Daily life after a kidney-pancreas transplantation
A successful kidney-pancreas transplantation improves and stabilises patients’ daily lives. It also brings with it new elements of uncertainty that are important to convey to the patient.
Background: A successful kidney-pancreas transplantation (KPT) is the most effective treatment for patients with diabetes who develop late-stage chronic renal failure. Although studies show an improvement in self-reported quality of life following a KPT, daily life can nevertheless be challenging due to the risk of organ rejection and side effects from immunosuppressive drugs. Little is known about KPT recipients’ personal experiences of the transition from chronic disease to daily life after a KPT.
Objective: To examine patients’ experiences in the transition from a life with diabetes and chronic renal failure to daily life in the first year after a KPT.
Method: The study has an exploratory design, and data are collected through semi-structured interviews. Six men agreed to an interview at the one-year follow-up after their KPT, and we used a stepwise deductive-inductive method to analyse the interviews.
Results: Transplant recipients’ new daily life was characterised by greater autonomy, independence, coping and motivation, but also by new elements of uncertainty. The main uncertainties related to fear of the new organs being rejected and side effects from immunosuppressive drugs.
Conclusion: The study provides an insight into the everyday challenges faced by transplant recipients in the first year after a KPT. One key finding of the study was the need for a greater focus on good information before and after a KPT, both for patients and their families. More tailored patient education and psychosocial support over time can be crucial the first year after transplantation.
A successful kidney-pancreas transplantation (KPT) is the most effective treatment for patients with unstable diabetes who develop late-stage chronic renal failure (nephropathy). A transplantation can prevent further development of late-stage complications from diabetes, and to some extent reverse already existing complications (1–3).
Oslo University Hospital (OUH), Rikshospitalet is home to Norway’s only organ transplantation centre, and performs between 15 and 20 KPTs every year (4). Studies show that 87 per cent of KPT recipients are insulin-free one year after the transplantation, 78 per cent five years later and 64 per cent ten years later. Meanwhile, 95 per cent have a functioning transplanted kidney one year after a KPT, 79 per cent five years later and 59 per cent after ten years (1).
After the transplantation
Patients who have undergone a KPT often report an improvement in their quality of life (2, 5–7). Nevertheless, KPTs present new challenges in their daily lives. Following transplantation, immunosuppressive drugs are essential for preventing organ rejection (3). These drugs have a number of side effects that the recipient has to make allowances for.
In order to reduce the extent of side effects such as infections, cardiovascular disease, osteoporosis and skin cancer, transplant recipients must be mindful of their health, including good hygiene, a healthy diet, physical activity and prudent exposure to the sun (3). Following a KPT, recipients must, therefore, be vigilant for signs of infection and side effects of drugs. Organ rejection will always be a source of uncertainty (3).
In addition to changes in patients’ health situation, an organ transplantation brings about changes in roles, abilities and expectations. This requires new knowledge, new skills and, for some, new coping strategies (8, 9). Amerena and Wallace (9) showed that kidney transplant recipients had conflicting experiences in the post-transplant period. Everyday life could feel like a roller coaster, changing between good health and illness. Society viewed them as healthy even though they felt physically vulnerable and feared infections and organ rejection.
Objective of the study
Earlier studies examining the post-transplant lives of KPT patients have mainly used quantitative mapping of self-perceived quality of life (2, 5–7, 10). Few studies have investigated patients’ experiences in the transition from life with diabetes and renal failure to daily life after a KPT. The purpose of this study was therefore to identify the important aspects of the transition from the KPT patients’ perspective. We posed the following question:
‘How do people who have undergone a kidney-pancreas transplantation describe the transition from life with diabetes and chronic renal failure to daily life in the first year after the transplantation?’
The study may serve as a useful contribution to the follow-up provided both before and after a KPT.
Method
Design and sample
The study has a qualitative, exploratory design (11). We recruited informants in connection with the one-year KPT follow-up. In order to meet the inclusion criteria, participants had to be competent to give consent, speak Norwegian, have good functioning in the transplanted organs at the time of interview and not suffer from other serious medical conditions. In the period October 2013 to May 2014, eight people – seven men and one woman – were called in to the one-year follow-up. Six men agreed to participate in the study.
