Using personas to allow greater input by home dialysis patients to the innovation process
A digital monitoring tool for home dialysis was at the development stage, but the patients were too ill to get involved. By using fictional patients, or personas, we were able to find a solution to the problem.
Background: The target is for at least 30 per cent of dialysis patients to be treated at home. Close monitoring by the specialist health service is vital for boosting the patients’ confidence and sense of coping with home dialysis. The study originated in a renal outpatient clinic where the renal nurses were using routines and support tools that provided no scope for increasing the share of patients on home dialysis. A digital monitoring tool needed pilot testing. The objective was to establish the practical value of the tool, and how it would need to be further developed in order to meet the needs of the hospital and the patients.
Objective: During the innovation process, the renal nurses at the outpatient clinic played an active part in the pilot project, while it proved more difficult to bring out the patients’ perspective due to their poor health. We therefore wanted to investigate how personas might be developed to provide a clearer picture of the patients’ needs and the relationship between the patients and the health service. We also wanted to promote a more user-centred focus for the development of monitoring technology for home treatment programmes.
Method: The study is an explorative, qualitative and longitudinal case study designed to test the digital monitoring tool. We collected data through interviews, observations and workshops with patients and renal nurses at the renal outpatient clinic as well as with hospital and community nursing staff, and the supplier’s employees. Our thematic analysis of case data gave us a base from which to develop personas that were later presented to the specialist renal nurses for validation.
Results: Our results show considerable variation in the patients’ need for monitoring and their access to methods that allow them to cope with home dialysis in their everyday lives. These varied needs are met by the renal nurses, who spend a considerable amount of time on communication, logistics and facilitation to secure the best possible treatment compliance. The personas were designed to take account of this interaction.
Conclusion: The use of personas has attracted criticism because the practice may be perceived to cause reduced involvement in the process by genuine service users. In this study, however, we have used personas precisely because there was limited opportunity to involve severely ill patients with the innovation process. To a large extent, personas can illustrate the interaction between renal nurses and patients, and the choices made by patients. Further work on personas should include descriptions of characters other than patients, e.g. members of the community nursing team and the patient’s relatives.
Introduction
One of the objectives set out in the National Health and Hospital Plan (1), is for patients to receive treatment in their own homes to the greatest extent possible. This means that healthcare personnel will visit the patient at home (2, 3), like in the hospital at home setting, or that the patient personally administers the treatment at home, supported by specialist health service advice and guidance through remote management (4).
The health effects of home treatment can be as good as or better than treatment in hospital, and the patient’s quality of life will be considerably better (5, 6). Home treatment also reduces the cost to the hospital (7). In Norway, the goal is to increase the share of patients who receive home treatment. Within the field of dialysis, the target is for at least 30 per cent of patients to be treated in their own home (8, resolution 170316).
At the end of 2020, 26 per cent of dialysis patients in Norway were receiving home dialysis (9). For comparison, the share of patients on home dialysis in the United States was 12.5 per cent in 2018 (10), while in Australia and New Zealand the figures were 25 per cent and 41 per cent respectively in 2020 (11). In Hong Kong, 75 per cent of patients were receiving home dialysis in 2018 (12).
It has been demonstrated that home dialysis improves the patient’s quality of life and lowers the cost to the hospital (7). However, several barriers to an active implementation of the home treatment regime have been identified, including the patient’ fear of not coping with the treatment (6).
Having a specialist renal nurse at the hospital contributes considerably to boosting the patient’s confidence and sense of coping (13, 14) in that there is close follow-up with training, advice and mental support. New digital solutions designed to support the communication between specialist renal nurses and home dialysis patients may well help to grow the share of patients on home dialysis, help nurses make more efficient use of their time and improve the treatment’s clinical quality (15, 16).
To be able to develop good digital solutions for patient monitoring and communication, suppliers need to be familiar with the needs of patients and healthcare personnel as the users of these systems.
