Registered nurses’ assessments of the ‘Four Habits Model’ course – a cross-sectional study
The registered nurses who participated in the ‘Four Habits Model’ communication skills course became more aware of asking open-ended questions, actively listening and structuring their conversations with patients.
Background: By training in specific skills, healthcare personnel can learn how to systematically communicate with patients and their families in the best way possible. The ‘Four Habits Model’ (4HM) was developed by Kaiser Permanente in the United States, and is a method for eliciting and seeking understanding of the patient's perspective, demonstrating empathy in patient care, ensuring that patients understand and remember information they are given, and involving patients in treatment decisions. As of 2021, the 4HM course is a standard part of the internal training at seven Norwegian hospitals, both for doctors and as an interdisciplinary course.
Objective: The purpose of the study was to investigate whether registered nurses (RNs) felt that the course had improved their communication skills and changed how they communicate with patients.
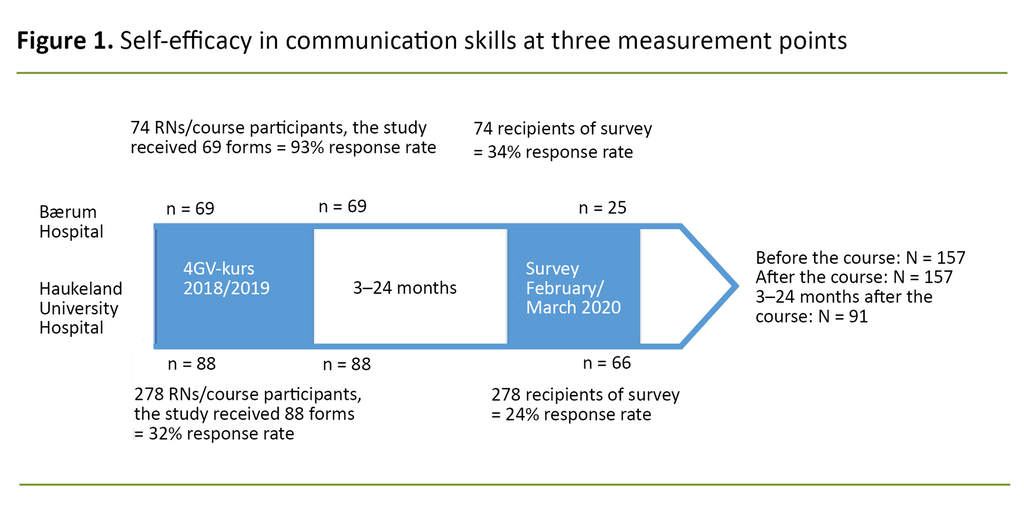
Method: The study consisted of a descriptive cross-sectional study and a follow-up evaluation of self-efficacy in communication before and after a two-day interdisciplinary 4HM course. We used two different data collection methods: Sub-study 1: evaluation of 157 RNs from Bærum Hospital and Haukeland University Hospital via a questionnaire about self-efficacy in communication skills before and after participation in a 4HM course. Sub-study 2: a detailed online questionnaire completed 3–24 months after participation in a 4HM course. A total of 91 RNs from the two hospitals responded to the online questionnaire.
Results: Analysis of both studies shows that the 4HM course improved the RNs’ communication skills and led to changes in how they communicated with patients. The changes became an integral part of the RNs’ practice and particularly related to being aware of the patient’s perspective by asking open-ended questions, actively listening and structuring conversations with the patient. All four habits seem to be more or less equally useful. The RNs called for the course to be repeated and for implementation of the method to be more widespread.
Conclusion: The findings in this study show that a two-day interdisciplinary communication skills course covering 4HM improved RNs’ communication skills, and consequently led to changes in how they communicated in the clinical setting.
Communication has been described as the cornerstone of nursing (1) and something that permeates all elements of professional practice – from Kari Martinsen's description ‘to see with the heart’s eye’ (2) to calls for greater patient involvement in decisions about their treatment (3).
RNs need to be adept at communication in the clinical setting, show empathy and communicate in a professional manner. This involves professional, patient-oriented and healthy communication (1) that is adapted to the patient's ability to give and receive information (4).
We know that patient satisfaction and compliance are improved when healthcare personnel successfully convey information to patients about their diagnosis, cause of illness and expected duration of symptoms in a way that they understand it. This also leads to better follow-up of treatment and reduces the risk of patients receiving the wrong treatment (5–8).
As nurses, we experience situations where we feel safe and competent in conversations, but there are also times when communication is difficult. This could relate to, for example, conversations aimed at increasing patient involvement that require planning and knowledge about the patient, or conversations where the patient is emotional and the nurse needs to demonstrate empathy.
