Prick up your hearing aid: deaf people’s perceptions of encounters with the health services
Healthcare personnel need more knowledge regarding hearing loss and communication with deaf people. In addition, some healthcare personnel have negative attitudes towards this patient group.
Background: There are approximately 5 000 deaf people in Norway who use sign language to communicate. According to Norwegian legislation, people who are deaf or have severe hearing loss have a right to adapted communication in interactions with the health services. However, research indicates that the health services rarely accommodate their communication needs. This leads to misunderstandings about diagnosis, treatment and medication, and may have serious consequences for the patient in question. Much of the international research in this area is difficult to transfer to the Norwegian context, either because it has been carried out in countries whose healthcare systems differ to that of Norway or it only deals with the challenges faced by healthcare personnel. Therefore, it is important to explore deaf people’s perceptions of their encounters with the health services in Norway.
Objective: To explore how people who are deaf or have severe hearing loss perceive encounters with the health services in Norway.
Method: The study has a qualitative design. We conducted individual, semi-structured interviews with ten people who use sign language in their daily lives. The interviews were carried out in the period from October 2018 to November 2021. The data have been analysed using Braun and Clarke’s method of thematic analysis.
Results: The challenges experienced by deaf people in their interactions with the health services were primarily related to communication with healthcare personnel. The participants did not feel that communication was adapted to their needs. The reasons for this include a lack of knowledge among healthcare personnel concerning hearing loss and communication with deaf people, insufficient coverage of the topic in health-related study programmes and in society generally, as well as variations in the attitudes of healthcare personnel towards deaf people.
Conclusion: When interacting with the health services, deaf people have a right to communication that is adapted to their needs. The findings of the study indicate, however, that healthcare personnel need more knowledge regarding communication with deaf people. This should be put on the agenda of the health services and educational institutions that train healthcare personnel.
Of the 16 500 people who communicate using sign language in Norway, 4–5 000 are classified as deaf (1). Although deaf people have a right to communication that is specially adapted to their needs when interacting with the health services (2, 3), research indicates that they often encounter barriers (4–7). Norwegian sign language is one of the largest minority languages in the country (1).
The Norwegian Act relating to Language guarantees deaf people the right to use sign language, and clearly states that sign language is equal to spoken Norwegian (3). Whether someone uses sign language as their first language does not always depend on their level of hearing loss, but may also reflect hearing function and deaf identity (1).
Deaf people’s access to and experience of the health services vary greatly across countries (8, 9). Several studies have shown that communication barriers are often a problem for deaf people in interactions with the health services.This leads to misunderstandings between deaf patients and healthcare personnel in relation to diagnosis, treatment and medication (7, 10).
Due to previous negative experiences, deaf people avoided using the health services until it was absolutely necessary in a number of cases (5, 11). Deaf people also reported significantly poorer communication and a lower level of satisfaction with the primary health service than the general population (10). Communication difficulties also have an impact on the rights of deaf people, such as the right to autonomy, protection of privacy and communication in their own language (12).
For their part, healthcare personnel find it challenging to communicate with deaf people (13, 14). They state that the health services are not good enough for deaf patients, and that the healthcare system is not adapted to the needs of this patient group (15).
In addition to this, a study of doctors’ attitudes shows that they find it more difficult to communicate with deaf people than the rest of the population, and they feel less comfortable in their interactions with deaf patients (16).
Research exploring deaf people’s encounters with the health services is scant. Previous studies in this area have either focused on the challenges faced by healthcare personnel or have been carried out in countries whose healthcare systems differ to that of Norway (17), which makes it difficult to transfer the findings to the Norwegian context. Therefore, it is important to explore deaf people’s perceptions of their encounters with the health services in Norway.
Objective of the study
We wanted to explore how people who are deaf or have severe hearing loss perceive their encounters with the health services in Norway.
Method
The study is based on a qualitative exploratory design. We conducted ten in-depth interviews with adults who are deaf or have severe hearing loss to gain more insight into their perceptions of their encounters with the health services (18).