Background to the study
The study originated from the needs of a renal outpatient clinic where the share of home dialysis was close to the 30 per cent target, but where it was felt that the renal nurses’ existing routines and support tools would not allow room for a further increase.
The hospital wanted to pilot test and customise a digital monitoring tool in order to establish whether it might be useful for the patients and the hospital, and to investigate how such a tool might be developed further in order to meet the needs of the various parties (17).
The pilot project was organised as a Triple Helix innovation project (18) involving the public sector (the hospital), the private sector (the IT supplier) and the university sector/academia as participants.
While the IT supplier had extensive knowledge of communication and logistics solutions, dialysis was a new field to them. The supplier needed to learenal nurse how the service was provided, and what the renal nurses and patients might have of pre-existing skills in using an IT tool and what might restrict its use.
The hospital needed a system that would simplify the ordering procedure for supplies, and that would help them keep better tabs on the patients’ condition during the periods between physical consultations with renal nurse or a doctor. They also needed a system that would provide a better overview of communications between the patients and the renal nurses at the outpatient clinic.
By defining these needs and taking part in interviews, workshops and observations, the renal nurses at the outpatient clinic were active contributors to the innovation work. Because the patients were also prospective users of the digital tool, it was important to identify their needs and wishes, so that the tool might be tailored to the needs of different dialysis patients. However, the patients’ poor health restricted their ability to be actively involved. In their absence, we had to look for different ways of making sure that the patients’ voices were heard in the innovation process.
In the field of product development, personas are frequently used to describe different service users (19). Personas are ‘detailed descriptions of imaginary people constructed out of well-understood, highly specified data about real people’ (19, p. 3).
Personas may give development teams a shared understanding of who the service users are, in that the service user profiles are made clearer (20). Personas ensure that developers are less inclined to base their work on their own experiences and preferences or to allow themselves to be steered by assumptions that generalise the service users’ needs (21).
The objective of the study
The pilot project’s overall goal was to understand how the technology would need to be designed. The objective of the study, however, was to investigate how we might develop personas in order to allow developers to better understand who the patients are, what will be important to them, and how different patient needs affect the work routines at the outpatient clinic. The study therefore focused on the following research questions:
- How can personas help to clarify how the patients handle home dialysis and the relationship between the patient and the health service?
- How can personas contribute to an enhanced user-centred focus in the development of technology for monitoring patients on home dialysis?
Method
Design, recruitment and data collection
The research questions were suited to a case study approach (22). The study was explorative, qualitative and longitudinal, and the case was the testing of the monitoring tool. This provided the context for developing personas.
We collected the data in the period from August 2019 to May 2020. We conducted individual, semi-structured in-depth telephone interviews with patients (n = 7), members of community nursing teams (n = 1) and the supplier’s members of staff (n = 1). The interviews lasted 45–60 minutes. Audio recording of interviews was subject to the informants’ explicit consent. The audio recordings were transcribed verbatim and later anonymised.
We also held workshops with renal nurses at the renal department (n = 3), medical management staff and employees in the hospital’s innovation department (n = 3) as well as members of the supplier’s staff (n = 2). The renal nurses also took part in group interviews. We took field notes during workshops and group interviews, and made an audio recording of one of the group interviews.
One of the group interviews was conducted as a structured review of a list of 16 patients who were being seen by the outpatient clinic at that particular time. During the review, the renal nurses described factors such as type of dialysis, family relationships and employment situation, how long the patient had been on home dialysis, whether the patient carried out the procedure unaided or was assisted by others, whether the patient needed contact with the outpatient clinic, what the nature of any such contact would typically be, and the degree to which the patient managed to comply with different aspects of the treatment regime. The latter included compliance with the dialysis plan, filling in flow sheets, taking regular blood pressure readings, reporting any potential treatment complications and keeping tabs on the stock of supplies at home.
