Prehospital healthcare personnel are apprehensive about paediatric airway management
The study’s informants were particularly apprehensive about critical emergencies and unsure how to use medical equipment such as bag valve masks.
Background: Research on prehospital work indicates that paediatric airway management is neither straightforward nor simple. The prehospital expertise available in the field is inconsistent, and there is no standardisation of prehospital healthcare competence across the Nordic region.
Objective: To enhance our knowledge about prehospital healthcare personnel’s perceptions of professional and interactive competencies within the service with respect to paediatric airway management.
Method: We employed a qualitative design and conducted three focus group interviews with five, seven and eight informants respectively. They represented eight different ambulance stations and medical centres in Central Norway. Our analysis was based on an inductive approach.
Results: The study demonstrates general apprehension with respect to paediatric airway management, particularly in critical emergencies. The informants also lacked confidence in using medical equipment such as bag valve masks. The informants felt they had received insufficient top-up training and were inadequately prepared for following procedures and for collaborating with other personnel.
Conclusion: The study suggests that there may be a need to enhance competencies in order to optimise the prehospital treatment of children with acute and critical respiratory problems. The informants were looking for high-volume training, internships and simulations in order to maintain their professional and interactive competencies.
Airway obstruction may well be one of the most frequent causes of death in children (1), but acute illness can also bring respiratory problems (2). It is therefore important that prehospital healthcare personnel are proficient in applying techniques that clear the airways of patients (2–4). Prehospital healthcare personnel include paramedics, nurses, ambulance workers and doctors.
In children, the epiglottis is sharper and the larynx is located higher than in adults, and the dimensions are smaller. The techniques, however, are generally the same (4). Several factors can help to prevent undesirable incidents in children; one of them is enhanced knowledge and skills among healthcare personnel.
Cross-professional interaction
Prehospital healthcare personnel have a unique opportunity to prevent undesirable incidents by practising how to deal with serious illness by applying simple, life-saving measures in the acute phase. For anaesthetists, ambulance personnel and doctors to be able to implement life-saving measures and prevent the development of serious illness or complications, they must work to a high professional standard and have the adequate level of professional and interactive competence (5).
Cross-professional interactive skills are required for the treatment of patients to be effective and to achieve a broad platform of competencies (6–8). It is therefore essential that healthcare personnel have the required skills and are familiar with the necessary procedures and equipment for use in emergency situations.
Prehospital work in rural areas
Report to the Storting (white paper) no. 13 (6) makes it clear that there is a growing need for a range of skills within the healthcare sector, yet approximate 30 per cent of workers in the primary health service are unskilled. It is unclear which sectors are represented, and whether the content of this report may put the standard of prehospital work at risk. However, it may be necessary to enhance prehospital competencies, particularly in rural areas.
According to the Official Norwegian Report NOU 2015:17 (9), a shortage of trained healthcare personnel in remote areas may come to represent a challenge to the management of illness and injuries outside of hospital. The Health Directorate’s report on the need for paramedic competence (10) points out that there will be a demand for healthcare personnel with skills across a range of levels, and that there is a need for enhanced competencies in the ambulance service, currently and in the future.
Proficiency requirements
Research confirms that all members of staff are expected to maintain their skills in basic paediatric airway management as well as their familiarity with essential medical equipment such as bag valve masks, medication and intubation (1, 3–4). Emergency healthcare personnel should be proficient in basic airway management and practise implementing the procedures (4, 11).
There is no documentation to suggest that intubation is a life-saving prehospital measure, but there is sufficient documentation to indicate that basic airway management saves lives (11). It is vital that first-aiders feel confident in their work and provide effective life-saving first aid when the minutes count (3). This assertion is supported by Goldmann and Ferson (12), who point out that basic airway management is a first-line treatment and requires ongoing skills training.
Objective of the study
The study’s objective is to enhance our knowledge of prehospital healthcare personnel’s insights into the professional and interactive competencies that are available in the workplace with respect to paediatric airway management.
