Home health care services in collaboration with the specialist health care services
Different perspectives on what to prioritise, characterise the cooperation.
Bakgrunn: Samhandling mellom aktører i spesialist- og kommunehelsetjenesten om pasienter som skrives ut fra sykehus har vært en utfordring. Ett av målene med tiltakene i samhandlingsreformen er at denne samhandlingen skal bedres.
Hensikt: I denne studien har vi sett på samhandlingen mellom aktørene i spesialist- og kommunehelsetjenesten. Hensikten var å få kunnskap om hvordan sykepleierne i hjemmesykepleien opplever at samhandlingen fungerer når pasienter skrives ut fra sykehus, to og et halvt år etter innføringen av samhandlingsreformen.
Metode: En kvalitativ studie med individuelle dybdeintervju av sju sykepleiere i hjemmesykepleien ble gjennomført sommeren 2014. Datamateriale ble analysert og fortolket etter fenomenologisk-hermeneutisk metode.
Resultat: Sykepleierne beskriver at samhandlingen om pasienter med kreft fungerer godt. Samhandlingen om andre pasienter er imidlertid utfordrende. Samhandlingen er preget av ulike perspektiver på hva som skal tillegges vekt. Sykepleierne i hjemmesykepleien opplever også å ha begrenset makt og innflytelse samt at informasjonsflyten er begrenset.
Konklusjon: Samhandlingen mellom helsepersonell på sykehus og hjemmesykepleie om pasienter som skrives ut fra sykehus fungerer ikke etter hensikten. Dette ser ut til å ha sammenheng med skjev maktfordeling mellom
aktørene og at det ikke er etablert en felles forståelse av hva de skal samhandle om, og hvordan. Bedring krever organisatoriske endringer slik at maktrelasjonen mellom aktørene balanseres. I tillegg må aktørene utvikle kunnskap, vilje og evne til å samarbeide på
tvers av organisatoriske enheter.
Introduction
According to Report No. 47 to the Storting – the Coordination Reform (hereafter called the reform) – improved coordination is one of the health care services’ most important areas of development. Coordination is emphasised as central to achieving the goal of continuous and cohesive health services to the patients (1). The reform describes the coordination of specialist and municipal health care services as particularly challenging. Studies show, a.o., that the follow-up of patients in the transition from hospital to home health care has proven particularly difficult (2-9). In order to establish a more cohesive patient trajectory many municipalities have introduced various forms of the purchaser-provider model. Studies show, however, that collaboration between health personnel is unsystematic and incomplete with regard to the assessment of patients’ level of functioning and need of assistance, and that documentation accompanying patients is unsatisfactory (3-8). The reform measures introduced in January 2012 thus have as their goal to improve collaboration between the actors. In this article we present a study of how nurses in home health care services experience collaborationwith health personnel in the specialist health care services two and a half years after the introduction of the reform. We shed light on the collaboration between the actors by focusing on the challenges that arise when patients are discharged from hospital and transferred to home health care services. The purpose of the article is to develop knowledge regarding challenges that arise in the collaboration and how such challenges are met.
Background
Coordination is “ health care services’ ability to divide tasks between services in order to reach a common, agreed-upon goal, and the ability to perform the tasks in a coordinated and rational manner “ (1 p.13). According to Orvik (10), such collaboration obligates and carries a legal and ethical imperative entailing that the actors shall act jointly in concrete situationsso that patients and family experience continuity in services and measures. Coordination thus demands mutual adjustment of the parties’ tasks, a common understanding of the situation and of the necessity for collaboration. Collaboration and cooperation are central to coordination (2,10). Collaboration is described as a positive attitude between actors leading to informal contact without a necessary presence of a strong degree of obligation to concrete actions (10). Coordination is about formalising measures, either within the individual organisation or between organisations, in order to solve certain tasks and realise common goals. Coordination demands decisions at a system level (10).
