’ (‘lethargic’) and ‘døsig’ (‘drowsy’, ‘dazed’).
Our results corroborate this line of argument. Even though the validity of an instrument has been documented by a single study and published in one academic journal, there are no set standards for validation. Cultural adaptation of an instrument should be an ongoing process in order to ensure its validity. This view is supported by a review article that points out the necessity of continuing the validation process (30).
Using a professional for the back-translation
International translation procedures set as a standard that a professional translator be used when translating back to the original language (22). Some studies refer specifically to the back-translation and comment on linguistic challenges (33, 34). To our knowledge, the use of a professional translator as a language expert after completion of the first back-translation has not been described previously.
By using an authorised translator in the process of argumentation in a Norwegian context, the researchers will be able to ensure validation of the language used and thus also the validity of the instrument’s content. If no authorised translator is used in the dialogue with the instrument developer, the expert panel risks accepting the instrument developer’s response to the translator’s version without question.
In our study, the user representative emphasised that the word ‘ekstrem’ (‘extremely’), which was one of the end points of the scale, should not be used. In the quality-of-life instrument RAND-36, the end point of the scale in the Norwegian version is ‘ekstremt mye’, which is a direct translation of ‘extremely’.
It is questionable whether responding that ‘... physical health or emotional problems have extremely affected daily activities with family, friends, neighbours or other groups of people’ (... ekstremt mye’) is as common in Norway as it is in the USA. Boel and collaborators point out that attention must be paid to the end points of the scale, giving a Danish version of ESAS as an example, in which ‘unconscious’ is one of the end points (32).
Linguistic challenges in translation
The pilot test of AFI that was undertaken once the expert panel and the instrument developer had reached agreement showed that the instrument was easy to complete. The vast majority answered all questions. There were, however, objections to one question in particular: ‘La være å si eller gjøre noe du ikke vil’ (‘Keeping yourself from saying or doing things you did not want to say or do’). The translator and the instrument developer had previously discussed this question, and the psychologist and other members of the expert panel had commented on it.
The expression ‘keeping yourself from’ has no obvious Norwegian translation. The expert group assessed the input conceptually, culturally and in terms of language. In particular, we discussed whether ‘la være’ (‘refrain from’) is a negation or not. After thorough consideration the expert panel chose not to change the wording.
The results from the pilot test showed that the question ‘La være å si eller gjøre noe du ikke vil’ had the most missing scores and most comments in the questionnaires. Eight persons did not answer the question, and 18 others had entered comments. Since this applied only to this question, one possible explanation could be that that the respondents simply failed to understand what was asked.
This discussion illustrates that translating an American instrument into Norwegian, in terms of language as well as culture, may involve challenges. If the argumentation on which a translation is based is made available to those who want to use the instrument, this will increase the understanding of the choices made and the changes that can be made, if any are called for.
Reversed scores
It is interesting to note that on the whole, the standard deviations for the four last questions in the AFI are higher than for the other questions. The same tendency is reported from a sample of young women with breast cancer, for whom the same instrument was used (5).
We cannot know for certain whether this is due to the content of the questions or a larger variation in the responses. We may speculate, though, that this is a result of the reversal of the scales, when compared to the preceding questions.
On the other hand, the use of reversed scoring may indicate the respondent’s level of attention, since this instrument also measures any attention deficit in the respondents (35). Results from the participants in our study are comparable to those in a study undertaken among women and men aged 65–87 who were living at home (36).
However, they had better cognitive function than women aged 27–86 with breast cancer (5). Since the sample in our study included persons older than 60 years, without any known cancer diagnosis as an inclusion criterion, this may indicate that the instrument functioned well.
One of the strengths of this study is its use of an expert panel with a user representative and a professional translator. Moreover, the participants in the pilot study had the opportunity to provide feedback on the design of the instrument. We might have wished for a representative sample of the general population, but this was impossible for practical, ethical and financial reasons.
Use of snowball sampling may be another strength, since large parts of the country were included. On the other hand, this methodology may have a weakness in causing sampling bias, nor do we have any information about the participants’ condition of health.
