Can we trust urine dipsticks?
Urine dispsticks are frequently used in the clinic to diagnose urinary tract infection in elderly patients even though the urine disptick does not distinguish between urinary tract infection and asymptomatic baceriuria.
Background: Urinary tract infection is the most common bacterial infection in the elderly population. Overtreatment among this population is common, partly due to the fact that the differential diagnosis between urinary infection and asymptomatic bacteriuria is difficult. Urine dipstick appears to be a tool widely used in the clinic to diagnose urinary tract infection in the elderly.
Objective: Investigate whether or not urine dipstick is a reliable tool to diagnose urinary tract infection in the elderly patients in nursing homes and home care services.
Method: A systematic literature review approach was adopted. Cinahl, PubMed, Cochrane and Embase databases were used for systematic literature searches in January 2015.
Result: Five of the six studies that we included, showed that neither leukocytes nor nitrite, or a combination of the two, were adequate for sensitivity or specificity for clinical use. A positive urine dipstick has a great chance of being false positive. The average of the positive predictive value in the studies shows 61 percent. However, a negative urine dipstick seems to be more reliable, in which the negative predictive value shows an average of 83 percent.
Conclusion: The literature review shows that urine dipstick does not seem to be an appropriate tool in the diagnosis of urinary tract infection among elderly patients. It has low reliability and it cannot differentiate between a urinary infection and asymptomatic bacteriuria. Despite this, we apparently have no other tool that is better. Nurses have shown to have an important role in urine collection and prescription of antibiotics for urinary tract infection among elderly patients. Therefore, it is important that they know the limitations of the urine dipstick, indications for use of the urine dipstick, and how to interpret the urine dipstick.
The urine dipstick is a tool much used in diagnosing urinary tract infection (UTI) among older adult patients in nursing homes and home care services, but is it reliable? In this literature study we try to answer this question and discuss alternative approaches.
UTI is the most common infection in the elderly population, with the highest prevalence in nursing homes (1). UTI is a collective term for infection in the urinary tracts, and the patient has usually been infected by his or her own colonic bacterial flora. UTI is frequently accompanied by painful symptoms and, in the most serious cases, leads to sepsis and death (2). To initiate treatment of UTI among adult women and men, a medical history is usually sufficient. The most important tool in diagnosing UTI is the examination of a urine sample, but that may be skipped if the symptoms are clear and recognised by the patient based on earlier experience (3).
Difficult to diagnose
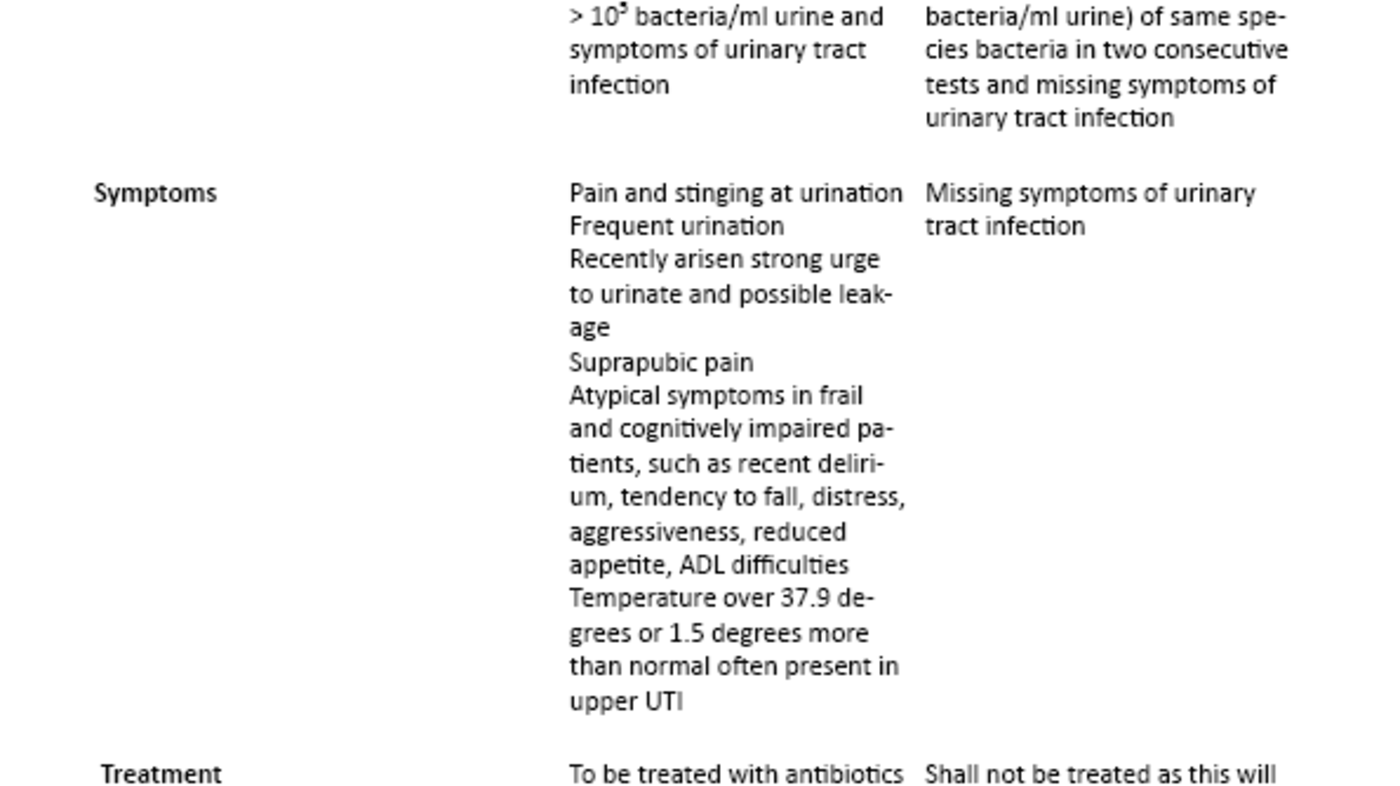
The urine sample collection method must be knowledge based and requires special attention in the case of patients who use incontinence products or urinary catheter (4,5). In the elderly the diagnosis UTI may be difficult to arrive at, as the usual symptoms are not always present. The high proportion of patients with asymptomatic bacteriuria (ASB) (2) further complicates such diagnostics. The prevalence of ASB in nursing homes is estimated at 25-50 per cent for women and 15-40 per cent for men (6). The difference between UTI and ASB is presented in Table 1 (2, 7-10). As opposed to UTI, ASB shall not be treated with antibiotics. Medication side effects are more common among older than younger adults (11), and proper use of antibiotics is therefore necessary to avoid unnecessary side effects, avoid developing antibiotic resistance and to reduce costs (12).