In Report No. 47 to the Storting (1) the challenges relating to the collaboration between the specialist health care services and the municipalities are attributed, a.o., to that health care providers and municipalities are regulated by different laws and have different payment structures and incentives. Further, the aim of the specialist health care services is curative while the municipal health care services emphasise the patient’s level of functioning and coping ability. The report to the Storting also lists as a coordination problem that patients ready to be discharged occupy a significant number of bed days in hospitals. The reform has therefore had as a goal the implementation of system measures to support collaboration when the patient’s need of services is at odds with administrative levels or organisational boundaries. The reform’s major move has been to transfer tasks and responsibility from specialist health care services to municipal health care services. Measures implemented to meet the shifting of tasks and responsibilities to the municipalities are among others: Requirement of “collaboration agreements” between the parties, municipal payment for bed days in hospital for patients who are defined as ready for discharge, and the creation of positions for coordinators of collaboration in the regional health authorities (1,11,12).
Coordination statistics for 2013-2014 show that the incentive of municipal payment has contributed to a significant reduction in the number of bed days for patients ready for discharge (13,14). The number of patients that the municipalities must serve has risen, and the patients discharged are sicker than before (13-21). The municipalities’ new responsibilities are thus, to a great extent, about treatment related tasks and caring for patients in a very vulnerable phase (13,16,17,20). This entails an increased pressure on municipal services, and home health care services in particular, especially in the municipalities that have a shortage of short-term placements (16,18). Organising the services according to a purchaser-provider model also appears to limit the possibilities for meeting older patients’ needs for treatment and care (15). Concern for whether the municipal follow-up services of patients are satisfactory has been voiced (13,16,17,19,20). It remains unclear whether the coordination of hospital and municipalities regarding the individual patient has improved after the implementation of the reform measures (13,19,29).
Method and material
In line with the purpose of the study, we chose a qualitative design (22,23). The snowball method was used to gain access to informants with experience from collaborating with actors in the specialist care services. Through social networks we gained information on potential informants whom we contacted. These informants directed us to other nurses in the home health care services who collaborate with the specialist health care services. We used semi-structured in-depth interviews as data collection method (22,23). Seven nurses distributed on one rural municipality and one urban municipality within the same regional health authority were interviewed. Four nurses worked with providing services directly to the patients. Three nurses were administrative leaders responsible for planning the services and receiving patients from the hospital. We chose to interview nurses with both clinical and administrative responsibilities. We assumed that with a variety of responsibilities in the home health care services they might have a variety of experiences on collaborating with the specialist health services. In the interviews we