Depth of sleep measured during anaesthesia in elective caesarean section following induction with propofol or thiopental
Patients who had induction of anaesthesia with thiopental had a higher risk of experiencing accidental awareness.
Background: Caesarean section under general anaesthesia is the surgical intervention with the highest incidence of accidental awareness. This state can result in traumatic complications such as anxiety, nightmares, sleep problems and post-traumatic stress disorder.
Objective: The aim of this systematic review was to synthesise measurements of sleep depth throughout the whole course of anaesthesia from randomised controlled trials where we compared induction of anaesthesia with propofol and thiopental in elective caesarean section.
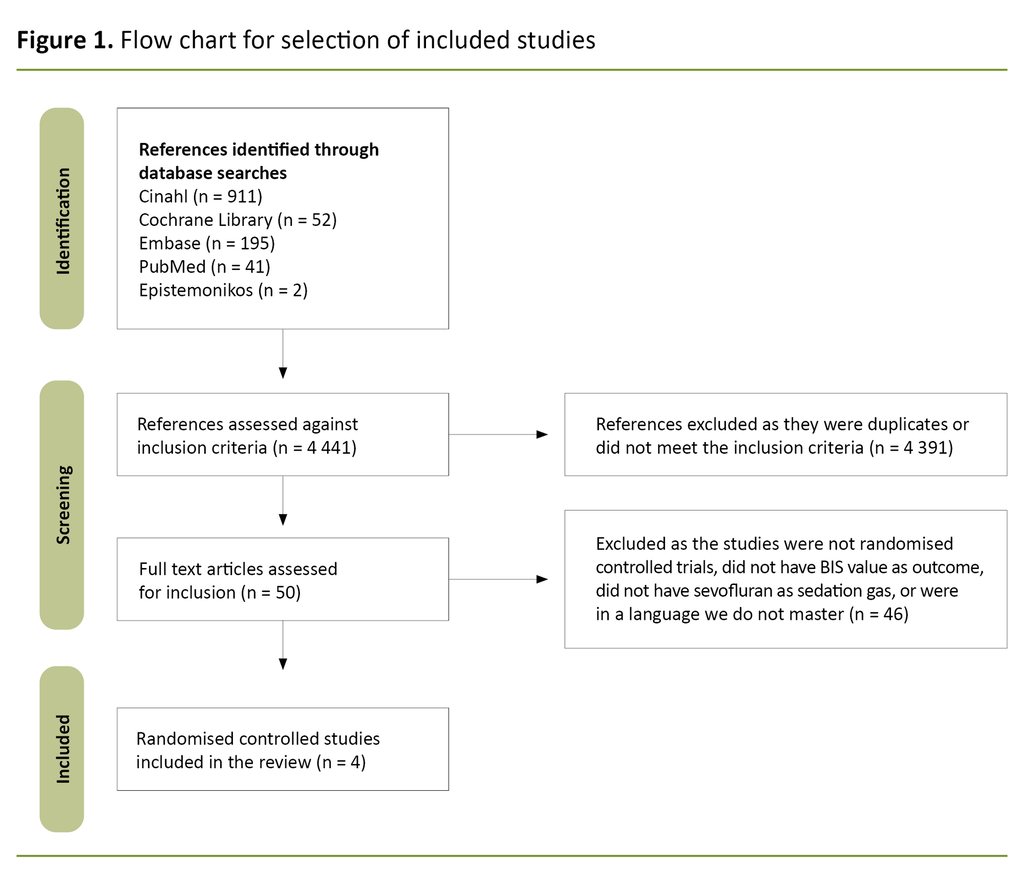
Method: The study is a systematic review with meta-analysis. Systematic searches were carried out in the following databases: the Cochrane Database of Systematic Reviews (CDSR), Embase (OVID), Cinahl (EBSCO), PubMed, Google Scholar and Epistemonikos. The objective was to obtain bispectral index (BIS) values at the following measurement points: induction, intubation, skin incision, uterine incision, delivery, uterine suture and skin suture.
