Reported competence enhancement from participation in resource nurse cancer and palliative care networks
Participation in cancer and palliative care networks increased the registered nurses’ competence. Staff exchange training schemes and frequent participation in clinical practice days were also highly beneficial.
Background: Norwegian authorities recommend the establishment of competence networks for resource nurses in cancer and palliative care and such networks have been set up in all the regional health authorities. Networks are assumed to enhance competence, but the specific benefits are not known.
Objective: To examine the extent to which the networks provide competence enhancement in the form of knowledge, skills and general competence in exercising the role of resource person in palliative care for patients and their families, and colleagues.
Method: Descriptive cross-sectional design. We devised an electronic questionnaire based on the networks’ framework documents and earlier research. Self-reported competence enhancement was assessed for 107 registered nurse from hospitals, nursing homes and community nursing services. They were members of three different competence networks in the South-Eastern Norway Regional Health Authority. Recruitment took place via local network leaders. We analysed the data using descriptive statistics.
Results: The registered nurses reported that in general, their competence was greatly enhanced through network participation. There were no significant differences between the various levels of the health service as regards the reported benefits. Staff exchange training schemes and frequent participation in group sessions were associated with greater competence enhancement.
Conclusion: The members reported that network participation resulted in competence enhancement in key areas. The results can inspire further work as well as greater participation in the networks, and future research could focus on the resource nurse’s role as local knowledge disseminator.
Competence networks for resource nurses in cancer and palliative care have been established in all Norwegian regional health authorities. They involve one or two registered nurses (RNs) from the community nursing service and most of the units in hospitals and nursing homes that provide care for seriously ill and dying patients. The combined nationwide membership of local networks is over 2000 (1).
The aim of a network is to enhance competence at all levels of the health service and improve interaction, thereby achieving improved services for patients and their families (2). The members of the networks are to act as local resource persons for patients and their families, and for colleagues. In order to equip them for this task, they are invited to attend clinical practice days and are encouraged to stay in contact with each other at other times (1).
Recommendations for network organisation, operation and competence-related content are made by the regional advisory units for palliative care in the four health regions (3, 4), while the networks are managed and operated locally by the regional health authorities.
The South-Eastern Norway Regional Advisory Unit for Palliative Care recommends annual sessions of altogether 18 hours in addition to a six-hour introductory course for new members (4). Such networks are recommended in leading publications on palliative care (1, 2, 5).
What is palliative care?
Palliative care is characterised by patient-centred care and palliation, with improved quality of life as the main goal. This approach should be integrated into the care provided at all stages of the illness (1). Seriously ill and dying patients are treated in a variety of institutions, and competence in basic palliative care is required in all units and at all levels (1, 6).
Although the need for specialised palliative expertise will increase at all levels in the years ahead, this applies particularly to the primary health care service, since the goal is for more patients to be treated at home and fewer hospitalisation days (1, 7).
The Norwegian Directorate of Health describes professional competence as being composed of knowledge, skills and attitudes (2). Descriptions of learning outcomes in ‘The Norwegian qualifications framework for lifelong learning’ are similarly categorised, and such factors as ethics, societal knowledge and attitudes are also spoken of as general competence (8). We will use this expression in the article from now on.
One of the objectives of the networks is to promote more interaction between the members. From a sociocultural learning perspective, social interaction and a sense of community with others constitute a good starting point for learning (9).
Lev Vygotskij asserted that learning takes place in social interaction with others through exchanging thoughts, ideas, knowledge and experiences. He believed that active participation is the key to the learning process, and that language and communication skills are our most important tools in achieving this (9, 10).
Earlier research
Two interview studies and one evaluation of the palliative network in the Western Norway Regional Health Authority have been conducted previously (11–13). In addition, the network was evaluated in SINTEF’S evaluation report of the provision of services to people requiring palliative care (5). It has been shown that resource nurses assert that participation in the network increases their competence, but we lack knowledge about specific learning outcomes (5, 11–13).