The research question
‘What is the experience of prehospital healthcare personnel with respect to professional and interactive competencies in acute paediatric airway management in rural areas?’
Method
Design
We have employed a qualitative design in this study. This design is well suited for research that seeks to explore experiences and opinions (13). We made use of focus groups in order to draw on a range of experiences and gain a wider understanding of the topic from the different professions employed by the ambulance service.
Sample
Staff at the Clinic of Emergency Medicine and Prehospital Care and at one municipal Accident and Emergency Department in Central Norway were invited to take part in the study. We selected a random sample of ambulance stations and medical centres. Information letters were sent to the managers of twelve random ambulance stations, three medical centres and the Norwegian air ambulance service.
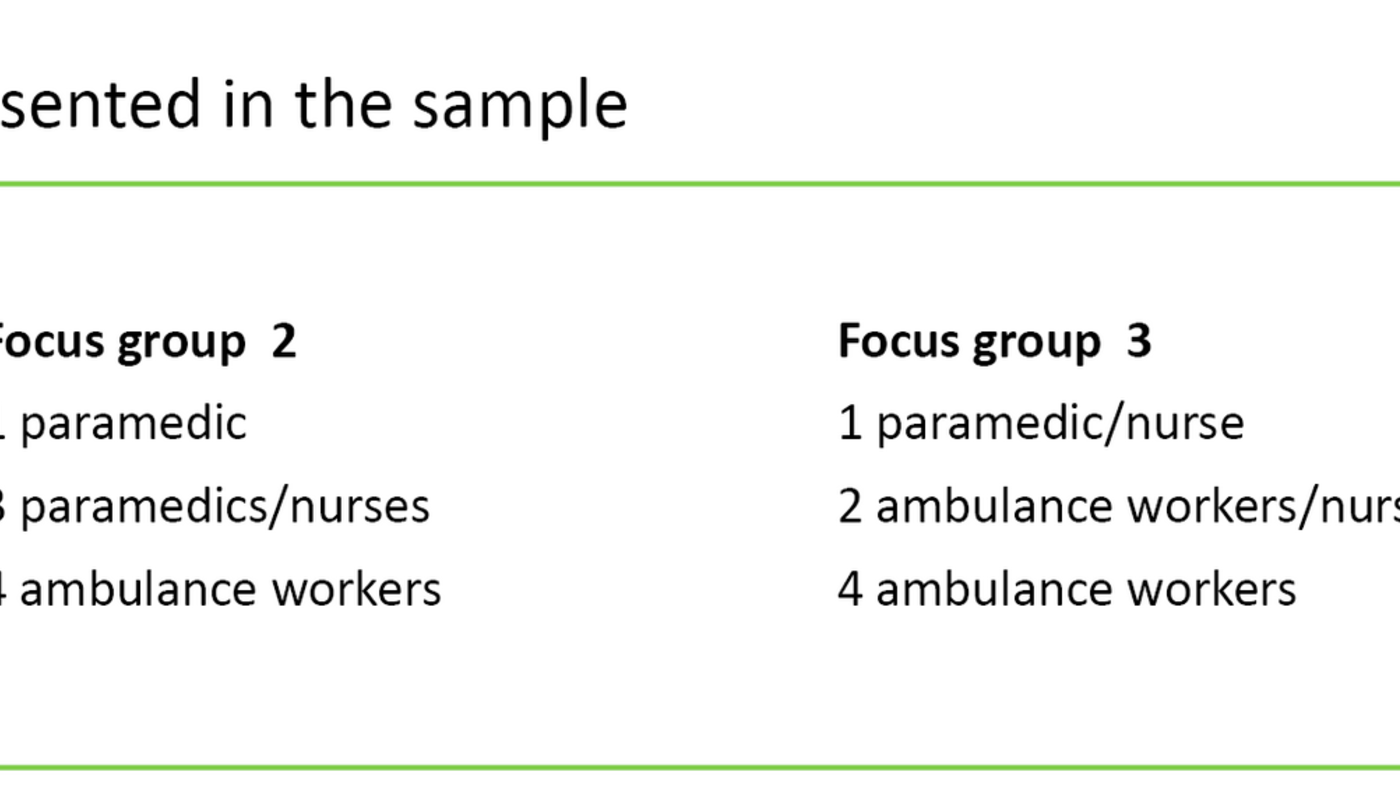
Seven ambulance stations with considerable geographic spread, and one medical centre, enlisted for the study. A total of 25 informants accepted our invitation to take part, but only 20 made themselves available for interview. The informants were from a cross-professional background and between 21 and 49 years of age. Their work experience ranged from 2 to 24 years. Current employment in the prehospital services was the only informant inclusion criterion. Table 1 shows the number of informants included from the various professions.