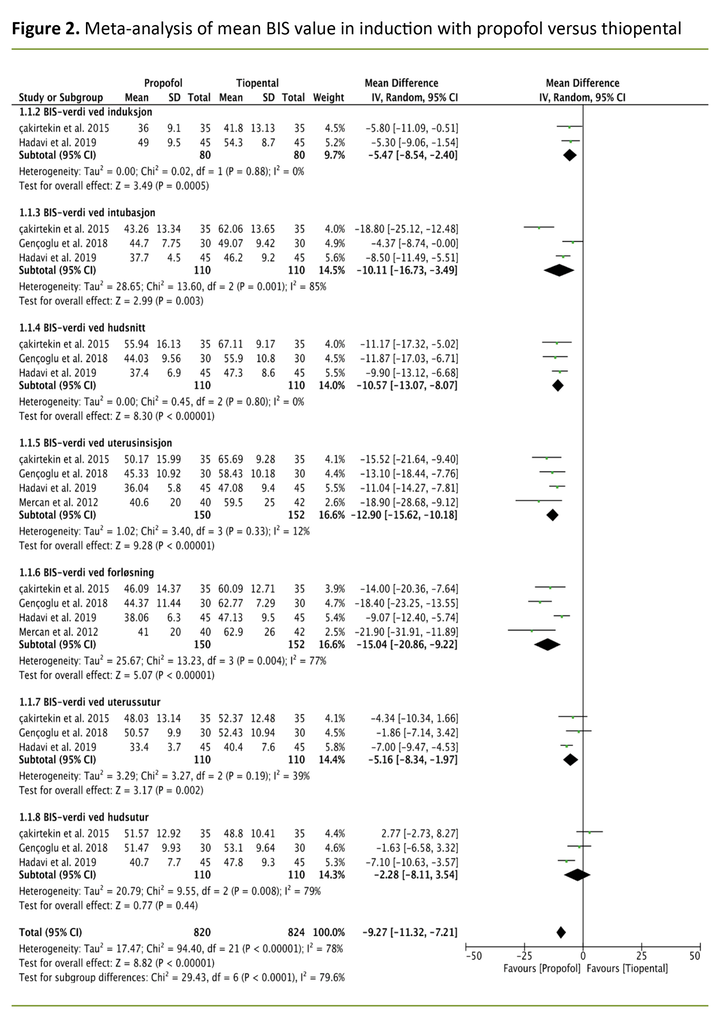
Result: a total of four randomised controlled trials were included in this systematic review. The meta-analysis shows significantly lower BIS values in favour of the propofol group (mean difference –9.27; 95 per cent confidence interval –11.32; –7.2). For patients who had induction of anaesthesia with propofol, the mean BIS value was below 60 and the participants had a low risk of awareness compared with the thiopental group across all studies. The sub-groups of ‘induction’, ‘intubation’, ‘skin incision’, ‘uterine incision’, ‘delivery’ and ‘uterine suture’ show significant results in favour of lower BIS in induction with propofol compared with thiopental. The calculation of heterogeneity in the meta-analysis shows a high degree of statistical heterogeneity between the studies, with a p-value of < 0.00001 and I² at 78 per cent.
Conclusion: This study shows that patients who had induction of anaesthesia with propofol in elective caesareans have a lower risk of experiencing accidental awareness during general anaesthesia. Furthermore, it illustrates the necessity of nurse anaesthetists measuring sleep depth and being conscious of risk factors in the pregnant woman which may involve increased risk of awareness.
Introduction
Caesarean section under general anaesthesia is associated with an increased risk of perioperative accidental awareness (1, 2, 8).
Regional anaesthesia is the preferred method for caesarean section; however, in certain circumstances a general anaesthetic may be an alternative, including in elective procedures. General anaesthesia is an alternative in cases where the mother suffers from a coagulation disorder, certain neurological conditions, spinal deformities, or where regional anaesthesia has failed to work or the mother prefers it (1, 2, 8).
Awareness under general anaesthesia is a feared complication where the patient may experience being conscious without being able to move. At the same time, the patient may feel pain and/or hear what is happening without being able to communicate it (1, 5). One important cause of awareness is underdosing of sleep medication in combination with muscle relaxant drugs (2, 4).
The challenge with anaesthesia in caesarean section is that the need of the mother for pain relief and sufficient sleep depth must be safeguarded, while the drugs being administered affect the child via the placenta (1).
Inhalation drugs which ensure sleep can cause uterine atony, while benzodiazepines and opioids which prevent pain and discomfort in the mother can cause respiratory depression in the child. Underdosage of these drugs increases the risk of awareness in the mother (1, 3).
The studies of Brown et al. (2) and Odor et al. (3) found that patients who experienced awareness might suffer later from anxiety, nightmares, sleep problems, stress and post-traumatic disorder (3, 4).
Risk factors for awareness during caesarean sections have been shown to be young age, anxiety and a low or high body mass index (1, 3, 4). Other risk factors are acute surgery immediately after induction of anaesthesia, carrying out caesarean section at night, perioperative bleeding and inexperienced anaesthesia personnel. Physiological changes in the pregnant woman, such as increased cardiac output per minute which in turn increases the redistribution of intravenous anaesthetic drugs and slows the establishment of sufficient partial pressure of anaesthetic gas, are also trigger factors (1).
Increased cardiac output per minute reduces the duration of action of a bolus dose of the induction drug. At the same time, the altered physiology contributes to the mother needing longer to achieve the effect of the anaesthetic gas (1).
In 2019, 8 670 caesarean sections were registered in Norway. Of these, 959 (11.1 per cent) were carried out under general anaesthesia (5). Awareness during general anaesthesia in caesarean section corresponds to 1 in 670 compared to 1 in 19 000 for other surgical procedures (6). The most common anaesthetics used to induce anaesthesia in caesarean section are thiopental and propofol. Since 1959, the standard medications used to induce general anaesthesia in caesarean sections have been thiopental and suxamethonium (1, 7).
Propofol entered the market in the 1980s, but for a number of reasons it was not adopted for use in caesarean section. Unlike propofol, thiopental was authorised for use in pregnant women, and it was further claimed that thiopental had a more rapid onset of action and could be used in rapid sequence induction (RSI).
Compared with propofol, thiopental had less of a haemodynamic effect on the mother and the placenta. Based on these findings, thiopental remained the first choice over propofol (7).
The study by Tumukunde et al. (8) compared induction with thiopental and propofol in emergency caesarean section. They investigated the condition of neonates after delivery (Apgar score) and the time from when the mother received induction of anaesthesia until she was awake.