The members find it difficult to distinguish between the competence they have gained through the network, and what they have acquired elsewhere. Another subject of debate is whether the group sessions could lead to the furtherance of malpractice (13).
Considerable resources are used on the networks, by those who manage them and those who send RNs to participate in the group sessions. More knowledge about the experiences of professional networks in palliative care is advisable (14). We have not found any mention of similar networks internationally.
The objective of the study
The objective of the study was to examine the extent to which the network provides enhanced competence in the form of knowledge, skills and general competence that help resource nurses at all levels of the health service perform their role as a resource person for patients and their families, and colleagues.
We answer the following research questions:
- To what extent do resource nurses report that network participation gives them competence in selected areas based on governing documents and recommendations?
- Are there any differences in the competence gained by RNs at different levels of the health service?
- What single factors are important for competence enhancement?
Method
The study is a descriptive cross-sectional study. We gathered data via an online questionnaire.
Sample
Everyone on the email lists of three out of nine networks in the South-Eastern Norway Regional Health Authority was invited to participate. As far as we know, these are the networks that have role descriptions and competence plans that are most closely based on the regional recommendations (3, 4).
Continuity and updated network lists represent a challenge as pointed out by SINTEF (5). Since we expected to get replies from some people who did not have the role of resource nurses, we excluded those who were not RNs, or who did not have the role of resource nurse.
We assumed that the most recent members had not yet gained increased competence in all areas, and chose to set an inclusion limit of one year’s participation. Figure 1 refers to invited participants who were included in the study.
Development of the questionnaire
We constructed the questionnaire for this study ourselves since there were no validated forms suited to the network’s competence goals. The questionnaire had mainly close-ended response alternatives and consisted of seven background questions, four questions about own network practice, sixteen questions about competence enhancement, and six questions about teaching methods.
We formulated specific questions about competence enhancement based on governing documents and earlier research (2–5, 13). We chose five questions related to knowledge, skills and general competence respectively in accordance with the definitions of the Ministry of Education and Research (8). We endeavoured to make the questions specific and precise, balance the role of RNs as a resource for colleagues, patients and their relatives, and also cover clinical work, interaction and knowledge dissemination.
We conducted a pilot study among six RNs who knew the network and the professional field, but who were not invited to take part in the study. Hospitals, the community nursing service and nursing homes were represented. The ‘pilot nurses’ reported that the questions were relevant and easy to understand. In keeping with their wishes, age was changed to a categorical variable. Three questions were simplified and made more explicit following a final critical reading.
We asked about the extent to which participation in the network had enhanced their own competence in various areas. We used a Likert-scale with values from 1 ‘Not at all’ to 5 ‘A very great extent’. Whether a scale with five variables can be considered a continuous variable is debatable (15), but we decided to use five categories rather than seven since we assumed that fewer alternatives made it easier for the participants to answer the questions.
The central tendency for the 15 questions was used as a result measure. We calculated a sum score for all 15 questions, and this score was used as an independent variable in the regression analysis.
Recruitment and implementation
The local network leaders sent out prior notification of the study on our behalf in October 2018. The members were also given oral information on clinical practice days. The information letter and link to the study were sent out in the same way in November, with a reminder after three weeks. Six weeks after this had been despatched, we concluded the data collection.
Data analysis
We collected the data in Nettskjema and transferred them to the IBM SPSS 24 analysis software. The file was checked for transfer errors and inappropriate values by means of a visual check and frequency tables.
We compiled descriptive statistics, conducted bivariate and multiple regression analyses and used the Kruskal-Wallis-test to compare total competence enhancement for RNs in hospitals, the community nursing service and nursing homes respectively (16).
Prior to carrying out the regression analysis, we created a new dichotomous variable for staff exchange training schemes: ‘Have participated in a staff exchange training scheme in one or two institutions’, or ‘Have not participated in a staff exchange training scheme’. Eight participants answered ‘Not applicable’ as regards exchange training at a hospital, and ‘No’ to exchange training at another unit. These were coded as ‘Has not participated in a staff exchange training scheme’.
