How intensive care patients’ family members can play a more active role
A calm atmosphere with single rooms, flexible visiting hours and trust in the healthcare personnel can help the family members to serve as a resource for heart surgery patients with a prolonged stay in intensive care.
Background: Family members can provide crucial support for the patient, including during stays in an intensive care unit, but the family members’ situation and efforts have not been sufficiently elucidated in earlier research. The focus has been on identifying the family members’ needs and their satisfaction with how healthcare personnel meet these needs.
Visiting hours in intensive care units have traditionally been restricted. Multi-bed wards were sometimes considered overwhelming, with limited opportunities for privacy. Little research is available on family members’ experiences with single rooms and flexible visiting hours.
Objective: We wanted to obtain more knowledge about families’ experiences in connection with prolonged stays in intensive care units following heart surgery in a unit with single rooms and flexible visiting hours.
Method: A grounded theory-based study, including semi-structured interviews with six family members of intensive care patients. The data were analysed in accordance with constructivist grounded theory (CGT).
Results: Patients’ family members sought and fostered a sense of security by being present for the patient and helping the patient to get through the intensive care treatment. They found that single rooms, short waiting times, flexible visiting hours, information, trust in healthcare personnel, privacy and a calm atmosphere in the unit enabled them to play an active role in which they could support and protect the patients.
Family members had a strong desire to make the patient and other relatives feel more secure in an uncertain, unfamiliar, busy and challenging situation characterised by fluctuating hope and emotions. During visits, they were primarily concerned with supporting the patient and protecting them from their own reactions and difficult topics of conversations. Strong impressions and concern for the patient sometimes made it difficult to comprehend important information given by healthcare personnel.
Conclusion: Family members wanted to play a role in making the patients feel more secure during their stay in intensive care, and they felt that their efforts were an important resource. A calm atmosphere, trust in the healthcare personnel and private visits with the patients made it possible for them to support and care for the patients. The findings challenge traditional perspectives on the roles of patients’ families, where families are ascribed a passive recipient role as a visitor.
Intensive care treatment is constantly changing. The changes affect the interaction between healthcare personnel, patients and patients’ families (1, 2). While the public health service’s treatment responsibilities are mandatory, family members can provide crucial support for the patient, including during intensive care treatment (1, 3).
The situation and efforts of family members have not been sufficiently elucidated in earlier research (1, 3, 4). The aim of this study is therefore to examine their situation in connection with heart surgery patients with a prolonged stay in intensive care.
A planned heart surgery trajectory involves 24 hours in an intensive care unit, where the patients are extubated after a few hours. Most patients are weak at this point. They are then transferred to intermediate monitoring for 24 hours, followed by a few days in a ward, and then transferred to a local hospital where necessary. In cases where a patient’s stay in intensive care needs to be prolonged, the nature of the trajectory changes and has several similarities with a general stay in intensive care.
Earlier research
Research on families of intensive care patients has centred around perceptions of crises and reactions to stress that can pose a health risk to the patients’ families. The most important needs of the family members are identified as open and honest information, the opportunity to spend time with the patient, assurance that the patient is being taken care of, hope, updates on the patient’s condition and the need for comfort and support.
These findings are confirmed in several studies and appear to be well-documented (4–8). How well the families’ needs are taken care of is primarily documented through measurements of family satisfaction (9, 10). The intensive care setting is part of everyday life for the staff, but is a unique experience for the patients and their families. Patients, their families and the staff can therefore have different interpretations of the same events (2, 6).
There is limited knowledge about families’ experiences in several contexts – about how these experiences are influenced by society, the culture, the type of health service and by various underlying reasons why patients need intensive care treatment. The focus of research in the field has been based on the situation of the bereaved (4). Thus, families’ experiences with intensive care survivors and with other types of intensive care stays are not as well documented (2, 10).
Guidelines
Families can find the intensive care environment to be an alien, stressful and hectic world characterised by complex treatment using a great deal of technology. Families are exposed to high noise levels, limited physical space in rooms with several beds, extensive visiting restrictions, waiting times for visits without appropriate facilities and strong impressions from the concentration of intensive care patients in large rooms (11–13).
In response to these challenges in the intensive care environment, guidelines have been drawn up for patient and family-oriented care in intensive care units, where a family-friendly structure includes waiting rooms, single rooms and flexible visiting hours (11, 12). The guidelines allow the patients’ families to be involved during the intensive care stay, and ensure that the families’ needs in a difficult situation are recognised and met by the healthcare personnel (3, 6, 12).
Objective of the study
Despite over 30 years of research on the subject and ongoing debate, particularly in relation to visiting hours, there are still unanswered questions about families’ experiences with the different structures of intensive care units, and how the families perceive the interplay between the patients and the healthcare personnel within different frameworks and space solutions.
Earlier research has called for studies that can provide more knowledge about structure and interaction in the intensive care setting (9, 14), with a view to helping healthcare personnel to make better provision for patients’ families.
The purpose of our study was therefore to provide knowledge on family members’ experiences and perceptions in connection with intensive care stays following heart surgery in a unit with single rooms and flexible visiting hours.