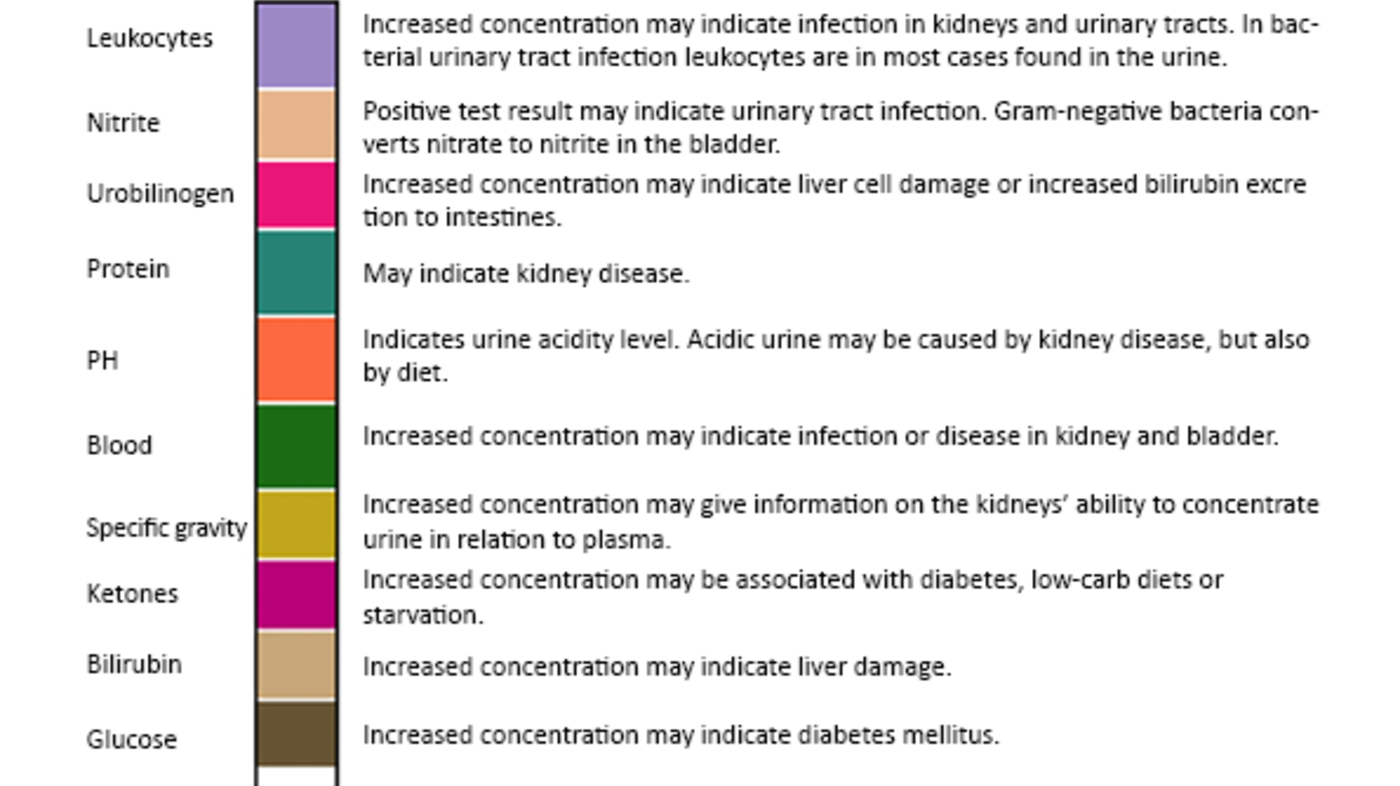
In the care for the elderly today, urine dipsticks are often used when UTI is suspected (2). A urine dipstick is a strip of paper with chemicals added, to be immersed in the urine. The strip will change colour if the urine contains bacteria, blood or sugar (13). Figure 1 describes briefly the significance of various urine strip reactions (4, 14-16). Urine dipstick tests are used at the suspicion of UTI based on the typical UTI symptoms. Urine dipsticks are also commonly used at any change in the condition of the elderly, anything from weeping to increased distress (17).
The urine dipstick was developed to diagnose a.o. UTI. It is easy to use, it is inexpensive, and a tool that yields quick results. Urine dipsticks have been on the market for 25 years and many studies have assessed its accuracy in discovering UTI and bacteriuria in various populations and age groups (18). A urine dipstick can tell us whether there are leukocytes or nitrite in the urine, but it cannot distinguish between UTI and ASB. When we know that ASB is very common among the elderly, using only the urine dipstick to arrive at a diagnosis probably leads to much overtreatment.
Are urine dipsticks reliable?
The literature supports that overtreatment of UTI is a known problem (19). A study showed that when doctors used only the urine dipstick test to diagnose classical lower urinary tract symptoms, 47 per cent of the patients received unnecessary antibiotics, while 11 per cent did not receive proper treatment (20). Most studies on urine dipsticks are, however, done on other population groups than the elderly. When we know that there is a high prevalence of both UTI and ASB in the elderly population, and that it is important to distinguish between the two, it is interesting to study the reliability of urine dipstick tests for elderly patients. The research question for this study was thus the following:
Is the urine dipstick a reliable tool for diagnosing UTI in elderly patients in nursing homes and home care services?