Many patients find it easier to ask difficult questions when healthcare personnel know them as a person, show empathy and appear to be dependable. Consequently, showing empathy is one of the most impactful interactions a healthcare professional can engage in (9-11).
Patient involvement is more difficult when multiple people are involved in the decision-making, and when this takes place over a period of time that extends beyond one consultation or conversation (12). This is particularly challenging in cases of acute illness (13), and requires close cooperation within the treatment team (14).
RNs in Norway have called for more communication skills training (15). Historically, communication has been perceived as a personal quality, but today it is regarded as a skill that can be taught (16-18).
In order for communication skills training to be successful in large organisations, standardised training of the instructors is vital, as is prioritisation at the organisational level (11, 19).
The ‘Four Habits Model’ (4HM)
The 4HM and communication skills course was developed for the private American healthcare company Kaiser Permanente in 1999. The aim of 4HM is for healthcare personnel to consciously and subconsciously incorporate communication patterns and habits into clinical practice (16). The course is based on four good habits for communication between healthcare personnel and patients:
- Habit 1: Invest in the beginning
- Habit 2: Elicit the patient’s perspective
- Habit 3: Demonstrate empathy
- Habit 4: Invest in the end
The goal is to improve patient satisfaction and compliance with treatment, and reduce the number of complaints and conflicts (20). The course is held over two days and includes both plenary sessions and group work involving role play. 4HM was originally designed for doctors, and an observational study of the course in the United States showed a positive effect on both patient and doctor satisfaction (6).
The course was adapted for the Norwegian setting by Pål Gulbrandsen and Arnstein Finset, and studies in Norway have shown improved communication skills and self-efficacy among doctors following participation in the course (20, 21). 4HM was originally structured around an imaginary medical consultation with a patient who was able to explain their views and needs.
The instructors at the various hospitals were largely responsible for adapting the course for an interdisciplinary group of participants. Although the template for the course remains the same, the content and the emphasis have been adapted as necessary for the target group.
There are few international studies into the impact of 4HM on nurses, and no such studies have been conducted in Norway. An American study shows that nurses derive benefit from the method even after only one hour of training (22), while an African study concludes that nursing and midwifery students do not demonstrate more empathy as a result of participating in the course (23).
Studies into similar communication skills courses show increased self-efficacy in communication skills (24–26). More studies are therefore needed to investigate the benefits of the 4HM course for RNs.
As of 2021, the 4HM course is a standard part of the internal communication skills training at seven Norwegian hospitals: Diakonhjemmet Hospital, Akershus University Hospital, Vestfold Hospital, Telemark Hospital, the University Hospital of Northern Norway and the hospitals in this study: Bærum Hospital and Haukeland University Hospital.
Both hospitals train their own instructors and have been running courses since 2015. They hold interdisciplinary courses, and about 60% of the participants are RNs. The course had to be adapted to change the emphasis from doctor consultations and doctor-patient conversations to different types of patient contact with other occupational groups and hospital staff.
Both hospitals use standard evaluation forms before and after the courses, and we have been able to use these in this study to compare the RNs’ self-efficacy in communication skills.
Objective
The purpose of the study was to investigate whether RNs who took part in a two-day interdisciplinary 4HM course improved their communication skills, applied the method in the clinical setting and consequently experienced a change in how they communicated with patients. To answer this, the two sub-studies measured self-efficacy in communication skills at three points in time (sub-studies 1 and 2) and whether the course is adapted to RNs working in different parts of the hospital (sub-study 2).
Method
Design
In the study, we used two data collection methods: a pre–post study that shows results before and after participation in a 4HM course (sub-study 1), and a cross-sectional study in which we obtained data 3–24 months after participation in a 4HM course (sub-study 2). The study was designed to describe change and explore correlations based on participants’ self-reported perceptions, attitudes, behaviours, experiences and preferences (27).
Sample
All RNs working at Bærum Hospital and Haukeland University Hospital in the spring of 2020, and who had taken part in 4HM in the period 2015–2019, were invited to participate. Due to a very low response rate from course participants in 2015–2017, we only used the responses from 2018 and 2019 in the study, which means that the respondents were asked about their self-efficacy in communication skills 3–24 months after taking the course.
Both groups are made up of the same population (RNs working at the hospital in the period 2018–2019), but it is not necessarily the same nurses who completed the questionnaire in both data collection rounds (Figure 1).