emphasised bringing out the nurses’ descriptions of how the collaboration with the hospitals, regarding patients ready to be discharged into home health care services, works after the implementation of the reform. To ensure the quality of the data we frequently rephrased the informants’ statements as questions. This was done to ensure that we had understood what the informants wanted to communicate (23). The interviews were carried out during the summer of 2014 by two researchers, and lasted from one to one and a half hours. The interviews were recorded and transcribed.
Analysis
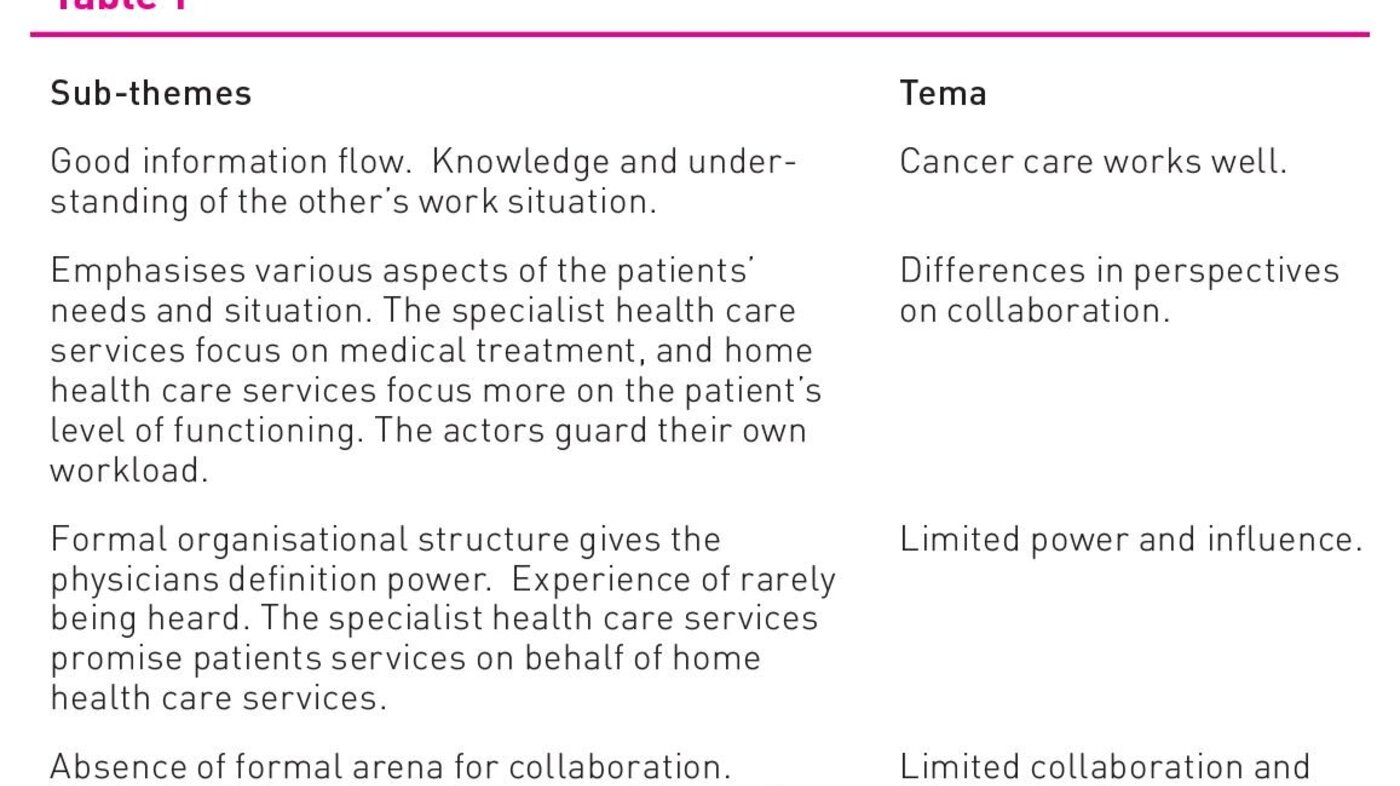
The data were analysed and interpreted using a phenomenological hermeneutic approach (23). We performed meaning condensation and generated units of meaning; this was not a linear process, but an interpretive meandering between raw data, potential sub-themes, and themes. Quotes regarding challenges in the collaboration were first marked and possible sub-themes noted in the margins. Next, we made a summary of each individual interview, quotes were gathered in sub-themes, and potential themes were developed in parallel. Then sub-themes and themes from all the summaries were viewed crosswise. This entailed bringing out, through analysis, common sub-themes and themes and removing superfluous material. It emerged early on that collaboration on cancer patient was a theme that stood out, as this collaboration seemed to work quite well. Collaboration on other patients who were to be transferred to home health services was, however, described as problematic. The problem related to the actors’ differences in perspectives on what to emphasise in such collaboration. Home health nurses also consider it a problem that they have limited power and influence in the coordination effort and that there is limited collaboration and flow of information between the actors. The table below illustrates the analysis from sub-theme to theme.
After developing the themes we analysed the interviews one more time to ensure the validity of the study (23). The analysis of the interviews showed that the nurses’ experiences with collaborating with actors in the specialist health care services were more or less identical. Consequently, we do not distinguish between informants with administrative and clinical responsibilities in the presentation of the data and in the discussion.
Ethical Considerations
An information memo and invitation to participate in the project were sent to the administration of the home health care services in two municipalities who then recruited informants. The participants gave written informed consent and they were notified that they could withdraw from the study at any time, which nobody did. The study was approved by The Norwegian Centre for Research Data. Personal, identifiable information was anonymised in the transcription. The data are stored in accordance with current regulations.
Results
In the following, the thematic findings of the study are presented, and sub-themes appear implicitly through the informants’ statements.
Cancer care works
According to the nurses, collaboration with the hospital works well in the case of cancer patients. The nurses state that the hospital has a professionally strong team that is easy to contact, and that they “think about everything” when a patient is discharged into the care of home health services. One informant explains why this works: “It is everything. From the ordering of supplies to all the equipment we are expected to need for medication. When we have general questions they are very easy to reach and very service minded. Both to us and the patients.”