Recruitment and selection
First, we attempted to recruit research participants through associations and organisations for the deaf and hard of hearing, but no one contacted us. Therefore, we recruited participants for the study through the first author’s (TM) social media network, using snowball sampling. TM is a woman who has studied sign language and works as a nurse in an ear, nose and throat department at a hospital. She made a number of contacts with sign language users when she was a student.
Snowball sampling is a method for selecting participants in which existing research participants find potential new participants for a study by telling their social network about it (19). Since sign language users are a minority that can be difficult to reach using traditional recruitment methods (20), we considered it practical to use TM’s network as a basis for recruitment using snowball sampling.
We recruited six women and four men aged 25–50 for the study. The sample is heterogenous in relation to their place of residence and the level of the health service they have interacted with. Eight of the participants were interviewed while at work.
The research participants have varying degrees of hearing loss, from severe to profoundly deaf. They were not explicit about the degree to which they identify as deaf or hard of hearing, but their use of sign language was a common factor, and they are therefore referred to as deaf in this study (21).
Interviews
We prepared a semi-structured interview guide with open-ended questions to get an understanding of the participants’ perceptions of their encounters with the health services, including the positive and negative aspects. We also wanted to find out how they perceived communication with healthcare personnel. The interview guide was prepared with a basis in the first author’s experience with deaf people, our knowledge of health services for minority groups and available research in this field (4–12).
The study is based on ten in-depth interviews, with a duration of 30–90 minutes. Two of the interviews lasted for 30 minutes because the participants had few encounters to relate. The other interviews lasted for over an hour due to the comprehensive descriptions of encounters and/or the use of a sign language interpreter. The first interview was conducted in 2018.