Specialisation was also recoded as the dichotomous variable ‘Have…’ or ‘Have not specialised in cancer or palliative care’ based on the recommendations for the network (4).
The highest number of missing responses to any one question was eight. Missing data were not replaced by computed values due to the small size of the dataset and the lack of a theoretical framework. Eleven datasets lacked responses to one or more of the 15 competence-related questions, and these were not included in the regression analysis. The significance level was set at 0.05.
Ethical considerations
The plan for data processing and obtaining consent was approved by the Norwegian Centre for Research Data (NSD), reference number 196889. Participation was voluntary and submission of responses was regarded as consent. We stored the dataset on an encrypted memory stick and analysed this off-line. No individuals are identifiable in the published material.
Results
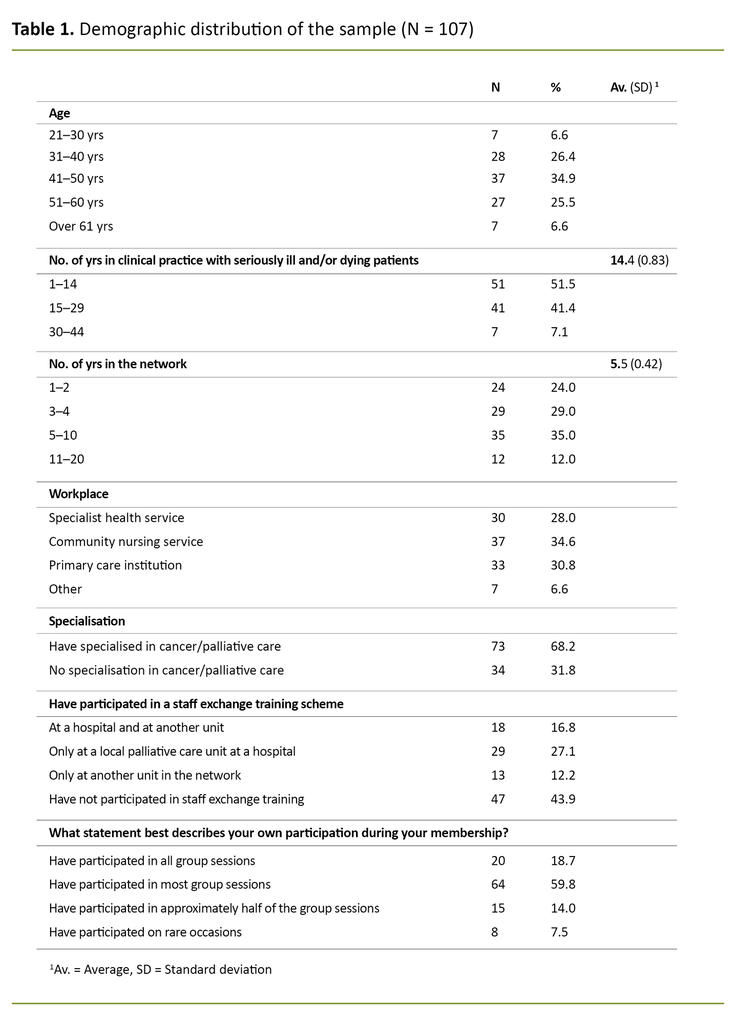
Figure 1 provides an overview of the participants in the study. There was a total response rate of 27 per cent, but after the exclusion of those who did not meet the criteria, we were left with a response rate of 22 per cent. Table 1 shows the sample’s demographic distribution. To provide an overview for the reader, we show the distribution for number of years of experience with the patient group and length of membership of the three groups, in addition to the mean value.
The typical resource nurse was between 41 and 50 years of age, had 10 years’ clinical experience with sick and dying patients, and had participated in most of the network sessions during their years of membership. The sample was relatively evenly distributed by workplace and age, and everyone had participated in at least one group session.