Data collection
Sub-study 1: The study included anonymous data that were collected during ongoing monitoring by both hospitals immediately before and after participation in the courses. These data were collected in the period 2018–2019.
Sub-study 2: The data were collected in the period 25 February to 19 March 2020 by means of an anonymous questionnaire. We sent invitations by e-mail to the employers, and submission of the questionnaire was considered to indicate the respondents’ informed consent. At the end of February 2020, both hospitals were under pressure due to the COVID-19 pandemic, and the data collection came to an end much sooner than we had planned.
We have used four identical statements from sub-studies 1 and 2 to compare self-efficacy in communication skills before, immediately after and 3–24 months after participation in the course.
The questionnaire in sub-study 2 was produced using the online data collection tool Nettskjema (28). The questionnaire was based on two forms that were developed to evaluate the communication skills course 4HM: ‘Long-term effect of communication training on the relationship between physicians’ self-efficacy and performance’ (21) and the evaluation form from sub-study 1 used before and after participation in the course (Appendix 1 – only Norwegian).
The questionnaire consisted of 23 questions about the effectiveness of particular elements of the training course, their benefit in the clinical setting, self-efficacy in communication skills, whether the respondents found that they changed how they communicated after the course, and whether communication skills courses can improve the communication with patients.
The data we collected also included socio-demographic variables: hospital and ward employed in, date of course participation, previous experience before taking the course, and a focus on the ‘Four Habits Model’ used in the clinical setting.
Twenty of the questions were set out as matrix questions, with answer alternatives based on a 10-point Likert scale. Communication skills were measured in statements under the question ‘How sure are you that you can successfully perform each of the following tasks?’, with answer alternatives on a scale from 1–10 (1 = not at all sure, 10 = very sure).
We compared four identical statements in sub-studies 1 and 2, and used Cronbach’s alpha to test the internal consistency of the questionnaire. Total α = 0.90, which indicates high covariation and good internal reliability (29). A pilot questionnaire was tested on six RNs who had participated in a 4HM course at hospitals other than Bærum or Haukeland.
Data analysis
The data were analysed using SPSS Statistics 26 software.
The results from sub-study 1: the data did not meet the criteria for normal distribution. We therefore used the Wilcoxon signed-rank test to examine changes in the respondents’ self-efficacy in communication techniques on a sliding scale, before and immediately after participation in the 4HM course.
The results from sub-study 2: categorical variables were measured in chi-square tests. The results are presented as descriptive statistics, numbers and percentages. Two questions had open answer alternatives to enable respondents to elaborate on how and why their communication might have changed, and one question provided an opportunity to give additional feedback.
Ethical considerations
Prior to the study, we considered the ethics in respect of the data collection, and we conducted the surveys in accordance with ethical principles of confidentiality, informed consent and safeguarding the integrity of research subjects (27).
We used online questionnaires and did not consider the questions to be triggering. The responses were anonymised. We therefore deemed the study to be in line with ethical conventions for quantitative research.
The study was approved by the Norwegian Centre for Research Data (project number 857834), the University of Oslo and the management and data protection officer at Bærum Hospital and Haukeland University Hospital.
It is important to emphasise that the study analyses changes that have taken place after the course, and not the work or efforts of individuals (27). In order to protect the privacy of respondents, all results are presented in aggregate form, and the courses and hospitals are assessed as a whole.
The first author is a clinical nurse educator with experience from medical wards, and is an instructor on the 4HM course. Prior understanding includes knowledge of teaching and implementation of 4HM.
Results
In sub-study 1, a total of 157 evaluation forms (69 from Bærum and 88 from Haukeland) were completed by the participants immediately before and after participation in a 4HM course in the period 2018–2019.
In sub-study 2, we sent an e-mail with a link to an online questionnaire to a total of 352 RNs, 91 (26 per cent) of whom responded. Of these, 66 were working at Haukeland University Hospital (response rate of 24 per cent) and 25 were employed at Bærum Hospital (response rate of 34 per cent).
Background variables from sub-study 2
The breakdown of respondents was as follows: 29 in wards, 21 in outpatient clinics, 7 worked in more than one unit or department, 1 worked in the accident and emergency department, 11 worked in surgical/intensive care units and 19 worked in other areas, including substance use, psychiatry and maternity care.
Three respondents did not provide information about their workplace. A total of 77 respondents had over five years of experience as a nurse at the time of taking the 4HM course, 13 had two to five years of experience, and 1 had less than one year of experience.
