Doctor’s visits to nursing homes: Are out-of-hours doctors given sufficient patient information?
The out-of-hours doctor did not receive formal patient information in at least half of the doctor’s visits to nursing homes in Oslo. This may subject the patients to inappropriate treatment and unnecessary hospitalisation.
Background: The Oslo out-of-hours primary healthcare service is responsible for making doctor’s visits when the nursing home doctor is unavailable. Out-of-hours doctors report that the patient information they are given varies widely.
Objective: To chart the patient information provided to out-of-hours doctors during nursing home visits. We also sought to identify factors associated with the availability of patients’ medical records, information about advance care plans, and the active treatment commenced.
Method: Out-of-hours doctors filled out a survey for each nursing home visit in Oslo during a three-month period in 2013. We analysed the data as a cross-sectional study with binary logical regression.
Results: We registered a total of 362 doctor’s visits. Altogether 60.2 per cent of the patients visited were women, 76.0 per cent were > 80 years old, and 68.5 per cent were assessed as being cognitively impaired or having dementia. The most frequent reasons for the visits were infections and symptoms in the urinary tract (26.8 per cent) and respiratory tract (25.7 per cent). Of the total number of patients, 18.5 per cent were hospitalised. Parenteral treatment was administered to 14.1 per cent of the patients.
The out-of-hours doctor was not given access to the patient’s medical record in 52.5 per cent of the visits. Patient age under 80 years old was positively associated with access to the patient’s medical record [odds ratio, OR 1.68 (1.07–2.81), p = 0.05]. Factors negatively associated with access to the patient’s medical record were visits during the daytime on weekdays [OR 0.49 (0.25–0.97), p = 0.04] or when the doctor perceived that the care staff were unfamiliar with the patient [OR 0.23 (0.11–0.48), p < 0.01]. Out-of-hours doctors were informed about decisions relating to reduced therapeutic intensity for a small number of patients: hospital admission (21.3 per cent), intravenous treatment (17.1 per cent), attempt at cardiopulmonary resuscitation (19.6 per cent).
Explanatory variables positively associated with receiving such information were that the patient had a limited ability to communicate [OR 2.13 (1.31–3.46), p < 0.01] or that the doctor’s visits took place during the daytime [OR 1.97 (1.3–3.76), p = 0.04]. Doctors commenced active treatment at the nursing home less often for patients in sheltered units than for those in open wards [OR 0.46 (0.23–0.95), p = 0.04].
Conclusion: The finding that out-of-hours doctors regularly were not given or did not acquire clinical background information about acutely ill nursing home patients represents a quality-related problem for diagnosis and treatment. Inappropriate treatment and unnecessary hospitalisation are potential consequences.
The out-of-hours primary healthcare service is called when nursing home residents experience acute illness, injury or death, and the nursing home doctor is not available. In Oslo, this service is responsible for arranging doctor’s visits, which are coordinated by an experienced nurse at the emergency medical communication centre. The nursing coordinator at the centre decides whether the condition is acute or whether it can wait until the next work day when the nursing home doctor is present.
The handbook for doctor’s services at nursing homes states that a nursing home doctor must conduct an intake interview with the patient and/or the patient’s family and write comments in an intake journal (1–2). The intake journal should include items such as information about the patient’s diagnoses, medications the patient is taking, and a description of the patient’s physical and mental capacity.
Many nursing home patients are in the final phase of life, and the disadvantages of active medical treatment and hospitalisation may outweigh the benefits. Nursing home doctors are therefore recommended to document any assessments and decisions about treatment intensity in the patient’s medical record in the event of acute deterioration of the patient’s condition or illness in the future (3).
Must clarify advance care plans
To ensure good, individualised treatment, it is the nursing home doctor’s responsibility to ensure that the patient’s values and wishes regarding life-prolonging treatment are clarified. The doctor must also ensure that the information about such values and wishes is easily accessible if the patient is examined and treated by doctors who do not know him/her, and when hospitalisation might be necessary (4).
Thorough advance care planning entails discussing with the patient and/or the patient’s family whether it is best to refrain from intravenous fluid or antibiotic therapy and hospitalisation if acute illness occurs, or from an attempt at cardiopulmonary resuscitation (CPR) in the event of heart failure.