Another informant says: “The collaboration depends on the people at the hospital knowing the municipality the patient is going into, and on whom we meet (in the specialist health care services). Palliation has worked really well.” Here the nurses emphasise that a good flow of information is crucial to the delivery of good services. They further express that collaboration presupposes knowledge and understanding of the situation of the other.
Different perspectives
According to the nurses, collaboration with the hospital on patients that do not have cancer and who are about to be transferred to home health services represents a problem. Data show that the actors have different perspectives on what to emphasise in the collaboration regarding the needs and situation of the patient: “Collaboration starts in the system you work in. You may take a different view of collaboration depending on where you work […]. My perspective is that we work towards the user living at home. But when it is a matter of a user going home, it is more like they see that user in a medical perspective”.
According to the informants, actors in the specialist health care services have more of a medical perspective on the needs of the patients than the nurses, who have a more contextual understanding of the patient’s needs. Hospital personnel, for instance, is more concerned with the medical treatment of the patient’s illness, while the home health nurses say they focus more on the patient’s level of functioning and home situation. The differences in perspectives may make collaboration difficult, as the actors emphasise different aspects of the patient’s needs and situation. According to the informants, the content of the collaboration is also influenced by the health care services having a pressured workday and that it is “a rat race”. The informants say that everyone protects themselves and shifts the responsibility to others whenever possible.
Limited power and influence
The nurses describe an experience of limited power and influence in the collaboration. They say that the hospital physicians define when a patient is to be transferred to the municipality, and this may constitute a problem for the home health services. One informant says that: “We certainly do not experience having all the power in the world. We are generally told that he or she is coming home - and this is what you have to do. Period. Either from the hospital or through a decision from the administrative office, which may not be totally in line, to put it that way … “
Another informant states that: “We simply have to accept the patients”. The informants say here that they have to accommodate the patients without the care services being adapted to the needs of the patient. They further say that the patients are being transferred to the municipalities when the hospital physicians have assessed the patient’s medical situation. The patients, however, are still in need of treatment and care from home health services. According to the informants this has resulted in a greater workload and increased professional demands on the nurses in the home health services. This has also resulted in more frequent readmissions and patients being moved back and forth more now than earlier. The informants say that they have a coordination agreement with the hospital stating that patients shall not be returned to their homes between 14:00 hours on Fridays and 08:00 hours on Mondays. According to the nurses this worked well at first; now, however, the hospital frequently breaks the agreement and patients are transferred to the municipality and may arrive home late Friday nights and also on weekends.The nurses also say that they are rarely heard when they try to communicate with the hospital. They may, for instance. give information innumerable times on the work situation of home health care services to the hospital, without the actors in the hospital acting in accordance with the information. One informant says: “We feel like we are fighting against a superior power”.
Another informant says: “What frequently happens is that we receive the patient, holding a prescription – and no medication. It just doesn’t seem to help however many times we say that we do not have a pharmacy here in … and we have no medication, we don’t have all that many supplies. We just don’t have anything stored. So we frequently receive patients that are sent home without the things they need.”
The nurses further say that the time the home health care services need to plan the arrival of a new patient is rarely taken into consideration. According to the informants the need for planning relates, a. o., to that the home health care services do not have any supply of equipment or medication. The workforce is limited in the afternoons and on weekends, and days are unpredictable. Nurses also say that physicians and nurses both may promise patients services from home health services without asking home health services whether they will be able to deliver such services. One nurse puts it like this: “Then the doctor or nurse at hospital tells the patient: “Now you will receive home health care x 4, you need that”. And they have no idea about how the home is adapted. What they have done before. We have sent an admission report, but that is just a rough mapping. And then the patient is told that now you’ll get home health care x 4, and they will meet you, and then this is just not real.”
According to the informants, the hospital’s promises create expectations in the patients that home health services cannot always meet. The nurses say that they frequently know the patients and are able solve such situations through dialogues in which expectations are lowered and the patients are “secured”.
Limited cooperation and flow of information
According to the nurses, collaboration between actors is limited. The informants say that home health services do not have regular, formal arenas for collaboration with the hospital, which they did have prior to the reform. One informant says: “We attend coordination meetings at the hospital much less frequently now […]. I hear many people at the administrative office say that the coordination meetings at the hospital are a waste of time, for there is nobody there who knows the patients. […] We have said that we want to attend and they say they will include us, but there is no change”.