Method
The complexity of family members’ experiences and our ambition to ascertain their perspectives led us to using a qualitative research design based on the Corbin and Strauss (15) approach to grounded theory (GT). In line with an exploratory basis, we chose an inductive design. We performed the data analysis in accordance with the principles of constructivist grounded theory (CGT) (15).
GT is traditionally based on symbolic interactionism combined with pragmatic philosophy. GT studies seek explanations, processes, experiences and knowledge of how situations are handled. Analysis of the interplay between action, structure and interaction is central.
CGT represents a continuation of GT, with a goal of improving knowledge about various possible interpretations of reality in a given context, where the researcher is regarded as a co-participant as opposed to a neutral discoverer of objective findings (15).
We recruited family members through patients who had undergone heart surgery and had been in an intensive care unit for more than 24 hours. The unit is part of a relatively new hospital with single rooms, waiting rooms, rooms for private conversations and no fixed visiting hours.
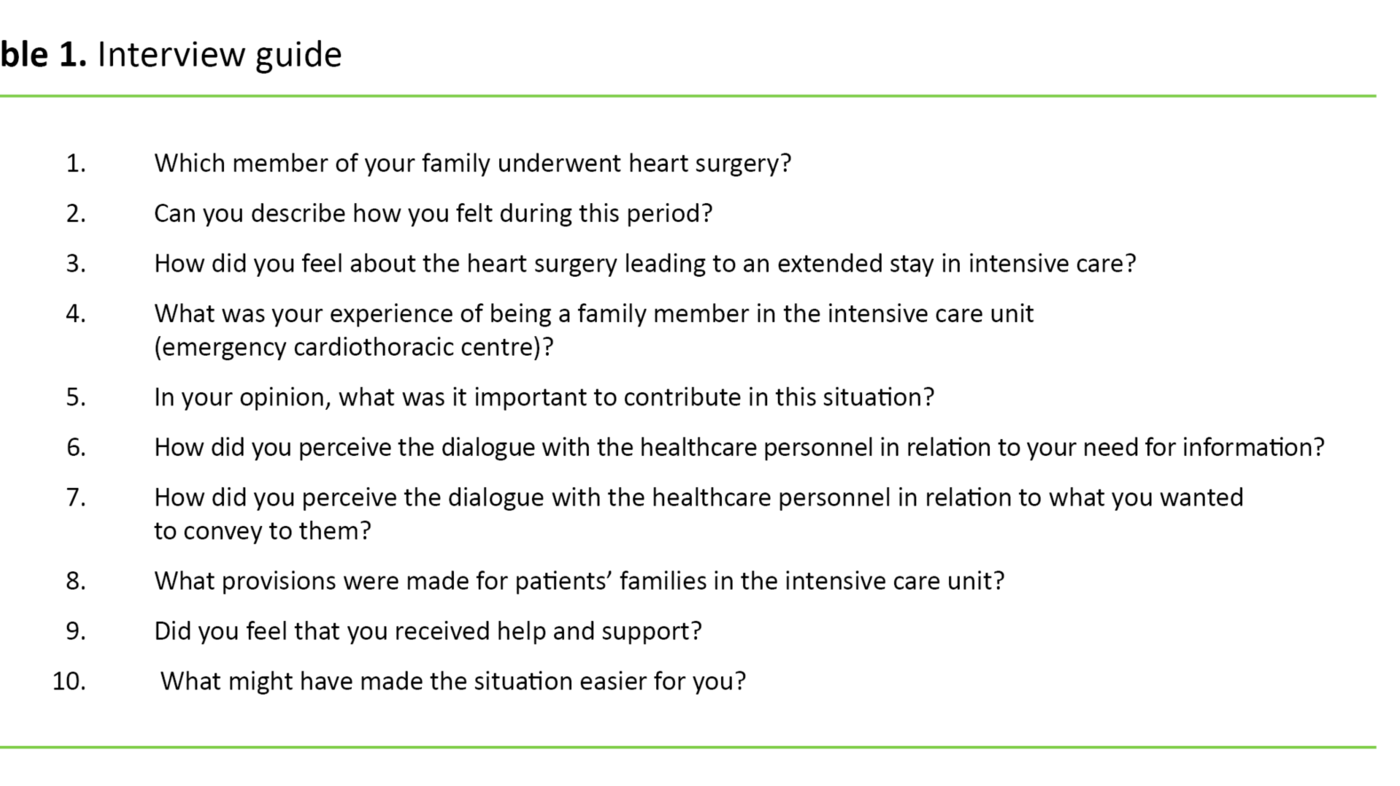
The data were collected through semi-structured interviews with family members of heart surgery patients who had survived intensive care. The stay in intensive care was longer than is normally expected following standard heart surgery. Table 1 shows the interview guide.
Sample
Our ambition was to recruit ten informants, but this was not possible within the timeframe of the project. The interviews were conducted two to six months after the hospital stay, when we assumed that the situation was probably clearer for the patients and that the family had had time to reflect on events.
We contacted the patients in writing in order to recruit the person they chose as their closest family member over the age of 18.
Due to the risk of confusing the researcher role with the role of intensive care nurse or healthcare personnel, the letters were sent by the hospital without us knowing who was contacted. We first learned the identity of the participants when they responded with their contact details.