Advance care plans provide especially useful information for out-of-hours doctors who are called in to treat acutely ill nursing home residents: This is because, firstly, the doctor has not met the patient before; secondly, a large percentage of nursing home patients are cognitively impaired and have a limited ability to speak for themselves; and thirdly, nursing home patients usually have a short life expectancy.
Families may have unrealistic expectations
The family’s wishes probably have an influence on the out-of-hours doctor’s decision regarding treatment intensity and hospitalisation (5). Previous studies show that the family’s views and participation in discussions about treatment intensity may supersede the patient’s wishes and what is clinically regarded as appropriate life-prolonging treatment (6, 7).
Families that have not had the chance to discuss the level of intervention in the event of acute illness while the patient is still stable are often unprepared for a sudden deterioration of the patient’s condition. Even though the acute deterioration signals that the patient is actually about to die, unprepared family members may have unrealistic expectations about medical treatment and therefore insist that the patient is admitted to hospital.
Out-of-hours doctors need correct patient information
The decision of the out-of-hours doctor regarding hospitalisation and commencement or cessation of treatment is taken on the basis of the available medical information about the patient and the doctor’s clinical assessment. An out-of-hours doctor who is called in to treat an acutely ill nursing home patient may have difficulties assessing the appropriate level of intervention for any treatment.
A lack of medical information about the patient’s normal condition and wishes, as well as any information from the family, may make it difficult to choose good treatment options and increases the likelihood of overtreatment and unwelcome hospital stays (5, 8). Hospitalisation may be useful for diagnostic clarification and treatment that may result in a better chance of survival or functioning (9).
Nursing home staff feel unsure about palliation
However, emergency hospitalisation for physically frail patients with serious dementia and a short life expectancy will often be inappropriate, especially if good, palliative treatment can be provided at the nursing home (10). In the experience of the Oslo out-of-hours primary healthcare service, nursing home staff are often unskilled and feel unsure about administering palliative treatment.
A lack of qualified nursing home staff most commonly occurs outside of normal working hours and at weekends, when the percentage of unskilled staff is highest (11). During weekend and night shifts, on-duty nurses are often responsible for multiple wards where the nurses do not know all the residents.
When acute deterioration of a chronic condition occurs, having prior clarification on the treatment intensity and interventions and easily accessible documentation in the patient’s medical record will be beneficial and save resources. Staff that must provide palliative care feel a greater sense of security when advance care plans are already in place should the patient’s condition rapidly deteriorate (12).
Two-thirds of Norwegian nursing homes reported in a recent survey that they ‘always’ or ‘frequently’ had conversations with patients about preparing for such a scenario (7). This is far more than a similar study from 2007 in which few nursing homes reported having had such conversations (13). However, we know very little about how the content of these conversations is documented.
Objective of the study
Doctors at the Oslo out-of-hours primary healthcare service have reported that the patient information they are given at the nursing homes they are called to varies widely. The objective of our study was to compile an overview of the medical information that Oslo municipality’s out-of-hours doctors are given when they call on nursing home patients in the municipality. We also asked the out-of-hours doctors about the potential consequences that insufficient patient information could have for their diagnosis and treatment of patients.
Methods
Survey
Doctors permanently employed at the Oslo out-of-hours primary healthcare service make visits during the daytime (n = 48), while GPs with on-call shifts make visits in the evening and at night (n = 311). The out-of-hours doctors completed a questionnaire in connection with visits to nursing homes in the period from 21 May–20 August 2013. The survey asked questions regarding visits for both short-term and long-term residents, regardless of whether the patient lived in a sheltered unit or an open ward. Visits for the purpose of completing a death certificate were not included in the study.
Part I of the survey provides a general description of the patient (gender, age, cognitive functioning, actual diagnosis and type of unit). Part II documents the patient information that was made available during the visit (intake journal and annual examination) and whether advance care plans (hospital admission or antibiotics in case of acute illness, or CPR in the event of heart failure) were made available.
In Part III, the visiting doctors listed the interventions that were carried out (active treatment, hospital admission or no intervention). They also gave their assessment of the treatment indications (clear or unclear) and of relevant information in the patient’s medical record, as well as the care staff’s familiarity with the patient.