Method
This literature review is based on quantitative primary studies that assess the urine dipstick as a tool in diagnosing urinary tract infection in elderly patients in nursing homes or home care services. The inclusion criteria chosen for the study were that the articles be primary studies, the sample populations patients over 65 years of age, the articles written in English or a Scandinavian language, and the studies addressing the reliability of the urine dipstick as a tool in diagnosing UTI. We did not set any limitations with regard to the articles’ year of publication, as it was important to find all research done on this subject. We performed systematic searches in the databases PubMed, Cinahl, Embase and Cochrane in January 2015. The following search words were used: “urinary tract infection*”, UTI, reagent strip, urine dipstick, dipstick urinalysis, Urine* adj stick* TW, combined with “residential facilities, nursing homes, long term care, homes of the aged, primary care”.
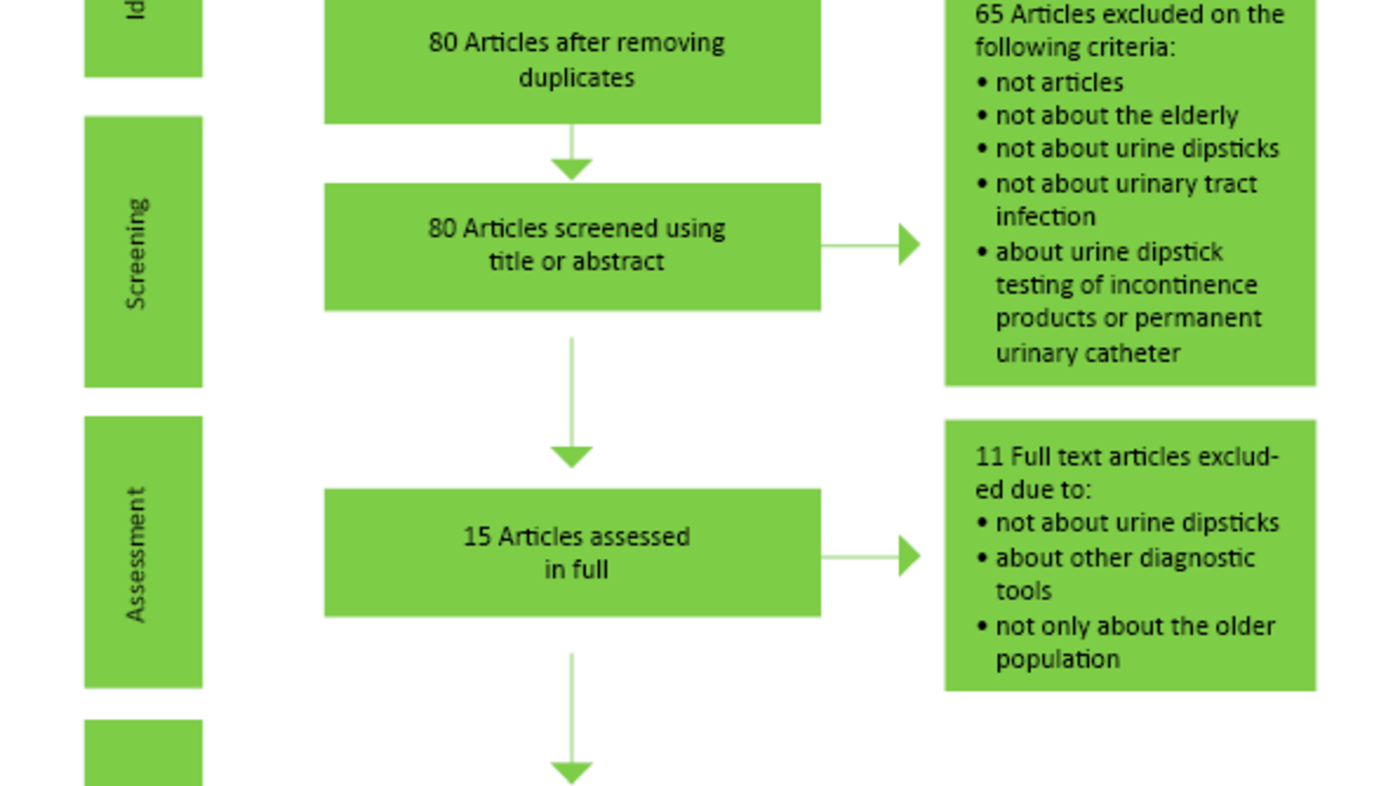
The searches were somewhat different in the different databases due to the different construction of the databases. A filter was finally added so that the articles dealt only with persons over 65 years. We found a total of 100 articles in the various databases, and at a review of the articles 20 duplicates were removed. The remaining 80 articles were screened by reading headings and abstracts. A total of 65 articles were excluded as they turned out not to be research articles, not about the elderly, not about urine dipsticks, not about UTI or were about urine dipstick testing of incontinence products or urinary catheters. A total of 15 articles were read in full, but of these 11 were excluded, as they did not deal with urine dipstick testing, dealt with other tools or did not deal with the elderly population. We went through the reference lists of the articles found, and included another two articles in the study. The flow chart in figure 2 illustrates the search and selection process.