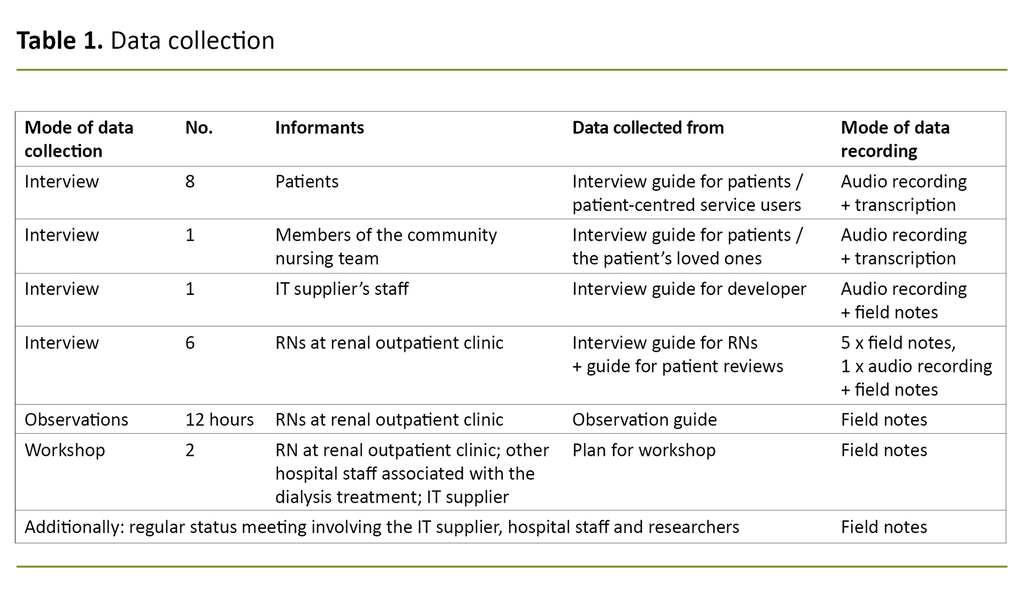
All informants gave their informed consent to taking part. Data collected in 2019 formed the basis for creating the personas, which were then validated by the data collected in 2020. At that point, the personas were presented to healthcare personnel who were well acquainted with the patient group and who made the personas a topic for discussion during one of the workshops. The personas were also used by the renal nurses to recruit patient informants. Table 1 provides an overview of the data.
Context
The study was conducted at the renal outpatient clinic of a medium-sized Norwegian hospital. This renal outpatient clinic offers training and monitoring of patients on home dialysis.
Dialysis is an equipment-intensive treatment. The patients need a supply of dialysate bags, tubing and equipment for transferring fluids, as well as consumables for cleaning and maintaining catheters. It is nevertheless not desirable for patients to be storing excessive supplies at home, because their need for equipment may change and deliveries already made may need to be scrapped. Frequent deliveries of supplies are therefore required.
At the renal outpatient clinic in question, the specialist renal nurses rang each patient weekly or every two weeks to record the patient’s level of supplies. This conversation allowed the nurses to respond to any questions the patient might have and exchange information about the patient’s health or other matters. This put the nurses in a position to assess whether the treatment and range of equipment would need to be adjusted for the next period, and whether there was a need to change the frequency of consultations.
The frequency of the patient’s hospital consultations depends on how the disease progresses. Patients are supposed to bring a log of their fluid balance to the consultation, either in the form of a manual log or the memory card from the dialysis machine. However, patients frequently forgot to bring this along, or they failed to keep a log on paper, which gave an incomplete basis for making adjustments to the continued treatment.
Analysis
We analysed patient information provided by the patients during interviews and workshops. This was done by drawing up a form where different aspects were given predefined, quantifiable values. Examples of such aspects and values are: treatment compliance (good, medium, poor), assistance from others (relatives, local authorities, relatives and local authorities), personally planning ahead for stocks of supplies (yes, no), and declared confidence in their own coping skills (great, some, little, don’t know).