Information for the participants
The lead author held informational meetings for permanently employed doctors and nurses at the Oslo out-of-hours primary healthcare service prior to the survey period. Coordinators at the emergency medical communication centre distributed registration forms and provided the doctors with information about the study when they arrived at work, before their shifts began. Information about the study and registration forms were also given to the doctors’ permanent drivers, who were encouraged to make the forms easily accessible for the doctors when they visited nursing homes. We only included the data in our study when the registration form was filled out.
Analysis
We chose to analyse the doctor’s visits as independent, individual events, and did not take into account the potentially uneven distribution of the number of visits at the various nursing homes. We used binary logical regression to identify potential explanatory variables associated with various factors, e.g. the patient’s medical record was made available, information about advance care plans was provided, or active treatment was commenced.
The logical regression was performed in three stages and based on unadjusted analyses. This was followed by the full model (Model 1) with all variables included. From the full model we made two new models, one of them (Model 2) for variables with p < 0.20 in the full model. The other one (Model 3) only included variables from the full model when the significance level was <0.05.
We used the Akaike Information Criterion (AIC) (14) for each stage in the model adjustment (Models 1–3) in the logical regression to check whether including one or more variables improved adjustment of the model. The model with the lower AIC value was regarded as the most suitable one. We therefore use this one as the basis for our presentation of results. We performed all the analyses using Stata/SE 13, and set the significance level at 5 per cent.
Approvals
The project was submitted to the Regional Committees for Medical and Health Research Ethics (REC), which responded that this quality study did not require its approval. We deemed it unnecessary to obtain approval from the Norwegian Centre for Research Data, as we did not record any personally identifiable information, either for patients or for doctors.
Results
During the 92-day survey period, Oslo municipality’s out-of-hours doctors made 610 visits to nursing home patients in the region. Fifty visits concerned deaths, and in the case of the remaining 560 visits, we received registration forms from the doctors in 362 (64.6 per cent) of the cases. Some forms were not completely filled out so that the denominator for some of the variables was less than 362.
The characteristics of the 362 nursing home residents visited by Oslo municipality’s out-of-hours doctors are shown in Table 1. The majority of the patients (60.2 per cent) were women with an average age of 86. The doctors observed that 68.5 per cent of the residents had cognitive impairment or dementia. Most of them (56.1 per cent) had been living at the nursing home for more than three months (Table 1).
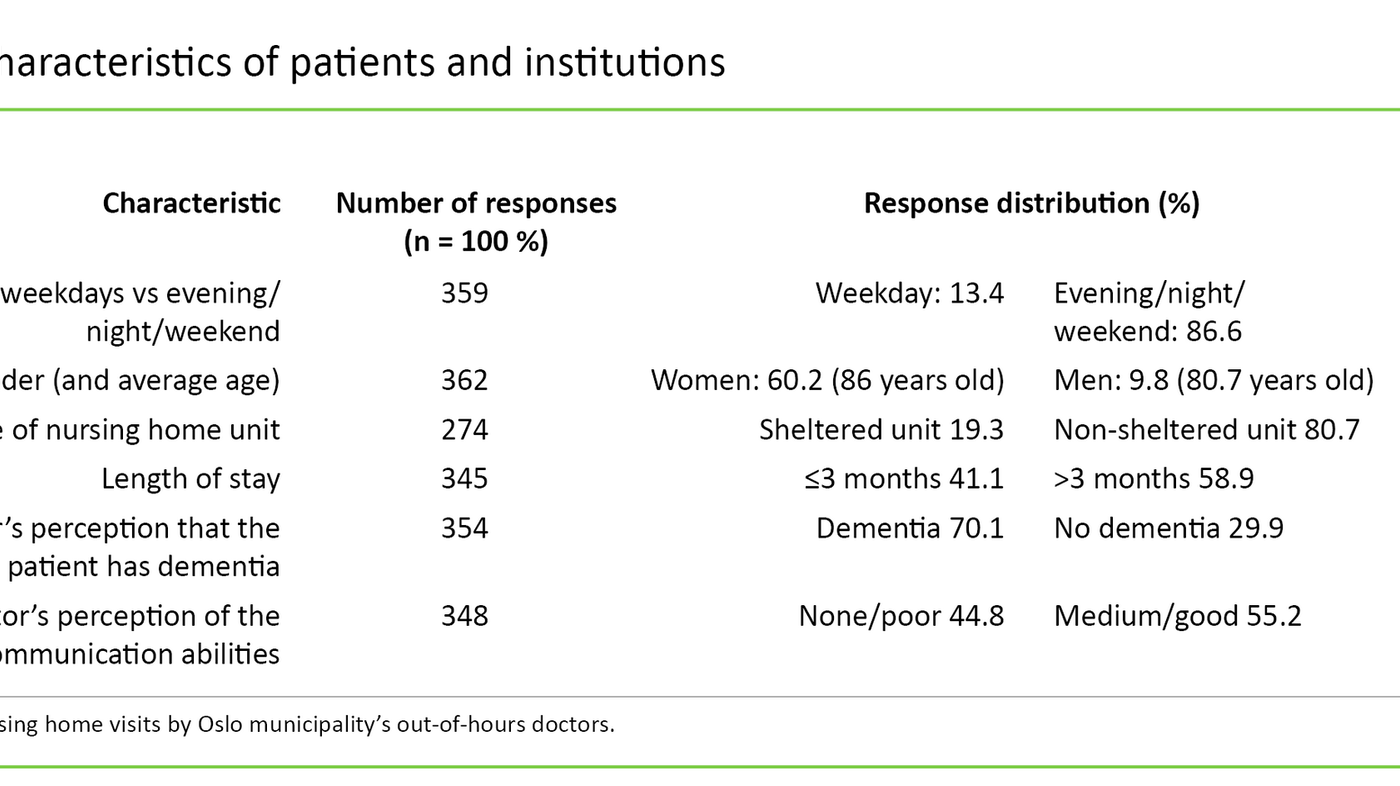
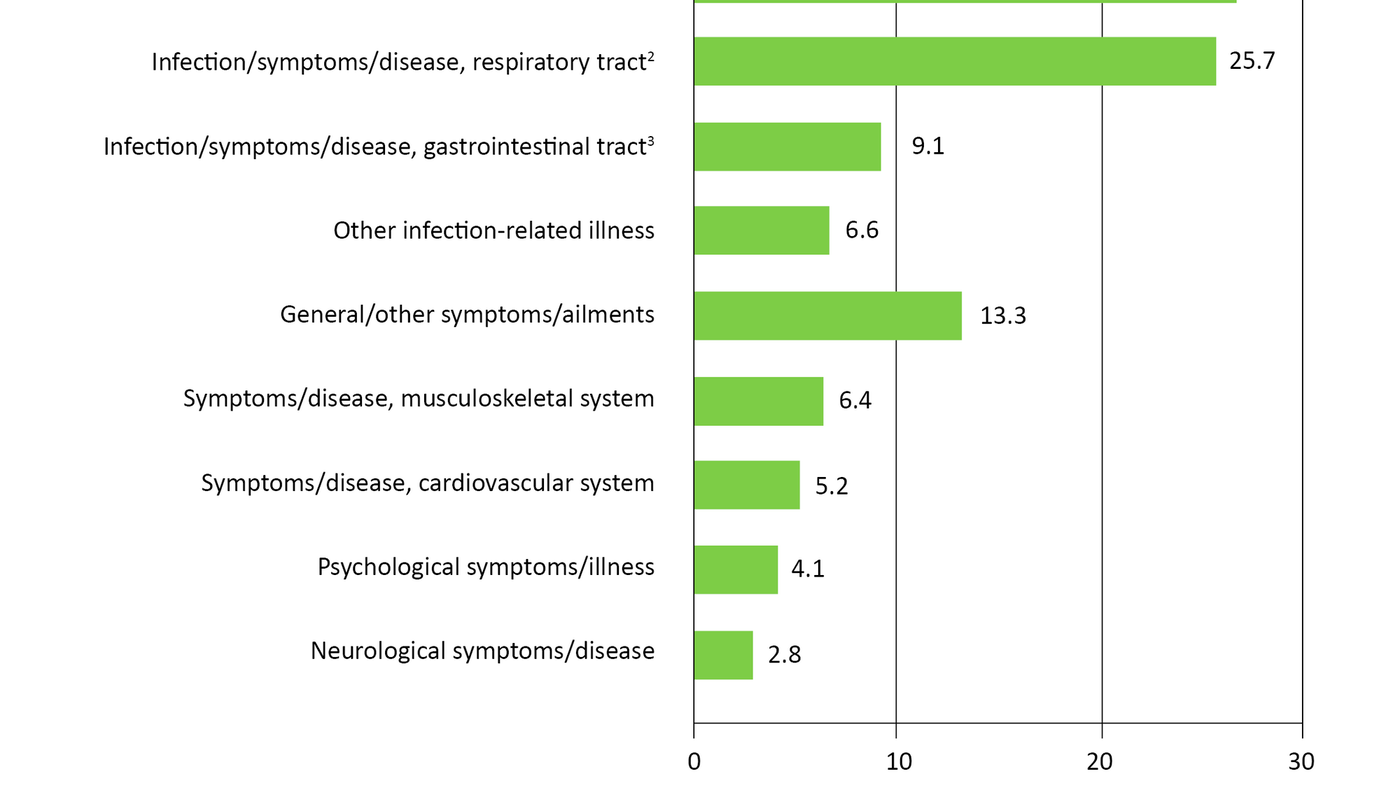
At least half of the patients were diagnosed with infections or symptoms in the urinary or respiratory tract (26.8 and 25.7 per cent, respectively) (Figure 1).