The study was delayed as a result of the COVID-19 pandemic. We therefore conducted the second interview in autumn 2020 and the others in autumn 2021. The first author carried out in-person interviews either at the private homes of the participants or at another previously arranged place. We clarified with each participant in advance how the interview would be conducted and whether they would like to use a sign language interpreter.
Six of the interviews were conducted via a sign language interpreter, but this was not required in four of the interviews. Two of these four participants responded orally in the interview, and two communicated using sign language, which the first author observed and transcribed to written text.
Afterwards, we sent the transcriptions to the participants for them to review and make corrections if necessary. TM knew one of the participants from her student days, but they had not had contact since then. Otherwise, TM and the participants did not know each other.
Analysis
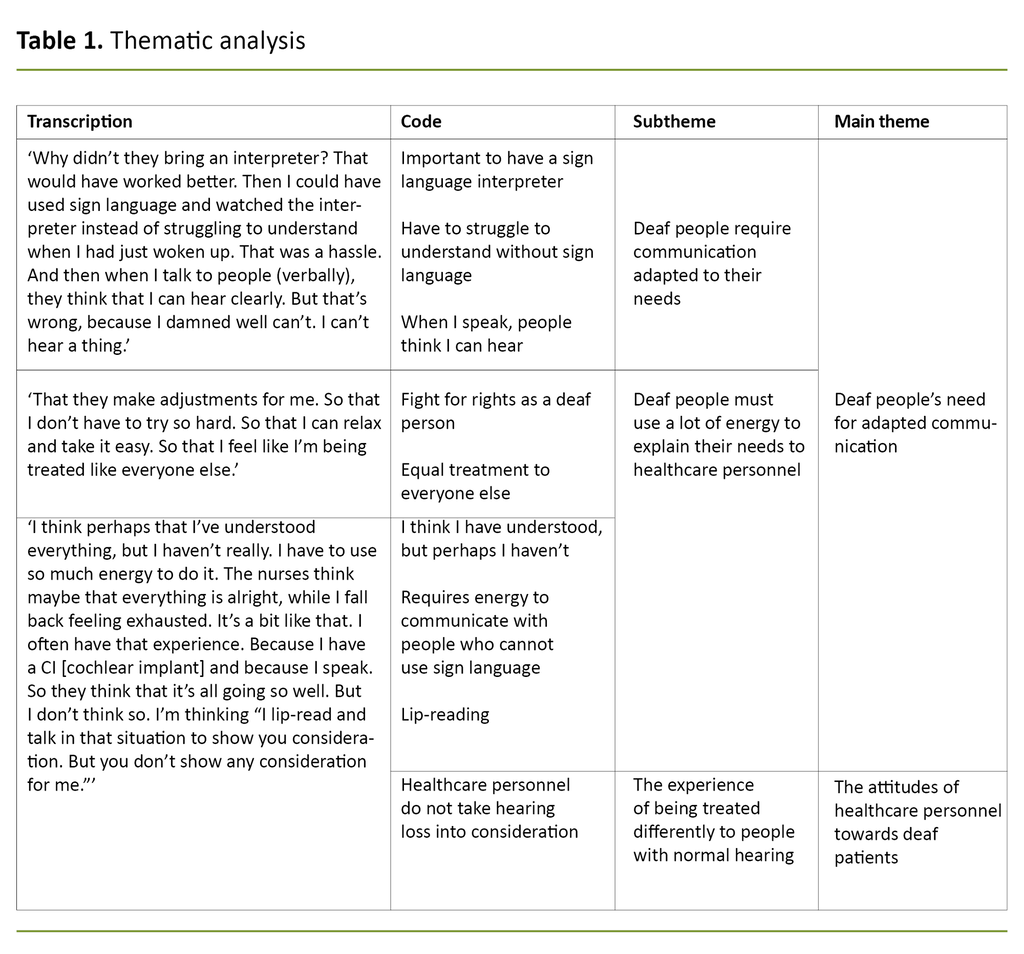
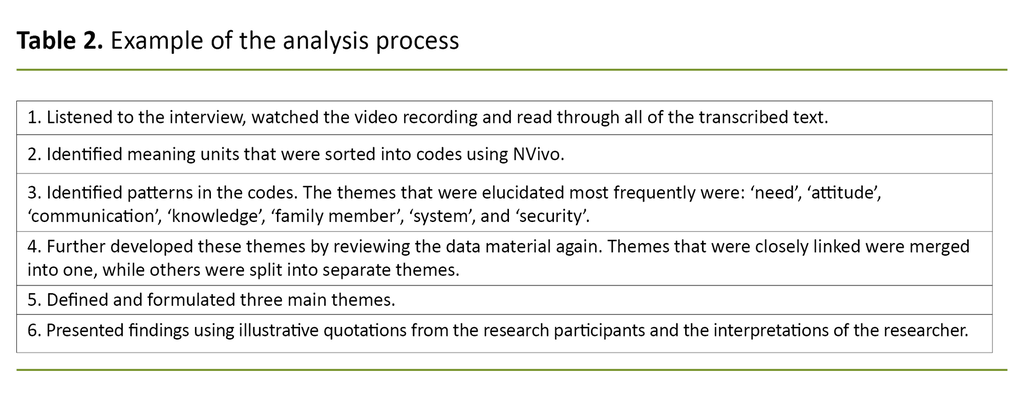
To analyse the participants’ responses in sign language, the interviews were recorded on video and later transcribed by the first author. After that, we analysed the data, using Braun and Clarke’s (22) six-step method of thematic text analysis as inspiration. The data were coded according to whether the responses were of interest in relation to the objective and central research question of the study, known as ‘data-driven coding’ (Table 1).
Both authors took part in the data analysis. In cases where we disagreed, we discussed the meaning units and themes until we reached consensus. Table 2 shows examples of the process of developing meaning units into themes.
Ethical considerations
The study was submitted to the Norwegian Centre for Research Data (NSD) for approval (reference number 510500). The participants received written information about the study. They were informed that they were free to withdraw from the study without giving a reason, and that all of the data collected would be anonymised. All of the participants provided written consent to participate.
Results
The analysis of the interviews shows that the research participants’ interactions with the health services were influenced by the extent to which their communication needs were accommodated, the attitude of health personnel towards deaf patients, and the level of knowledge health personnel had regarding communicating with deaf people.