The study was approved by the Regional Committee for Medical and Health Research Ethics (REC) (project number 2014/1144) and the participants’ written consent was obtained.
Data
The data include material from interviews with four spouses and two adult children; a total of four women and two men. The first author, who is an intensive care nurse with many years of experience with heart surgery patients in intensive care, interviewed the informants. Four of the interviews were conducted in the informant’s home and two were held at office premises.
The interviews lasted between 1.25 and 1.75 hours, and were recorded on audio tapes and transcribed in full text. In order to strengthen credibility, we summarised the main points at the end of the interviews by asking questions such as ‘Have I understood you correctly...?’.
The analysis included the transcription of interviews, memo writing and a writing process in line with GT, coding of the material and further analysis with the development of concepts and categories (15). One of the co-authors read through the transcripts, and both co-authors took part in the analysis and writing process.
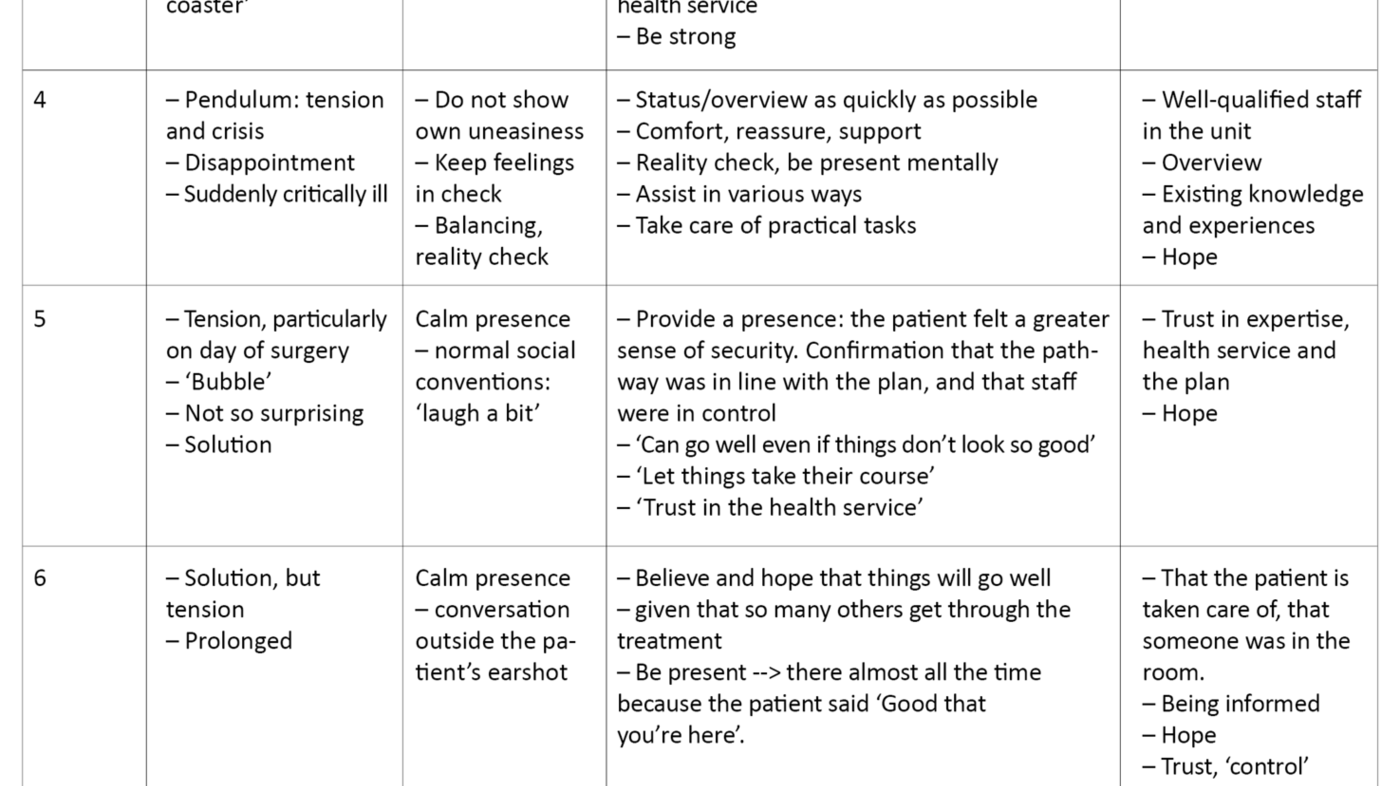
In the open coding process, the purpose was to break down the data into smaller and more manageable units. We therefore created matrices to gain an overview. See the example in Table 2.
Open coding, matrices, notes from interviews and transcription enabled us to structure the data using axial coding in different themes and categories, then, in line with a circular work method, to return to the data to validate the analysis (15). Table 3 illustrates the analysis process.