Altogether 18.5 percent of the patients were hospitalised. The out-of-hours doctors were not given written patient information at the nursing home in 52.5 per cent of the visits (Table 2). Factors positively associated with the doctor being given access to the patient’s medical record was a patient’s age less than 80 years [odds ratio (OR) 1.68 (1.07–2.81), p = 0.05].
Factors negatively associated with access to the patient’s medical record were that the visit took place during the daytime on a weekday [OR 0.49 (0.25–0.97), p = 0.04] or that the doctor perceived that the care staff did not know the patient well [OR 0.23 (0.11–0.48), p < 0.01].
The out-of-hours doctors were only informed of decisions relating to reduced therapeutic intensity for a small number of patients: hospital admission (21.3 per cent), intravenous treatment (17.1 per cent), attempt at cardiopulmonary resuscitation (19.6 per cent) (Table 2).
Explanatory variables positively associated with such information were that the patient had little or no ability to communicate [OR 2.13 (1.31–3.46), p < 0.01] or that the visit took place during the daytime [OR 1.97 (1.3–3.76), p = 0.04].
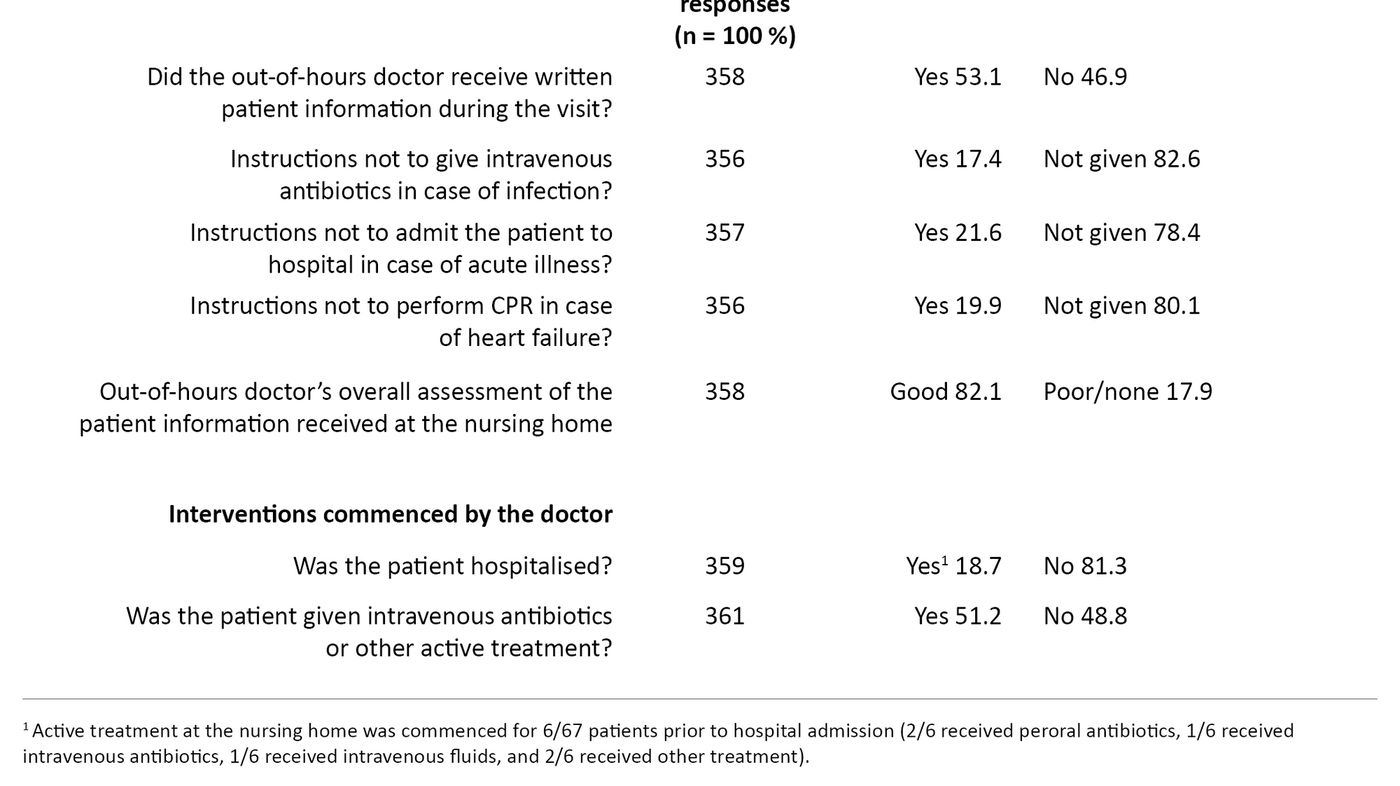
Doctors commenced active treatment, such as intravenous fluids and/or antibiotics, at the nursing home less frequently for patients in sheltered units versus open wards [OR 0.46 (0.23–0.95), p = 0.04].
Although less than half of the out-of-hours doctors had seen written, up-to-date patient information, the majority of those doctors (81.2 per cent) believed that they had been given sufficient information to be able to reach a diagnosis and begin treatment.
Discussion
Formal patient information was not given to out-of-hours doctors in at least half of the nursing home visits. Information about advance care plans was provided in only one-fifth of the visits. However, most of the out-of-hours doctors believed that they had sufficient information to be able to make a sound diagnosis and commence treatment.
When the health condition of a nursing home patient rapidly deteriorates, it is often a sign that the patient is about to die a natural death. A doctor unfamiliar with the patient may find it difficult to make a medical assessment in this situation. It is therefore crucial that clinical background information and decisions about therapeutic intensity are given to the out-of-hours doctors as a matter of course.