Data collection
We conducted three focus group interviews in the spring of 2017, involving five, seven and eight informants respectively. We obtained the participants’ consent declarations and mapped their experience, training and age. The interviews were conducted at three different ambulance stations. Interview duration was 30 to 50 minutes, with each interview ending in a concluding summary.
We used a Dictaphone for recording purposes, and the first author transcribed the interviews immediately afterwards. All data were erased at the end of the project. We made use of an interview guide with the following four open-ended questions:
- What competencies do you consider to be important in order to optimise the treatment of children?
- What is your experience of cross-professional collaboration in such circumstances?
- Tell us about your familiarity with or skills in using the technical medical equipment for children.
- Tell us about the sort of courses and practice sessions you have attended in paediatric airway management or in the use of equipment.
Analysis
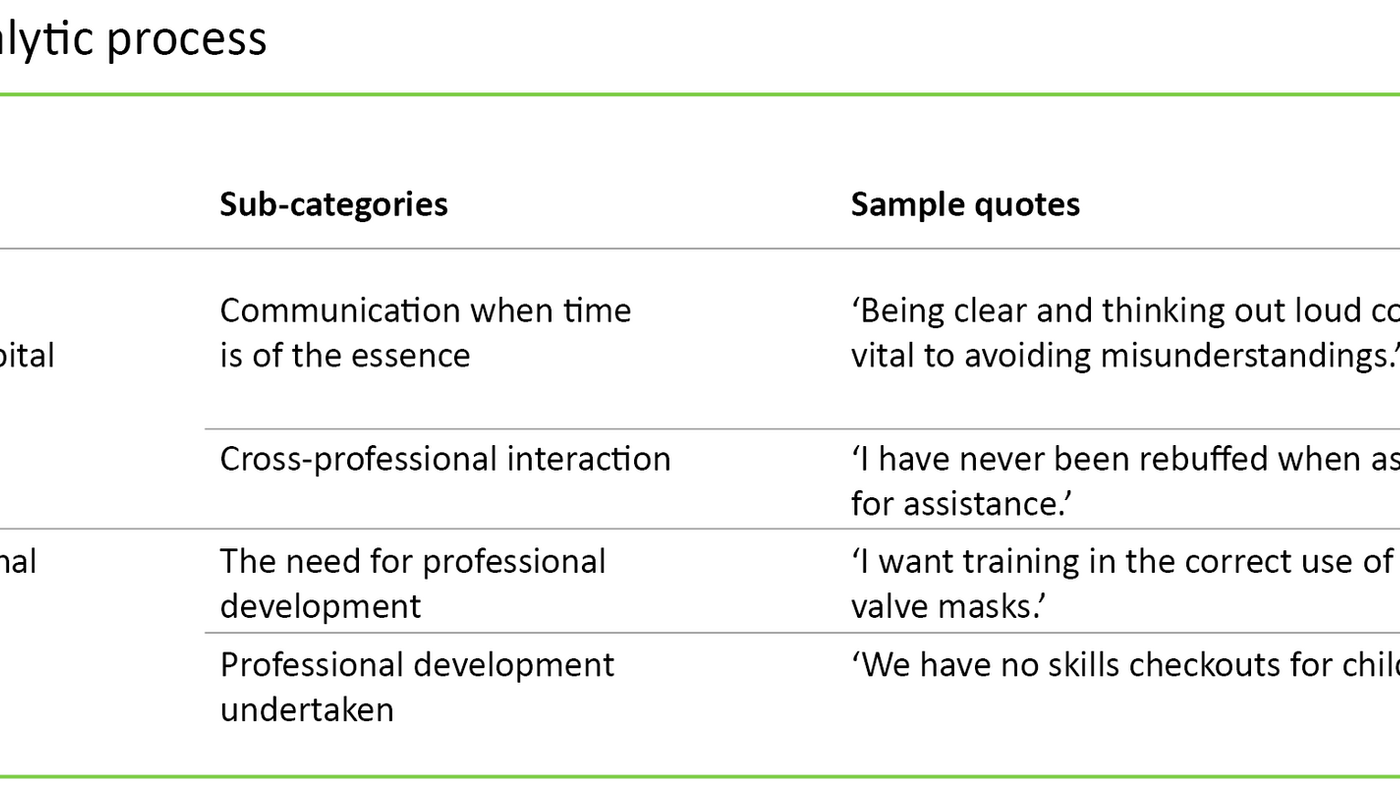
We based our analysis on an inductive approach; the findings became meaningful through a process of interpretation and abstraction (14). Our analysis of the interview transcripts was inspired by Giorgi’s (15) analytic strategy. The first and last authors conducted the analysis without using any computer software. The four stages of the analytic strategy were implemented as follows:
Total impression. Repeated close readings of the transcribed material allowed us to form a total impression.
Identifying meaning units. We divided the text into a number of meaning units, each with a unique colour code.
Abstraction and condensation of the text. This process helped us to develop two meaning units: a) communication and interaction in prehospital work with children, and b) prehospital professional development. Each of the meaning units were then condensed into four sub-categories, two per unit. These were used as headings for our Results chapter.
Synthesising the meaning of the text. Critical conceptualisation of the text highlighted helpful quotes and drew out the essence of the interviews.
Results
Communication and interaction in prehospital work with children
Communication when the minutes count
‘Being clear, and thinking out loud, could be vital to avoiding misunderstandings’, said one informant who received the backing of several others. In their opinion, good communication between prehospital healthcare personnel and other resources, such as the emergency calls service (AMK), the air ambulance service and the accident and emergency department, is essential to ensuring that patients receive good treatment.