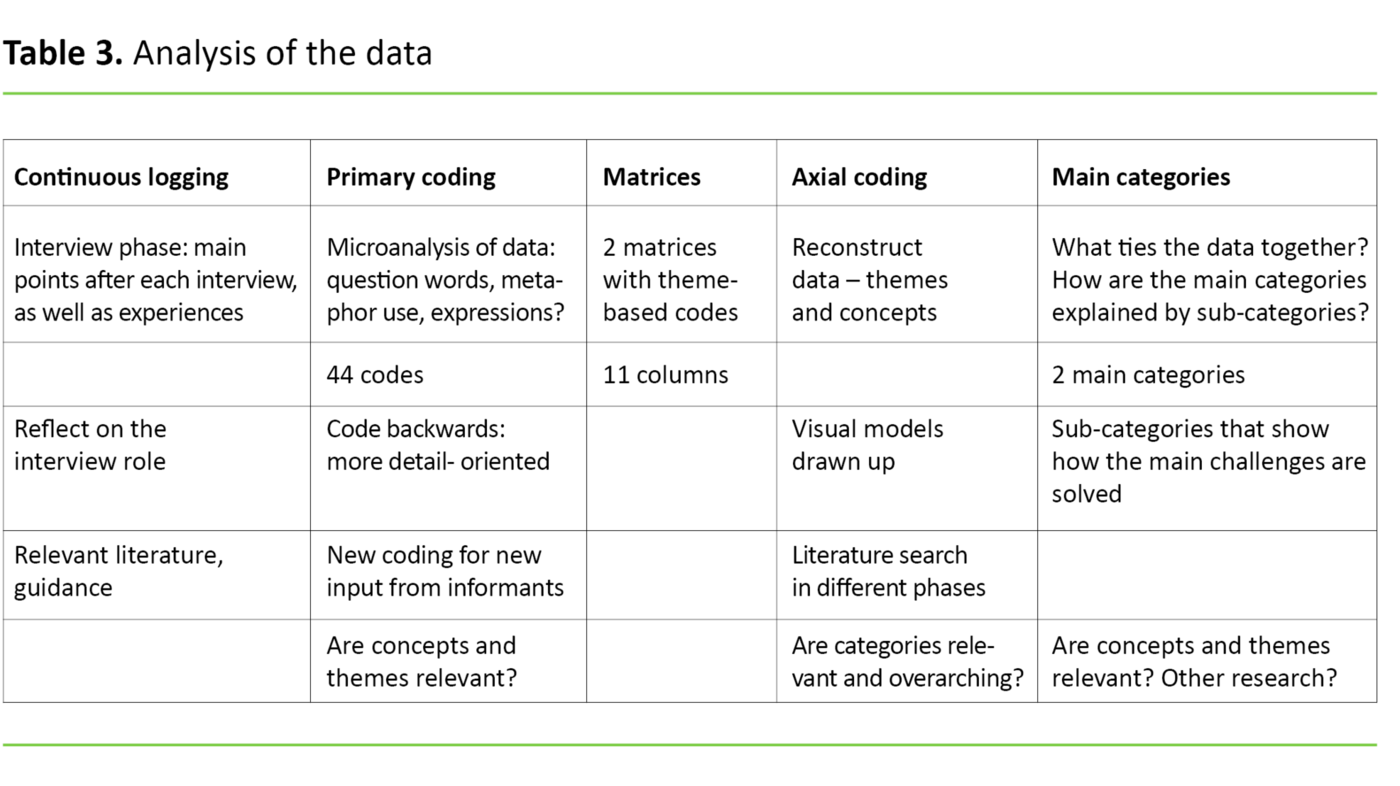
During the analysis process, we noted both typical and anomalous findings and focused our attention on alternative explanations (15). After each interview, we changed and controlled concepts and categories in the data in line with the GT principle of constant comparison (15).
The aim was to strengthen the credibility of our interpretation of the data since the goal was to elucidate the situation from the informants’ perspective. We also enhanced the credibility of the categories and concepts by presenting relevant quotes from the transcripts.
Results
The analysis produced two main themes: family members sought and fostered a sense of security by providing support and care for the patient whilst in intensive care. The second theme was that the combination of a family-friendly structure with single rooms, flexible visiting hours and positive perceptions of healthcare personnel in the intensive care unit enabled the families to play a supportive and active role during visits.
Fostering a sense of security
The most important aspect for the family members was to seek a sense of security, primarily for the patient, but also for themselves and other relatives. The informants felt that they were in a ‘bubble’, where all the attention was directed towards the patient’s well-being, and found that they were able to muster the energy and strength to support the patient during the intensive care stay. The primary agenda of the families was to serve as a supportive presence:
‘Then the tears started without him saying anything. So, yes, he felt that we were there. Because he said that it was good to see me: ‘Good that you’re here’, he said. And that was enough to make me want to stay.’
Intensive care stays varied from a few days up to two weeks, and both planned and emergency cases were represented in the family members’ narratives. The day of surgery, however, entailed unbearable tension for them.
Some patients recovered quickly after undergoing a new intervention, while others were subject to complications and an uncertain prognosis. The family members also told of respiratory treatment and various forms of impaired consciousness. They visited the patients at least once a day.
During the course of the clinical pathway, family members had visited the patient in one or more hospitals, and their time was taken up with travelling, work and family obligations. Being a family member of a seriously ill patient was a challenge. They likened the twists and turns in the clinical pathway and the patient’s uneasiness to being on ‘an emotional rollercoaster’.