Formal patient information was not provided to the out-of-hours doctors in at least half of the nursing home visits. This represents a quality-related problem since it can make reaching a diagnosis and choosing treatment options more difficult. Thus, our study suggests that the quality of the cooperation between the nursing home and the out-of-hours doctor may need to be improved.
Insufficient information about refraining from CPR
In almost eight of ten nursing home visits, the doctor reported that there was no information about whether to refrain from cardiopulmonary resuscitation (CPR) in the event of acute heart failure or that intravenous treatment or hospitalisation was not desired. In most cases, CPR performed on multimorbid residents with cognitive impairment and a short life expectancy represents futile overtreatment, which in itself raises ethical questions.
Nursing home residents usually have dementia or cognitive impairment. They often lack the ability to state whether or not they want active treatment. It is therefore reassuring that information about advance care plans was available more often in those cases where the patient was unable to communicate with the doctor.
Short life expectancy and the diminishing benefit of active treatment underscores the general need to have information about treatment intensity and emergency hospitalisation easily available. This can prevent potentially harmful overtreatment and unnecessary, difficult hospitalisation.
Pressure to admit patients to hospital
Regarding the issue of hospitalisation, a Norwegian focus group study on cooperation between nursing home doctors and hospital doctors revealed that the nursing home doctors put great emphasis on avoiding unnecessary admissions (15). The nursing home doctors said that they write in the patient’s medical record in advance if a patient should not be hospitalised, but that out-of-hours doctors often admitted the patient anyway. The nursing home doctors also pointed out that they often feel pressure, from both family and staff, to hospitalise acutely ill nursing home patients (15).