The informants were from different parts of Norway, aged between 38 and 46 years and had been diagnosed with diabetes type 1 25-34 years before the KPT. They had all developed nephropathy as a late-stage complication of diabetes. In addition, the majority had retinopathy with impaired vision and neuropathies with pain and reduced function in their legs prior to the KPT. None of the informants underwent dialysis.
Data collection
Data were collected through interviews with a view to obtaining rich descriptions of participants’ daily lives prior to the KPT and in the first year after the transplantation. We developed an interview guide in order to ensure we covered the same main themes with all participants. These themes were the transition from life with a chronic illness to life after the transplantation, social relationships and follow-up after the transplantation. We chose these themes based on findings from studies of quality of life following a KPT (2, 5–7, 10), transplant recipients’ experiences (8, 9, 12) and clinical experiences from transplant surgical wards.
The term ‘daily life’ was not predefined since the purpose of the study was to collect subjective descriptions of daily life. The interviews were conducted by the first author in an office near the medical outpatient clinic, and lasted for 45–80 minutes. The audio recordings were transcribed after each interview.
Data analysis
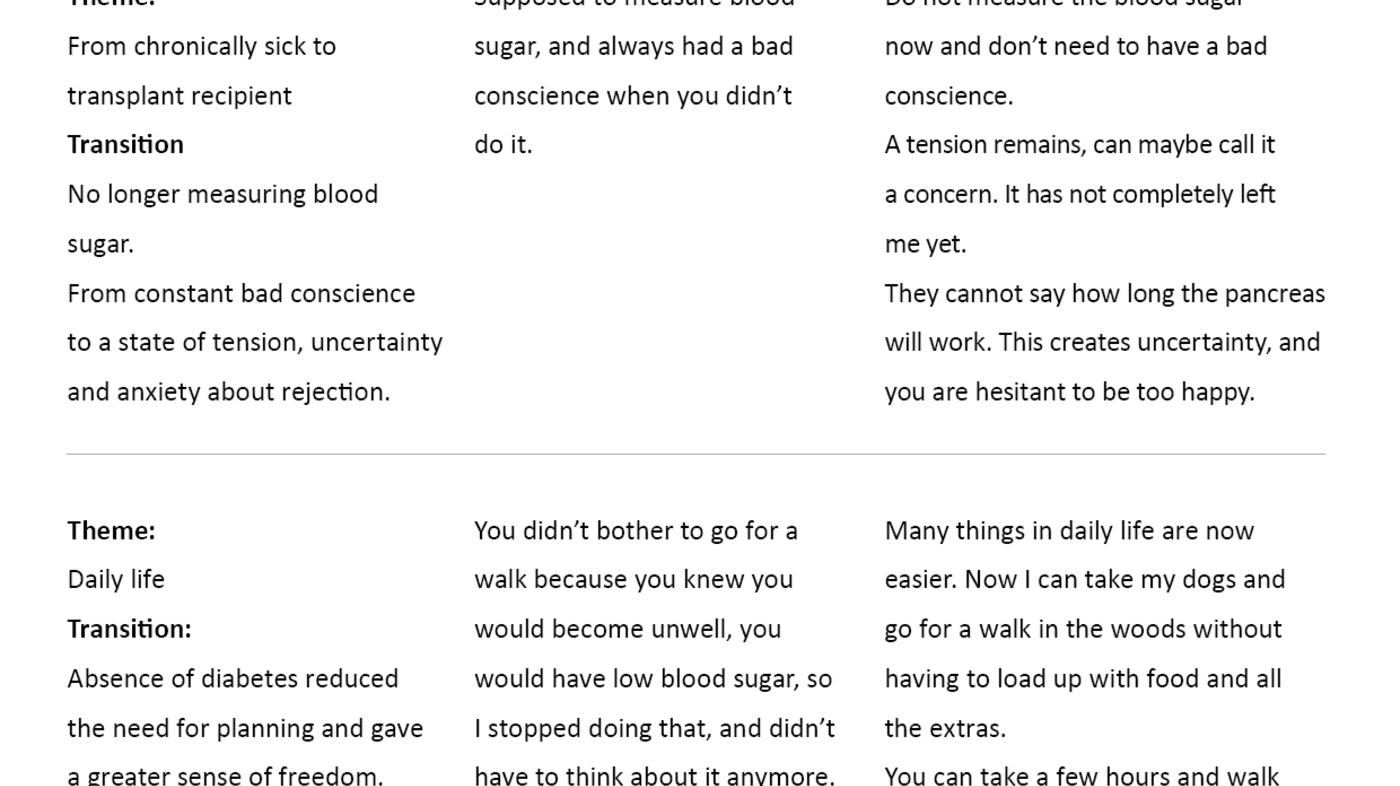
We used Tjoras’ (13) stepwise deductive-inductive (SDI) method in the analysis. This method was chosen because it is textual and because we wanted the results to reflect the participants’ descriptions as accurately as possible. We applied a deductive coding approach to the data analysis based on the words and expressions used by the informants. In order to make it easier to identify the transitions, we then categorised the codes according to pre and post-transplanttimeframes. The codes were subsequently categorised by themes and transitions, which in turn provided the basis for the main themes presented in this article (see Figure 1).