They also pointed out that healthcare personnel should be flexible in all emergency situations involving children, because ‘parents often come rushing out and fling their kid into the arms of the first person they see’, in the words of one informant. Several informants pointed out that prehospital personnel cannot therefore be locked into a pre-planned distribution of work. It was also made clear that staff should be imaginative and seek to distract children from the most critical aspects of the situation.
Cross-professional interaction
The informants agreed that good cross-professional collaboration was key to their work, but it was considered to be down to personalities whether this collaboration worked well. They also reported that they could draw on significant assistance from the emergency calls service, the air ambulance service, accident and emergency departments and hospitals, even if they were not in the immediate vicinity.
Several informants reported that their experience with collaborative interaction was good. One of them said: ‘I have never been rebuffed when asking for assistance.’ This informant pointed out that although they have access to all collaborative partners, it is essential that the ambulance personnel are able to work independently.
This independence was essential because the geographic distances involved are vast, and time may be short. Moreover, because many local authorities depend on inter-municipal partnership agreements, there may be no accident and emergency Department available at certain times. Whenever an Accident and Emergency Department is available, this is considered a helpful resource and a confidence boost for the ambulance personnel.
The informants emphasised that doctors have wider experience with children and are therefore more skilled at distinguishing between the healthy and the poorly, and between incidents that carry little risk and those that are potentially serious.
Prehospital professional development
The need for professional development
Some of the informants pointed out that it was impossible for them to learn practical skills by reading about them when there was no opportunity to practise or receive skills training to boost their experience. They said they needed procedural training and added that they wanted internships at hospitals with organised practical skills training. In the words of one of the informants: ‘I want training in the correct use of bag valve masks.’