Deaf people’s need for adapted communication
Several of the research participants told us that it was important that they received information about their own health in sign language. They said that it was best if health personnel were able to communicate with them directly using sign language, but in many cases, this was not possible. The participants stressed how important it was for them to have access to a sign language interpreter when they needed it. Nevertheless, they found that they were not provided with an interpreter despite having made their needs known:
‘On several occasions, I have sat there wondering “well, when is the doctor coming?” I hear him call out, but whose name is he calling? I have to go to the receptionist and ask, “What’s happening?” “Yes, we have called your name,” but I have already told them that I have poor hearing! So, [it’s] like, just a typical experience. And I think I speak for many others, to put it like that. So you sit there with your ears pricked up, or your hearing aid pricked up [resigned laughter], and I have to be really switched on, all the time. It’s tiresome.’
The participants called for routines for communicating with deaf patients, such as having a special folder containing all relevant information, a brochure or something similar, so that healthcare personnel are better informed about the need for help and how to address different situations:
‘So, I was lying ready on the operating table and the surgeon had a surgical mask on. And I saw that he was starting to speak, so I said, “No, I don’t understand.” Then he held up two syringes, like this [holds up both hands as if he has a syringe in each hand, and shows his head falling to one side with closed eyes (asleep)]. And then I understood.’
Checking to make sure that the information that has been given has been understood, facing the patient, and agreeing on and informing the patient prior to carrying out examinations are good strategies, according to the participants.
Healthcare personnel’s level of knowledge about communication with deaf patients
Participants felt that healthcare personnel did not have enough knowledge about hearing loss and deafness, communication with deaf people, how to enlist and use the services of an interpreter, and what they should do when faced with a deaf patient:
‘“Can she read?” and Mum just says “Er, yes. She can do everything except hear. That is, it’s just her hearing.” “But tell her it’s very important that she administers the medicine, that is, that she doesn’t doing anything wrong to her child.” So, it’s like I am being underestimated as a human being. So then Mum said, “There’s nothing wrong with her brain, it’s just her hearing!” It’s possible that the doctor on duty said something, maybe they had explained a little beforehand. I don’t know, but the doctor themself knew something. It was like, the doctor’s friend is deaf or something or other. Something like that. But, then again, that’s knowledge.’
The participants told us that it made a big difference to them when they met healthcare personnel who could use sign language, and that they wished more of them could do so. Communication in sign language, either with healthcare personnel who could use it themselves or via a sign language interpreter, made them feel more secure in their interaction with the health services. They called for more training and teaching on the topic of hearing loss and communication with deaf people, and felt that it should be included in health-related study programmes.
The attitudes of healthcare personnel towards deaf patients
Many of the participants indicated that they often had good experiences with the health services when they encountered healthcare personnel who were solution-oriented and did their best to ensure that communication was effective. However, they also reported having been in situations where they felt their needs were not addressed.
One of them described a situation during the COVID-19 pandemic where there was a discussion about whether interpreters or family members could be present at the hospital. Family members were allowed to be with the participant in their room, but were not allowed to be with them outside their room even though this is what the participant needed, because consideration for the other patients was given precedence:
‘There was a buffet, but there was a person serving it up on your plate. I needed an interpreter there really, to talk to the person. I was completely exhausted – hadn’t slept for three days. To stand there and have to lip-read and all of that. But no, my family member was not allowed to leave my room because we had to consider the feelings of the other patients [dry laughter]. And that’s the way it is. I didn’t think about it so much there and then, because I was just happy that my family member was allowed to stay. But afterwards, I have felt more and more that, okay, considering the feelings of those non-disabled patients was more important than accommodating my needs.’
This participant knew that the same thing had happened to another deaf patient who did not have a toilet in their room. The person’s family member had to urinate in the wash basin in the room so that the other patients did not see that the patient was allowed to have a family member with them.
Discussion
The objective of the study was to explore how people who are deaf or have severe hearing loss perceive encounters with the health services. One of the main findings of our study is that deaf people have a need for adapted communication in interactions with the health services. This finding corresponds with other studies on interactions between deaf people and the health services (6, 7, 11, 12).
Deaf patients experienced, for example, unpleasant situations that made them feel embarrassed or ashamed when communication was not adapted to their needs. Consequently, many of them avoided using the health services (23). Major misunderstandings in communication with healthcare personnel also led deaf people to avoid the primary health service altogether, contacting emergency departments or outpatient clinics instead (5).