The deductive part of the SDI method entailed verifying the codes, categories, main themes and results by constantly returning to the transcribed text from the interviews. The co-author participated in the analysis. Figure 1 shows an analysis example.
Ethics
Before conducting the study, we obtained the necessary permission from the Data Protection Official, the head of research and departmental heads in the Department of Transplantation Medicine at Oslo University Hospital (OUH), Rikshospitalet. The Data Protection Official did not consider it necessary to seek approval from the Regional Committees for Medical and Health Research Ethics (REC) since the main focus of the study was on quality assurance in connection with KPTs.
Potential informants received information about the study together with their one-year follow-up letter. The information was repeated during their appointment at the medical outpatient clinic, and written informed consent was obtained from those who wanted to participate. The nurses at the medical outpatient clinic recruited the informants. The first author of the article is a nurse at the Section for Clinical Transplantation Surgery, but was on leave when the informants were admitted for transplantation. Therefore, the author did not meet the informants before the interviews.
Results
The analysis identified four main findings that dominated the transition from life with a chronic illness to life after the KPT: greater autonomy, independence, coping and motivation, in addition to some new elements of uncertainty.
Greater autonomy
The biggest change following the KPT was the informants’ stable blood sugar levels. One major area of transition was that it was no longer necessary to regularly measure blood sugar or to plan meals and activities. Before the transplantation, unpredictable blood sugar levels and the risk of hypoglycaemia and loss of consciousness were a source of worry and anxiety, especially before bedtime. One informant explained it as follows:
‘I was terrified to go to bed because I never knew if I would wake up ... Now I can go to bed in the knowledge that I will wake up in the morning!’ (Informant 6).
Several informants said that before the KPT, the planning that was necessary for physical activities was tiresome. One informant expressed this as follows:
‘You couldn’t be bothered going for a walk because you knew you would become unwell anyway, you would get hypoglycaemia. So I stopped doing it, and didn’t need to think about it any longer.’ (Informant 2).
Normal levels of blood sugar gave the informants more freedom, and they were able to choose food and activities according to their own wishes as opposed to the need to stabilise their blood sugar:
‘I can walk for four to five hours without eating, it's a dream.’ (Informant 5).
The informants felt they had greater autonomy and more stability in their daily lives.
All of the informants had been affected by their renal failure to some degree, experiencing tiredness and fatigue before the transplantation. They said that they felt exhausted at the end of the working day, and that they had little energy left to engage in family life or other social activities:
‘I didn’t realise just how ill I had become, daily life had become a real struggle.’ (Informant 3).
One year after the transplantation, all of the informants described how they had considerably more energy in their daily lives and at work, which played a large role in their experience of freedom and autonomy.
Greater independence
Four of the six informants had very unstable blood sugar levels before the transplantation, and two had ‘unawareness’ symptoms where they did not feel any sign of hypoglycaemia. These informants in particular were therefore dependent on family, friends and colleagues knowing what to do in the event of a hypoglycaemic episode. One informant told how he had to explain to new colleagues what to do if he had such an episode. Another described how colleagues had to contact his parents if he did not show up at work in the morning.
One year after the transplantation, the informants expressed their sense of relief at being less dependent on others. They also found that relatives were no longer worried and anxious, and they also felt relief. One informant described this as follows:
‘My mum has lost a huge weight from her shoulders ... she sleeps well at night now.’ (Informant 2).