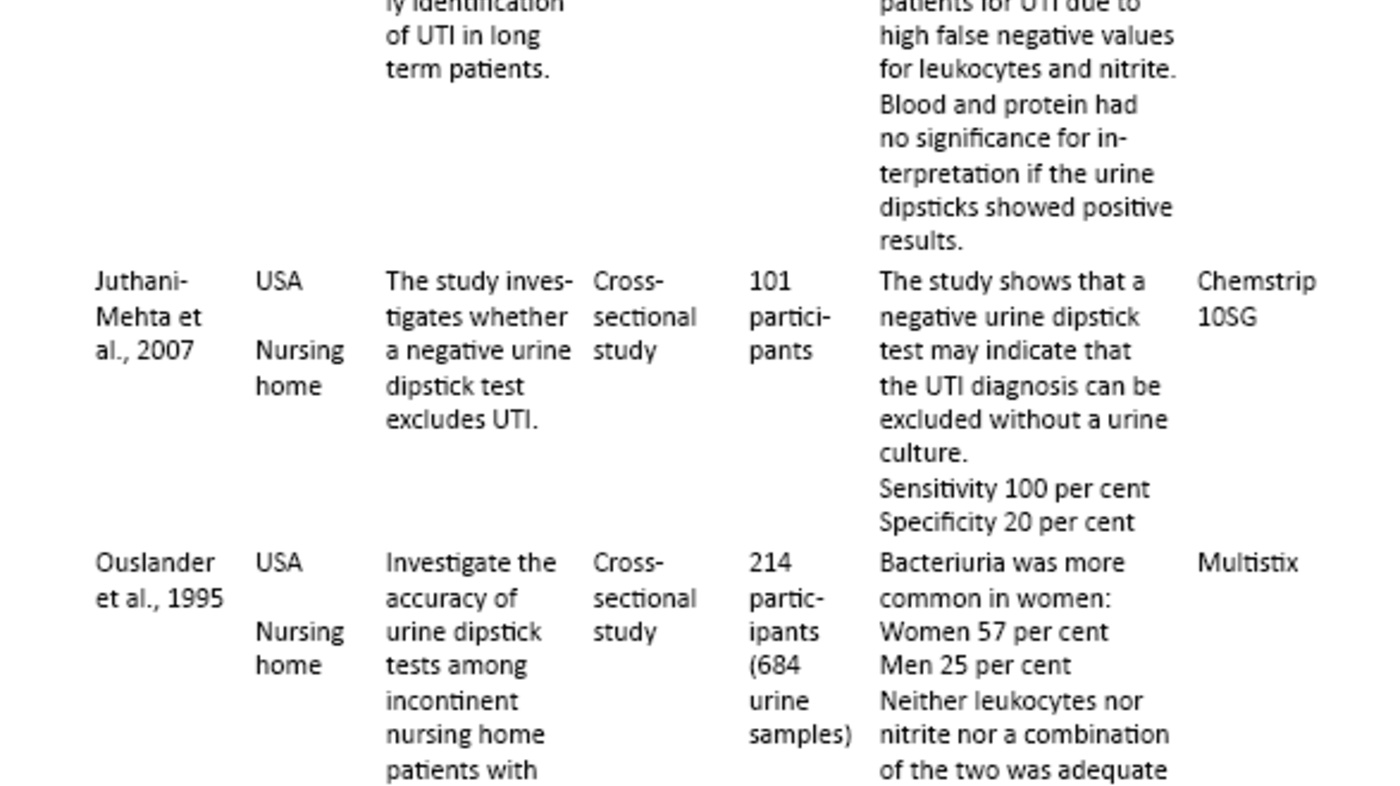
We included six articles in our literature review. We analysed the articles by entering them in a literature matrix (21-26) and assessing them according to the PRISMA criteria (27). We categorised the findings according to the country in which the study was performed, type of urine dipstick used, number of participants, study design, the purpose of the studies and the results of the studies.
Results
The systematic literature search resulted in a review of six articles addressing the reliability of urine dipsticks in diagnosing urinary tract infection in elderly patients. The included studies compare urine dipstick test results and urine culture results for elderly patients. The urine culture is used as a gold standard to assess the accuracy of urine dipsticks. The results from the six included studies are presented in table 2 as a literature matrix of the included studies. The studies look at leukocytes and nitrite as indicators of bacteriuria and assess the urine dipstick’s sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV). Diagnostic sensitivity and specificity indicate the test’s ability to identify healthy and sick individuals in a group, while PPV and NPV indicate the chance of the patient being ill when the test is positive and the chance of the patient not being ill when the test is negative, respectively. The results are presented in per cent so that an error free urine dipstick would show a sensitivity, specificity, PPV and NPV of 100 per cent. Table 3 is a compilation of the results for sensitivity, specificity, PPV and NPV in the included studies (21 – 26).
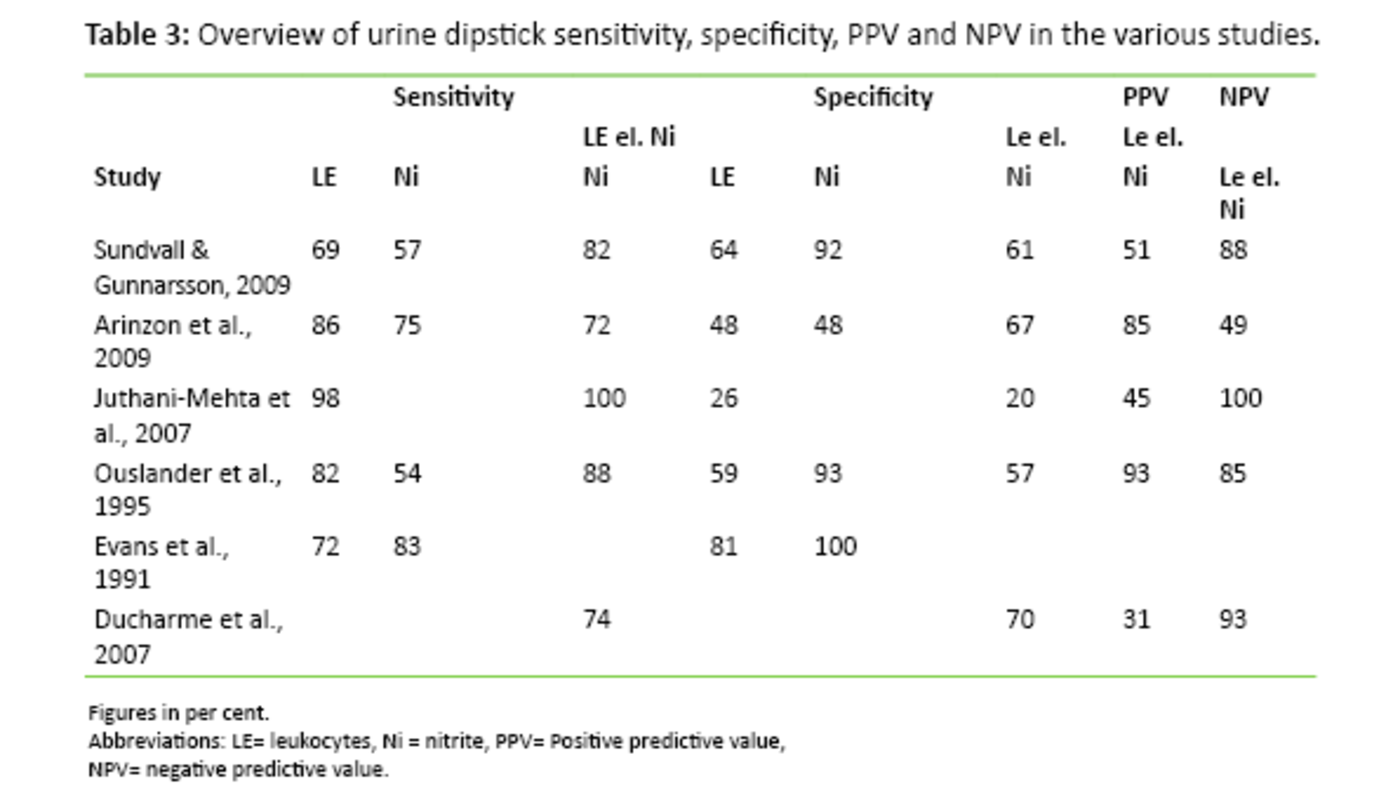
Sensitivity and specificity
Sensitivity indicates the urine dipstick’s ability to discover whether the patient has bacteriuria. Sensitivity varied considerably in the included studies. Juthani-Mehta et al. (23) reported that a urine dipstick that showed presence of nitrite or leukocytes or both, had a sensitivity of 100 per cent. On the other hand, Arinzon et al. (22) reported a sensitivity of 72 per cent. All studies do not report on the sensitivity to nitrite and leukocytes alone, but in the studies that do, the results vary from 69 – 98 per cent on leukocytes and from 54 – 83 per cent on nitrite.
As opposed to sensitivity, specificity is used to describe the urine dipstick’s ability to uncover whether the patient does not have bacteriuria. The specificity varies in the various studies. Juthani-Metha et al. (23) looked at cases where the urine dipstick is positive for leukocytes and nitrite, or for either one. The specificity is then 20 per cent. Ducharme et al.’s Canadian study (26), however, reports a specificity of 70 per cent. When only leukocytes are examined, the specificity is 26 – 81 per cent. Nitrite, on the other hand, has a specificity of 48 – 100 per cent.
Positive predictive value and negative predictive value
Positive predictive value (PPV) and negative predictive value (NPV) tell us about the probability of the urine dipstick giving a correct result. All the studies, except Evans et al. (25), say something about PPV and NPV when both leukocytes and nitrite are present, or when leukocytes or nitrite alone is indicated on the urine dipstick. PPV shows a percentage from 31 – 93 in the various studies, whereas NPV varies from 49 to 100 per cent.
Other relevant findings
