Health education competence, self-management
A systematic literature review shows that six competence areas play a key role in enabling health personnel to give patients and service users good outcomes from self-management programmes.
Background: The health education competence of health professionals who deliver self-management programmes to those with long-term health challenges have been little reported and discussed in either Nordic or international research literature.
Purpose: The purpose of the study is to provide a systematic literature review of studies describing key health education competencies. We included both quantitative and qualitative studies as well as a systematic literature review.
Method: We conducted a systematic literature search in Medline, Embase, PsychInfo and Cinahl to identify various types of studies describing health education skills in self-management programmes.
Results: The studies describe six competence areas considered essential for ensuring patients and service users good outcomes from self-management programmes. These areas are: knowledge and skills in group management, disease and diagnosis, communication, coping and coping strategies, education and personal qualities and attitudes. The quality of the studies varies.
Conclusion: The studies emphasise that competence in health education is crucial for ensuring that patients and service users derive benefit from self-management programmes. We need more high-quality research together with efforts to improve the quality of health education training measures and the education of students, health professionals and service user representatives.
The clinical picture in Norway like other European countries is characterised by non-infectious diseases and long-term health challenges, for example cardiovascular disease, type 2 diabetes, overweight or obesity, chronic obstructive pulmonary disease (COPD) and cancer (1). The increase in the number of people living with such challenges is due to medical progress, new lifestyle habits and longer life expectancy. Patients with chronic illnesses, service users and next of kin must learn to cope with health problems, symptoms and treatment in their everyday lives. These challenges cannot be solved by therapy, short hospital stays and outpatient contact with the specialist health service.
Self-management programmes have a different goal than treatment in that they are intended to boost the self-management abilities of the individual patient or next of kin. Norwegian health authorities stress that self-management programmes in both the specialist and municipal health services are of decisive importance in learning to cope with long-term health problems (2). Here self-management programmes are understood as programmes or initiatives that provide support and guidance in order to strengthen the individual’s ability to live with long-term health challenges (3). In this systematic review, we focus on group-based programmes in which user involvement is integrated.
A number of international literature reviews systematise research on the impact of self-management programmes in respect of biological, psychological and behavioural outcome goals (4, 5). In Norway, the Knowledge Centre for the Health Service has published literature overviews and reviews of available research. The overviews show that the quality of the studies of group-based self-management programmes and initiatives with user involvement varies, but that nevertheless such programmes and initiatives may have positive impacts (3, 6, 7).
As yet, there is little research documenting what kind of competence is important to boost self-management, and in what way.
Self-management programmes require health education competence (8–10). In Norway, self-management centres in the specialist health service support health education training programmes for health professionals and service user representatives who offer such services (11). However, health education is a relatively new discipline, and as yet, there is little research documenting what kind of competence is important in boosting self-management, and in what way. In contrast to research in the nursing, medicine and psychology professions (12–14), there is a lack of studies on the practitioner’s impact on self-management programmes, i.e. studies of the role the personal qualities of health professionals play in determining the outcome of such programmes. There are also few studies of the health professionals’ key competencies (9, 15).
Purpose
To establish what competence health personnel should possess in order to boost self-management among users, we have therefore conducted a systematic review of the research literature. Here we present research literature referring to the competence health personnel must have to be able to provide good group-based self-management programmes.
Method
A key aim of this study is to acquire an overview of what kind of studies can be found on the topic. Since research on this is limited and little reported, we chose to include both quantitative and qualitative studies. In order to be included, the studies had to discuss the importance of the health professions’ competence in respect of implementation of group-based self-management programmes where service user involvement is an important element. These were international articles written in English and with a study population in age group 18+.
We also included systematic literature reviews. In cooperation with a research librarian, we have conducted systematic literature searches in the databases Medline (Ovid), Embase (Ovid), PsychInfo (Ovid) and Cinahl (Ebsco) in the period from 1 January 2005 to 1 February 2015. We carried out the searches using the following key words in different combinations: chronic illness, patient education, professional competence, patient experience or satisfaction, group processes and patient participation.