We grouped these aspects into themes (23) such as ‘degree of coping’, ‘compliance with the treatment plan’ and ‘on top of supplies and life situation’, from which we formed the basic characteristics of our personas. These themes indirectly support the level of assistance that the patient will need from the renal nurses in order to manage their disease.
They also describe whether the patients are surrounded by a social network or close family members who may help them boost their sense of coping, or otherwise if there is a need for more extensive assistance from the renal nurses. The themes impact on the development of the monitoring technology.
One example is whether there are several different assistants, like a spouse or other close family, neighbours or community nurses. If these people are intended to use the tool together with or on behalf of the patient, there will be a need to define and differentiate between the type of medical information they should each have access to, whether they should be able to communicate with the hospital on the patient’s behalf, and whether they should be able to report or order equipment on the patient’s behalf. If there is a large group of assistants, or if they need very different things from the IT tool to be able to assist the patient effectively, then a more sophisticated system may be required.
Based on in-depth interviews with patients and on the renal nurses’ reflections concerning life with dialysis treatment, we identified the following themes: how the treatment fitted in with the patients’ everyday lives, how the patients related to the regular monitoring calls from the renal outpatient clinic, and what choices the patients made in order to be able to receive the treatment. These themes were used to give our personas ‘richer’ lives.
We presented the personas to the renal nurses, who confirmed that they presented an appropriate picture of the patients and provided sufficient anonymisation of individuals. This helped us to validate our study (24).
Results
Patients with differing needs
In general, the only characteristic that was shared by all the patients, was that their daily lives were significantly impacted by their disease. When reviewing the 16 patients, the renal nurses established that two found themselves in a start-up phase and had yet to begin the actual treatment. Of the remaining 14 patients, half of them managed the treatment by themselves, while 29 per cent (4) managed with assistance from relatives or the community nursing team. A total of 21 per cent (3) were completely dependent on assistance provided by the community health care and/or relatives.
Of the 11 patients (79 per cent) who took personal responsibility for their treatment, with or without assistance from others, the renal nurses felt that only one appeared to be less than confident in their own ability to cope with the treatment. Half of those receiving active treatment, needed significant monitoring by the outpatient clinic. The reasons for this included an unstable clinical situation, frequent changes in daily routines due to holidays, activities, hospitalisation or such, or they needed significant contact with the renal nurses for mental support.
Treatment schedules and the ordering procedures for supplies were largely adjusted to the individual patient’s clinical situation, lifestyle and personal preferences. This applied in respect of stocks to be ordered, whether it was an RENAL NURSE or a patient who calculated the quantities to be ordered, what records of the treatment were kept by the patients, like fluid inputs/outputs, weight, blood pressure and suchlike, and what means of communication was being used.
For most patients, the renal nurses calculated the quantities of supplies that were needed for the next period based on the patient’s at-home stock check. Three patients personally calculated what supplies they needed to order and reported this by phone, email or text message. Two patients were receiving haemodialysis while five were receiving Continuous Ambulatory Peritoneal Dialysis (CAPD). The remaining seven were receiving Automated Peritoneal Dialysis (APD), but periodically CAPD.
All these customisations increased the renal nurses’ workload. They were nevertheless adamant that the customisations were necessary to give patients the best possible support during their treatment. The customisations were of considerable value to the patients. In the words of one of the patients:
‘If you couldn’t submit your order by email, or if you would have to phone in the order between the hours of this and that, then it would have had an adverse effect on my work, and on my quality of life, in a way. Because it would have meant that I couldn’t do my job in the way that I do now. It’s obviously they [the renal nurses] who facilitate things so that I’m able to work, among other things. There is no doubt about that.’
The renal nurses were clear that patients on home dialysis need to take personal responsibility for their own treatment, and that they therefore should be able to choose not to comply with the treatment plan. However, they pointed out that patients needed adequate training to make informed decisions; they had to be aware of the bodily effects of insufficient treatment in the short and long term.