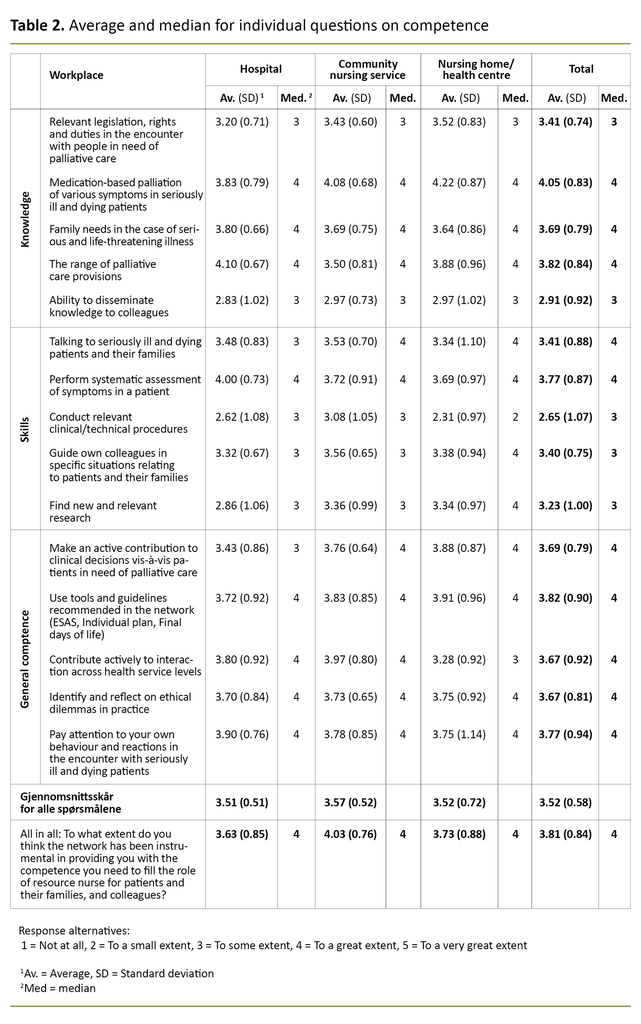
Table 2 shows the median and average values for the individual questions about competence as well as the average benefit. The results show that the RNs generally reported that they had benefitted considerably from participating in the network. In answer to ten out of fifteen individual questions, over half stated that they had benefitted to a great or very great extent (values 4 and 5).
More than 20 per cent responded ‘Not at all’ or ‘To a small extent’ in answer to only three questions: knowledge of disseminating competence, skills in finding new research, and performing relevant clinical or technical procedures. The scores on questions about skills were lower, while they were higher in relation to general competence, measured as a median.
RNs generally reported that they benefitted considerably from participating in the network.
There were no significant differences in the average total benefits reported by RNs at hospitals, in the community nursing service and at nursing homes or convalescent homes (Table 2).
Bivariate regression analysis showed that the number of years in the network, self-reported participation in network sessions, staff exchange training schemes, supervising and training colleagues as well as contacting others when necessary, were all positively associated with competence enhancement.
Multiple regression analysis showed that only staff exchange training schemes and self-reported degree of participation showed a significant association with competence enhancement (Table 3).
Discussion
The resource nurses reported that their competence was enhanced by participating in the network, and there were no significant differences between nurses at different levels of the health service. Participating in staff exchange training schemes and a self-reported high level of participation in network sessions are associated with a high level of competence enhancement.
This study therefore supports earlier findings and assumptions that the network enhances competence (5, 12,13), but has also increased our knowledge about the specific competencies that participation in the network can help enhance and what facilitates this.
Benefits of the network
A report from the Norwegian Research Centre for Health Services points out that the effect of learning networks is hard to measure (17). In practice, a resource nurse network is more loosely organised than a learning network, and the members find it difficult to distinguish between competence enhancement gained from the network and other learning (13).
The study design cannot establish causal relationships and the effect of the network, but regression analysis indicates that self-reported high participation in group sessions is positively associated with high overall competence enhancement (Table 3).