Family members take part more often in conversations about treatment intensity than the nursing home patients themselves (7). This emphasises the need for knowledge among healthcare personnel about ethical considerations and current statutory provisions on patient and service user rights (6, 16). A minority of Norwegian nursing homes have guidelines for such conversations, and the content of the conversations varies (7).
Many unskilled and substitute workers
Unskilled personnel and substitutes continue to comprise a large share of the staffing in Norwegian nursing homes (11). It is alarming that out-of-hours doctors had less access to patients’ medical records during visits in which they perceived that the care staff had little familiarity with the patient in question. Care staff who are unfamiliar with the patient are probably more uncertain in treatment situations, and it is therefore likely they will more often want the patient to be hospitalised.
Oslo municipality’s out-of-hours doctors are most often called in on evenings, nights and weekends, when the nursing home doctor is not available and the proportion of unskilled employees is greatest (11). In such cases, it is particularly important that information about limitations on possible therapeutic interventions in the event of acute illness is easily available to the out-of-hours doctor (1).
A few nursing homes in Norway have introduced on-call schemes for their own nursing home doctors to ensure that the patients can receive adequate emergency treatment at the nursing home and to avoid unnecessary transport to the out-of-hours clinic or admission to hospital (17).
Difference for those over and under 80?
It is also thought-provoking that the care staff in nursing homes more often give doctors the patient’s medical record for nursing home residents under 80 years of age than for those over 80. However, it should be mentioned that patients under 80 comprised only 24 per cent of the nursing home residents visited by an out-of-hours doctor.
Information about therapeutic intensity was provided more often during daytime visits, which corresponds well with the fact that there are more staff working at that time of day who know the patient well. On the other hand, the finding of less access to medical records during daytime visits on weekdays can be explained because permanent employees who are familiar with the patient in question are usually at work then.
Difficult access to medical records
Two-thirds of Norwegian nursing homes carry out conversations about advance care plans (7), but little is known about how decisions taken during such conversations are documented. Our study may suggest that the availability of such patient information does not conform with current guidelines (1, 16). In addition, many doctors find that Gerica, the medical records system used at nursing homes in Oslo, is generally very cumbersome and time-consuming to navigate. This may have made access to medical records difficult, but we did not explore this aspect in our study.
When the preliminary results from this study were presented to Oslo municipality’s out-of-hours doctors, they told us that they managed fine without access to more detailed patient information in certain situations, e.g. changing a catheter or prescribing peroral antibiotic treatments for infections of the urinary or respiratory tract. Furthermore, they had become used to not expecting patient information to be available about limitations on therapeutic intensity, although it would clearly have been beneficial.
The out-of-hours doctors described the ‘on-call doctor’s nature’ as the ability to make a diagnosis and assess interventions without much background information about the patient. They believed that factors such as satisfaction with one’s own effort vis-à-vis the patient and the opportunity to discuss the problem with on-duty care personnel probably had affected their evaluation of the patient information they had received during their nursing home visit.
Limitations of the study
A limitation of our study is that we did not chart whether the out-of-hours doctors requested the patient information when such information was not provided to them by the care staff as a matter of course. Is it the doctor’s responsibility to ask for this information or does the responsibility rest primarily with the nursing home staff? Or is it a joint responsibility? Regardless of how responsibility is assigned, our study indicates that establishing clearer routines in this area may be necessary.
It is important to mention that there are geographical differences in how out-of-hours doctor services and nursing home services are organised. We have described the challenges related to patient documentation during doctor visits at nursing homes in Oslo, but it is natural to assume that out-of-hours doctors outside of Oslo are also familiar with this problem. However, a factor that distinguishes Oslo from most other municipalities in Norway is that the Oslo out-of-hours primary healthcare service has permanently employed doctors that make home visits during the daytime. Outside of daytime hours and at weekends, however, it is the GPs with on-call shifts who perform this task.
Changes at the conclusion of the study
Since the conclusion of this study in 2013, many municipalities have established better routines for documenting patient and/or family conversations about treatment intensity. Oslo municipality has launched a palliation project (18) which aims to formulate the most appropriate level of medical treatment for patients with a short life expectancy. More emphasis is now being placed on conversations between the patient, family members and healthcare personnel about issues related to end-of-life, as well as planning and documentation of the final phase of life.