Deaf people also reported having significantly poorer communication with their GP than the general population (10). These findings differ from our study, in which the participants told us that they had a satisfactory or good relationship with their GP, and that it was often an advantage to get acquainted with healthcare personnel, so that they could explain their needs to someone who recognised them the next time they met.
Deaf people want to be able to choose the way in which they communicate
Our findings show that it was important for participants to communicate in the way that suited them best, either via a sign language interpreter, in writing or by lip-reading. However, this was not always accommodated, a finding that has been corroborated by several other studies (6, 7, 10–12).
In a British study, deaf patients often found themselves in situations characterised by poor communication, where they were not able to express themselves in their preferred manner (10). For many deaf people, sign language interpreters are an important medium for good communication with those who cannot use sign language. Some of them found that, as a rule, they were provided with an interpreter when they needed it. Several others found that their need for an interpreter was not met, even though the health services are obligated to ensure that communication between healthcare personnel and patients is adapted to patients’ needs (2, 3, 24).
Several international studies also indicate that there was an absence of interpreters in meetings between the health services and deaf patients (7, 12). Some of the participants felt very insecure and uncertain without an interpreter, which Løkken (4) also found in her study. The participants themselves pointed to possible reasons why they had not been provided with an interpreter, such as healthcare personnel not knowing how to enlist the services of an interpreter, a lack of routines, the fact that the hospital pays for an interpreter on admission, while the National Insurance Scheme covers expenses for an interpreter in most other situations.
Other possible reasons are that healthcare personnel did not know enough about deaf people to understand why it was important to have an interpreter present for more than just a visit to the doctor, and that it could be difficult to find available interpreters in the evening.
Healthcare personnel report that they primarily use miming and written communication in their contact with deaf patients (25). Some of the participants in our study preferred to use written communication with healthcare personnel. There were also some that were dependent on receiving information through sign language in order to understand, and written communication was not sufficient for all people with hearing loss.
Similar findings were made in another study (11), in which deaf patients were interviewed about their experiences when communicating with healthcare personnel at an emergency department or outpatient clinic. Information was often given in writing and orally, and this did not provide the deaf patients in the study with adequate information (11).
Although the participants in our study clarified their needs to healthcare professionals, in several instances these were not met. The same experience has also been reported in other studies. Deaf people pointed out, for example, that asking for communication adapted to their needs could be stressful, frustrating and time-consuming (11).
Healthcare personnel lack knowledge about deaf people and how to enlist and use the services of an interpreter
Another main finding in our study was that participants linked their experience of not having their needs met when interacting with the health services with a lack of knowledge among healthcare personnel regarding deaf people, communication with deaf people and how to enlist and use the services of an interpreter. This corresponds with findings from other studies, in which participants expressed a wish that healthcare personnel received more education and training in the subject (6, 11).
Research also shows that nurses who were offered relevant training had more knowledge about deaf people and their situation than those who were not offered training (14). Providing healthcare personnel with training in communication with the deaf could be a useful measure for improving their knowledge about the deaf.
Furthermore, the participants in our study found that while they did meet solution-oriented healthcare personnel, they also met personnel who were nervous, evasive, stressed or who ignored them. Similar attitudes have been found in other studies. Deaf people had encounters with healthcare professionals that, for example, became frightened, ran away, did not know what to do, and were prejudiced against them (23).
Older deaf people found that they were treated differently, as if they were worth less than patients with normal hearing (26). Facial expression and body language are important aspects of sign language. People who communicate using sign language are used to reading nonverbal communication.
According to Vonen’s (27) description, sign language consists of visible movements of the hands, arms and face, all of which contribute to the total communicative expression. In all communication, body language and nonverbal communication are important aspects of how we interact with other people (28), and this is particularly the case for people who use sign language to communicate.
Strengths and weaknesses of the study
The findings from this study can be transferred to other situations in which people who are deaf or have severe hearing loss encounter healthcare personnel. However, the transfer value is limited to countries with well-developed health services and rights for deaf people.
The deaf are a group that can be difficult to recruit for research purposes. Snowball sampling using the contact network of the first author may have led to the selection of a more homogenous group of participants in regard to age, living situation and employment than might otherwise have been the case using a different method of recruitment.