Tumukunde et al. concluded that there was no significant difference in the Apgar score after delivery between the group receiving thiopental and the group receiving propofol (8). Mothers in the propofol group were found to take significantly less time to wake up. In their study, Park et al. (9) found no significant haemodynamic difference in women who were given induction with propofol or thiopental respectively.
Previously a single dose of thiopental was recommended as the preferred induction agent for general anaesthesia in caesarean section; however, in the last few years there has been a change in which propofol is used together with suxamethonium for induction in caesarean section (3).
Compared to propofol, there is a four-times greater risk of awareness (3), and many textbooks, guidelines and studies now recommend the use of propofol. Induction agents such as thiopental, etomidate and propofol have not been shown to have any teratogenic effect. Neither have they affected brain development in animal embryos. Their use is nevertheless not stated as safe in the Norwegian Pharmaceutical Product Compendium (Felleskatalogen) (3).
It is, however, highly likely that propofol is being used off label because the drug is not licensed in many countries apart from the USA. Most medicines used in obstetric anaesthesia are only allowed if the therapeutic effect outweighs the risk (3).
The Bispectral index (BIS) is based on electroencephalography (EEG) and shows electrical impulses from the brain. The values reflect the patient’s level of consciousness. A value of 0 represents an absence of brain activity and 100 shows an awake state (10).
In order to assess how deeply anaesthetised a patient is during general anaesthesia, BIS has proved to be a safe measurement tool (10). BIS values between 40 and 60 represent sufficient sleep depth and are recommended in order to reduce the risk of awareness during anaesthesia (10).
The aim of the study
The aim of this systematic review was to investigate whether there is a difference in BIS values throughout the whole course of anaesthesia following induction with propofol versus thiopental in elective caesarean section. The following research question is addressed:
‘How does propofol, compared to thiopental, affect BIS values in the course of anaesthesia measured in elective caesarean section under general anaesthesia?’
Method
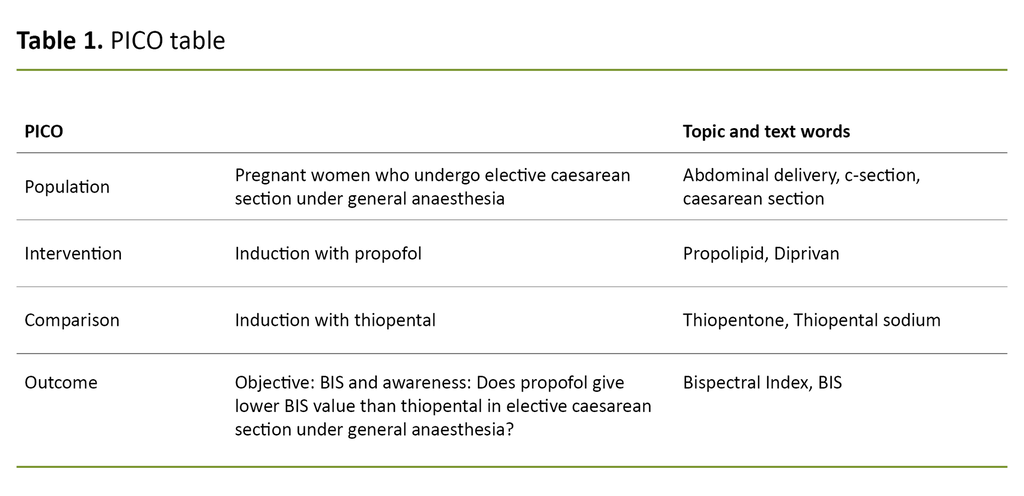
In order to be able to formulate an explicit and focused research question we systematised and structured the search strategy using the PICO model (Table 1), which was also used to develop the research question.
In PICO the clinical questions are formulated to identify four components: population, intervention, control and outcomes (11). Search words were structured using PICO, and mesh.uia.no was used to find text words and topic words for the search strategy.
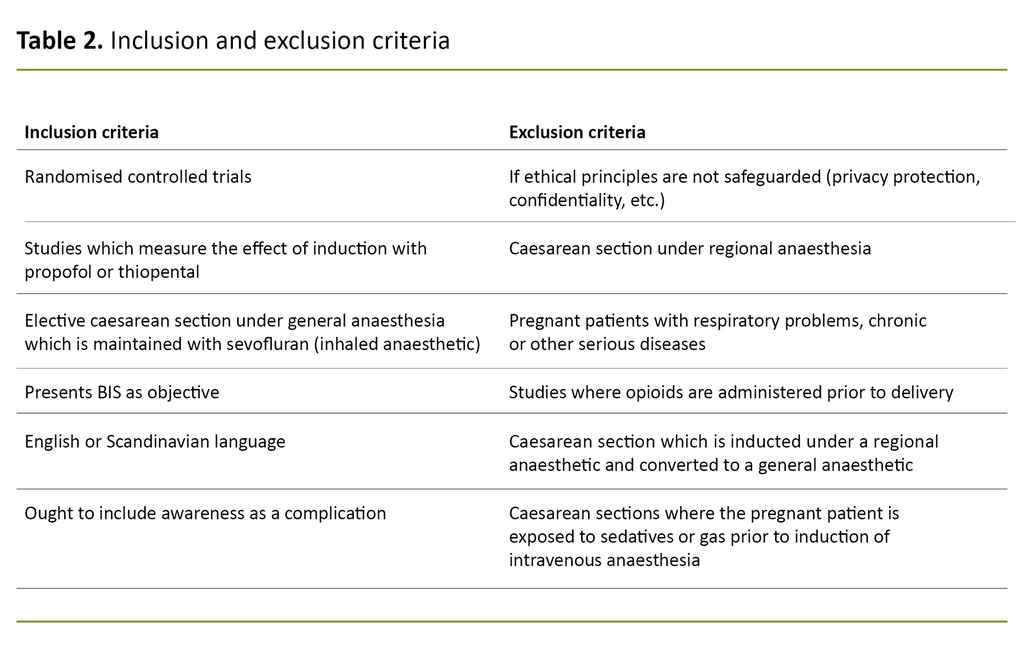
Inclusion and exclusion criteria are presented in Table 2.