Since 2010, a separate module for advance care plans has been available in the Gerica medical records system. While in 2013 this module was only used for 0.5 per cent of the patients in Oslo with a permanent nursing home place, this number increased to 42 per cent in 2014 and 86 per cent in 2017, according to the nursing home agency in Oslo municipality (figures from Gerica on 15 May 2018 given verbally). The availability of such documentation will probably facilitate the on-duty nurse’s communication with the out-of-hours doctors and the doctor’s decisions during nursing home visits.
Conclusion
If out-of-hours doctors are not given access to relevant clinical background information about acutely ill nursing home patients, this represents a quality-related problem for diagnostics and treatment, which may result in inappropriate treatment and unnecessary hospitalisation.
The study has received a grant from the General Medical Research Committee of the Norwegian Medical Association. We wish to thank all the participating doctors for filling out the registration form.
References
1. Helsedirektoratet. Veileder IS-1436. Legetjenester i sykehjem – en veileder for kommunene. Oslo; 2007.
2. Høie J. Sykehjemmenes oppgaver og legens rolle. Tidsskr Nor Legeforen. 2005;125(8):1009–10.
3. Engtrø E, Nore SP, Kittang BR, Krüger K. Metodebok for sykehjemsleger. Bergen: Bergen kommune; 2015.
4. Helsedirektoratet. Beslutningsprosesser ved begrensning av livsforlengende behandling. Revidert 2013. Oslo; 2009.
5. Ouslander JG, Naharci I, Enstrom G, Shutes J, Wolf DG, Alpert G, et al. Root cause analyses of transfers of skilled nursing facility patients to acute hospitals: Lessons learned for reducing unnecessary hospitalizations. JAMDA. 2016;17(3):256–62.
6. Romøren M, Pedersesn R, Førde R. How do nursing home doctors involve patients and next of kin in end-of-life decisions? A qualitative study from Norway. BMC Med Ethics. 2016;17:5. DOI: 10.1186/s12910-016-0088-2.
7. Gjerberg E, Lillemoen L, Weaver K, Pedersen R, Førde R. Forberedende samtaler i norske sykehjem. Tidsskr Nor Legeforen. 2017;137(6):447–50.
8. von Hofacker S, Naalsund S, Iversen GS, Rosland JH. Akutte innleggelser fra sykehjem til sykehus i livets sluttfase. Tidsskr Nor Legeforen. 2010;130(17):1721–4.
9. Ranhoff AH, Linnsund JM. Når skal sykehjemspasienter innlegges i sykehus? Tidsskr Nor Legeforen. 2005;125(13):1844–7.
10. Björck M, Wijk H. Is hospitalization necessary? A survey of frail older persons with cognitive impairment transferred from nursing homes to the emergency department. Scand J Caring Sci. 2018;32(3):1138–47. DOI: 10.1111/scs12559.
11. Dolonen KA. Ikke etter planen. Sykepleien 12.08.2009. Available at: https://sykepleien.no/2009/08/ikke-etter-planen(downloaded 20.05.2017).
12. O’Neill B, Parkinson L, Dwyer T. Nursing home nurses’ perceptions of emergency transfers from nursing homes to hospital: A review of qualitative studies using systematic methods. Geriatric Nursing. 2015;36(6):423–30.
13. Gjerberg E, Førde R, Bjørndal A. Staff and family relationships in end-of-life nursing home care. Nurs Ethics. 2011;18:42–53.
14. Akaike H. A new look at the statistical model identification. IEEE Trans Automat Contr. 1974;356:716–23. DOI: 10.1109/TAC.1974.1100705.
15. Romøren M, Pedersen R, Førde R. Én pasient, to verdener – samhandling mellom sykehjemsleger og sykehusleger. Tidsskr Nor Legeforen. 2017;137(3):193–7.
16. Lov 2. juli 1999 nr. 63 om pasient- og brukerrettigheter (pasient- og brukerrettighetsloven). Available at: https://lovdata.no/dokument/NL/lov/1999-07-02-63 (downloaded 19.05.2017).
17. Bollig G, Husebø BS, Husebø S. Vakttjeneste for leger i sykehjem. Tidsskr Nor Legeforen. 2008;128(23):2722–4.
18. Sluttrapport palliasjonsprosjektet 2016–2017. Kompetanseheving i lindrende behandling, pleie og omsorg for alvorlig syke og døende. Sykehjemsetaten.










Comments