When interviewed, the patients reported that the disease and its treatment took up a lot of space in their lives, in the form of time, attention and reduced capacity for other activities. One informant expressed it like this:
‘I can’t be bothered to go over and count whether I’ve got thirteen or seventeen [sticky plasters]. It feels as if the disease takes such a lot of time, the illness takes so much of my time anyway.’
The more experienced patients reported that they were becoming so familiar with the treatment that they no longer spent time on diligently recording things like fluids and weight, but that they instead were sticking to the dialysis routine and took care to note whether anything felt unusual:
‘I’m supposed to check my weight every morenal nurseing, but I don’t, ‘cos I get weighed at the hospital.’
One patient also described how they sometimes skipped a dialysis or extended the period between bag changes because other activities were prioritised:
‘I’m pretty active, so it doesn’t always suit, so at times I’ll just empty, I’m just emptying out rather than emptying and filling up. […] if I have travelled to the cabin and plan on staying there for a few days, I’ve been known to just empty in the morenal nurseing and the fill up at five o’clock.’
The renal nurses reported that they saw the need to adjust the record-keeping requirements according to how well each patient was coping with the treatment and their life situation in general, and also with the extra workload that the treatment represented for each individual. Nevertheless, they felt that they at times were unable to keep fully up to speed with how the patient was really doing.
Personas describe needs and interactions
We developed our five personas based on the results presented above. They describe different stages of life, networks, forms of communication and degrees of coping in typical home dialysis patients without identifying individuals. They also illustrate how dialysis patients will come at treatment procedures and technology from different starting points and with different levels of motivation (Table 2).
They also illustrate the interaction between the patient and the renal nurses at the renal outpatient clinic, and how the patient’s life situation, motivation, coping strategy and needs affect the renal nurses’ work style and workload.
Using personas
Personas formed the starting point for discussions between the IT supplier, the healthcare personnel and the authors about how the development of the digital monitoring tool ought to continue, and what adjustments were necessary to support the patients’ various needs. In this process, the renal nurses personally conveyed their own needs, while the personas highlighted the needs of the patients.
For example, one important patient requirement might be to have a choice between communicating with the hospital by phone or through the digital monitoring tool’s text messaging system or recording sheets. Another requirement might be for patients to choose how to convey their need for further supplies or their need for a change to their treatment plan.
Personas also provided a framework for the renal nurses as they sought to recruit patients for follow-up interviews after the monitoring tool had been pilot tested over a period of time.
Ethical considerations
The project was submitted to the Norwegian Centre for Research Data (NSD), reference number 2019/539488. Patients who were recruited to the project consented to the renal nurses sharing information with us about their treatment. Nevertheless, the healthcare personnel were diligent in ensuring that none of the information they passed on could be used to identify individual patients.
Discussion
The use of personas has attracted criticism because this may cause fewer genuine service users to be included in the process, or service users may come to be less frequently involved (25). However, in this study we made use of personas because it was impossible for severely ill patients to contribute actively to the innovation process.
When developing the personas, we could have chosen to base our work on interviews with patients and a purely structural matching of the patient lists with the aspects described above. However, we wanted to acknowledge the specialist renal nurses’ in-depth knowledge of the patient group. This insight has been essential to our efforts to enrich our personas with nuances that would otherwise not have emerged.
The renal nurses understand the patients’ need for customisation
The patients in our study frequently referred to their close contact with the specialist renal nurses, who were familiar with their life situation and knew what was important to them. The patients reported this to be an important source of reassurance. This is a finding that matches those described by Rygh et al. (13) and Virtanen et al. (14).
We also found what Polaschek (26) refers to as ‘negotiation’, where the healthcare personnel’s objective of optimal treatment to prevent late-onset injury and adverse health effects, does not always coincide with the patient’s aim of having a good quality of life, now and in the longer term.