The informants felt that the individual staff members were given too much responsibility for their own learning. They argued that having to take responsibility for their own learning would lead to considerable individual differences in skill levels.
They went on to point out that they are entitled to have time set aside for professional training during working hours, but that it is left to the individual station manager to decide how much time is earmarked for such training. An internal reference book with clear procedures was a good aid, particularly in emergency situations involving children.
Professional development undertaken
Several informants were concerned that they did not automatically receive feedback once the patient had been transferred to hospital, or that they had no right to see the patient’s records due to confidentiality regulations. The informants maintained that a lack of feedback can be an obstacle to learning from experience and hold back professional development.
Furthermore, several informants emphasised that they should be offered to attend courses and other skills-enhancing programmes, and that several such measures should be made mandatory. ‘Us ambulance workers have completed our online training, and today this is the only re-certification programme available’, said one informant. Several informants were keen to point out that courses and annual skills checkouts had boosted their confidence and improved their skills: ‘Increase the requirements we need to meet and make us better at our job.’
Some informants pointed out that a certain level of baseline knowledge was necessary in order to understand the body’s anatomy and the effect of medication: ‘There is often only one person with medication management authority on duty in the ambulance service. Much of the responsibility is therefore resting on the shoulders of this one person.’ Some of the informants missed having an instructor with specialist expertise: ‘We have no practical checkouts for children.’
Discussion
Handling emergency situations
Several informants mentioned that a lack of confidence in the work situation may be a cause of stress, which is supported by Smith and Roberts (17). They maintain that stress, in turn, can lead to a loss of confidence. Prehospital healthcare personnel should be confident in their work in order to cope with stress in emergency situations. Terrified parents and distressed children who find themselves in a crisis constitute a stress factor for ambulance personnel, according to Bohnström et al. (18).
How ambulance personnel handle stress in emergency situations has also been the subject of studies conducted by LeBlanc et al. (19), who maintain that ambulance personnel often found themselves in highly stressful situations. They also point out that it is necessary to prepare prehospital healthcare personnel for acute stress situations and that an appropriate level of competence is required (19).
Calm communication is important
The informants pointed out that clear, calm, simple and targeted communication, particularly in emergency situations, was essential in order to optimise the treatment. According to Rehn et al. (11), calm dialogue with parents and children makes for a better approach and is more reassuring, thus representing a good investment in the treatment. They go on to point out that communication is a skill that can be acquired through practice.
According to O’Malley et al. (20), there may be communication challenges associated with dealing with terrified parents and frightened children. Information is easily forgotten in a shock phase and should therefore be repeated. Some informants maintained that talking to the child in a pleasant, amiable way can generate calm and trust, which may be the start of an optimal treatment chain.
According to Richardsen (2), and Grønseth and Markestad (21), it can also be reassuring if healthcare personnel explain what is being done to the child. Children generally have a limited capacity to describe discomfort and pain. This challenge increases the need for observation, and observation is essential for correct prioritisations to be made.
Communicating with children
Communicating with children is different to communicating with adults. Healthcare personnel must engage with the child at the child’s own level, using simple words and explanations: calmly and considerately, but in a focused tone of voice and a relaxed posture that signals neither stress nor anxiety. Using the equipment in a creative and playful way may help to establish trust, which in turn enhances communication (22).
The informants gave several examples of things that might help to defuse the situation and distract the child, including the use of a plastic cup rather than a mask in oxygen treatment, inflating rubber gloves, demonstrating on a teddy or using humour and stories.
A conscious choice of words
Levetown (23) asserts that it may be a useful and life-saving approach to choose words and expressions clearly and consciously, and that relatives expect to receive information. The various professions have their own terminology, which is difficult to understand for patients and their relatives. Communication must be adjusted to the receiver, and it is important to be clear in conversation and to use simple words in order to avoid misunderstandings.
According to Aggarwal et al. (24), approximately 70 per cent of incidents are caused by a failure in communication and interaction. This includes communication with colleagues as well as with the child or with parents. LeBlanc et al. (19) emphasise that the most common intervention in emergency medicine is precise communication.