Change in communication technique after taking the course (sub-study 2)
The main question in the survey was whether the RNs had experienced a change in how they communicated after taking the course. A total of 77% answered ‘Partly’ or ‘Yes’ to this question. Among the respondents working in wards and outpatient clinics, 87% answered ‘Partly’ or ‘Yes’, and the corresponding figure for RNs working in accident and emergency departments, surgical and intensive care units was 58%.
Respondents from wards and outpatient clinics tended to report a greater change in communication (partial or complete change) than those from accident and emergency departments and intensive care units or those who worked in more than one department (X2 = 7.2, p = 0.07).
As many as 92% indicated that they remembered the habits they had learned 3–24 months after taking the 4HM course, and 99% thought that the course had improved their communication skills. When asked if they discussed the course at work, 75% answered ‘Partly’ or ‘Yes’.
99% thought that the course had improved their communication skills.
A statistically significant correlation was observed between discussing the 4HM course at work and a change in communication 3–24 months after the course. As many as 87% of those who indicated that they discussed the course at work, reported a change in their style of communication, and the corresponding figure for those who did not discuss the course was 45% (X2 = 16.19, p <0.001).
Twenty-one respondents answered ‘No’ when asked if there had been a change in their communication. Nineteen of these had more than five years of experience at the time of the course, and all believed that taking such a course can improve communication skills.
In the open-ended questions, 10 of the 21 respondents indicated no change in their communication because they were already applying the skills from the course, and that the course confirmed that they had good communication skills.
The significance of the four habits and teaching methods (sub-study 2)
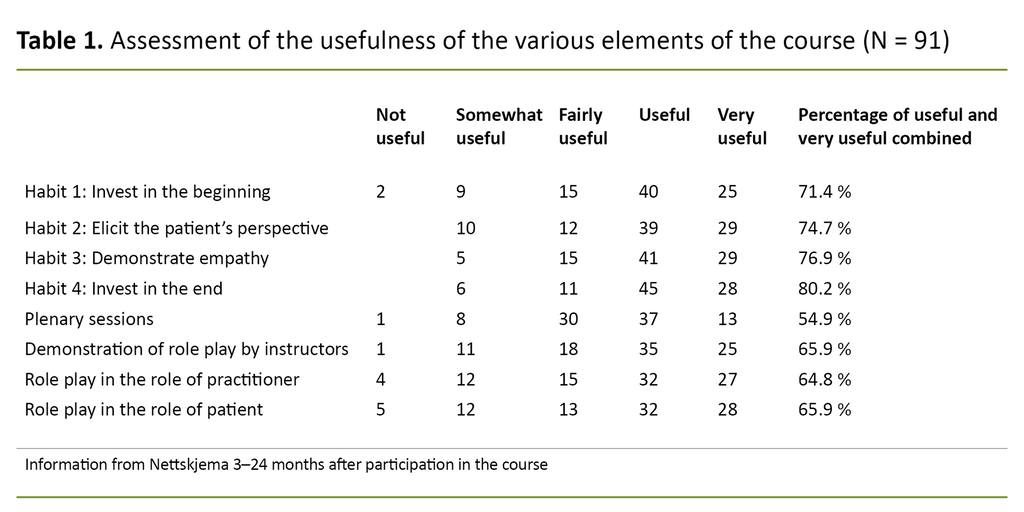
Between 71.4% and 80.2% of the respondents considered the four habits to be useful or very useful, while ‘investing in the end’ and ‘eliciting the patient’s perspective’ received the highest scores. The assessment of the usefulness of the various teaching methods used in the course showed that role-playing was considered more beneficial than plenary sessions (Table 1).
Working with patients after the course and practical benefits of 4HM (sub-study 2)
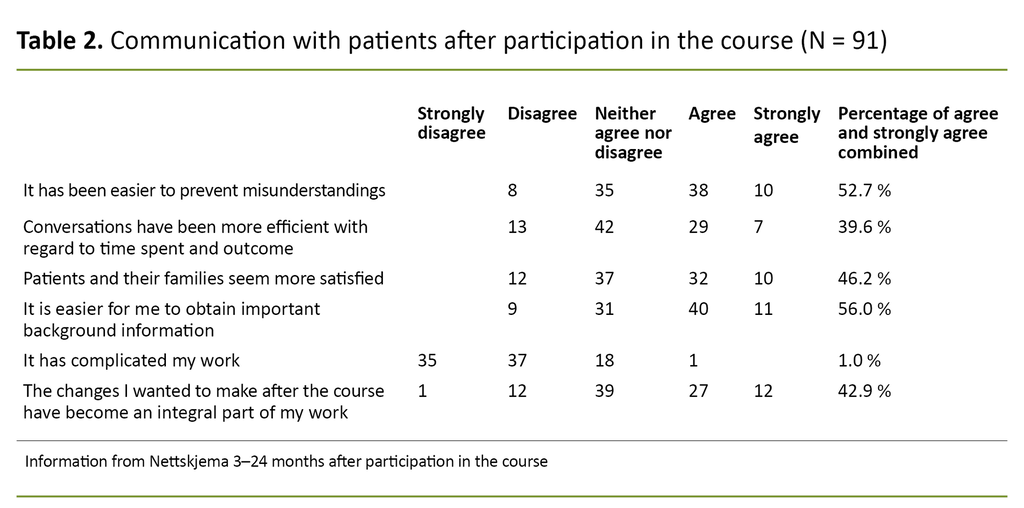
As shown in Table 2, more than half of the respondents indicated that it was easier to prevent misunderstandings in their communication with patients 3–24 months after participation in the 4HM course. It was also easier to obtain important background information, and the patients and their families seemed more satisfied. Only one respondent thought that 4HM had made their work more complicated (Table 2).