Article search and search words
We carried out systematic searches in the last quarter of 2020. An updated search was carried out in April 2021, which did not result in the inclusion of any new articles. We consulted a university librarian for guidance on search strategy and relevant databases.
In order to achieve the maximum number of hits we did not apply limits on publication year or other filters in the databases. We contacted an expert in the specialist field who made suggestions about reference works and supporting literature.
We used SveMed+ and MeSH to identify subject headings and text words. Systematic searches were carried out in the following databases: the Cochrane Database of Systematic Reviews, Embase (OVID), Cinahl (EBSCO), PubMed, Google Scholar and Epistemonikos.
The reference lists of included studies were reviewed in order to capture articles which had not been identified by the search; however this only identified duplicates. Because the results of the systematic searches provided relatively few hits, we carried out a thorough manual review of these rather than using EndNote. All relevant hits in Google Scholar, which was the last database we searched in, were duplicates of other hits.
We identified six articles in languages we do not master, such as Iranian, Farsi and Korean. In an attempt to obtain these in an English version we emailed the principal authors of all the articles, but did not receive any replies.
Selection and critical appraisal
Independently of each other, the principal author and co-author (JØ, LMR) went through titles, summaries and complete articles for inclusion based on the inclusion and exclusion criteria. The assessments of the texts were then compared before a pilot test on the first 40 studies was carried out in order to quality-assure a common understanding of the criteria. The pilot test confirmed that we agreed on the inclusion and exclusion criteria.
Two articles were critically appraised in order to obtain a common understanding of how to interpret and assess the questions in the Norwegian Electronic Health Library’s checklist for randomised controlled trials (12). The included articles were subsequently critically assessed by two individuals independently of each other.
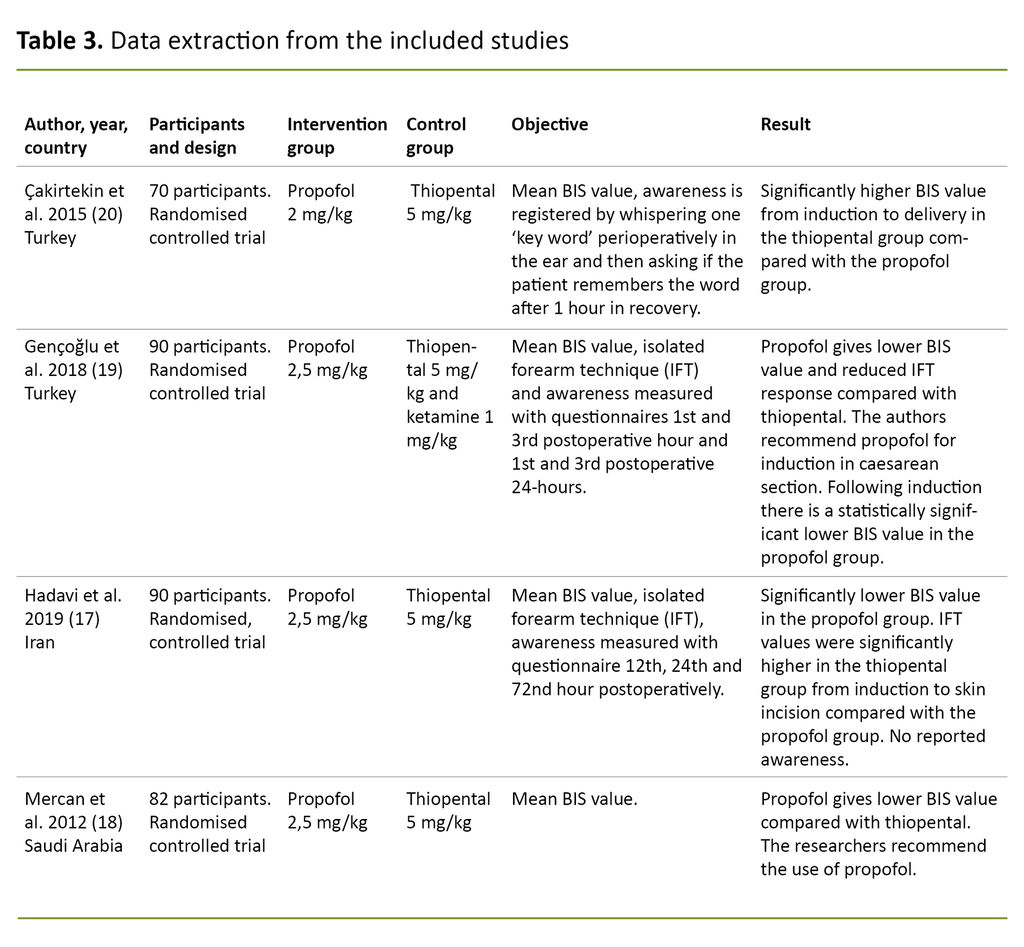
The following data were captured and systematised in the data extraction (see Table 3 for details): author, country, year, number of participants, study design, intervention, control, outcome and how the outcome was measured, as well as the result.