Several informants were keen to see good cross-professional collaboration, and many wanted more training. Team training across professional boundaries can help to improve collaboration (25, 26).
Professional and interactive competencies within the service
Parents whose children suffer from respiratory problems may find the situation extremely distressing. They expect to encounter competent healthcare personnel. It is essential that prehospital healthcare personnel are confident in their work and provide effective, life-saving assistance when the minutes count. Such confidence is in line with the minimum requirements for basic prehospital airway management (3).
In critical situations it is essential that healthcare personnel have sufficient professional and interactive competence (4). An Official Norwegian Report (NOU) (9) points out that health trusts must ensure that staff who provide emergency medical services meet specific requirements and that the trusts are obliged to provide the necessary training and practice. They are also obliged to ensure that all parts of the health service meet a certain set of requirements.
The informants said that feedback was not automatically forthcoming once the patient had been transferred to hospital, largely due to confidentiality regulations. Hospital culture focuses on the patient’s treatment and health in general. Prehospital training is therefore not a key issue in a hospital setting. It is not clear whether confidentiality regulations are in fact the root cause.
The informants claimed that the management fails to provide follow-up skills training, and that there is no skills checkout for children. According to Bjerkelund et al. (4), each individual member of staff is responsible for maintaining their competence and undertaking in-practice skills training. The informants intimated that they wanted an instructor with specialist expertise and were looking for organised training and practice sessions.
Simulations are desirable
Some currently make use of checklists for completed practical training, but it is up to the individual whether the need for further practice and knowledge is followed up. Simulation as an educational method is an alternative to in-practice learning, according to Aggarwal et al. (24). Simulation is appropriate in this context because there are few opportunities to learn by experience, and the level of stress is high.
Smith and Roberts (17) maintain that simulations prevent stress, which is a valuable factor in this line of work. Simulations can help healthcare personnel raise their awareness of their own expertise, strengthen their qualifications and create good, controlled learning scenarios that provide realistic practice.
Simulations can replace real-life situations under guidance and enable reconstructions of recent events. Simulations will therefore be useful for practising and evaluating learnt skills. Healthcare personnel can sit down together to reflect on the treatment provided (19, 25, 27). Simulations are all about becoming competent and ready to implement procedures that are special to a particular profession (26).
Good collaboration depended on personalities
Good clinical competence is essential to be able to work independently and to maintain the patient’s safety (28). The informants felt that they worked well with air ambulance and hospital personnel, and that the cross-professional interaction was good. According to Aggarwal et al. (24), good cross-professional collaboration and management can lead to better independent working.
Several informants expressed the opinion that the standard of collaboration depended on who was on duty. Personal qualities should not be a key factor in emergency interaction. Systematic, shared routines can help prevent patients from receiving different treatment depending on whose shift it is. The pattern of actions in emergency situations must be predictable (9).
The informants found that internal procedures provided a good reference, and that they were easily accessible, updated at all times and useful in the treatment of patients. Jewkes (29) supports the use of written internal procedures and maintains that in the face of limited access to sophisticated equipment and varying competence levels among staff, standards can be improved by good procedures.
Inadequate competence enhancement
The informants were concerned that they often worked independently, but clearly signalled that they needed to be flexible in order to be able to work well with their partner, the doctor, the emergency call service and the hospital. The study also showed that ambulance personnel should boost their professional and interactive competencies, particularly considering the fact that several local authorities have entered into inter-municipal partnerships with respect to their accident and emergency services and that timing conflicts may arise that require them to work without assistance from, for example, the air ambulance service.
It may be necessary to introduce competence-enhancing measures into the education programme. The informants demonstrated clear frustration over the paramedic foundation course, which does not include the testing of skills in paediatric airway management. This suggests that the responsibility for skills training in paediatric airway management may rest with the practice field.