Although we posed open-ended questions to get an understanding of the participants’ positive and negative experiences in their interactions with the health services, it is not improbable that participants reported the more extraordinary episodes and, conversely, underplayed their positive experiences (29). However, it would have been difficult to uncover the information that they shared with us without the first author’s familiarity with the field, which is a strength of the study (18, 30).
There is also a risk that we may have interpreted some of the communication in the interviews in a different way than the participant intended, as a consequence of using an interpreter as an external medium and through the transcription of the interviews from Norwegian sign language to Norwegian written language by the first author.
We attempted to counteract possible misunderstandings by posing questions that summed up and affirmed what had been said during the interviews, and by asking the two participants whose responses from sign language were transcribed to review and correct the transcriptions. Authorised interpreters with a bachelor’s degree in sign language interpretation were used in all of the interviews involving an interpreter.
Conclusion
The study’s findings indicate that healthcare personnel have a need for more education and training in regard to deaf people and communication with the deaf, as well as better routines for following up this group. These factors may perhaps help to ensure that the needs of deaf people are addressed in a more satisfactory way.
Increasing healthcare personnel’s knowledge can help to ensure that deaf people have access to secure and equitable health services as well as legal protection. Good routines and procedures can contribute to making information more readily accessible.
In further studies, there should be greater exploration of how younger and older deaf people perceive encounters with the health services, as well as examining deaf people’s experiences in specific sectors of the health services. How healthcare personnel perceive their interactions with deaf patients should also be explored.
The authors declared no conflicts of interest.
References
1. Norges Døveforbund. Tegnspråk. Available at: https://www.doveforbundet.no/tegnsprak/hva (downloaded 07.02.2022).
2. Lov 2. juli 1999 nr. 63 om pasient- og brukerrettigheter (pasient- og brukerrettighetsloven). Available at: https://lovdata.no/dokument/NL/lov/1999-07-02-63 (downloaded 17.02.2022).
3. Lov 21. mai 2021 nr. 42 om språk (språklova). Available at: https://lovdata.no/dokument/NL/lov/2021-05-21-42 (downloaded 17.02.2022).
4. Løkken M. Døve og sterkt tunghørte pasienter i somatiske sykehus: likeverdige offentlige helsetjenester? [Master's Thesis]. Trondheim: Norges teknisk-naturvitenskapelige universitet, Institutt for sosialt arbeid; 2014.
5. Sheppard K. Deaf adults and health care: giving voice to their stories. J Am Assoc Nurse Pract. 2014;26(9):504–10. DOI: 10.1002/2327-6924.12087
6. Sirch L, Salvador L, Palese A. Communication difficulties experienced by deaf male patients during their in-hospital stay: findings from a qualitative descriptive study. Scandinavian Journal of Caring Sciences. 2017;31(2):368–77. DOI: 10.1111/scs.12356
7. Rezende RF, Guerra LB, Carvalho SADS. Satisfaction of deaf patients with the health care. Speech, language, hearing sciences and education journals. 2020;22(5):1–17. DOI: 10.1590/1982-0216/20202258119
8. Kuenburg A, Fellinger P, Fellinger J. Health access among deaf people. Journal of Deaf Studies and Deaf Education. 2016;1(10):1–10. DOI: 10.1093/deafed/env042
9. Nilsson A-L, Turner GH, Sheikh H, Dean RK. A prescription for change: report on EU healthcare provision for deaf sign language users. Dublin: Interesource Group (Ireland); 2013. Available at: https://www.researchgate.net/publication/260119583_Medisigns_A_prescription_for_change_-_An_overview_of_European_healthcare_provision_for_Deaf_sign_language_users (downloaded 17.02.2022).