Self-efficacy in communication skills (sub-studies 1 and 2)
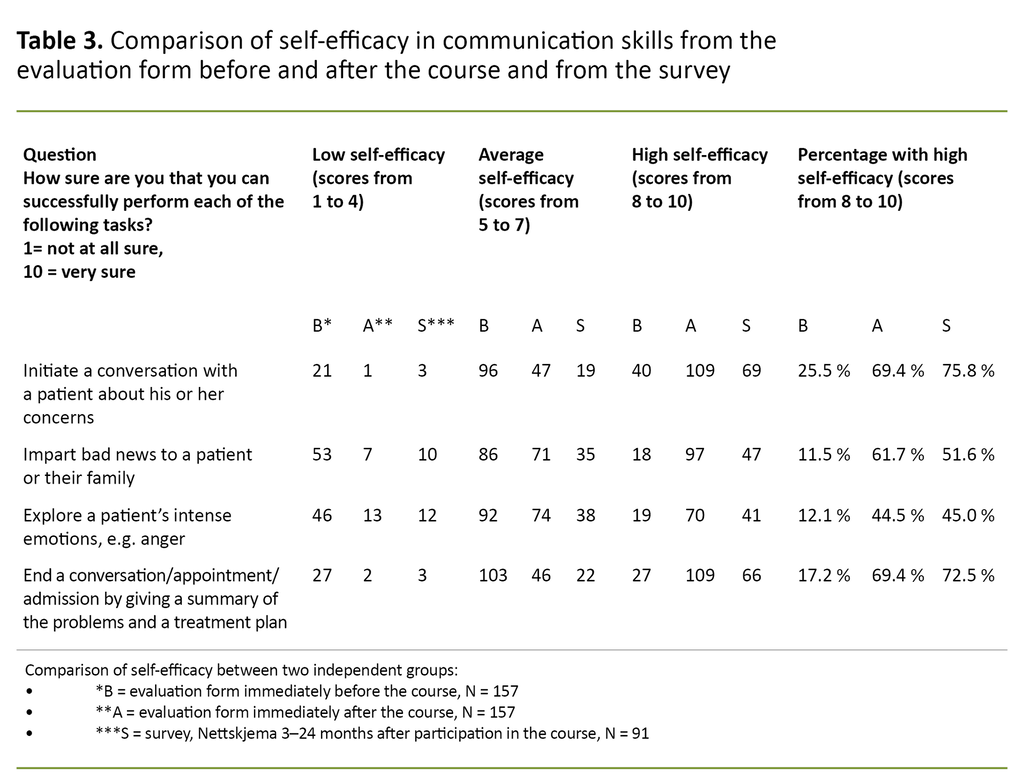
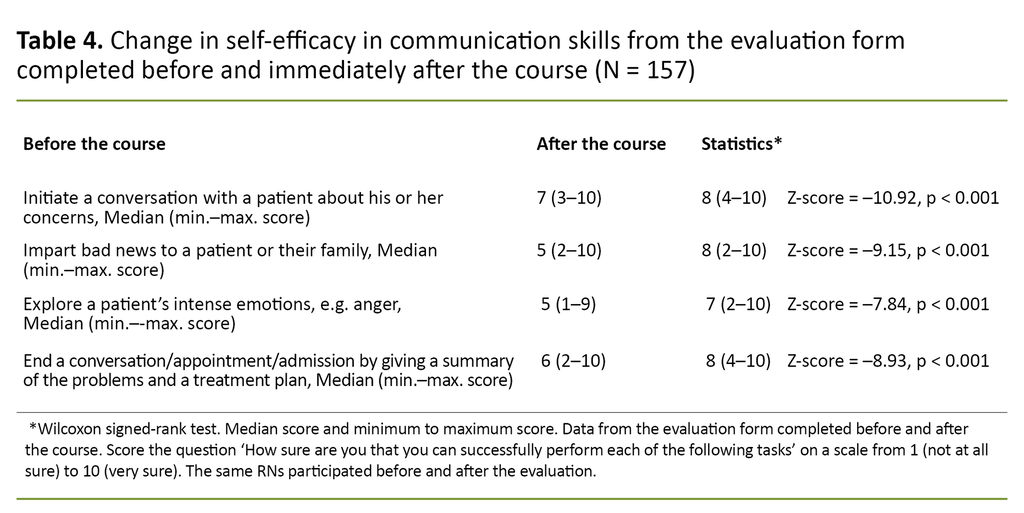
The respondents considered their communication skills to be significantly improved after taking the 4HM course (Tables 3 and 4). Respondents reported that taking the course had taught them skills in initiating a conversation with a patient about his or her concerns, skills in imparting bad news to a patient or family, skills in exploring patients’ intense emotions and competence in dealing with treatment plans.