Analysis and classification of data
In order to classify and analyse the results from the included studies we carried out a meta-analysis, since we considered the studies to have low clinical heterogeneity (13) in relation to population characteristics, intervention and surgical procedure. The meta-analysis was carried out using Review Manager software (14).
Single studies may give rise to diverging results as a result of chance factors, so a meta-analysis can provide a more secure basis for establishing causal effects (15). Mean BIS values were extracted for the following measurement time points: induction, intubation, skin incision, uterine incision, delivery, uterine suture and skin suture. The measurement time points for BIS during a caesarean section were defined in the planning of the systematic review, following the identification of a relevant study in the pilot search.
The mean BIS-value is a continuous variable, and the mean difference (MD) was therefore calculated with a 95 per cent confidence interval (CI) and p-value (significance level ˂ 0.05), in order to measure the effect in the intervention group (propofol) versus the control group (thiopental) in each sub-group, as well as the total effect for the whole course of anaesthesia. We chose an inverse-variance, random-effects meta-analysis model (16). The findings are presented as a forest plot in Figure 2.
Results
We identified 4 441 references through systematic literature searches. Of these, 4 391 were excluded because the title and abstract did not meet the inclusion criteria, were duplicates of hits in other databases, were in languages we do not master, were not randomised controlled trials (RCTs) or lacked abstracts or full texts. Duplicates were removed manually.
Fifty articles were then read in full-text and assessed in accordance with the inclusion and exclusion criteria. In total, four RCTs fulfilled the criteria for meta-analysis. A total of 302 patients were included in the studies in the meta-analysis.
The included studies were carried out in Turkey, Iran, Saudi Arabia and Korea between 2012 and 2020. All the studies had been approved by a research ethics committee. All the studies included in the meta-analysis compared propofol and thiopental for induction of anaesthesia in caesarean section under general anaesthesia.
There were no significant differences in the number of participants in each group, the age of the participants, body mass index, gestational age of the foetus or the inclusion and exclusion criteria of the studies.
All participants were aged between 18 and 44 and assessed as healthy without functional limitations. The participants underwent elective caesarean section, and all were voluntary participants in the research. In all the studies the participants were randomly placed in groups, either with the help of a table or a data program.
Critical appraisal
Two of the articles have higher validity (17, 18) because they have a thorough description of method and randomisation compared with the articles by Gençoğlu et al. (19) and Çakırtekin et al. (20).
The participants in all four studies are described as being equally monitored and all the studies use BIS to measure sleep depth. The studies by Gençoğlu et al. (19) and Çakırtekin et al. (20) do not describe how the randomisation was carried out, only that the participants were randomised, while the studies by Hadavi et al.(17) and Mercan et al.(18) describe using a double-blind technique in relation to both participants and anaesthesia personnel.
There may be a greater risk of bias in the articles where there is no detailed description of how the participants were randomised. One may therefore have less faith in those articles (19, 20). All the four studies (17–20) are well described, and the method is approximately the same. This makes them well suited to a meta-analysis.
The effect of propofol versus thiopental on mean BIS values
Total effect measurements in the meta-analysis showed significantly lower BIS in the patients for whom anaesthesia was induced with propofol versus thiopental (MD –9.27; 95 per cent CI –11.32; –7.2), which indicates a significantly reduced danger that the patient may experience awareness.
If we look at effect in the various sub-groups, the findings are more varied and six of the sub-groups show effect in favour of lower BIS in patients who had induction with propofol, while the sub-group ‘skin suture’ does not show any significant difference between the groups. Below we present the findings for the various sub-groups.
The sub-group ‘induction’ shows lower BIS for the intervention group propofol (MD –5.47; 95 per cent CI –8.54; –2.40). If we look at mean BIS and standard deviation in the two studies addressing this sub-group, BIS is below 60 in the intervention and the control groups in both studies.
BIS values in the sub-group ‘intubation’ also show a significant difference between the propofol group and the thiopental group, but not as great a significance as ‘induction’ (MD –10.11; 95 per cent CI –16.73; –3.49). In one of the included studies, the patients who had induction with thiopental had mean BIS above 60 and were therefore at risk of awareness.
In the sub-groups ‘skin incision’ and ‘uterine incision’ the analysis shows major differences between the intervention and the control groups with, respectively, MD –10.57 (95 per cent CI –13.07; –8.07) for ‘skin incision’, and MD –12.9 (95 per cent CI –15.62; –10.8) for ‘uterine incision’.
The mean BIS value was once more above 60 in patients for whom anaesthesia was induced with thiopental in several of the studies we included in our analysis. On delivery of the child it becomes apparent that there is a highly significant difference between the groups. The mean difference here is –15.04 (95 per cent CI), and it is precisely in this comparison that we see the most significant difference between the groups. The mean BIS value was again over 60 in the control group in three of the included studies.
Following delivery of the child there is a smaller significant difference between the groups in the sub-group ‘uterine suture’ (MD –5.16; 95 per cent CI –8.34; –1.97), still in favour of the patients in whom anaesthesia was induced with propofol. In some of the patients who had induction with thiopental, the mean BIS was above 60.