The informants also said they felt a sense of relief as they no longer had to feel guilty about passing the responsibility to others when they had a hypoglycaemic episode. Their new daily life after the transplantation therefore meant greater independence and a less guilty conscience towards others.
Greater coping and motivation
Several informants described how challenging it was to monitor their own health in a satisfactory manner before the transplantation. They suffered from a guilty conscience if they did not monitor their blood sugar levels well enough, and felt that the late-stage complications of diabetes were their own fault:
‘Ideally, you were supposed to measure your blood sugar, and when you didn’t, you had a constant guilty conscience.’ (Informant 1).
‘I don’t need to have a guilty conscience all the time, because whatever you do, you never feel that you’ve done enough (talking about the time prior to KPT).’ (Informant 3).
The informants further explained how risky it was to follow the doctor’s recommendation for a low long-term blood sugar level, because the risk of hypoglycaemia increased. Although they knew that hyperglycaemia could have adverse effects on their body, several of the informants said they preferred a high blood sugar level, especially before they went to bed or before driving:
‘I was anxious about having a hypoglycaemic episode so I took very little insulin.’ (Informant 4).
After the transplantation, it was easier to exercise and have an active life. The informants were no longer reliant on sugary foods and drinks to prevent hypoglycaemic episodes. It was easier to choose a healthy lifestyle, and many coped better and felt more motivated to take care of their own health.
New elements of uncertainty
A significant source of uncertainty for the informants after the transplantation was the risk of organ rejection. One informant described it as a sense of uneasiness that occurred immediately after the transplantation, and that stayed with him. The informants dealt with this uncertainty in different ways. Some collected stories about transplant recipients whose transplantation had been performed a long time ago. Others relied on medical developments, while some avoided thinking about it and wanted to focus on the present. However, several expressed concern about potential rejection. One informant said he went from having a constant guilty conscience about not monitoring his blood sugar level properly to feeling uncertain and concerned about the lifetime of the organs:
‘It creates uncertainty, and makes you hesitant about feeling too happy.’ (Informant 1).
Another informant found it difficult to apply for a new job because he was afraid of becoming an unreliable employee. Several of the informants also mentioned that the fear of organ rejection was not a topic that healthcare personnel discussed very much with them. It was difficult for some of the informants to talk to those closest to them about this uncertainty, largely because they did not want to worry them:
‘I try to avoid saying things that can frighten her [his wife].’ (Informant 3).
The uncertainty surrounding potential organ rejection led to the informants frequently measuring their blood sugar levels for a long time after the transplantation. A blood sugar reading served as effective confirmation that the pancreatic transplant was working well. The informants described a combination of positive curiosity and fear associated with measuring blood sugar levels:
‘After six to seven months, the doctor told me to stop, but it’s intriguing to keep monitoring it ... you become curious and then you become afraid.’ (Informant 5).
‘I didn’t really believe in this, so I measured my blood sugar much more after the transplantation than before.’ (Informant 6).
Three out of six informants reported that they had symptoms of abnormal blood sugar even though the measurements were within the reference range. They described symptoms of hypoglycaemia, such as tremors and ‘a sensation in the stomach’ (informant 6), or symptoms of hyperglycaemia, such as dry mouth or ‘a strange feeling in the body’ (informant 4). An abnormal blood sugar reading could increase their fear of organ rejection and cause them to measure their blood sugar more often.
Another important element of uncertainty for the informants was the side effects from immunosuppressive drugs. Five of the informants reported periods of diarrhoea and/or obstipation. Some reported having a poor appetite, constantly feeling hungry, tremors, rashes, excessive sweating and a reduced libido, thin and dry skin, and cuts taking longer to heal. Several had had a urinary, respiratory or wound infection, or a cytomegalovirus (CMV) infection. Infections had led to either short or long hospital stays and sick leave from work.
None of the informants had considered themselves to be sick before the transplantation because their diabetes was part of their normal life, and the renal failure happened so gradually that it was difficult to see the changes in health. An impaired immunity system and the long-lasting infections represented a new way of being sick, and for some of the informants this was both unexpected and tiresome. The informants who had suffered from frequent hypoglycaemic episodes before the transplantation nevertheless described daily life as more stable and generally better despite these new elements of uncertainty.