All six studies included, except Evans et al. (25), looked at both leukocytes and nitrite as reagents. This indicates that either nitrite or leukocytes were present, or that the urine dipstick reacted to both variables. Several studies also looked at whether there were indications of proteins and blood. With respect to protein and blood, none of the studies showed that these reagents have any significance in establishing bacteriuria if this is indicated on the urine dipstick. Indications of protein and blood are thus not reliable indicators of UTI. Further, Sundvall et al. also compare manual reading of urine dipsticks with an automatic analyzer of the type Clinitek 50. The study shows that the test method does not make a difference, the results are equally good or bad with manual as with automatic reading.
Little research on the subject
UTI is one of the most common bacterial infections in the older population. Nevertheless, UTI is often overdiagnosed and overtreated among the elderly based on unspecific clinical indications and symptoms and a high prevalence among the elderly of ASB (5) that should not be treated, according to clinical guidelines (7, 9, 28). Although a urine dipstick is unable to distinguish between an ASB and a UTI, urine dipsticks are commonly used to diagnose UTI in elderly patients. Urine dipsticks are frequently used in the clinic, and antibiotic treatment may be initiated based on a positive urine dipstick test until a urine culture result is available (26). As urine dipsticks appear to be much used in the clinic and the results of urine dipstick tests have a crucial role in diagnosing UTI in the elderly, it is interesting to see how reliable urine dipsticks are. The purpose of this literature study was to assess the reliability of urine dipsticks in diagnosing UTI in elderly patients in nursing homes and home care services. In spite of extensive and systematic literature search, we found only six research articles dealing with this subject. This low number makes one wonder, considering the widespread use of urine dipsticks.
Much research is done on urine dipsticks in other populations such as children, working adults and predominantly on women. These studies give various results depending on age group and patient criteria (21). Much research is done on pregnant women as a group, and in this population urine dipsticks are recommended used to discover bacteriuria (18). There is, however, not much research on the combination of elderly and the use of urine dipsticks; this is supported by Bevridge et al. (5). This literature study is therefore an important contribution to knowledge on the use of urine dipsticks in a population much plagued with UTI, but with a high prevalence of ASB.
Using urine dipsticks in the clinic
When the general condition or behaviour of an elderly patient changes today, UTI is generally the first suspect. A urine dipstick is a simple, inexpensive and non-invasive tool for confirming or excluding whether a patient has UTI, and is therefore frequently used. If a urine dipstick proves positive for nitrite and leukocytes, common practice is to contact a physician (17), oftentimes by telephone, and antibiotics are prescribed (29).
The widespread use of urine dipstick tests in Norway is not surprising. Norwegian guidelines for prescription of antibiotics in the primary health services (7) state that testing for leukocytes and nitrite on a urine test strip may help establish whether an infection is present. The guidelines also state that microscopy of the urine will not yield any additional information to the use of urine dipsticks, that leukocytes have good test value (sensitivity and specificity are around 85 per cent), and that a positive nitrite test corresponds with gram-negative strings when the urine has remained four hours in the urine bladder (specificity 96 per cent) (7). In other words, Norwegian guidelines have great faith in urine dipsticks as a diagnostic tool.