Home health services have an agreement about a “coordination council” with the hospital twice a year, but mostly information is distributed through the administrative office. The informants describe this as a disadvantage because important information gets lost, such as information on the functional level of the patient.
They further say that patients are sent home without discharge summaries and medication lists, which makes the planning of the patients’ services difficult. At times the papers are sent to the administrative office, and then home health services get the papers the day after the patient has arrived home. They may also get incomplete discharge summaries. One informant says: “If we are lucky enough to get anything at all, the discharge summaries are incomplete. I have contacted the hospital and pointed out something in the discharge summary and asked specific questions and I am just told that ‘this is not a complete discharge summary – you cannot use it. You have to wait for a complete version’. And that may arrive in a week, so…”.
The nurses say that the limited coordination of patient information makes them uncertain and as a result they double-check the incomplete information they receive. This leads to many telephone calls, extra work, and a stressful situation. The greatest challenge is, according to one nurse: “… to find the right people with the right expertise when I need it”. The nurses say that the actors at the hospital are friendly when called, but they frequently get hold of a nurse who just started a shift and does not know the patient. One nurse says that the absence of medication lists once forced her to make decisions regarding medication, and this is the physician’s responsibility
Discussion
The findings show that collaboration on cancer patients works well. The main impression is, however, that collaboration between hospital health care personnel and home health care services is tainted by an organisational unequal distribution of formal power between the various actors. Data further suggest that there is no common understanding established regarding what is important to collaborate on. This may, a.o., relate to the actors having limited knowledge about each others’ work situation.
The actors’ formal power is vested in the laws and regulations that regulate the coordination of the transfers of patients from specialist to municipal health care services (1,11). Power may, according to Hernes (24), be described as the actors’ capacity to realise their own interests. Power is here considered a relational concept (25). The unequal distribution of power in the collaboration between hospital personnel and home health care services is anchored in formal organisational structures. The hospital physicians have formal power to define when patients shall be transferred to the municipalities. Home health care services state that they do not have any choice but to “simply accept” patients that are sent home. Our study shows, in line with other studies, that patients are discharged earlier, are sicker, and need more treatment than before (16,17,19-20,26). Based on Hernes’ perspective on power, early discharge of patients may be understood as a case of the actors in the specialist health services realising their own organization’s interests and the intention of the reform that patients be sent home as soon as possible. The formal power distribution in the relation between actors does, however, seem to limit collaboration. This is because the physicians in the specialist health services can make decisions that influence the workday of the home health services, without involving them. Formalised measures that bind actors morally and legally to collaboration, may, to a certain degree, even out the differences in power. The study shows, however, that the coordinating council, which may be considered as a formalised measure for collaboration, hardly functions according to the intention.
The collaborative challenges also emerge when nurses need to seek informal contact with actors in the specialist health care services and experience rarely being heard. The interaction between the actors reveal limited collaboration, because, according to Orvik (10), collaboration rests on the actors having a positive attitude, leaving them room to establish informal contact. Not being heard may also give the nurses in the home health care services a feeling of powerlessness (24). Important premises for collaboration, such as mutual responsibility and equal worth, may thus be under threat (10).
The study further shows that hospital personnel promises the patients more extensive services than home health services can deliver, and that they break collaboration agreements. Such choices of actions may be seen in the context of the informants describing the health services as “a rat race” and that the actors first and foremost think about own “workload”. This entails that the actors to a limited extent solve tasks together, and the intentions of the coordination reform to “ensure flow in work processes so that patients experience cohesion in services and measures” (10, p.210), seem to suffer. The formal power structure appears to a limited degree to further a collaboration that obligates the actors, leaving room for shifting responsibility from the specialist services to the home health services.