In some cases, specialist renal nurses have to accept a patient’s less-than-perfect treatment compliance, or a renal nurse’s less-than-perfect knowledge of the patient’s condition, because this is better than if the patient gives up completely. These aspects are highlighted by our ‘Kari’ persona. The renal nurses ease their flow and weight reporting demands to prevent ‘Kari’ from feeling that the treatment is too onerous so that her compliance lapses for long periods at the time.
We also find this ‘negotiation’ in patients who gradually have acquired a certain level of knowledge and experience, and who personally make decisions about what constitutes ‘adequate’ treatment. This is illustrated by our ‘Fredrik’ persona.
Kutner (27) similarly describes how such patient-initiated adjustment to the treatment can give patients a greater sense of control, which makes it easier for them, mentally, to stick to the rest of the treatment plan.
Digital tools should not only support the optimal treatment
A digital tool designed to support the interaction between patients and Renal nurses will need to take account of real-life negotiations and adjustments. In other words, solutions cannot be developed based on ideal treatment scenarios (28, 29).
Our personas therefore illustrate that patients have different ways of handling the challenges of their everyday lives. The personas help ensure that the finished digital tool does not become yet another burden for the patients. Furthermore, the personas will help ensure that the digital tool can be tailored to the patients’ different coping strategies. This means that it should also be possible to use the digital tool when the patient does not comply with the treatment or report optimally.
Using personas may potentially be useful to the renal ward, in that they raise awareness of what adjustments are made to accommodate the various patients. Our results show that the various individual customisations involve considerable additional work for the renal nurses, which may prevent the department from handling an increasing share of patients on home dialysis.
Personas can be useful to the department’s continued work to evaluate its own routines and devise more standardised forms of patient monitoring. Personas can be used as a framework for this work to structure varying patient needs and different monitoring routines.
The study’s strengths and weaknesses
One of the study’s weaknesses was the low number of patients that formed the basis for our persona development work. This weakness is partly balanced out by the fact that experienced renal nurses gave their assessment of the personas based on their own experiences with the general patient group, and they introduced adjustments to the personas accordingly.
During the pilot project, the hospital deliberately opted to start with the relationship between specialist renal nurses and patients. At an early stage, the results of observations indicated that the working day of specialist renal nurses involves a large number of people who enable them to assist patients with their treatment. These contributors may be the community nursing team, municipal short-stay units, other departments in the same hospital, other hospitals, the Norwegian Labour and Welfare Administration, relatives and general practitioners (17).
In the process of identifying relevant users of the digital monitoring tool, the personas played an important part by describing parties that routinely participate in dialysis-related communications and routines, reporting and equipment orders.
Gradually, it became clear that another two contributors ought to be represented by separate personas in order to support further development of the technology: a member of the community nursing team and a partner or family member who is involved with the treatment, like the persona Lillian’s spouse. However, the study’s duration was not long enough for us to develop these additional personas and use them in the continued innovation work.
Conclusion
In a study where it is difficult to involve patients as active contributors to the development of a digital monitoring solution, personas have been useful tools in that they give the patients a clear voice as service users. This voice was strengthened because we involved the renal nurses’ in-depth knowledge of the patients’ general needs when we developed the personas.
Personas can therefore also shed light on the interaction between the patients’ everyday lives with home dialysis and the renal nurses’ organisation and implementation of their work. The personas were not intended to describe the renal nurses’ work in detail, because the renal nurses were able to contribute actively as participants in the development process.
In a time-limited study where the digital monitoring tool will be developed further after its completion, personas are useful to the IT supplier because they provide a structured picture of the patients’ needs, even after the pilot project has come to an end.
The project was funded by RFF Oslofjordfondet.
The authors declare no conflicts of interest.