Discussion
Daily life after the KPT was mainly described as positive one year after the transplantation, particularly because the stable blood sugar level gave a stronger sense of autonomy, independence and coping. Nevertheless, the informants described challenges in the change from a state of uncertainty as a diabetic to a new state of uncertainty as a transplant recipient. Fear of organ rejection was the main element of uncertainty. Organ rejection can lead to elevated blood sugar levels, abdominal pains where the organ is situated, fever, flu-like symptoms, weight gain and reduced urine production (3). However, not all transplant recipients suffer such symptoms. It is therefore essential to monitor the kidney -and pancreas function with regular blood tests, as well as a biopsy of the transplanted organs (3, 14).
Three of the informants described a sensation of abnormal blood sugar fluctuations, even though the glucose level was within the reference range. This could make it difficult to interpret the definition of ‘normal’, and what could be signs of rejection. However, Redmon et al. (15) show that symptoms of hypoglycaemia can occur in 30 to 50 per cent of pancreas transplant recipients, even when the blood sugar is within the reference range.
In order to alleviate concerns, it is important that transplant recipients who experience the sensation of abnormal blood sugar – but who are within the normal range – are told that the symptoms are normal. Nilsson et al. (14) show that many transplant recipients fear organ rejection, and that this fear does not diminish with time. Our study also shows that the fear of organ rejection is still present one year after the KPT.
Studies of kidney transplant recipients show that it can be difficult to assess and differentiate between symptoms (12, 16). For example, both fever and flu-like symptoms can be a sign of organ rejection and infection. The challenges faced when interpreting symptoms underlines the importance of close contact with the health service, and that the threshold for making contact should be low. The new elements of uncertainty require follow-up in the form of good information and psychosocial support. Our study showed that the six informants coped with the uncertainty surrounding organ rejection in different ways, whilst also reporting that it was a topic that is seldom discussed.
Patient education should be customised
The patient education provided by healthcare personnel on organ rejection is usually general and not well adapted to the individual’s thoughts about what a rejection entails or their personal coping strategies (14). Nilsson et al. (14) are concerned that healthcare personnel should acknowledge the recipient’s own thoughts about what rejection entails in order to help them form a realistic perspective of the risk and consequences. Avoidance can also be a coping technique, but this can be risky if the recipient does not want to know details that can be vital to self-monitoring and preventing organ rejection (14).
A Norwegian study of patient educational intervention after kidney transplantation showed how customised teaching for seven weeks gave good results. Providing relevant information about medication, rejection and lifestyle, as well as competence building and interactive support from nurses, led to an increase in recipients’ level of knowledge and improved self-monitoring of medication within six months. Coping expectations and perceived quality of life were also higher (16). Changes to the patient education given to recipients in the clinic have recently been implemented based on findings in Urstad’s (16) study. Since these changes were implemented after the transplantation of the informants in our study, everyday life after the KPT should also be examined in order to identify possible effects.
Side effects of immunosuppressive drugs
Five out of six informants reported various side effects from immunosuppressive drugs, including infections that had led to long-term absences from work. Such fluctuations between good health and illness can affect the recipient’s perception of autonomy, independence, coping and motivation. It is challenging and perhaps paradoxical that a recipient’s life following a KPT may still entail long periods of impaired health (9).
Some informants said that it could be difficult to share their concerns about side effects or other symptoms after the transplantation, which is consistent with other studies of kidney transplant recipients (8, 9). The role of a healthy transplant recipient can create expectations that may be challenged by a fluctuating health condition. Such expectations can prevent recipients from sharing their concerns about organ rejection, infections and side effects of medication. They can also lead to concerns not being taken seriously (8, 9).
The findings of this study indicate that there is a need for healthcare personnel to customise their conversations with transplant recipients and their families both before and after the transplantation. Conversations prior to a KPT may be useful for managing the expectations of recipients and their families, and for providing helpful information about what their new daily life after a KPT may entail. Meanwhile, conversations after the transplantation will be crucial to addressing the individual’s personal challenges and helping to establish relevant coping strategies.
Limitations of the study
The theme of the study is complex, diverse and largely unexplored. It was therefore necessary to retrieve data that could capture many aspects of daily life one year after transplantation. The interview guide could have had fewer themes to make the study more in-depth. Six out of eight potential informants were included in the study, and only men agreed to participate. The sample may be one limitation because some studies show that women, more so than men, report lower quality of life, more side effects of immunosuppressive drugs and more concern following a transplantation (6, 7, 17).