The high scores may indicate that we have chosen areas of competence that both participants and those who plan the group sessions deem relevant. The results also show that the network benefits the RNs through enhancing knowledge, skills and general competence, in accordance with the guidelines (4).
A slight tendency to report greater increases in general competence as opposed to skills may be due to the selection of individual questions, or the specific focus in the networks on topics related to general competence. It may also be the case that it is easier to choose a higher score on questions about general competence than on more specific questions about knowledge and skills.
Procedural skills stand out as having a low score.
Systematic symptom assessment, symptom relief, interaction and looking after the patient’s family are core competencies in basic palliative care (6), and the results suggest that participating in a network is beneficial in respect of these areas.
The explanation may be that these topics are emphasised at the network group sessions in keeping with the goal of promoting core palliative care competence in all parts of the health service (1, 2). Resource nurses with such expertise will be able to boost their colleagues’ palliative care skills and thereby facilitate the provision of qualified help to dying patients, also in units that do not have palliative care as a main objective.
Procedural skills stand out as having a low score. The community nursing service shows the best results – perhaps because RNs in this setting more often meet patients in need of many different nursing procedures.
Earlier research has suggested that RNs in the primary care health service lacked knowledge of advanced procedures (18). The specialist health service is responsible for providing the necessary training on equipment and procedures when the patient is to be discharged (19).
The training is often given in the ward in connection with the individual patient. The community nurses’ high score may perhaps indicate that those who are resource nurses are also prioritised for such training so that they can instruct colleagues (20).
Finding and applying research received a low score, which concurs with earlier studies (13). However, it is uncertain whether the participants interpreted the question as referring to methodological literature searches, or as a question about their knowledge of where to find new relevant knowledge.
Regardless of the interpretation, there is reason to believe that the workdays of clinical RNs are hectic and that they have little time for clinical studies. RNs have a duty to keep up-to-date in their own discipline (2), but a lack of time and competence have proved to be barriers to applying research in clinical practice (21).
Disseminating knowledge to colleagues also received a low score.
Perhaps the networks should prioritise the dissemination of relevant research and implement national professional guidelines and standardised patient-centred pathways (1) rather than teaching resource nurses how to look for new research?
Disseminating knowledge to colleagues also received a low score. These results may serve to remind those responsible for the networks that they should include more pedagogical topics in the teaching.
Teaching and supervision are learning goals in bachelor’s degree studies in nursing (22, 23), but there is reason to believe that specific advice on presentation techniques and planning the teaching would greatly help resource nurses to disseminate knowledge at their own workplace (3).
No difference between the levels
Since learning outcomes among nurses did not differ whether they worked in a hospital, the community nursing service, and nursing homes or convalescent homes, this may indicate that the network has reached its goal of promoting competence enhancement at all levels of the health service (2).
However, the results must be interpreted with care since the dataset is small. Patients with complex needs for palliative care are found at all levels of the health service (1), and it may be the case that differences in competence enhancement relate to the patients the informant works with rather than health service level.
Factors promoting greater learning outcomes
A self-reported high degree of participation in clinical practice days had a positive impact on competence enhancement. A natural interpretation is that the instruction led to good results, but the participants probably also benefitted from participating in and belonging to a community, as reported by resource nurses in the Western Norway Regional Health Authority (13).
Vygotskij argues that learning takes place through social interaction in conversations and through language (9, 10). Getting to know each other and exchanging experiences, thoughts and ideas in informal conversations during breaks may also be instrumental in reinforcing learning in the knowledge community.
A self-reported high degree of participation in clinical practice days had a positive impact on competence enhancement.
Staff exchange training schemes also help to explain greater overall benefit. Our study cannot elucidate why this contributes positively, but staff exchange training schemes in hospitals have previously been cited as learning arenas by primary care cancer nurses (20).