Sub-study 2 also shows increased self-efficacy in communication skills 3–24 months after the course.
Responses to open-ended questions 3–24 months after the course (sub-study 2)
When asked how their communication had changed, a total of 60 respondents indicated that they applied elements of all the habits, and particularly ‘eliciting the patient’s perspective’ (n = 23). Eight reported a change in their conversation structure, and 18 listed a minimum of two elements from more than one habit.
Most indicated that they have become more aware of their own communication, and that they recognise the benefit of using the method.
A total of 74 respondents answered an open-ended question about why they had changed their way of communicating. Most indicated that they have become more aware of their own communication, and that they recognise the benefit of using the method. The last open-ended question provided an opportunity for other feedback. A total of 42 RNs answered this question, with 23 calling for the course to be repeated and/or for implementation of the method to be more widespread.
Discussion
In recent years, RNs at several Norwegian hospitals have had the opportunity to take the 4HM course. We therefore wanted to investigate whether there was any change in RNs’ own assessments of their communication skills.
We did this by asking questions about self-efficacy in communication skills before and after the course, whether the course content is adapted for RNs, as well as prioritisation at the organisational level. This is the first Norwegian study to examine the effect of the 4HM course on RNs’ communication skills.
‘Has your communication technique changed…?’ (sub-study 2)
A total of 77% indicated that they had changed how they communicate after the course. Those who reported otherwise explained that they were already using the communication skills taught on the course. Thus, 88% of the RNs were using the ‘Four Habits Model’ or something similar in their communication with patients and families 3–24 months after the 4HM course.
One RN explained why she changed her communication technique: ‘I changed my way of communicating because I realised that small adjustments can make a big difference in my contact with patients’ (RN 1).
RNs in wards and outpatient clinics indicated a greater change in their communication technique after the course than RNs working in anaesthesia, intensive care or surgical units. The reason for this disparity is not apparent in the study, but as an 4HM course instructor, the first author is familiar with this problem.
The findings of the study may be an indication that the course has not yet been sufficiently adapted for RNs working in certain areas.
Some RNs, e.g. surgical nurses, have found it difficult in the past to identify realistic situations from their own practice that they can use in role-playing for habit 2, ‘elicit the patient’s perspective’, and habit 4, ‘invest in the end’.
In order to benefit from the course, it is important that the role-play scenario is realistic with regard to the participant’s clinical practice and is adapted to their specific competence (25). The findings of the study may be an indication that the course has not yet been sufficiently adapted for RNs working in certain areas.
In order for the training to have a positive effect, courses and training must be prioritised at the organisational level (19). The study finds a significant correlation (p <0.001) between discussing 4HM at work and changes in communication techniques after participation in the course.
As one nurse wrote: ‘It is difficult to make changes on my own, it would have been easier if the entire ward was involved’ (RN 2). It is therefore a positive sign that 69 of the 91 nurses answered ‘Partly’ or ‘Yes’ when asked if they discuss or work with 4HM in the clinical setting.
It is not clear from the study whether this is person-dependent or system-dependent, but discussing the course in the workplace does seem to increase the positive effect of 4HM and help ensure that the skills are maintained over time.