In the final stages of surgery in the sub-group ‘skin suture’ the analysis does not show any significant difference between the two groups (MD –2.28; 95 per cent CI –8.11; 3.54). Here it is natural to envisage that the concentration of sevoflurane is the same in both groups, and that neither propofol nor thiopental are relevant components at that stage, hence no significant difference.
In the meta-analysis it is worth noting that the BIS value for some of the patients will be above 60 even in the intervention group, even though the mean BIS value is below 60. The calculation of heterogeneity in the meta-analysis shows a high degree of statistical heterogeneity between the studies, with a p-value of < 0.00001 and I² of 78 per cent, as shown in Figure 2.
The findings in the meta-analysis show significant differences in the mean BIS values between the groups at the measurement points of induction, skin incision, uterine incision and delivery, and we have great confidence in the estimates. The results in several of our sub-groups are in favour of the intervention group (propofol) and have effect estimates which do not cross the no-effect line (16). In the ‘skin suture’ sub-group, the result is not significant.
Discussion
The result of the meta-analysis in this systematic review indicates that the switch from thiopental to propofol for induction of anaesthesia in elective caesarean section may contribute to preventing awareness. Patients who had induction with propofol clearly had a lower BIS value compared to those who had induction with thiopental.
The findings from this systematic review show that the patients in whom anaesthesia was induced with thiopental had BIS values which put them in danger of experiencing awareness. The included studies involved elective patients, and this means a reduction in risk factors such as night shifts, urgency and limited time for preparation.
Thiopental increased the risk of awareness compared with propofol
The result from the sub-group analysis showed significantly higher BIS values from induction to delivery in the control group thiopental, something which corresponds to patient casuistics that report on awareness in this period (3).
The result is supported by Odor et al. (3), who found that thiopental had a four times greater risk of awareness compared with propofol. They suggest there may be a pharmacological basis for these observations and argue that there ought to be a specific rationale for using thiopental as an induction agent, rather than regarding it as a standard choice (3).
Even though awareness is a feared complication in caesarean section, there are several other factors that affect the mother and the child. For example, haemodynamic stability is important to ensure adequate oxygenation of the foetus.
The findings from our systematic review indicate that propofol is preferable for induction in elective caesarean section, as the risk of accidental awareness is reduced. However, it is not a given that propofol should be the first choice in emergency caesareans (1, 2). In emergency caesarean section where the mother is haemodynamically unstable, propofol can affect the haemodynamics of the mother to such a degree that it is no longer appropriate to use propofol as the sole medicament (8).
Several studies have mapped predisposing factors, situations and possible reasons for awareness without making any concrete proposals for changes in order to prevent the condition (1, 3, 4).
Lack of experience in the use of thiopental increases the danger of complications
In addition to lower BIS, there are other factors contributing to a possible recommendation to change from thiopental to propofol. According to Chaggar and Campbell (1), less experienced anaesthetists have little knowledge of the use of thiopental, and this has led to both overdosing and underdosing when using this substance. It has further resulted in cases where the pregnant woman becomes haemodynamically unstable or experiences accidental awareness.
Syringe swaps, due to the resemblance thiopental has to antibiotics, have also been described, as well as the fact that it is time-consuming to dilute thiopental in saline solution (1). In comparison, there is no need for propofol to be diluted in advance which saves time and makes it cheaper than thiopental (1, 7).
Midazolam in combination with propofol further reduces the risk of awareness
In the studies included in the meta-analysis, opioids were administered to patients following delivery. Opioids do not cause retrograde amnesia and do not have the same anxioltic properties as midazolam.
In the studies by Hadavi et al. (17) and Ok et al. (21), midazolam was administered to patients following delivery, which further reduced the BIS values. BIS values below 60 are shown to reduce the risk of intraoperative consciousness in populations with a high risk of awareness (18).
In a large, retrospective study, midazolam was administered to all patients following delivery and none of the patients experienced awareness (9). The findings from our review show that the BIS value was not below the recommended limit in the thiopental control group in three of the included studies, and that the risk of awareness was highest at delivery (18–20).
BIS monitoring ought to be standard in caesarean section
In an expert article, Chaggar and Campbell recommend that sleep depth is monitored as standard practice in caesarean section under general anaesthesia (1). This may indicate that the anaesthesia team needs to focus more closely on sleep depth, and that BIS monitoring should be standard practice in caesarean section (4, 18–20).
It is the task of anaesthesia personnel to regularly assess the level of consciousness and anaesthetic depth during surgery, for example, by observing the pupil diameter, cilia reaction by stroking the patient’s eyelashes, as well as blood pressure and pulse. In cases of high risk of accidental awareness, measuring the depth of sleep with BIS monitoring is recommended (22). Based on the findings in this study, the argumentation for measuring BIS during elective caesarean section is reinforced.¤
Updated research must be the basis of any change in practice
The shift from thiopental to propofol as anaesthesia for patients undergoing elective caesarean section was made as a result of research findings (1, 4, 7). Even if the evidence base for the induction agents’ effect on BIS is small, this meta-analysis supports a shift from thiopental to propofol. However, in order to achieve a more secure basis for the change there is a need for further robust studies, preferably randomised controlled trials.