10. Reeves DM, Kokoruwe B. Communication and communication support in primary care: a survey of deaf patients. Audiological Medicine. 2005;3(2):95–107. DOI: 10.1080/16513860510033747
11. James TG, Coady KA, Stacciarini JR, McKee MM, Phillips DG, Maruca D, et al. «They're not willing to accommodate deaf patients»: communication experiences of deaf American sign language users in the emergency department. Qual Health Res. 2022;32(1):48–63. DOI: 10.1177/10497323211046238
12. Rodriguez-Martin D, Rodriguez-Garcia C, Falco-Pegueroles A. Ethnographic analysis of communication and the deaf community's rights in the clinical context. Contemp Nurse. 2018;54(2):126–38. DOI: 10.1080/10376178.2018.1441731
13. Orrie S, Motsohi T. Challenges experienced by healthcare workers in managing patients with hearing impairment at a primary health care setting: a descriptive case study. South African Family Practice. 2018;60(6):1–5. DOI: 10.1080/20786190.2018.1507566
14. Velonaki VS, Kampouroglou G, Velonaki M, Dimakopoulou K, Sourtzi P, Kalokerinou A. Nurses' knowledge, attitudes and behavior toward deaf patients. Disabil Health J. 2015;8(1):109–17. DOI: 10.1016/j.dhjo.2014.08.005
15. Ferndale D, Munro L, Watson B. A discourse of «abnormality»: exploring discussions of people living in Australia with deafness or hearing loss. Am Ann Deaf. 2016;160(5):483–95. DOI: 10.1353/aad.2016.0001
16. Ralston E, Zazove P, Gorenflo DW. Physicians' attitudes and beliefs about deaf patients. J Am Board Fam Pract. 1996;9(3):167–73.
17. Reibling N, Ariaans M, Wendt C. Worlds of healthcare: a healthcare system typology of OECD countries. Health Policy. 2019;123(7):611–20. DOI: 10.1016/j.healthpol.2019.05.001
18. Kvale S, Brinkmann S. Det kvalitative forskningsintervju. 3rd ed. Oslo: Gyldendal Akademisk; 2015.
19. Malterud K. Kvalitative forskningsmetoder for medisin og helsefag. 4th ed. Oslo: Universitetsforlaget; 2017.
20. Sadler G, Lee HC, Lim RS, Fullerton J. Recruitment of hard-to-reach population subgroups via adaptations of the snowball sampling strategy. Nurs Health Sci. 2010;12(3):369–74. DOI: 10.1111/j.1442-2018.2010.00541.x
21. Werngren-Elgström M, Dehlin O, Iwarsson S. A Swedish prevalence study of deaf people using sign language: a prerequisite for deaf studies. Disability & Society. 2003;18(3):311–23. DOI: 10.1080/0968759032000052888
22. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology 2006;3(27):77–101. DOI: 10.1191/1478088706qp063oa
23. Pereira PC, Fortes PA. Communication and information barriers to health assistance for deaf patients. Am Ann Deaf. 2010;155(1):31–7. DOI: 10.1353/aad.0.0128
24. Lov 2. juli 1999 nr. 64 om helsepersonell (helsepersonelloven). Available at: https://lovdata.no/dokument/NL/lov/1999-07-02-64 (downloaded 17.02.2022).
25. Machado WCA, Machado DA, Nébia M, Tonini T, De Miranda RS, de Oliveira GMB. Sign language: how the nursing staff interacts to take care of deaf patients? Revista de Pesquisa: Cuidado é Fundamental Online. 2013;5(3):283–92. DOI: 10.9789/2175-5361.2013v5n3p283
26. Witte TN, Kuzel AJ. Elderly deaf patients' health care experiences. J Am Board Fam Pract. 2000;13(1):17–22. DOI: 10.3122/jabfm.13.1.17
27. Vonen AM. Tegnspråk i et lingvistisk perspektiv. In: Jørgensen SR, Anjum RL, eds. Tegn som språk. Oslo: Gyldendal Norsk Forlag; 2006. pp. 125–50.
28. Eide T, Eide H. Kommunikasjon i praksis. Oslo: Gyldendal Akademisk; 2008.
29. Maynard-Moody SW, Musheno MC. Cops, teachers, counselors: stories from the front lines of public service. Ann Arbor, Michigan: University of Michigan Press; 2003.
30. Tjora AH. Kvalitative forskningsmetoder i praksis. Oslo: Gyldendal Akademisk; 2010.









Comments