Staff exchange training schemes can be one way of getting to know your interaction partners and it may lower the threshold for getting in touch with them later about challenging situations. Being able to observe examples of how to tackle complex patient situations may provide a basis for experience-based learning and further reflection.
From a sociocultural perspective (9, 10), learning takes place in interaction and reflection with others, and staff exchange training schemes may be a good arena for this. At the same time, it establishes a platform for new patterns of interaction, which again promotes learning, according to Dysthe (9).
The actions or activities that are specifically mentioned in the recommendations on resource nurses’ role descriptions and competence plans (2, 3) had no significant impact on overall competence enhancement. However, teaching and supervising colleagues as well as contacting others in the network had a positive impact on competence enhancement (Table 3).
We do not know whether the most active learn most, or whether those who learn most are the most active. To our knowledge, this has not been examined in other studies of the networks. Nevertheless, all these activities will require active participation and interaction, and the tendencies may perhaps be supported by Vygotskij’s theory of learning in a social community and by verbalising one’s own knowledge and experience (9, 10).
The strengths and weaknesses of the study
To the best of our knowledge, this is the first study to investigate specific competence enhancement among resource nurses in cancer and palliative care, and the first to examine the networks in the South-Eastern Norway Regional Health Authority. Clear inclusion and exclusion criteria meant that we received responses from the targeted sample.
Questions based on different dimensions of the competence concept and resource nurses’ framework documents (2–4) strengthened the study’s contextual validity and provided a nuanced and comprehensive picture of the competence the network wished to provide.
Pilot testing among the RNs who were familiar with the field showed that the selected areas of competence were relevant. The main findings are in agreement with earlier research.
Using a constructed sum score, we were able to perform a regression analysis and compare overall competence enhancement (combination of knowledge, skills and general competence) in different groups.
However, this summary is not theoretically-based, and the results must be interpreted with care. Moreover, the analyses are based on the assumption of equal distance between the various values on the Likert-scale, which is also debatable (15). By showing the median and average values for each of the 15 questions about competence (Table 2), we comply with research requirements for transparency (24).
A clear weakness is the collection of data using a questionnaire that is not validated or psychometrically tested (24). Since we only invited participants from the South-Eastern Norway Regional Health Authority, the findings are not directly transferable to other networks in Norway.
Demographic distribution in the sample concurs with the impression the first author had after six years of working with the network, but a low response rate gives limited generalisability. An extra reminder could possibly have resulted in a higher response rate. We assume that it is those who read their emails regularly and those who are most positive to the network who replied.
The fact that we found no differences in competence enhancement between the different levels of the health service might be a type-II error, i.e. that significant differences were not revealed because the sample was too small. Perhaps such a difference might have been identified in a larger dataset with the same tendencies (24).
Due to personal data protection, we did not map local network affiliation. Thus we were unable to discover any bias in the sample. Network affiliation could potentially be an underlying factor in the regression analysis.
The first author headed one of the sub-networks during the study. We took this into account in the invitation and recruitment in order to promote voluntary participation.
Conclusion
Participating in a cancer and palliative care network for resource nurses seems to give members greater competence in key areas when performing their functions vis-à-vis patients and their families, and colleagues. RNs at all levels of the health service reported gaining much greater competence as a result of network participation.
Staff exchange training schemes and participation in clinical practice days were associated with greater competence enhancement. The study supports earlier findings and assumptions, but has also further expanded our knowledge of competence areas and specific learning outcomes.
The results can inspire heads of networks to invest more efforts in staff exchange training schemes, different methods of teaching and the role of resource nurses as knowledge disseminators. The resource nurses and network heads can use the results to stress the importance of participating in the network.
We recommend that future research on resource nurse networks focuses on the role as local knowledge disseminator: how competence is passed on, and how managers and colleagues view the resource nurse’s role and competence.
Moreover, follow-up research is needed in order to obtain knowledge about lasting learning and what topics and areas of competence the network should prioritise.