The study further shows that the actors have different perspectives on what is collaboration. Differences in perspectives may be an expression of the actors only to a limited degree having established a common understanding of what collaboration entails, and what is important to collaborate on. Such challenges were also described by others before the implementation of the reform (1,3-5). That the actors involved act based on different perspectives may explain the informants’ experiences of incomplete information frequently accompanying the patient. Limited flow of information may also be understood as an expression of the formal organisational structure to a limited degree opening for exchange of knowledge between the actors. The very organisation of the work in the health care services as shifts also makes it difficult to get hold of the actors who have the relevant patient information. The way the health care services are organised may thus reduce the possibilities for collaboration between actors, and the preconditions for establishing such collaboration may thus be reduced (10). The study thus suggests that establishing a common understanding of the significance and content of collaboration across professions and organisational levels remains a challenge. According to Orvik, a common understanding of both collaboration and the current situation is necessary in order to achieve a mutual adjustment of work tasks (10).
The nurses say that the collaboration on cancer patients is a success, a. o. because the discharge processes are characterised by a good flow of information and dialogue between actors. The data also suggest that the actors in the hospital know that the home health care services have limited medical equipment and make sure that what patients need is available at discharge. This may indicate that the actors have a common understanding of what to collaborate on and how. A possible explanation for the actors having established a common understanding may be that cancer is a serious illness that brings forth existential questions that also touch the actors involved. At the same time, research shows that cancer is ranked high in the prestige hierarchy of disease diagnoses (27). This may be significant in the follow-up of patients when discharged from hospital and thus also for the collaboration between actors.
This study has contributed to shedding light on the way seven nurses from two different municipalities describe collaboration with actors in one hospital. The findings are thus not statistically generalisable. The nurses emphasise that the collaboration regarding cancer patients works well, whereas collaboration on patients with other illnesses remains a challenge. They experience the collaboration as characterised by an unequal distribution of power, and that involved actors have a different understanding of what collaboration entails and on what they are supposed to collaborate.
Conclusion
The study suggests that there is a need for both inter- and intra-organisational changes in order to improve collaboration. One important measure may be to establish a common collaborative arena, which would be in line with Report No 26 (2014-2015) to the Storting (28). This will likely further both the exchange of knowledge and contribute to increased understanding of the other’s work situation in collaboration on the care for the individual patient within the given framework. Organisational changes alone will probably not, however, solve the collaborative challenges (2,28). Actors need both the willingness and the capacity to collaborate to make coordination possible (10,28). Knowledge, willingness and capacity seem to characterise the coordination of cancer patients. Studying successful collaboration may yield valuable knowledge that may be used to improve collaboration within less successful areas. There is also a need for further research to clarify what is to be coordinated by the actors, how to create willingness to collaborate, and how to balance power relations between the actors. In order to explore the mentioned research topics, developing theories that contextualise what is relational in collaboration may be useful.
References
1. St.meld. 47. Samhandlingsreformen (2008-2009). Rett
behandling – på rett sted – til rett tid. Helse- og
omsorgsdepartementet. Oslo. 2009.
2. Melby L, Tjora A. Samhandlingens mange ansikter. I: Melby L.
Tjora A. (red). Samhandling for helse. Kunnskap, kommunikasjons og
teknologi i helsetjenesten. Gyldendal Akademisk. Oslo. 2013.
3. Hellesø R, Fagermoen M-S. Cultural diversity between
hospital and community nurses: implications for continuity of care.
Journal of Integrated Care 2010;10;1–9.
4. Hellesø R, Melby L. Forhandlinger og samspill i
utskrivningsplanleggingen av pasienter på sykehus. I. Melby L.
Tjora A. (red). Samhandling for helse. Kunnskap, kommunikasjons og
teknologi i helsetjenesten. Gyldendal Akademisk. Oslo. 2013.
5. Olsen RM. Informasjonsutveksling mellom sykepleiere i
hjemmesykepleie og sykehus ved overføring av eldre pasienter.
(Doktoravhandling). Kopieringen Mittuniversitetet, Sundsvall.
2013
6. Tingvoll WA, Sæterstrand T, Fredriksen ST. Kompetanse i
tiltakskjeden–avdelingslederes erfaringer om utskrivninger av eldre
pasienter fra sykehus. Vård i Norden 2010; 30:29–33.
7. Danielsen BV, Fjær S. Erfaringer med å overføre syke eldre
pasienter fra sykehus til kommune. Sykepleien Forskning 2010;
5:1:28–34.
8. Groene RO, Orrego C, Sunol R, Barach P, Groene O. «It›s like
two worlds apart»: an analysis of vulnerable patient handover
practices at discharge from hospital. BMJ quality & safety.