References
1. Meld. St. 7 (2019–2020). Nasjonal helse- og sykehusplan 2020–2023. Oslo: Helse- og omsorgsdepartementet; 2019. Available at: https://www.regjeringen.no/no/dokumenter/nasjonal-helse--og-sykehusplan-2020-2023/id2679013/ (downloaded 30.10.2021).
2. Lippert M, Semmens S, Tacey L, Rent T, Defoe K, Bucsis M, et al. The hospital at home program: no place like home. Curr Oncol. 2017;24(1):23–7. DOI: 10.3747/co.24.3326
3. De Zen L, Del Rizzo I, Ronfani L, Barbieri F, Rabusin M, Dall'Amico R, et al. Safety and family satisfaction of a home-delivered chemotherapy program for children with cancer. Ital J Pediatr. 2021;47(1):43. DOI: 10.1186/s13052-021-00993-x
4. Manani SM, Rosner MH, Virzì GM, Giuliani A, Berti S, Crepaldi C, et al. Longitudinal experience with remote monitoring for automated peritoneal dialysis patients. Nephron. 2019;142(1):1–9. DOI: 10.1159/000496182
5. Olivari Z, Giacomelli S, Gubian L, Mancin S, Visentin E, Di Francesco V, et al. The effectiveness of remote monitoring of elderly patients after hospitalisation for heart failure: the renewing health European project. Int J Cardiol. 2018;257:137–42. DOI: 10.1016/j.ijcard.2017.10.099
6. Walker RC, Howard K, Morton RL, Palmer SC, Marshall MR, Tong A. Patient and caregiver values, beliefs and experiences when considering home dialysis as a treatment option: a semi-structured interview study. Nephrology Dialysis Transplantation. 2016;31(1):133–41. DOI: 10.1093/ndt/gfv330
7. Wong CKH, Chen J, Fung SKS, Mok MMY, Cheng YL, Kong I, et al. Direct and indirect costs of end-stage renal disease patients in the first and second years after initiation of nocturnal home haemodialysis, hospital haemodialysis and peritoneal dialysis. Nephrol Dial Transplant. 2019;34(9):1565–76. DOI: 10.1093/ndt/gfy395
8. Helsedirektoratet. Saker behandlet av Prioriteringsrådet 2007–2017 [Internet]. Oslo: Helsedirektoratet 01.05.2019 [updated 01.05.2019, cited 30.11.2021]. Available at: https://www.helsedirektoratet.no/tema/prioritering-i-helsetjenesten/saker-behandlet-av-prioriteringsradet-2007-2017
9. Åsberg A, Steinskog ØS, Thomsen J, Vikse BE, Leh S, Waldum-Grevbo BE, et al. Norsk nyreregister. Årsrapport for 2020 med plan for forbedringstiltak. Nasjonalt servicemiljø for medisinske kvalitetsregistre; 2021. Available at: https://www.kvalitetsregistre.no/sites/default/files/2021-06/Nyrereg.%20A%CC%8Arsrapport%202020.pdf (downloaded 29.11.2021).
10. United States Renal Data System. Volume 2: end stage renal disease. I: 2020 USRDS annual data report: epidemiology of kidney disease in the United States. Bethesda, Maryland: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2020. Available at: https://adr.usrds.org/2020/end-stage-renal-disease (downloaded 30.11.2021).
11. ANZDATA Registry. 44th report, chapter 2: prevalence of kidney failure with replacement therapy. Adelaide, Australia: Australia and New Zealand Dialysis and Transplant Registry; 2021. Available at: https://www.anzdata.org.au/wp-content/uploads/2021/09/c02_prevalence_2020_ar_2021_chapter_v1.0_20211112_Final.pdf (downloaded 05.11.2021).