Self-efficacy in communication skills before, immediately after and 3–24 months after 4HM course
The findings of this study suggest that the 4HM course improves participants’ communication skills, and that these effects last for up to two years after the course. Our research findings are in line with a Danish study (n> 1000) by Wolderslund et al. (26), which found that the improvement in communication skills following participation in a communication course was still being seen six months after the course (26).
The findings of this study suggest that the 4HM course improves participants’ communication skills, and that these effects last for up to two years after the course.
Although the effect was somewhat reduced six months after the course compared with immediately after the course, the participants still scored significantly higher in the follow-up compared to before the course. The study by Wolderslund et al. (26) included a broader group of participants than our study; in addition to nurses it also consisted of doctors, student nurses, chiropractors and physiotherapists.
Wolderslund et al. (26) observed a greater post-course improvement in communication skills among nurses and physiotherapists than among the other occupational groups. This may be an indication that communication courses such as 4HM are particularly beneficial for nurses.
Strengths and limitations of the study
This is the first Norwegian study to examine the long-term effect of a 4HM course on RNs in Norway. The study has three measurement points: immediately before, immediately after and 3–24 months after participation in the course.
Several Norwegian hospitals offer 4HM courses, and the study’s findings on the practical benefits that can be gained from the course and the potential for further development may therefore have clinical value. We also consider it a strength that RNs from two different regional health authorities participated.
The low response rate was a weakness of the study. In sub-study 2, only 26% submitted a completed questionnaire. This reduces the external validity of the study and the statistical power of the analyses (27). Combining the questionnaire with patient interviews or an observational study may have been a better option.
Another weakness of the study is that, despite all participants being RNs at two hospitals (Bærum or Haukeland), it was not necessarily the same RNs who participated in sub-studies 1 and 2.
Conclusion
The findings from the study show that interdisciplinary courses on the ‘Four Habits Model’ lead to improvements in RNs’ communication skills and changes in their communication with patients. RNs find that applying the ‘Four Habits Model’ can make it easier to obtain important background information and avoid misunderstandings, and patients seem more satisfied.
The instructors seem to have successfully adapted the course for interdisciplinary groups of participants, but there is still potential for improvement, particularly with regard to specialist nurses in anaesthesia, intensive care or surgical wards.
RNs have called for the course to be repeated, and the study finds that it would be beneficial to repeat the course or hold a supplementary course covering skills in dealing with strong emotions and demonstrating empathy. The results support the idea that an interdisciplinary course on the ‘Four Habits Model’ is a good way of improving RNs’ communication skills over time.
We would like to thank all of the RNs who took part in this study.
References
1. Eide H, Eide T. Kommunikasjon i relasjoner – personorientering, samhandling, etikk. Oslo: Gyldendal Norsk Forlag; 2017.
2. Martinsen K. Øyet og kallet. Bergen: Fagbokforlaget; 2000.
3. Elwyn G, Edwards A, Thompson R. Shared decision making in health care. Achieving evidence-based patient choice. 3rd ed. Oxford: Oxford University Press; 2016.
4. Lov 2. juli 1999 nr. 63 om pasient- og brukerrettigheter (pasient- og brukerrettighetsloven). Available at: https://lovdata.no/dokument/NL/lov/1999-07-02-63?q=pasient-%20og%20brukerrettighetsloven (downloaded 07.10.2019).
5. Jackson JL, Chamberlin J, Kroenke K. Predictors of patient satisfaction. Social Science & Medicine. 2001;52(4):609–20. DOI: 10.1016/s0277-9536(00)00164-7
6. Stein T, Frankel RM, Krupat E. Enhancing clinical communication skills in a large healthcare organization: a longitudinal case study. Patient Education and Counseling. 2005;58(1):4–12. DOI: 10.1016/j.pec.2005.01.014
7. Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3(1):e001570. DOI: 10.1136/bmjopen-2012-001570
8. Lang EV. A better patient experience through better communication. Journal of Radiology Nursing. 2012;31(4):114–9. DOI: 10.1016/j.jradnu.2012.08.001
9. Kennedy DM, Fasolino JP, Gullen DJ. Improving the patient experience through provider communication skills building. Patient Experience Journal Article. 2014;1(10). DOI: 10.35680/2372-0247.1009
10. Frankel RM, Beckman H. «Won’t you be my doctor?»: four keys to a satisfying relationship in an increasingly virtual world. Journal of Patient Experience. 2020;7(6):851–5. DOI: 10.1177/2374373520957184
11. Gulbrandsen P, Finset A. Skreddersydde samtaler – en veileder i medisinsk kommunikasjon. Oslo: Gyldendal Akademisk; 2014.