2012;21 Suppl 1:67–75.
9. Debesay J, Harslof I, Rechel B, Vike H. Dispensing emotions:
Norwegian community nurses› handling of diversity in a changing
organizational context. Social science & medicine. 2014;
119:74-80.
10. Orvik A. Organisatorisk kompetanse. Innføring i
profesjonskunnskap og klinisk ledelse. Cappelen Damm Akademisk.
Oslo. 2014.
11. Helsedirektoratet. Samhandlingsavtaler mellom kommuner og
helseforetak (10.02.2015).
https://helsedirektoratet.no/samhandlingsreformen/samarbeidsavtaler-mel…;
12. Helse- og omsorgsdepartementet. Forskrift om kommunal
betaling for utskrivningsklare pasienter 18.11.2011.
13. Helsedirektoratet. Samhandlingsstatistikk 2013–2014.
(07.05.2015) http://www.helsedirektoratet.no
14. Hermansen Å, Grødem AS. Redusert liggetid blant de eldste.
Sykepleien Forskning 2015; 10:24-32.
15. Kassah BLL*, Tingvoll WA*, Dreyer Fredriksen ST.
Samhandling–sykepleieledere og bestiller-utførerenhet. Geriatrisk
sykepleie 2014; 3:26–33.
16. Abelsen B, Gaski M, Nødland SI, Stephansen A.
Samhandlingsreformens konsekvenser for det kommunale pleie- og
omsorgstilbudet. IRIS Rapport 382/2014. (07.05.2015)
http://www.iris.no/forskning/samfunn/politisk-organisering-og-styring/h…
17. Grimsmo, A. Hvordan har kommunene løst utfordringene med
utskrivningsklare pasienter? Sykepleien Forskning 2013; 8:148–155.
18. Norheim KH, Thoresen L. Sykepleiekompetanse i
hjemmesykepleien–på rett sted til rett tid? Sykepleien Forskning
2015; 10:14–22.
19. Kassah BLL, Tingvoll W-A, Tønnessen S.
Samhandlingsreformen–utfordringer, løsninger og implikasjoner. I:
Kassah, BLL, Tingvoll WA, Kassah AK (red). Samhandlingsreformen
under lupen. Kvalitet, organisering og makt i helse- og
omsorgstjenestene. Fagbokforlaget Vigmostad & Bjørke AS.
Bergen. 2014.
20. Gautun H, Syse A. Samhandlingsreformen. Hvordan tar de
kommunale helse- og omsorgstjenestene imot det økte antallet
pasienter som skrives ut fra sykehusene? Rapport nr. 8/13. NOVA.
2013.
21. Sæterstrand TM, Holm SG, Brinchmann BS.
Hjemmesykepleiepraksis: Hvordan ny organisering av helsetjenesten
påvirker sykepleiepraksis. Klinisk Sygepleje 2015:29:1:4–16.
22. Patton MQ. Qualitative research and evaluation methods.
Sage Publications. Thousand Oaks. Calif. 2002.
23. Kvale, S. InterViews. An introduction to qualitative
research interviewing. Sage pub. Inc. Thousand Oaks. Calif. 1997.
24. Hernes, G. Makt og avmakt. Universitetsforlaget. Oslo.
1975/1997.
25. Englestad, F. Hva er makt. Universitetsforlaget. Oslo.
2009.
26. Kassah BLL, Jenssen GM, Tingvoll WA. Informasjonsflyt i
omsorgstjenesten– bruk av elektronisk pasientjournal. I: Kassah,
BLL, Tingvoll WA, Kassah AK (red). Samhandlingsreformen under
lupen. Kvalitet, organisering og makt i helse- og
omsorgstjenestene. Fagbokforlaget Vigmostad & Bjørke AS.
Bergen. 2014.
27. Album D, Westin S. Do diseases have a prestisje hierarchy?
A survey among physicians and medical students. Social science and
medicine 2008:66:1; 182–188.
28. St.meld. 26. Fremtidens primærhelsetjeneste – nærhet og
helhet (2014-2015). Helse- og omsorgsdepartementet. Oslo.
2015.










Comments