Possible conflict of interest: While the study was conducted, the first author headed the competence network for the Oslo University Hospital sector, which included 89 out of 493 of those invited to participate in this study, She also headed the steering group for the Oslo network. She has no conflicting financial interests.
References
1. NOU 2017: 16. På liv og død. Oslo: Departementenes sikkerhets- og serviceorganisasjon, Informasjonsforvaltning; 2017. Available at: https://www.regjeringen.no/no/dokumenter/nou-2017-16/id2582548/ (downloaded 16.08.2018).
2. Helsedirektoratet. Nasjonalt handlingsprogram med retningslinjer for palliasjon i kreftomsorgen. Oslo: Helsedirektoratet; 2015. IS-2285. Available at: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/918/Nasjonalt%20handlingsprogram%20for%20palliasjon%20i%20kreftomsorgen-IS-2285.pdf (downloaded 20.08.2018).
3. Regional kompetansetjeneste for lindrende behandling (KLB), Helse Sør-Øst. Funksjonsbeskrivelse for ressurssykepleiere i palliasjon og kreftomsorg. Oslo: Regional kompetansetjeneste for lindrende behandling (KLB), Helse Sør-Øst. Available at: https://oslo-universitetssykehus.no/seksjon/kompetansesenter-for-lindrende-behandling-helseregion-sor-ost-kslb/Documents/Anbefaling%20til%20funksjonsbeskrivelse.pdf (downloaded 27.10.2020).
4. Regional kompetansetjeneste for lindrende behandling (KLB), Helse Sør-Øst. Anbefaling; Kompetanseplan for ressurssykepleiere i palliasjon og kreftomsorg, Helseregion Sør-Øst. Oslo: Regional kompetansetjeneste for lindrende behandling (KLB), Helse Sør-Øst; 2018. Available at: https://oslo-universitetssykehus.no/seksjon/kompetansesenter-for-lindrende-behandling-helseregion-sor-ost-kslb/Documents/2018.07_Anbefaling_%20kompetanseplan.pdf (downloaded 15.08.2018).
5. Melby L, Das A, Halvorsen T, Steihaug S. Evaluering av tjenestetilbudet til personer med behov for lindrende behandling og omsorg. Trondheim: Sintef; 2017. A27799. Available at: https://www.sintef.no/globalassets/sintef-teknologi-og-samfunn/avdelinger/helse/20.3.17-rapport-lindrende-behandling_revidert-i-versjonsbeskrivelse-og-i-5.2-002.pdf (downloaded 16.08.2018).
6. Kaasa S, Loge JH, Haugen DRF. Palliasjon: nordisk lærebok. 3rd ed. Oslo: Gyldendal Akademisk; 2016.
7. Helse- og omsorgsdepartementet. Leve med kreft. Nasjonal kreftstrategi (2018–2022). Oslo: Departementenes sikkerhets- og serviceorganisasjon; 2018. I-1184 B. Available at: https://www.regjeringen.no/no/dokumenter/leve-med-kreft/id2598282/ (downloaded 15.08.2018).
8. Kunnskapsdepartementet. Nasjonalt kvalifikasjonsrammeverk for livslang læring. Available at: https://www.regjeringen.no/no/tema/utdanning/hoyere-utdanning/nasjonalt-kvalifikasjonsrammeverk/id564809/ (downloaded 17.06.2018).
9. Dysthe O. Dialog, samspel og læring. Oslo: Abstrakt forlag; 2001.
10. Vygotskij LS, Roster MT, Bielenberg T-J, Skodvin A, Kozulin A. Tenkning og tale. Oslo: Gyldendal Akademisk; 2001.
11. Eriksson S. Faktorer som påvirker ressurssykepleierens rolle og funksjon i kommunehelsetjenestens kreftomsorg. Erfaringer hos ressurssykepleiere og sykepleiere i små kommuner i Helseregion Vest. (Masteroppgave.) Bergen: Universitetet i Bergen, Institutt for samfunnsmedisinske fag; 2009. Available at: http://bora.uib.no/bitstream/handle/1956/3405/Masterthesis_Eriksson.pdf?sequence=1&isAllwed=y (downloaded 05.08.2018).