It is important that the new research leads to changes and updates in procedures, and that the work of anaesthetic personnel is based on research as well as experience. The field of anaesthetics must be based on applied research, which implies using research directed at specific practical objectives or applications. It is easy to think that the more experience we gain the better we become. However, excellence in a specialist field is achieved by finding, assessing and using research-based knowledge in light of our experience in encounters with individual patients (23).
Methodical considerations
The search results were thoroughly reviewed several times to make sure we had not overlooked any relevant studies. We screened titles and abstracts manually as the number of hits was manageable. A university librarian helped us to structure searches and formulations in the PICO framework (24), and this is a strength of our study.
Data extraction from the various studies was carried out by two individuals independently of each other, who then discussed the results. This is another strength of our study (25). We did a critical review of the articles with the aid of the Norwegian Electronic Health Library’s checklist. Here we had the option of carrying out a risk-of-bias assessment. This involves creating a figure where the risk of bias is shown from green to red for each article, which was included in the meta-analysis. This helps to make it more visual for the reader.
The fact that we carried out a meta-analysis is a strength because the total findings are more precise. Only RCT reports were included in the meta-analysis (15). The weakness in only including RCTs is that the number of studies is limited (23). In order to maintain quality we have followed the manual of Cochrane Training. Guidance from a specialist with competence in this field who also went through the description of the result strengthens the analysis.
Implications for clinical practice and further research
This systematic review shows that BIS is lower with propofol compared to thiopental in elective caesarean section. In clinical practice the indication of using thiopental in preference to propofol for induction of general anaesthesia should therefore be considered.
This systematic review looks at the connection between thiopental or propofol and awareness, and calls for more research in this field. There is also a need for more research into midazolam administered in caesarean section, both in terms of whether it affects the child before delivery and how it affects the patient’s experience of awareness.
One of the risk factors of awareness is inexperienced personnel (3) and a lack of insight into the procedure of a caesarean section under general anaesthesia (26). In order to ensure better learning, simulation-based training and teaching can contribute to making the anaesthesia nurse better equipped to act in stressful situations. One important factor in the avoidance of awareness is BIS monitoring, which should also be used in this patient group to measure depth of sleep.
Conclusion
This systematic review shows that patients who have induction with propofol for general anaesthesia in elective caesareans have significantly lower BIS values than patients who had induction with thiopental. Patients who have induction with propofol in elective caesarean section may thus have a lower risk of experiencing accidental awareness under general anaesthesia.
However, this review includes only a small number of studies, and there is a need for more high-quality randomised controlled trials in order to achieve a more reliable conclusion. BIS monitoring is an evidence-based measure for monitoring sleep depth in patients, and it is therefore important for anaesthesia personnel to introduce this in patients undergoing elective caesarean section under general anaesthesia.
Our thanks to University Librarian June Audsdotter Stafsnes at Western Norway University of Applied Sciences for excellent guidance with literature searches. Thanks also to consultant anaesthetist Andreas Kurt Winkler for his expert opinion as well as advice on supporting literature and searches.
The authors report no conflicts of interest.
References
1. Chaggar R, Campbell J. The future of general anaesthesia in obstetrics. BJA Education. 2017;17(3):79–83. DOI: 10.1093/bjaed/mkw046
2. Brown J, Rahman R, Wilson S, Abir G. Accidental Awareness during General Anaesthesia (AAGA) in obstetrics. Obstetric Anaesthesia – tutorial 388. 2018. Available at: https://resources.wfsahq.org/wp-content/uploads/388_english-1.pdf (downloaded 18.10.2022).
3. Odor P, Bampoe S, Lucas D, Moonesinghe S, Andrade J, Pandit J, et al. Incidence of accidental awareness during general anaesthesia in obstetrics: a multicentre, prospective cohort study. Anaesthesia. 2021;76(6):759–76. DOI: 10.1111/anae.15385
4. Czarko K, Kwiatosz-Muc M, Fijalkowska A, Kowalczyk M, Rutyna R. Intraoperative awareness – comparison of its incidence in women undergoing general anaesthesia for Caesarean section and for gynaecological procedures. Anaesthesiol Intensive Ther. 2013;45(4):200–4. DOI: 10.5603/AIT.2013.0039
5. Folkehelseinstituttet. Medisinsk fødselsregister – Statistikkbank. Oslo: Folkehelseinstituttet; 2019. Available at: https://www.fhi.no/hn/helseregistre-og-registre/mfr/ (downloaded 18.10.2022).
6. Plaat F, Lucas N, Bogod DG. 16: AAGA in obstetric anaesthesia. In: NAP 5: Accidental awareness during General Anaesthesia in the United Kingdom and Ireland – report and findings. London: The Royal College of Anaesthetists; 2014. pp. 133–43. Available at: https://www.nationalauditprojects.org.uk/downloads/NAP5%20full%20report.pdf (downloaded 11.10.2022).