Varying degrees of security within the same family
Some family members barely managed to visit, and were described by the informants as ‘completely shattered’. The informants tried to hide their own uneasiness from the patient during visits. Some had a strong reaction to the first encounter with the patient in the intensive care unit, which was reinforced by the fact that they were not prepared for the patient’s changed appearance and level of consciousness. One family member described a visit to a previously healthy person after an emergency operation, as follows:
‘Many people are shocked by their own reactions when they see their mother or grandmother in such a situation and are overwhelmed when they encounter the intensive care unit for the first time, with the monitoring equipment, breathing apparatus and a close relative caught up in something that changed their skin colour from normal to grey during the course of a day.’
Protecting the patient entailed avoiding talking about disturbing topics of conversation, leaving the unit when they observed that the patient was tired, not obstructing the staff’s patient care work and trying to act calm in front of the patient:
‘I now have to show my mother that I’m worried, but not so worried that she’s worried about me being worried! That’s the kind of balancing act that family members need to maintain, because I saw how scared and badly affected she was then.’
Observing that the patient felt soothed by their presence seemed to reassure family members, and this strengthened their belief in their own efforts. The informants signalled a confirmatory family togetherness: this was something they would get through together. They encouraged the patient and distracted them from uneasiness and discomfort. Outside the hospital, they carried out tasks that the patient would normally undertake, cared for other family members, and updated social networks about the patient’s condition.
Scope for active presence
The environment in the intensive care unit was new and unknown to the informants, who described a quiet place with a calm atmosphere, and they were not frightened by the environment. Flexible visiting hours and single rooms made it easy for the family members to be present in the patient’s room:
‘How can I put it - I just went straight in. Getting access was no problem for us, we came straight in every time!’
‘We didn’t need to wait around much, we were in his room. He did have a single room after all.’
‘Being in a single room as opposed to a room with several other patients makes a huge difference. So I found it incredibly positive. In a way, it made my role easier; you have nothing else to focus on apart from the patient and the treatment. And that’s exactly what you want to be in focus when visiting a hospital.’
There were opportunities for safe, ‘private’ time, when the healthcare personnel took a step back, but continued to monitor the patient. The staff were mostly described as ‘nice’, and the informants felt welcome in the unit. However, the dialogue with the healthcare personnel in the patient’s room showed signs of restraint to some extent. As well as shielding the patient from uneasiness, family members were focussed on communicating with and caring for the patient.
Desire for more information from healthcare personnel
The family members were also conscious of not obstructing the staff’s patient care work. The informants therefore called on the healthcare personnel to take the initiative more often to provide information, not just about the patient, but about which professionals they had talked to, the daily routine, suitable visiting times and the healthcare personnel’s expectations of the families.
In addition, the informants made the following suggestions for the healthcare personnel: give the families a short briefing on the patient’s condition before a visit, have a brief conversation with them after the visit, and hold information meetings after the initial shock phase has passed. Conversations and meetings outside the patient’s room would also give families the opportunity to talk about their situation and their own reactions.
The informants were reassured by the fact that heart surgery is regarded as a routine operation nowadays, and by confirmation that the planned clinical pathway was mostly adhered to. Complications and significant deviations from the planned clinical pathway following surgery raised new, unanswered questions for some of the informants. Lack of information may have been the reason for these questions going unanswered, but in some cases, they may have misunderstood or forgot what they had been told:
‘We were told that quite a few patients had this operation and that it went well. We hoped so. We didn’t really get any explanation, they said that all the tests were fine. But I immediately thought that that’s no doubt something I’ll hear about later.’
Trust linked to information
A close link existed between whether the family members received information and whether they perceived the healthcare personnel as competent. How the staff conveyed information was the determining factor in whether the overall impression inspired trust:
‘Just how much of an overview I felt I had, I’m not sure. I had the impression that they were in control of the situation. That was really the most important thing for me. Medical jargon and all of that is not too important. The fact that I don’t remember everything the surgeon told me is not his fault.’
Trust was central to the informants’ narratives. Family members generally had a high level of trust in the health service, but in this particular setting they found the trust to be forced:
‘You are totally dependent on the people who are around you, and whether those machines work. You just need to believe that everything will work! You can’t just start expecting or looking for mistakes, you just have to have faith, you know?’
After observing that the patient was being taken care of, the informants found that their general confidence in the health service was maintained. This certainty helped them to trust that the patient was in good hands when they themselves were not present.
Support from healthcare personnel
The informants wanted information from doctors and nurses, but some thought that the healthcare personnel should concentrate primarily on the patient. Some family members took care of each other and therefore did not need support from the staff if the patient survived the intensive care treatment. Others wanted support, and they received the support they needed from the healthcare personnel, but the experiences varied:
‘For my own part, I think I was in shock, I wasn’t able to initiate contact myself. So I suppose if there had been someone there who had approached me and sat down and chatted, I think it would’ve helped.’
Informants who received support from healthcare personnel found it reassuring:
‘As a family member of a patient, you’re very vulnerable. You need to be there for the person who is sick. It’s therefore good to get some comfort and understanding from the experts, and for them to realise that you’re a bit fragile, that you actually need to hear that things are going well. It’s small things like that that take away the fear of all the tubes. That they take the time, that they look you in the eye, maybe even give you a little smile.’