12. Hauken MA, Helgesen R. Kreftnettverk gir trygghet. Sykepleien. 2011;99(11):58–61. Available at: https://sykepleien.no/forskning/2011/10/kreftnettverk-gir-trygghet (downloaded 05.08.2018).
13. Valen K, Ytrehus S, Grov EK. Tilnærminger anvendt i nettverksgrupper for kompetanseutvikling i det palliative fagfeltet. Vård i Norden. 2011;31(4):4–9. Available at: https://helse-bergen.no/seksjon/klb/documents/nettverk/tiln%C3%A6rminger%20anvendt%20i%20nettverksgrupper%20for%20kompetanseutvikling%20i%20det%20palliatuve%20fagfeltet.pdf (downloaded 05.08.2018).
14. Helsedirektoratet. Rapport om tilbudet til personer med behov for lindrende behandling og omsorg mot livets slutt: å skape liv til dagene. Oslo: Helsedirektoratet; 2015. IS-2278. Available at: https://www.regjeringen.no/contentassets/a4b45c8f57e741bdbb3bfb32c6b9ef43/rapport_hdir_palliasjonsrapport_160315.pdf (downloaded 20.08.2018).
15. Sullivan G, Artino Jr. AR. Analyzing and interpreting data from Likert-type scales. Journal of Graduate Medical Education. 2013;5(4):541–2.
16. Pallant J. SPSS survival manual: a step by step guide to data analysis using SPSS. 4th ed. Maidenhead: McGraw-Hill Open University Press; 2010.
17. Bakke T, Udness E, Harboe I. Læringsnettverk som verktøy i kvalitetsforbedring – en oppsummering av forskning og erfaring. Oslo: Nasjonalt kunnskapssenter for helsetjenesten; 2011. Available at: https://www.fhi.no/publ/2011/laringsnettverk-som-verktoy-i-kvalitetsforbedring---en-oppsummering-av-fors/ (downloaded 05.03.2019).
18. Bing-Jonsson PC, Hofoss D, Kirkevold M, Bjark IT, Foss C. Sufficient competence in community elderly care? Results from a competence measurement of nursing staff. BMC Nursing. 2016;15(5). Available at: https://bmcnurs.biomedcentral.com/articles/10.1186/s12912-016-0124-z (downloaded 10.04.2019).
19. Lov 2. juli 1999 nr. 61 om spesialisthelsetjenesten m.m. (spesialisthelsetjenesteloven). Available at: https://lovdata.no/dokument/NL/lov/1999-07-02-61 (downloaded 05.03.2019).
20. Hynne AB, Kvangarsnes M. Læring og kompetanseutvikling i kommunehelsetenesta. Ein intervjustudie av kreftsjukepleiarar. Nordisk tidsskrift for helseforskning. 2014;10(2):76–90. Available at: https://septentrio.uit.no/index.php/helseforsk/article/view/3324 (downloaded 15.04.2019).
21. Saunders H, Vehviläinen-Julkunen K. The state of readiness for evidence-based practice among nurses: an integrative review. Int J Nurs Stud 2016;56:128–40.
22. Kunnskapsdepartementet. Rammeplan for sykepleierutdanning. Oslo: Kunnskapsdepartementet; 2008. Available at: https://www.regjeringen.no/globalassets/upload/kd/vedlegg/uh/rammeplaner/helse/rammeplan_sykepleierutdanning_08.pdf (downloaded 15.04.2019).
23. Forskrift 15. mars 2019 nr. 412 om nasjonal retningslinje for sykepleierutdanning. Available at: https://lovdata.no/dokument/SF/forskrift/2019-03-15-412 (downloaded 15.04.2019).
24. Polit DF, Beck CT. Nursing research: generating and assessing evidence for nursing practice. 9th ed. Philadelphia: Wolters Kluwer Health; 2012.












Comments