7. Desai N, Carvalho B. General anaesthesia for caesarean section: is the end in sight for thiopental? British Journal of Hospital Medicine. 2017;78(6):358. DOI: 10.12968/hmed.2017.78.6.358
8. Tumukunde J, Lomangisi DD, Davidson O, Kintu A, Joseph E, Kwizera A. Effects of propofol versus thiopental on Apgar scores in newborns and peri-operative outcomes of women undergoing emergency cesarean section: a randomized clinical trial. BMC Anesthesiology. 2015;15(1):1–6. DOI: 10.1186/s12871-015-0044-6
9. Park H-S, Kim Y-S, Kim S-H, Jeon A-R, Kim S-E, Choi W-J. Comparison of electroencephalogram between propofol-and thiopental-induced anesthesia for awareness risk in pregnant women. Scientific Reports. 2020;10(1):1–10. DOI: 10.1038/s41598-020-62999-5
10. Mathur S, Patel J, Goldstein S, Jain A. Bispectral Index. Treasure Island, Florida: StatPearls Publishing; 2020.
11. Polit DF, Beck CT. Nursing research: generating and assessing evidence for nursing practice. 11th ed. Philadelphia, Pennsylvania: Lippincott Williams & Wilkins; 2020.
12. Helsebiblioteket. 4.1 Sjekklister. Randomisert kontrollert studie. Kunnskapsbasertpraksis.no. Available at: https://www.helsebiblioteket.no/kunnskapsbasert-praksis/kritisk-vurdering/sjekklister (downloaded 02.06.2020).
13. McKenzie J, Brennan S, Ryan R, Thomson H, Johnston R. 9. Summarizing study characteristics and preparing for synthesis. I: Cochrane Handbook for Systematic Reviews of Interventions. Version 6.3. The Cochrane Collaboration; 2022. Available at: www.training.cochrane.org/handbook (downloaded 06.08.2020).
14. The Nordic Cochrane Centre. Review Manager (RevMan). Version 5.4.1. The Cochrane Collaboration; 2020. Available at: http://community.cochrane.org/tools/review-production-tools/revman-5 (downloaded 09.08.2020).
15. Christoffersen L, Johannessen A, Tufte PA, Utne I. Forskningsmetode for sykepleierutdanningene. Oslo: Abstrakt forlag; 2015.
16. Deeks J, Higgins J, Altman D. 10. Analysing data and undertaking meta-analyses. I: Cochrane Handbook for Systematic Reviews of Interventions. Version 6.3. The Cochrane Collaboration; 2022. Available at: www.training.cochrane.org/handbook (downloaded 09.09.2020).
17. Hadavi M-R, Beihaghi M, Zand F, Sabetian G, Azemati S, Asadpour E. A comparison between thiopental sodium and propofol for induction of anesthesia in elective cesarean section using bispectral index and isolated forearm technique: a randomized, double-blind study. Asian Journal of Anesthesiology. 2019;57(3):93–100. DOI: 10.6859/aja.201909_57(3).0004
18. Mercan A, El-Kerdawy H, Khalill M, Al-Subaie H, Bakhamees HS. A prospective, randomized comparison of the effects of thiopental and propofol on bispectral index during caesarean section till delivery of newborn. MEJ Anesth. 2012;21:699–704.
19. Gençoğlu NN, Küçükosman G, Aydın BG, Okyay DR, Pişkin Ö, Sezer Ü, et al. Effects of preoperative anxiety and general anesthetic administration on intraoperative awareness in patients undergoing cesarean section. Medical Bulletin of Haseki. 2019;57(2). DOI: 10.4274/haseki.galenos.2018.4480
20. Çakırtekin V, Yıldırım A, Bakan N, Çelebi N, Bozkurt Ö. Comparison of the effects of thiopental sodium and propofol on haemodynamics, awareness and newborns during caesarean section under general anaesthesia. Turkish Journal of Anaesthesiology and Reanimation. 2015;43(2):106. DOI: 10.5152/TJAR.2014.75547
21. Ok SJ, Kim WY, Lee YS, Kim KG, Shin HW, Chang MS, et al. The effects of midazolam on the bispectral index after fetal expulsion in caesarean section under general anaesthesia with sevoflurane. J Int Med Res. 2009;37(1):154–62. DOI: 10.1177/147323000903700118
22. Anestesisykepleierne NSF. Grunnlagsdokumentet for anestesisykepleiere. IFNA – International Federation of Nurse Anesthetists; 2016. Available at: https://www.nsf.no/sites/default/files/inline-images/zQCAUnQvcUEpG7XzVJXOgvrSk28s29K0m2gG4EZxhW7s5zspvF.pdf (downloaded 22.10.2022).
23. Nortvedt MW, Jamtvedt G, Nordheim LV, Reinar LM, Graverholt B. Jobb kunnskapsbasert! En arbeidsbok. Oslo: Akribe; 2012.
24. Område for helsetjenester i Folkehelseinstituttet. Slik oppsummerer vi forskning. Håndbok for Folkehelseinstituttet. 4. utg. Oslo: Område for helsetjenester i Folkehelseinstituttet; 2018.
25. Deeks JJ, Higgins JP, Altman DG. 10. Analysing data and undertaking meta-analysis. In: Cochrane Handbook for Systematic Reviews of Interventions. Version 6.3. The Cochrane Collaboration; 2022. Available at: https://training.cochrane.org/handbook/archive/v6.1/chapter-10 (downloaded 24.10.2022).
26. Norsk anestesiologisk forening, Den Norske legeforening, Anestesisykepleiernes landsgruppe av NSF. Norsk standard for anestesi. 2016. Available at: https://www.nsf.no/sites/default/files/inline-images/f99njXla94iCUrYGJrm8qOM6nRwJscUypCJQM9lEb1KJd752LN.pdf (downloaded 24.10.2022).










Comments