Nurses have a central role
One study shows that doctors often choose to prescribe antibiotics on the basis of a positive urine dipstick test until a culture is available (30). This approach has, however, turned out to have a margin of error of 20 to 40 per cent. Such erroneous diagnoses are very unfortunate as treating older adults with antibiotics may lead to the development of resistance and unwanted side effects. In worst case it may keep one from discovering other, underlying, causes of the patients’ symptoms (2, 10).
The nurse has proved to have a central role in diagnosing UTI in the elderly. The nurse observes the patients’ condition and symptoms on a daily basis, prescribes the urine culture, uses the urine dipstick and influences the initiation of antibiotics (17). That is why it is important that nurses have knowledge on UTI in the elderly, so that they may make the correct assessments. Part of this assessment is to be able to interpret and know the limitations of the urine dipstick.
Is the urine dipstick a reliable tool?
The more recent studies included in this literature review (21 – 23, 26) emphasise that the urine dipstick is not a good enough tool in confirming bacteriuria in elderly patients. The studies point to results with many false positives and with low sensitivity and specificity, i.e. urine dipsticks are not reliable in distinguishing between health and illness with regard to UTI. Duchrame et al. (26) found that 61 per cent of patients with a positive urine dipstick test did not have bacteriuria according to the urine culture. Sundvall et al. (21) showed that with a positive urine dipstick test the probability of bacteriuria is just 51 – 73 per cent.
Deville et al. (31) have done a meta-analysis where they conclude that urine dipsticks alone may be useful in all populations to exclude the presence of infection when there are no positive findings of nitrite or leukocytes. Even if this meta-analysis is based on a small number of articles on the elderly, the findings correspond well with the findings in the articles included in our literature review. The studies included have a NPV from 88-100 per cent with the exception of the Arinzon et al. study (22), which has a NPV of 49 per cent. This indicates that the urine dipstick is not a very reliable tool for establishing UTI, but that it is more reliable for excluding UTI in elderly patients.
No better tools
Even if the urine dipstick is not very reliable in diagnosing UTI in the elderly, we have not so far found a better tool. A series of studies have been done to assess the reliability of other tools in diagnosing UTI. The McGeer criteria and the Loeb criteria are both short check lists for diagnosing UTI with the help of clinical signs such as rising temperature, burning pain at urination, frequent urination, suprapubic pain, change of character of urine, throbbing tenderness over kidneys, visible blood in the urine, urine incontinence and deterioration of mental condition (8, 32). Juthani-Mehta et al. did a study in 2007 where they assessed whether nursing home patients with suspected UTI met the Loeb or McGeer criteria, and whether they were in line with the laboratory results (33). Here the McGeer criteria turned out to have a sensitivity of 30 per cent, specificity of 82 per cent, PPV of 57 per cent and NPV of 61 per cent. The Loeb criteria showed almost the same results – that is, not very high reliability in diagnosing UTI.
Juthani-Mehta et al. (34) did a study where they identified clinical signs in connection with bacteriuria and pyuria (white blood cells in the urine) in nursing home patients with suspected UTI. They showed that dysuria (painful urination), change in character of urine and change in mental condition were related to bacteriuria combined with pyuria, but this study gave no better results than diagnosis with urine dipsticks.
Sundvall et al. (35) studied whether higher concentration of Interleukin-6 in the urine could indicate whether the patient had UTI with non-specific symptoms. Interleukin-6 is a mediator for infection and plays an important role in the regulation of the immune system. The substance can be examined with a urine analysis. This study showed that neither increased concentration of Interleukin-6 in the urine or the use of urine dipsticks is suitable as indicator of unspecific symptoms and bacteria in the urine in the elderly population.
Implications for practice
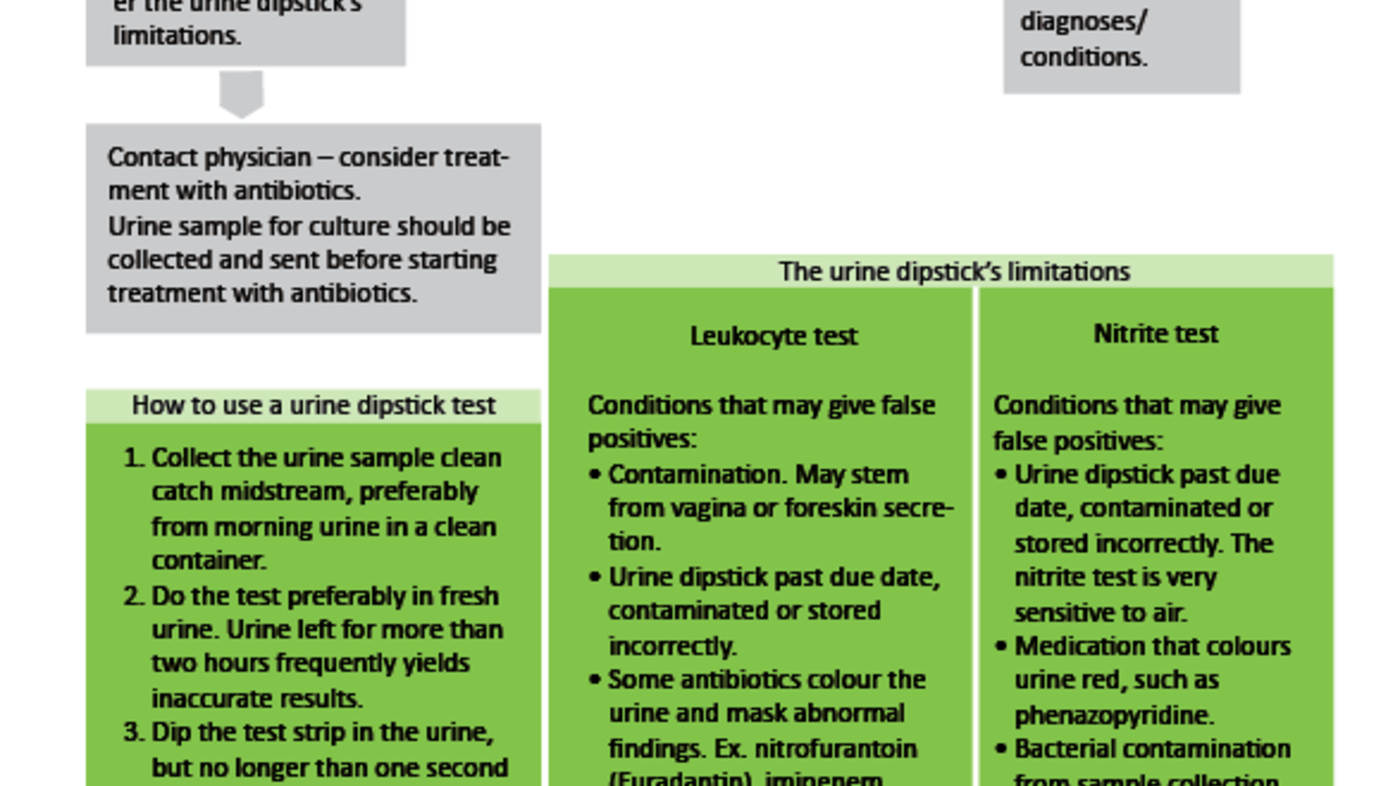
As mentioned, the urine dipstick is a quick, non-invasive and inexpensive tool, but apparently not very reliable. As we do not seem to have any other, better, tool, it may be appropriate to continue using the urine dipstick, given that the method is used properly and interpreted correctly. The nurse must know the limitations of the urine dipstick.