Although the majority of patients undergoing a KPT are probably men, more studies are needed on female kidney-pancreas transplant recipients. The informants had not received dialysis, and there is reason to believe that those who have undergone dialysis before a transplantation have a different experience of the post-transplantation transition. The findings in the study, however, point to important aspects of the transition to a new daily life after a KPT.
Conclusion
The findings in the study showed that the daily lives of informants were characterised by greater autonomy and independence. They expressed a greater sense of coping and improved motivation, but also new elements of uncertainty one year after the KPT. Important implications are therefore that healthcare personnel should place more emphasis on individually tailored conversations with recipients and their families before a KPT in order to manage expectations and prepare for the new set of challenges that patients may face following the transplantation. Meanwhile, it can also be crucial for the transplant recipient to receive more customised patient education and psychosocial support over time with a view to managing the challenges of daily life after a KPT.
References
1. Lindahl JP, Jenssen T, Hartmann A. Long-term outcomes after organ transplantation in diabetic end-stage renal disease. Diabetes Research and Clinical Practice 2014;105:14–21.
2. Sollinger HW, Odorico JS, Becker YTD, Alessandro AM, Pirsch JD. One thousand simultaneous pancreas-kidney transplants at a single center with 22-year follow-up. Annals of Surgery 2009;250:618–30.
3. McPhee IAM, Fronek J. Handbook of renal and pancreatic transplantation. Chichester, Great Britain: Wiley-Blackwell; 2012.
4. Bakken, PA. Organdonasjon og transplnatasjon. Oslo universitetssykehus, Rikshospitalet. Available at: https://organdonasjon.no/content/uploads/2017/01/organdonasjon-transplantasjon-4-kvartal-2016.pdf(downloaded 14.08.2017).
5. Sureshkumara KK, Patel BM, Markatos A, Nghien DD, Marcus RJ. Quality of life after organ transplantation in type 1 diabetics with end-stage renal disease. Clinical transplantation 2006;20:19–25.
6. Pera PI, Vasallo JM, Rabasa AT, Salinas FO, Laureano LFC, Brulles MJR. Quality of life in simultaneous pancreas-kidney transplant recipients. Clinical transplantation 2009;23:600–5.
7. Kwiatkowski A, Michalak G, Czerwinski J, Wszola M, Nosek R, Ostrowski K, Chmura A, Danielewicz R, Lisik W, Adadynski L. Quality of life after simultaneous pancreas-kidney transplantation. Transplantation Proceedings 2005;37:3558–9.
8. Nickles MW. Common psychiatric problems in the well transplant patient. Graft 2001;4:290–8.
9. Amerena P, Wallace P. Psychological experiences of renal transplant patients: A qualitative analysis. Counseling and Psychotherapy Research 2009;9:273–9.
10. Smith GC, Trauer T, Kerr PG, Chadban SJ. Prospective quality-of-life monitoring of simultaneous pancreas and kidney transplant recipients using the 36-itm short form health survey. American Journal of Kidney Disease 2010;55:698–707.
11. Polit DF, Beck CT. Nursing research: Generating and assessing evidence for nursing practice. Philadelphia, USA: Lippincott Williams & Wilkins; 2008.
12. Kamran F. Living with a kidney transplant: Perceptions and experiences. American Journal of Applied Psychology 2014;2:5–12.
13. Tjora A. Kvalitative forskningsmetoder i praksis. Oslo: Gyldendal Akademisk; 2012.
14. Nilsson M, Persson L-O, Forsberg A. Perceptions of experiences of graft rejection among organ transplant recipients striving to control the uncontrollable. Journal of Clinical Nursing 2008;17:2408–17.
15. Redmon BJ, Teucher AU, Robertson RP. Hypoglycemia after pancreas transplantation. Diabetes Care 1998;21:1944–50.
16. Urstad KH, Øyen O, Andersen MH, Moum T, Wahl AK. The effect of an educational intervention for renal recipients: a randomized controlled trial. Clinical Transplantation 2012;26:246–53.
17. Kugler C, Geyer S, Gottlieb J, Simon A, Haverich A, Dracup K. Symptom experience after solid organ transplantation. Journal of Psychosomatic Research 2009;66:101–10.









Comments