12. Ofstad EH, Frich JC, Schei E, Frankel RM, Benth JS, Gulbrandsen P. Clinical decisions presented to patients in hospital encounters: a cross-sectional study using a novel taxonomy. BMJ Open. 2018;8:e018042. DOI: 10.1136/bmjopen-2017-018042
13. Kvangarsnes M, Hole T, Bårdsgjerde EK, Landstad BJ. Pasientmedverknad ved akutt sjukdom – ein metasyntese av pasient- og helsepersonellerfaringar. Michael. 2020;17(24):77–93.
14. Oxelmark L, Ulin K, Chaboyer W, Bucknall T, Ringdal M. Registered nurses' experiences of patient participation in hospital care: supporting and hindering factors patient participation in care. Scandinavian Journal of Caring Sciences. 2018;32(2):612–21. DOI: 10.1111/scs.12486
15. Vareide PK, Hofseth C, Norvoll R. Stykkevis og helt – sykepleieres arbeidsoppgaver, kompetanse og yrkesidentitet i sykehus. Trondheim: SINTEF Unimed Helsetjenesteforskning; 2001. Rapport STF78 A013406. A6677.
16. Frankel RM, Stein T. Getting the most out of clinical encounter: the four habits model. The Permanente Journal. 1999;3(3):79–89. DOI: 10.7812/TPP/99-020
17. Tjora A. Den moderne pasient. Oslo: Gyldendal Akademisk; 2008.
18. De Haes H, Bensing J. Endpoints in medical communication research, proposing a framework of functions and outcomes. Patient Education and Counseling. 2009;74(3):287–94. DOI: 10.1016/j.pec.2008.12.006
19. Ammentorp J, Bigi S, Silverman J, Sator M, Gillen P, Ryan W, et al. Upscaling communication skills training – lessons learned from international initiatives. Patient Education and Counseling. 2020;104(2):352–9. DOI: 10.1016/j.pec.2020.08.028
20. Jensen BF, Gulbrandsen P, Dahl FA, Krupat E, Frankel RM, Finset A. Effectiveness of a short course in communication skills for hospital doctors: result of a crossover randomized controlled trial (ISRCTN22153332). Patient Education and Counseling. 2010;84(2):163–9. DOI: 10.1016/j.pec.2010.08.028
21. Gulbrandsen P, Jensen BF, Finset A, Blanch-Hartigan D. Long-term effect of communication training on the relationship between physicians’ self-efficacy and performance. Patient Education and Counseling. 2012;91(2):180–5. DOI: 10.1016/j.pec.2012.11.015
22. Fisher MJ, Broome ME, Friesth BM, Magee T, Frankel RM. The effectiveness of a brief intervention for emotion-focused nurse-patient communication. Patient Education and Counseling. 2014;96:72–8. DOI: 10.1016/j.pec.2014.04.004
23. Alhassan M. Effect of a 2-day communication skills training on nursing and midwifery student’s empathy: a randomized controlled trial. BMJ Open. 2019;9:e023666. DOI: 10.1136/bmjopen-2018-023666
24. Falch AL, Stubberud D-G, Gabrielsen AK, Karlsen M-MW, Leopolder ÅHM. Bedre pleie etter kommunikasjonskurs. Sykepleien. 2015;103(4):64–6. DOI: 10.4220/Sykepleiens.2015.53651
25. Gabrielsen AK, Karlsen M-MW, Falch AL, Stubberud D-G. Communication training course with simulation. Sykepleien Forskning. 2016;2(11):184–92. DOI: 10.4220/Sykepleienf.2016.57832en
26. Wolderslund M, Kofoed P-E, Ammentorp J. The effectiveness of a person-centered communication skills training programme for the health care professionals of a large hospital in Denmark. Patient Education and Counseling. 2020;104(26):1423–30. DOI: 10.1016/j.pec.2020.11.018
27. Polit DF, Beck CT. Nursing research: generating and assessing evidence for nursing practice. 10th ed. Philadelphia: Wolters Kluwer; 2017.
28. Universitetet i Oslo. Nettskjema. Oslo: Universitetet i Oslo; s.a. Available at: https://www.uio.no/tjenester/it/adm-app/nettskjema/ (downloaded 16.09.2021).
29. Pallant J. SPSS survival manual. 3rd ed. Maidenhead: Open University Press; 2007.
30. Riskin A, Erez A, Foulk TA, Riskin-Geuz K, Ziv A, Sela R, et al. Rudeness and medical team performance. Pediatrics. 2017;139(2):e20162305. DOI: 10.1542/peds.2016-2305










Comments