In Figure 3 (4, 7-10, 13-16, 36) we attempt to give an overview of the urine dipstick’s limitations with regard to the factors that may give false positives and false negative answers. Such knowledge will be of great value to the nurse in assessing the reliability of a urine dipstick result. Figure 3 may also be used as a clinical guide for when to use urine dipsticks and how to proceed after having collected the urine sample.
Strengths and weaknesses
This literature review’s greatest weakness is that it is based on merely six articles as little research has been done on elderly patients and the reliability of urine dipsticks. It is therefore difficult to draw any major conclusions. All studies included are published in large and acknowledged peer-reviewed journals that vouch for the quality of the research. We will, however, note that in the oldest study included the description of its methodological process was rather weak.
One strength of our study is that the included studies use only two types of urine dipsticks: the brands Multistix from Bayer or Chemstrip from Roche. The studies are further uniform in that they have used urine culture results as the gold standard, and all have used the same limit of > 105 bacteria/ml urine as significant bacteriuria. This strengthens the comparisons made in this literature review. The findings of the various studies can very likely be transferred to Norwegian conditions. The studies are performed in six different countries. The largest study is done in Sweden, a country we may compare ourselves with regarding the structure of the care for the elderly and the older population. In all the studies reviewed, the urine samples were cultured. There it was established that the bacteria findings were similar and corresponded with the literature in the field.
Conclusion
The urine dipstick does not appear to be an appropriate tool for diagnosing UTI in the elderly as it is not very reliable and cannot distinguish between a UTI and an ASB. We do not, however, seem to have any other better tool. Nurses have proved to have an important role in urine sample administration, use of urine dipsticks and initiation of antibiotic treatment for UTI in elderly patients. It is therefore important that nurses know the limitations of a urine dipstick test and indications for use. They also need to know how to interpret the urine dipstick. Urinary tract infection is very common among elderly in nursing homes and home care services, but due to difficulties in diagnosing this population group, there is great overtreatment with antibiotics. Such overtreatment is unwanted, as it leads to development of resistance, unwanted side effects and increased costs. Further research on differential diagnostics between UTI and ASB will be crucial in the future.
References
1. Omli R, Skotnes LH, Mykletun A, Bakke AM, Kuhry E. Residual urine as a risk factor for lower urinary tract infection: A 1-year follow-up study in nursing homes. J Am Geriatr Soc. 2008;56(5):871–74.
2. Wyller TB. Geriatri : en medisinsk lærebok. Oslo: Gyldendal Akademisk; 2011.
3. Hunskår S, Brekke M, Hjortdahl P, Holtedahl K, Sandvik H, Smith-Sivertsen T. Allmennmedisin. Oslo: Gyldendal Norsk Forlag; 2013.
4. Willacy H, Henderson R, Bonsall A. Urine dipstick analysis. Patient 2014–2015. Available from: http://www.patient.co.uk/doctor/urine-dipstick-analysis(Downloaded 14.04.2015).
5. Bevridge LA, Davey PG, Phillips G, McMurdo ME. Optimal management of urinary tract infections in older people. Clinical Interventions in Aging. 2011;6:173–80.
6. Sundvall PD, Ulleryd P, Gunnarsson RK. Urine culture doubtful in determining etiology of diffuse symptoms among elderly individuals: a cross-sectional study of 32 nursing homes. BMC Fam Pract. 2011;12:36.
7. Helsedirektoratet. Antibiotikabruk i primærhelsetjenesten. Nasjonal faglig retningslinje for antibiotikabruk i primærhelsetjenesten. Available from: https://helsedirektoratet.no/retningslinjer/nasjonal-faglig-retningslinje-for-antibiotikabruk-i-primerhelsetjenesten(Downloaded 08.08.2016).
8. Rowe TA, Juthani-Mehta M. Diagnosis and management of urinary tract infection in older adults. Infect Dis Clin North Am. 2014;28(1):75–89.
9. Fekete T, Hooton TM, Calderwood SB, Bloom A. Approach to the adult with asymptomatic bacteriuria 2015. Available from: http://www.uptodate.com/contents/approach-to-the-adult-with-asymptomatic-bacteriuria(Downloaded 01.05.2015).
10. Mody L, Juthani-Mehta M. Urinary tract infections in older women: a clinical review. Jama. 2014;311(8):844–54.
11. Knudsen J, Frimodt-Møller N. Ældre får flere bivirkninger og mere resistensudvikling af antibiotika. Ugeskr Læger 2013;175:2854–7.