The families’ experiences with the roles of the healthcare personnel varied, but they all wanted to be able to help the patient feel a greater sense of security through a supportive presence and care.
Discussion
During the patient’s prolonged stay in intensive care following heart surgery, it was important for the family members to make the patient feel more secure by serving as a calming, confirmatory, protective and encouraging presence.
Positive experiences with the health service and trust-inspiring healthcare personnel, no waiting times, flexible visiting hours and a calm atmosphere with opportunities for privacy in single rooms enabled families to play an active role, with a self-defined, patient-oriented agenda.
Role of the family
Engaged family members with a strong belief in the importance of their own role challenge traditional perspectives on family roles (16, 17), where families’ capacity and efforts in relation to the intensive care patient have received little attention (1, 3, 14).
Even in Norway, families have been regarded more as visitors than as a resource for the patients (18). Defining families as passive visitors or as resources can have an impact on the interaction between the families and the healthcare personnel.
The findings are in line with research on families of intensive care patients concerning the emphasis on the sense of security, the healthcare personnel’s expertise and patient care, honest information and the importance of a family-friendly structure (4–8, 12).
Families’ efforts are worthwhile
The informants’ desire to be there for the patients has been identified in earlier research (4, 7, 8, 19). Studies have emphasised that participation is important for the families’ own health (20, 21), but there is less of a focus on the importance of the family members’ efforts for the patients. The informants’ hopes and positive expectations for the heart surgery may have made it easier for them to assume an active role.
Research has shown that the burden on families is less in cases of intensive care treatment following planned surgery than for emergency intensive care (22). Meanwhile, the importance of families’ efforts for seriously ill intensive care patients has been documented in research (3, 23), which shows that the treatment context may have an impact, but is not a prerequisite for the family members taking an active role.
Expectations that the patient should recover from heart surgery and intensive care meant that some informants did not consider themselves to be a target group for support from healthcare personnel. All they wanted was information, since family members took care of each other. The importance of healthcare personnel’s support and care for families has almost been taken for granted, and is therefore not discussed to any great extent.
Earlier research has shown that families of intensive care patients suppress their own needs because they are so focussed on the patient’s situation (4, 7, 8, 20). While some family members do not feel a need for support, other members of the same family may react differently to the patient’s illness and intensive care stay and will consequently have a greater need for involvement from healthcare personnel. Families differ in terms of caring for the patient, participation, reactions to the patient’s illness and the need for support.
The informants wanted updates on the patient’s condition. For some, confirmatory information after heart surgery was sufficient, but not when the clinical pathway took a different direction. It has previously been shown that deviations from the described treatment pathway increase family members’ need for explanations (24). When the use of standardised clinical pathways in the health service becomes more widespread, reactions and needs in relation to pathway deviations may also be a relevant issue for families of other patient groups.
Trust in the health service
The informants generally trusted the health service. They felt that their trust in healthcare personnel in the unit was justified. Families’ observations of how healthcare personnel took care of the patient and the families’ contact with the staff confirmed that the patient was in safe hands. The importance of families experiencing that patients are well taken care of is consistent with research showing that families are reassured by care, expertise and dedication in healthcare personnel (4, 5, 8, 20, 21).
When the informants believed that the healthcare personnel were in control, it compensated for an incomplete picture of the pathway. The importance of trust in healthcare personnel may explain research results showing that even though the majority of informants did not understand the content of what was communicated to them, they were nevertheless satisfied with the supply of information (25).
Research also shows that relatives often refrain from asking for clarification when they trust the healthcare personnel (26). This finding is in contrast to research results from intensive care units that give very limited access to visitors, and where restrictions and waiting have led to considerable frustration for families and created more uncertainty (17).
Family members protected the patient
An important task for the informants was to protect the patient, which we interpret as shielding the patient and sparing their feelings. According to research on patients’ families living in countries with low levels of societal trust, protection took on a different meaning in that it entailed monitoring the healthcare personnel’s treatment and care for the patients.
They assumed that the healthcare personnel did more for the patients when the families were present (27). Consequently, family members assumed a role similar to a guard, or an advocate-like role, in order to safeguard the patient’s interests (3, 16, 17, 20, 23, 28), while our informants trusted that the patients were well taken care of whether a family member was present or not.
Ambitions to protect the patient conflicted with the informants’ desire to ask staff questions. Research has shown that families refrain from asking questions for reasons of protection; to spare the patient from disturbing topics of conversation in the patient’s room (7, 8, 29).
They assumed that healthcare personnel who perform patient care cannot dedicate too much attention to families. The studies point to a need for alternative arenas for communication with families of intensive care patients (13, 19, 24).
More satisfied with single rooms
The informants thought that the single-room structure made it easy for them to care for and support the patients during their stay in intensive care. There is little research on intensive care units with single rooms, but satisfaction surveys before and after the reorganisation of the room structure show that satisfaction increases when there is an opportunity for privacy and when more emphasis is placed on improving the atmosphere in the unit (30).
The results from these studies are in contrast to research in which the intensive care unit environment is described as frightening and noisy (10, 11). Although the environment is portrayed as quieter, encounters with a critically ill family member can nevertheless have a strong impact on relatives and they will therefore still have a need for preparatory information (4, 13, 31).