12. Li PK-T, Rosenberg ME. Foreign perspective on achieving a successful peritoneal dialysis-first program. Kidney360. 2020;1(7):680–4. DOI: 10.34067/KID.0000712019
13. Rygh E, Arild E, Johnsen E, Rumpsfeld M. Choosing to live with home dialysis-patients' experiences and potential for telemedicine support: a qualitative study. BMC Nephrology. 2012;13(1):1–8. DOI: 10.1186/1471-2369-13-13
14. Virtanen H, Tuominen R, Kiukainen S, Koskinen J, Koskenniemi J, Laulaja J, et al. Experiences of safety among patients receiving home dialysis therapies. Journal of Renal Care. 2019;45(4):223–31. DOI: 10.1111/jorc.12298
15. Wallace EL, Rosner MH, Alscher MD, Schmitt CP, Jain A, Tentori F, et al. Remote patient management for home dialysis patients. Kidney International Reports. 2017;2(6):1009–17. DOI: 10.1016/j.ekir.2017.07.010
16. Manani SM, Baretta M, Giuliani A, Virzì GM, Martino F, Crepaldi C, et al. Remote monitoring in peritoneal dialysis: benefits on clinical outcomes and on quality of life. Journal of Nephrology. 2020;33(6):1301–8. DOI: 10.1007/s40620-020-00812-2
17. Nilsen ER, Boysen ES, Ausen D, Skifte A, Eliassen R. Virtual hospital at home – co-creation and implementation of a digital solution [digital]. Norsk konferanse for organisasjoners bruk av IT (NOKOBIT), Universitetet i Sørøst-Norge; 2020.
18. Leydesdorff L, Etzkowitz H. Emergence of a Triple Helix of university–industry–government relations. Science and Public Policy. 1996;23(5):279–86. DOI: 10.1093/spp/23.5.279
19. Pruitt J, Adlin T. The persona lifecycle: keeping people in mind throughout product design. San Francisco, California: Morgan Kaufmann; 2006.
20. Pruitt J, Grudin J. Personas: practice and theory. In: Arnowitz J, Chalmers A, eds. DUX '03: Proceedings of the 2003 conference on designing for user experience. San Francisco, California: ACM; 2003:1–15. DOI: 10.1145/997078.997089
21. Miaskiewicz T, Kozar KA. Personas and user-centered design: How can personas benefit product design processes? Design Studies. 2011;32(5):417–30. DOI: 10.1016/j.destud.2011.03.003
22. Yin RK. Case study research. Design and methods. 5th ed. Thousand Oaks, California: SAGE Publications; 2014.
23. Corbin J, Strauss A. Basics of qualitative research: techniques and procedures for developing grounded theory. 3rd ed. Thousand Oaks, California: SAGE Publications; 2008.
24. Carlson JA. Avoiding traps in member checking. Qualitative Report. 2010;15(5):1102–13. DOI: 10.46743/2160-3715/2010.1332
25. Blomquist Å, Arvola M. Personas in action: ethnography in an interaction design team. In: Bertelsen O, Bødker S, Kuutti K, eds. Proceedings of the second Nordic conference on Human-computer interaction. Aarhus: ACM; 2002:197–200. DOI: 10.1145/572020.572044
26. Polaschek N. Client attitudes towards home dialysis therapy. J Ren Care. 2007;33(1):20–4. DOI: 10.1111/j.1755-6686.2007.tb00032.x
27. Kutner NG. Improving compliance in dialysis patients: Does anything work? Semin Dial. 2001;14(5):324–7. DOI: 10.1046/j.1525-139X.2001.00080.x
28. Dugstad J, Eide T, Nilsen ER, Eide H. Towards successful digital transformation through co-creation: a longitudinal study of a four-year implementation of digital monitoring technology in residential care for persons with dementia. BMC Health Services Research. 2019;19(1):1–17. DOI: 10.1186/s12913-019-4191-1
29. Lusch RF, Vargo SL. Service-dominant logic: reactions, reflections and refinements. Marketing Theory. 2006;6(3):281–8. DOI: 10.1177/1470593106066781















Comments