Because specialty training and a postgraduate degree is not a requirement for joining the service, there will be individual differences with respect to professional background. One of the reasons for this discrepancy among ambulance personnel is that vacancies are often advertised without citing specialty or postgraduate education as a minimum requirement. It may be useful to introduce mandatory postgraduate education in this field. The ambulance service often employs nurses, as seen from the sample.
Reflections on methodology
The first author works in the prehospital service and is therefore familiar with the field and the topic of our study. The second and third authors are less familiar with the field. A range of different backgrounds may be a strength for the study because we were able to identify different nuances within the data material. A small sample taken from a single region does not demonstrate breadth of knowledge, so we cannot know with any degree of certainty how prehospital staff in other areas perceive paediatric airway management. Nevertheless, the informants showed engagement and an interest in the questions we asked, which enabled us to collect nuanced data.
The focus group interviews constituted a strength because they facilitated discussion and reflection on the topics, and we felt that the material was sufficiently broad, varied and rich. It may nevertheless have been a weakness that there was a doctor included in only one of the three focus groups, because doctors train to a higher standard and may have acquired better knowledge of the study area. It may have been a strength that the analysis was conducted by two of the authors because the data was examined by more than one person.
Conclusion
The study shows that the informants were apprehensive about the prehospital treatment of children with acute and critical respiratory problems. They were unsure how to use medical equipment, had few opportunities to practise in order to maintain their competence, and their training was inadequate. Children who present with respiratory problems can therefore be a challenge for the prehospital service.
Several informants intimated that professional and interactive competencies were not consistently optimal throughout the emergency medicine chain. They wanted the required training so they would be able to provide health services of a high professional standard and maintain patient safety in emergencies and critical situations. The informants were looking for more high-volume training, internships and simulations in order to maintain their skills and competencies.
References
1. Smith AG, Gardner GH. Policy statement-prevention of choking among children. American Academy of Pediatrics. 2010;125(3):601–7.
2. Richardsen J. Akutt sykdom. Oslo: Gyldendal Undervisning; 2008.
3. Berlac P, Hyldmo PK, Kongstad P, Kurola J, Nakstad AR, Sandberg M. Prehospital airway management: guidelines from a task force from the Scandinavian Society for Anaesthesiology and Intensive Care Medicine. Acta Anaesthesiologica Scandinavia. 2008;52(7):897–902.
4. Bjerkelund CE, Christensen PC, Dragsund S, Aadahl S. Hvordan oppnå fri luftvei? Tidsskrift for Den norske legeforening. 2010;130(5):507–10.
5. Meld. St. nr. 47 (2008–2009). Samhandlingsreformen. Rett behandling – på rett sted – til rett tid. Oslo: Helse- og omsorgsdepartementet; 2009. Available at: https://www.regjeringen.no/contentassets/d4f0e16ad32e4bbd8d8ab5c21445a5dc/no/pdfs/stm200820090047000dddpdfs.pdf(downloaded 12.10.2018).
6. Meld. St. nr. 13 (2011–2012). Utdanning for velferd. Samspill i praksis. Oslo: Kunnskapsdepartementet; 2012. Available at: https://www.regjeringen.no/contentassets/ac91ff2dedee43e1be825fb097d9aa22/no/pdfs/stm201120120013000dddpdfs.pdf(downloaded 12.10.2018).
7. Almås S, Vasset F. Health and social care students pursuing different studies, and their written assignment from workshop and online interprofessional education. Nordic Journal of Nursing Research. 2015;36(3):116–21.
8. Ødegård A, Willumsen E. Tverrprofesjonelt samarbeid: et samfunnsoppdrag. Oslo: Universitetsforlaget; 2014.
9. NOU 2015:17. Først og fremst – Et helhetlig system for håndtering av akutte sykdommer og skader utenfor sykehus. Oslo: Departementenes sikkerhets- og servicesenter, Informasjonsforvaltning; 2015. Available at: https://www.regjeringen.no/contentassets/477c27aa89d645e09ece350eaf93fedf/no/pdfs/nou201520150017000dddpdfs.pdf(downloaded 12.10.2018).