Family members’ perceptions of their presence in the intensive care unit differed, but this finding is not well-documented in earlier research (4). According to Olsen et al., intensive care patients often worry that some family members cannot bear to visit (32). Such findings can highlight variations in experiences and perceptions, not only between families, but also within the same family.
Family members’ experiences showed that a modern, family-friendly structure and confidence-inspiring experiences with healthcare personnel helped families to take on a supportive and active role. This appears to be more of an active role and less of a recipient role than shown in earlier research.
Reflections on method
The interviews generated rich data on families’ experiences and perceptions. The perspectives and voices of family members emerged, including in relation to matters we did not include in the interview guide. For example, the informants placed a great deal of emphasis on the importance of trust in the health service in general and in the healthcare personnel they had contact with during the clinical pathway. We discussed the findings based on relevant research, and we have reason to believe that the findings are relevant for relatives’ experiences in a similar context.
The number of informants was lower than planned as we concluded recruitment after nine months, with six informants. This is a weakness of the study. Despite our ambitions to recruit more informants, we believe that the data on family members’ experiences include both common and more varied experiences, which strengthened the analysis of the findings (15, 33). In principle, the number of informants is assessed according to whether the data adequately elucidate the issue.
The fact that the sample consisted of informants who were taken from a limited population, where the informants had experiences from a limited and defined field, can justify a downward adjustment of the requirement for the number of informants (33).
We concluded that the sample of informants was composed of different familial roles, gender and geographic location, that the data basis was sufficient, and that we achieved saturation in the data. However, it is possible that the patients recruited family members based on different familial roles, but who nevertheless had several things in common, and that the findings reflected this.
The findings are based on an interpretation of the interview material. The interviewer undertook a dual role as a researcher and a professional practitioner. We avoided mixing professional roles and research roles in the interview setting by excluding patients for whom the first author, who is also an intensive care nurse, had been responsible. The role of intensive care nurse may nevertheless have influenced the informants and meant that they under-communicated criticism.
One of the strengths of the study is the first author’s and one of the co-author’s extensive knowledge of the field. Nevertheless, their occupational affiliation carries a risk of bias and insufficient distance to the field in the interpretation of data (15). We attempted to reduce this risk by involving a co-author in all parts of the research process who did not have the same affiliation.
The data are based on the informants’ narratives following the intensive care stay, which may have impacted on the findings, both in terms of the recollection and the assessment of the course of events. Small details can easily be forgotten, but it is uncertain whether forgotten information affects the quality when complex experiences and perceptions are being conveyed.
The informants were made up of the patients’ spouses of both sexes and adult children of both sexes. It is unknown whether the variation in familial roles and gender had a bearing on our findings, but we believe that family roles and family dynamics, in addition to individual reactions in the same families, should be elucidated through research.
Conclusion
Family members found that it was possible to feel a sense of security despite tension and uncertainty during the intensive care period. Trust in healthcare personnel, information, expectations of heart surgery and a family-friendly structure provided the basis for a more active role by family members than that described in earlier research.
Family members felt that their efforts made them an important resource for the intensive care patients. This finding challenges traditional perspectives on the roles of patients’ families, where family members are primarily ascribed a passive recipient role as a visitor. The findings point to considerable variation in the reaction patterns within the same family, which is an under-researched area and should be explored further.
We would like thank the patients who recruited a family member, as well as the family members who participated in the study.
We would also like to thank the Cardiothoracic Intensive Department and Department of Cardiothoracic Surgery at St. Olav’s hospital.
Finally, we thank the Norwegian Nurses Organisation’s Association of Intensive Care Nurses (NSFLIS) for allowing the first author to attend the writing seminar in 2017.
References
1. Schmidt M, Azoulay E. Having a loved one in the ICU: the forgotten family. Current Opinion in Critical Care. 2012;18(5):540–7.
2. Hwang DY, Yagoda D, Perrey HM, Currier PF, Tehan TM, Guanci M, et al. Anxiety and depression symptoms among families of adult intensive care unit survivors immediately following brief length of stay. Journal of Critical Care. 2014;29(2):278–82.
3. McAdam J, Arai S, Puntillo K. Unrecognized contributions of families in the intensive care unit. Intensive Care Medicine. 2008;34(6):1097–101.
4. Verhaeghe S, Defloor T, Van Zuuren F, Duijnstee M, Grypdonck M. The needs and experiences of family members of adult patients in an intensive care unit: a review of the literature. Journal of Clinical Nursing. 2005;14(4):501–9.
5. Obringer K, Hilgenberg C, Booker K. Needs of adult family members of intensive care unit patients. J Clin Nurs. 2012;21(11–12):1651–8.
6. Maxwell KE, Stuenkel D, Saylor C. Needs of family members of critically ill patients: A comparison of nurse and family perceptions. Heart & Lung: The Journal of Acute and Critical Care. 2007;36(5):367–76.
7. Burr G. Contextualizing critical care family needs through triangulation: an Australian study. Intensive and Critical Care Nursing. 1998;14(4):161–9.