Conclusion
Translation and cultural adaptation of an instrument is a comprehensive process. It is appropriate to make each step of the translation procedure available, thus to enable researchers to assess the choices that have been made. Including user representatives in an expert panel may help improve the validation of a questionnaire. In collaboration with the expert panel, the dialogue between the translator and the instrument developer may help ensure that the intention behind the instrument is maintained.
The Norwegian version of the AFI which is now available must be tested on a larger sample of cancer patients aged 60 and above before we can draw any final conclusions regarding its intercultural validity. Accordingly, this study does not permit any conclusions regarding the reliability, validity and responsiveness of this instrument.
References
1. Cancer in Norway 2015 – Cancer incidence, mortality, survival and prevalence in Norway. Oslo: Cancer Registry of Norway; 2016.
2. Mandelblatt JS, Hurria A, McDonald BC, Saykin AJ, Stern RA, Vanmeter JW, et al. Cognitive effects of cancer and its treatments at the intersection of aging: what do we know; what do we need to know? Seminars in Oncology. 2013;40(6):709–25.
3. Anderson-Hanley C, Sherman ML, Riggs R, Agocha VB, Compas BE. Neuropsychological effects of treatments for adults with cancer: a meta-analysis and review of the literature. Journal of the International Neuropsychological Society. 2003;9(7):967–82.
4. Ahles TA, Root JC, Ryan EL. Cancer- and cancer treatment-associated cognitive change: an update on the state of the science. Journal of Clinical Oncology. 2012;30(30):3675–86.
5. Cimprich B, Visovatti M, Ronis DL. The Attentional Function Index – a self-report cognitive measure. Psycho-oncology. 2011;20(2):194-202.
6. Von Ah D, Storey S, Jansen CE, Allen DH. Coping strategies and interventions for cognitive changes in patients with cancer. Seminars in Oncology Nursing. 2013;29(4):288–99.
7. Cimprich B. A theoretical perspective on attention and patient education. Advances in Nursing Science. 1992;14(3):39–51.
8. Jurado MB, Rosselli M. The elusive nature of executive functions: a review of our current understanding. Neuropsychology Review. 2007;17(3):213–33.
9. Engstad RT, Engstad TT, Davanger S, Wyller TB. Eksekutiv svikt etter hjerneslag. Tidsskrift for Den norske legeforening. 2013;133(5):524–7.
10. Cimprich B. Attentional fatigue following breast cancer surgery. Research in Nursing & Health. 1992;15(3):199–207.
11. Cimprich B, So H, Ronis DL, Trask C. Pre-treatment factors related to cognitive functioning in women newly diagnosed with breast cancer. Psycho-oncology. 2005;14(1):70–8.
12. Jansen CE, Dodd MJ, Miaskowski CA, Dowling GA, Kramer J. Preliminary results of a longitudinal study of changes in cognitive function in breast cancer patients undergoing chemotherapy with doxorubicin and cyclophosphamide. Psycho-oncology. 2008;17(12):1189–95.
13. Merriman JD, Jansen C, Koetters T, West C, Dodd M, Lee K, et al. Predictors of the trajectories of self-reported attentional fatigue in women with breast cancer undergoing radiation therapy. Oncology Nursing Forum. 2010;37(4):423–32.
14. Shih J, Leutwyler H, Ritchie C, Paul SM, Levine JD, Cooper B, et al. Characteristics associated with inter-individual differences in the trajectories of self-reported attentional function in oncology outpatients receiving chemotherapy. Supportive Care in Cancer. 2017;25(3):783–93.
15. Visovatti MA, Reuter-Lorenz PA, Chang AE, Northouse L, Cimprich B. Assessment of cognitive impairment and complaints in individuals with colorectal cancer. Oncology Nursing Forum. 2016;43(2):169–78.
16. Cimprich B. Development of an intervention to restore attention in cancer patients. Cancer Nursing. 1993;16(2):83–92.
17. Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. Journal of Clinical Epidemiology. 2010;63(7):737–45.
18. Mokkink LB, Terwee CB, Knol DL, Stratford PW, Alonso J, Patrick DL, et al. The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: a clarification of its content. BMC Medical Research Methodology. 2010;10:22.