12. Tobiassen T, Berild D, Hjortdahl P. Bruk av systemiske antibiotika ved et norsk sykehjem. Tidsskr Nor Laegeforen. 2002;122(24):2376–8. Available from: http://tidsskriftet.no/article/606500/(Downloaded 08.08.2016).
13. Roche. Compendium of urinalysis: Urine test strips and microscopy 2010. Available from: http://www.cobas.com/content/dam/cobas_com/pdf/product/urinalysis-compendium.pdf (Downloaded 20.04.2015).
14. Simerville JA, Maxted WC, Pahira JJ. Urinalysis: a comprehensive review. Am Fam Physician. 2005;71(6):1153–62.
15. Wilson LA. Urinanalysis. Nurs Stand. 2005;19(35):51–4.
16. Hegdal SM, Brønstad G, Kümmel A. Informasjon fra Avdeling for laboratoriemedisin (ALM) 2013. Available from: https://ekstranett.helse-midt.no/Samhandling/hnt/lab-nytt/Labnytt/Lab-nytt%202005-2013.pdf (Downloaded 02.09.2016).
17. Walker S, McGeer A, Simor AE, Armstrong-Evans M, Loeb M. Why are antibiotics prescribed for asymptomatic bacteriuria in institutionalized elderly people? A qualitative study of physicians' and nurses' perceptions. Canadian Medical Association Journal. 2000;163:273–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10951723(Downloaded 08.08.2016).
18. Krogsboll LT, Jorgensen KJ, Gotzsche PC. Screening with urinary dipsticks for reducing morbidity and mortality. Cochrane Database Syst Rev. 2015;1:CD010007.
19. Loeb M, Brazil K, Lohfeld L, McGeer A, Simor A, Stevenson K et al. Effect of a multifaceted intervention on number of antimicrobial prescriptions for suspected urinary tract infections in residents of nursing homes: cluster randomised controlled trial. BMJ. 2005;331(7518):669. Available from: http://www.bmj.com/content/331/7518/669(Downloaded 08.08.2016).
20. Lammers RL, Gibson S, Kovacs D, Sears W, Strachan G. Comparison of test characteristics of urine dipstick and urinalysis at various test cut- off points. Ann Emerg Med. 2001;38:505-12. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11679861(Downloaded 08.08.2016).
21. Sundvall PD, Gunnarsson RK. Evaluation of dipstick analysis among elderly residents to detect bacteriuria: a cross-sectional study in 32 nursing homes. BMC geriatr. 2009;9:32.
22. Arinzon Z, Peisakh A, Shuval I, Shabat S, Berner YN. Detection of urinary tract infection (UTI) in long-term care setting: Is the multireagent strip an adequate diagnostic tool? Arch Gerontol Geriatr. 2009;48(2):227–31.
23. Juthani-Mehta M, Tinetti M, Perrelli E, Towle V, Quagliarello V. Role of dipstick testing in the evaluation of urinary tract infection in nursing home residents. Infect Control Hosp Epidemiol. 2007;28(7):889–91.
24. Ouslander JG, Schapira M, Fingold S, Schnelle J. Accuracy of rapid urine screening tests among incontinent nursing home residents with asymptomatic bacteriuria. J Am Geriatr Soc. 1995;43(7):772–5.
25. Evans PJ, Leaker BR, McNabb WR, Lewis RR. Accuracy of reagent strip testing for urinary tract infection in the elderly. Journal of the Royal Society of Medicine. 1991;84(10):598–9.
26. Ducharme J, Neilson S, Ginn JL. Can urine cultures and reagent test strips be used to diagnose urinary tract infection in elderly emergency department patients without focal urinary symptoms? CJEM, Can. 2007;9(2):87–92.
27. Prisma. Preferred Reporting Items for Systematic Reviews and Meta-Analyses. Available from: http://www.prisma-statement.org/(Downloaded 08.08.2016).
28. High K, Schmader KE, Sokol HN. Evaluation of infection in the older adult 2014. Available from: http://www.uptodate.com/contents/evaluation-of-infection-in-the-older-adult?source=search_result&search=infection+elderly&selectedTitle=1%7E13#H1498008(Downloaded 08.08.2016).
29. Pettersson E, Vernby A, Molstad S, Lundborg CS. Infections and antibiotic prescribing in Swedish nursing homes: a cross-sectional study. Scand J Infect Dis. 2008;40(5):393–8.
30. Ackermann RJ, Monroe PW. Bacteremic urinary tract infection in older people. J Am Geriatr Soc. 1996;44(8):927–33. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8708302(Downloaded 08.08.2016).
31. Deville WL, Yzermans JC, van Duijn NP, Bezemer PD, van der Windt DA, Bouter LM. The urine dipstick test useful to rule out infections. A meta-analysis of the accuracy. BMC Urol. 2004;4(4).
32. Liu LM. UTIs in nursing home residents. Advance healthcare network 2015. Available from: http://nurse-practitioners-and-physician-assistants.advanceweb.com/Archives/Article-Archives/UTIs-in-Nursing-Home-Residents.aspx(Downloaded 26.04.2015).
33. Juthani-Mehta M, Tinetti M, Perrelli E, Towle V, Quagliarello V. Diagnostic accuracy of criteria for urinary tract infection in a cohort of nursing home residents. J Am Geriatr Soc. 2007;55(7):1072–77.
34. Juthani-Mehta M, Quagliarello V, Perrelli E, Towle V, Van Ness PH, Tinetti M. Clinical features to identify urinary tract infection in nursing home residents: a cohort study. J Am Geriatr Soc. 2009;57(6):963–70.
35. Sundvall PD, Elm M, Ulleryd P, Molstad S, Rodhe N, Jonsson L et al. Interleukin-6 concentrations in the urine and dipstick analyses were related to bacteriuria but not symptoms in the elderly: a cross sectional study of 421 nursing home residents. BMC Geriatr. 2014;14:88.
36. Midthun S, Paur R, Bruce AW, Midthun P. Urinary tract infections in the elderly: A survey of physicians and nurses. Geriatr Nurs. 2005;26:245–51.









Comments