8. Linnarsson JR, Bubini J, Perseius K-I. Review: a meta-synthesis of qualitative research into needs and experiences of significant others to critically ill or injured patients. Journal of Clinical Nursing. 2010;19(21–22):3102–11.
9. Rothen HU, Stricker KH, Heyland DK. Family satisfaction with critical care: measurements and messages. Current Opinion in Critical Care. 2010;16(6):623–31.
10. Wall RJ, Curtis JR, Cooke CR, Engelberg RA. Family satisfaction in the ICU: differences between families of survivors and nonsurvivors. Chest. 2007;132(5):1425–33.
11. Choi Y-S, Bosch SJ. Environmental affordances: Designing for family presence and involvement in patient care. HERD: Health Environments Research & Design Journal. 2013;6(4):53–75.
12. Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45(1):103–28.
13. Cappellini E, Bambi S, Lucchini A, Milanesio E. Open intensive care units: a global challenge for patients, relatives, and critical care teams. Dimensions of critical care nursing: DCCN. 2014;33(4):181–93.
14. Olding M, McMillan SE, Reeves S, Schmitt MH, Puntillo K, Kitto S. Patient and family involvement in adult critical and intensive care settings: a scoping review. Health Expectations. 2015;19(6):1183–1202.
15. Corbin JM, Strauss AL. Basics of qualitative research: techniques and procedures for developing grounded theory. Thousand Oaks, California: Sage; 2008.
16. Levine C, Zuckerman C. Hands on/hands off: Why health care professionals depend on families but keep them at arm's length. The Journal of Law, Medicine & Ethics. 2000;28(1):5–18.
17. Vandall-Walker V, Clark AM. It starts with access! A Grounded Theory of family members working to get through critical illness. Journal of Family Nursing. 2011;17(2):148–81.
18. Haugdahl HS, Eide R, Alexandersen I, Paulsby TE, Stjern B, Lund SB, et al. From breaking point to breakthrough during the ICU stay: A qualitative study of family members' experiences of long-term intensive care patients' pathways towards survival. J Clin Nurs. 2018;27(19–20):3630–40.
19. Blom H, Gustavsson C, Sundler AJ. Participation and support in intensive care as experienced by close relatives of patients – A phenomenological study. Intensive and Critical Care Nursing. 2013;29(1):1–8.
20. Johansson I, Fridlund B, Hildingh C. What is supportive when an adult next of kin is in critical care? Nursing in critical care. 2005;10(6):289–98.
21. Robley L, Ballard N, Holtzman D, Cooper W. The experience of stress for open heart surgery patients and their caregivers. Western Journal of Nursing Research. 2010;32(6):794–813.
22. Halm MA, Treat-Jacobson D, Lindquist R, Savik K. Caregiver burden and outcomes of caregiving of spouses of patients who undergo coronary artery bypass graft surgery. Heart & Lung: The Journal of Acute and Critical Care. 2007;36(3):170–87.
23. Nelson JE, Puntillo KA, Pronovost PJ, Walker AS, McAdam JL, Ilaoa D, et al. In their own words: Patients and families define high-quality palliative care in the intensive care unit. Critical Care Medicine. 2010;38(3):808–18.
24. Micik S, Borbasi S. Effect of support programme to reduce stress in spouses whose partners ‘fall off’ clinical pathways post cardiac surgery. Australian Critical Care. 2002;15(1):33–40.
25. Mathew JE, Azariah J, George SE, Grewal SS. Do they hear what we speak? Assessing the effectiveness of communication to families of critically ill neurosurgical patients. Journal of Anaesthesiology, Clinical Pharmacology. 2015;31(1):49–53.
26. Hughes F, Bryan K, Robbins I. Relatives’ experiences of critical care. Nursing in Critical Care. 2005;10(1):23–30.
27. Schenker Y, White DB, Asch DA, Kahn JM. Health-care system distrust in the intensive care unit. Journal of Critical Care. 2012;27(1):3–10.
28. Gibson V, Plowright C, Collins T, Dawson D, Evans S, Gibb P, et al. Position statement on visiting in adult critical care units in the UK. Nursing in Critical Care. 2012;17(4):213–8.
29. Dreyer A, Nortvedt P. Sedation of ventilated patients in intensive care units: relatives’ experiences. Journal of Advanced Nursing. 2008;61(5):549–56.
30. Jongerden IP, Slooter AJ, Peelen LM, Wessels H, Ram CM, Kesecioglu J, et al. Effect of intensive care environment on family and patient satisfaction: a before–after study. Intensive care medicine. 2013;39(9):1626–34.
31. Health talk.org. Intensive care: experiences of familiy & friends 2015 [updated 2016, cited 13.10.2016]. Available at: http://www.healthtalk.org/peoples-experiences/intensive-care/intensive-care-experiences-family-friends/topics.
32. Olsen KD, Dysvik E, Hansen BS. The meaning of family members’ presence during intensive care stay: A qualitative study. Intensive and Critical Care Nursing. 2009;25(4):190–8.
33. Kelly SE. Qualitative interviewing techniques and styles. In: Dingwall R, De Vries R, Bourgeault I, eds. The Sage handbook of qualitative methods in health research. London: Sage; 2010. s. 307–26.










Comments