19. Verdens helseorganisasjon (WHO). Process of translation and adaptation of instruments. 2016. Available at: http://www.who.int/substance_abuse/research_tools/translation/en/(downloaded 14.12.2017)
20. Utdanningsdirektoratet. Det felles europeiske rammeverket for språk. 2011. Available at: https://www.udir.no/Upload/Verktoy/5/UDIR_Rammeverk_sept_2011_web.pdf?epslanguage=no(downloaded 14.12.2017).
21. Gonzalez MT, Hartig T, Patil GG, Martinsen EW, Kirkevold M. Therapeutic horticulture in clinical depression: a prospective study. Research and Theory for Nursing Practice. 2009;23(4):312–28.
22. Polit DF, Beck CT. Essentials of nursing research : appraising evidence for nursing practice. 8. ed.Philadelphia, PA: Wolters Kluwer / Lippincott Williams & Wilkins; 2014.
23. Polit DF, Yang FM. Measurement and the measurement of change. Philadelphia, PA: Wolters Kluwer / Lippincott Williams & Wilkins; 2015.
24. Christoffersen L, Johannessen A, Tufte PA, Utne I. Forskningsmetode for sykepleierutdanningene. Oslo: Abstrakt forlag; 2015.
25. Polit DF, Beck CT. Nursing research : generating and assessing evidence for nursing practice. 10. ed. Philadelphia, PA: Wolters Kluwer; 2017.
26. Miki-Rosario N, Garcia Filho RJ, Garcia JG, Dini GM, Bottomley A, Chow E, et al. Translation into Portuguese, cross-cultural adaptation and validation of «The European Organization for Research and Treatment of Cancer-Quality of Life Questionnaire-Bone Metastases-22». Annals of Palliative Medicine. 2016;5(3):190–5.
27. Reinertsen H, Christophersen K-A, Helseth S. Vurdering av postoperativ smerte hos barn (0-5 år): Validering og reliabilitetstesting av smertevurderingsverktøyet FLACC. Sykepleien Forskning. 2014;9(2):136–44. Available at: https://sykepleien.no/forskning/2014/02/validering-og-reliabilitetstesting-av-smertevurderingsverktoyet-flacc(downloaded 15.12.2017).
28. Sjetne IS, Tvedt C, Squires A. Måleinstrumentet ʻThe Nursing Work Index-Revisedʼ – oversettelse og utprøvelse av en norsk versjon. Sykepleien Forskning. 2011;6(4). Available at: https://sykepleien.no/forskning/2011/11/maleinstrumentet-nursing-work-index-revised-oversettelse-og-utprovelse-av-en-norsk(downloaded 15.12.2017).
29. Johnson TP. Methods and frameworks for crosscultural measurement. Medical Care. 2006;44(11 Suppl 3):S17–20.
30. Nekolaichuk C, Watanabe S, Beaumont C. The Edmonton Symptom Assessment System: a 15-year retrospective review of validation studies (1991–2006). Palliative Medicine. 2008;22(2):111–22.
31. Bergh I, Aass N, Haugen DF, Kaasa S, Hjermstad MJ. Symptom assessment in palliative medicine. Tidsskrift for Den norske legeforening. 2012;132(1):18–9.
32. Boel K, Haaber K, Byskov, L. Dansk versjon av ESAS – symptomregistrering. Omsorg. 2009(1):41–6.
33. Beck CT, Bernal H, Froman RD. Methods to document semantic equivalence of a translated scale. Research in Nursing & Health. 2003;26(1):64–73.
34. Yu DS, Lee DT, Woo J. Issues and challenges of instrument translation. West J Nurs Res. 2004;26(3):307–20.
35. Podsakoff PM, MacKenzie SB, Podsakoff NP. Sources of method bias in social science research and recommendations on how to control it. Annual Review of Psychology. 2012;63:539–69.
36. Jansen DA. Attentional demands and daily functioning among community-dwelling elders. Journal of Community Health Nursing. 2006;23(1):1–13.










Comments