10. Helsedirektoratet. Kompetansebehov i ambulansefag. Rapport fra arbeidsgruppe. IS-0425. Oslo; 2014. Available at: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/134/Kompetansebehov-i-ambulansefag-rapport-fra-arbeidsgruppe-IS-0425.pdf(downloaded 12.10.2018).
11. Rehn M, Hyldmo PK, Magnusson V, Kurola J, Kongstad P, Rognås L, et al. Scandinavian SSAI clinical practice guideline on prehospital airway management. Acta Anaesthesiologica Scandinavia. 2016;60(7):852–64.
12. Goldmann, K, Ferson DZ. Education and training in airway management. Best Practice & Research Clinical Anaesthesiology. 2005;19(4):717–32.
13. Polit D, Beck C. Nursing research. New York: Lippincott Williams and Wilkins; 2017.
14. Malterud K. Kvalitative forskningsmetoder for medisin og helsefag. Oslo: Universitetsforlaget; 2017.
15. Giorgi A. Sketch of a psychological phenomenological method. Phenomenology and psychological research: essays. Pittsburgh, PA: Duquesne University Press; 1985.
16. Helse- og omsorgsdepartementet. Forskrift om organisering av medisinsk og helsefaglig forskning. Oslo; 2009. Available ata: https://www.regjeringen.no/globalassets/upload/hod/hra/helseforskning/forskriftstekst---forskrift-om-organisering-av-medisinsk-og-helsefaglig-forskning.pdf?id=2287758(downloaded 12.10.2018).
17. Smith A, Roberts K. Interventions for post-traumatic stress disorder and psychological distress in emergency ambulance personnel: a review of the literature. Emergency Medicine Journal. 2003;20(1):75–8.
18. Bohnström D, Carlström E, Sjøström N. Managing stress in prehospital care: Strategies used by ambulance nurses. International Emergency Nursing. 2017;32:28–33.
19. LeBlanc VR, Regehr C, Tavares W, Scott AK. The impact of stress on paramedic performance during simulated critical events. Prehospital and Disaster Medicine. 2012;27(4):369–74.
20. O'Malley PJ, Brown K, Krug SE. Patient and family centered care and children in emergency department. Pediatrics. 2008;122(2):511–21.
21. Grønseth R, Markestad T. Pediatri og pediatrisk sykepleie. Bergen: Fagbokforlaget; 2011.
22. Månsson ME. Förberedelser av barn och föräldrar inför undersøkelse eller åtgärd. In: Hallström I, Lindberg T, eds. Pediatrisk omvårdnad. 2. ed. Stockholm: Liber; 2015. p. 123–7.
23. Levetown M. Communicating with children and families: From everyday interactions to skill in conveying distressing information. Pediatrics. 2008;121(5):1441–60.
24. Aggarwal R, Mytton OT, Derbrew M, Hananel D, Heydenburg M, Issenberg B, et al. Training and simulation for patient safety. Qual Saf Health Care. 2010;19(2):34–43.
25. Hagen IH, Molnes SI, Simulering kan gi bedre praksis. Sykepleien. 2013;11:48-50. DOI: 10.4220/sykepleiens.2013.0103.
26. Stangeland S / Universitetet i Stavanger. Simulering redder liv. Intervju med Aase I, Husebø S. Forskning.no; 2011. Available at: https://forskning.no/forebyggende-helse-helsetjeneste-helseadministrasjon-medisinske-metoder-sykepleievitenskap/2011/06(downloaded 12.10.2018).
27. Tosterud R. Simulation used as a learning approach in nursing education. (Doktoravhandling.) Karlstad: Karlstads universitet, Fakulteten för hälsa, natur- och teknikvetenskap; 2015. Available at: http://www.diva-portal.org/smash/get/diva2:760893/fulltext01.pdf(downloaded 12.10.2018).
28. Aase K. Pasientsikkerhet teori og praksis. Oslo: Universitetsforlaget; 2015.
29. Jewkes F. Prehospital emergency care for children. Arch Dis Child. 2001;84(2):103–105.










Comments