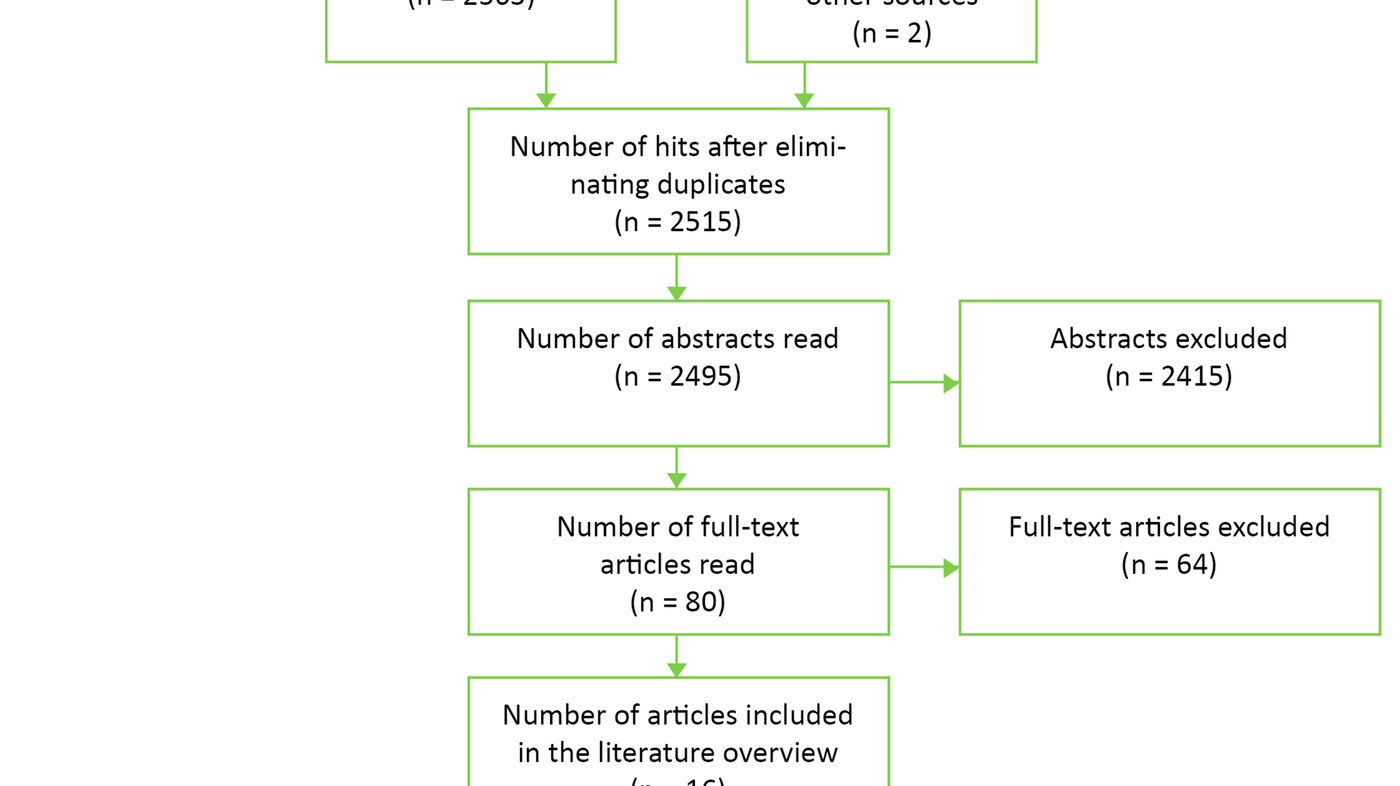
The first author carried out a preliminary sorting of titles and abstracts. Then the first author and co-author conducted a new and independent review of 103 titles and abstracts in accordance with the inclusion and exclusion criteria. We solved any disagreements through discussion. After that, the first author obtained full text versions of 80 studies. Altogether 63 studies were excluded, mainly because they did not specify competence as a topic. The first author then derived the following data from the 17 studies that were provisionally included: author, aim, design, sample and competence.
Subsequently the authors independently assessed the quality of the studies included. Based on the handbook of Kunnskapssenteret [Knowledge Centre for the Health Service] (16), the studies were assessed against checklists specific to studies with different designs. Altogether 16 studies satisfied the inclusion and quality criteria and were included in the review (Figure 1).
The research literature incorporates a variety of concepts and different understandings of professional competence and knowledge (17). This systematic review is based on a broad understanding of the concept of competence, including theoretical knowledge, vocational skills and attitudes as well as personal competence (18). By personal competence, we mean attitudes, values, experiences and manners that characterise the individual, for example the ability to establish relationships, to be mindfully attentive and to show empathy (18). This broad understanding is stressed in health and social education and professional work practice, as well as in literature on instructing patients and next of kin, and self-management (19, 20).
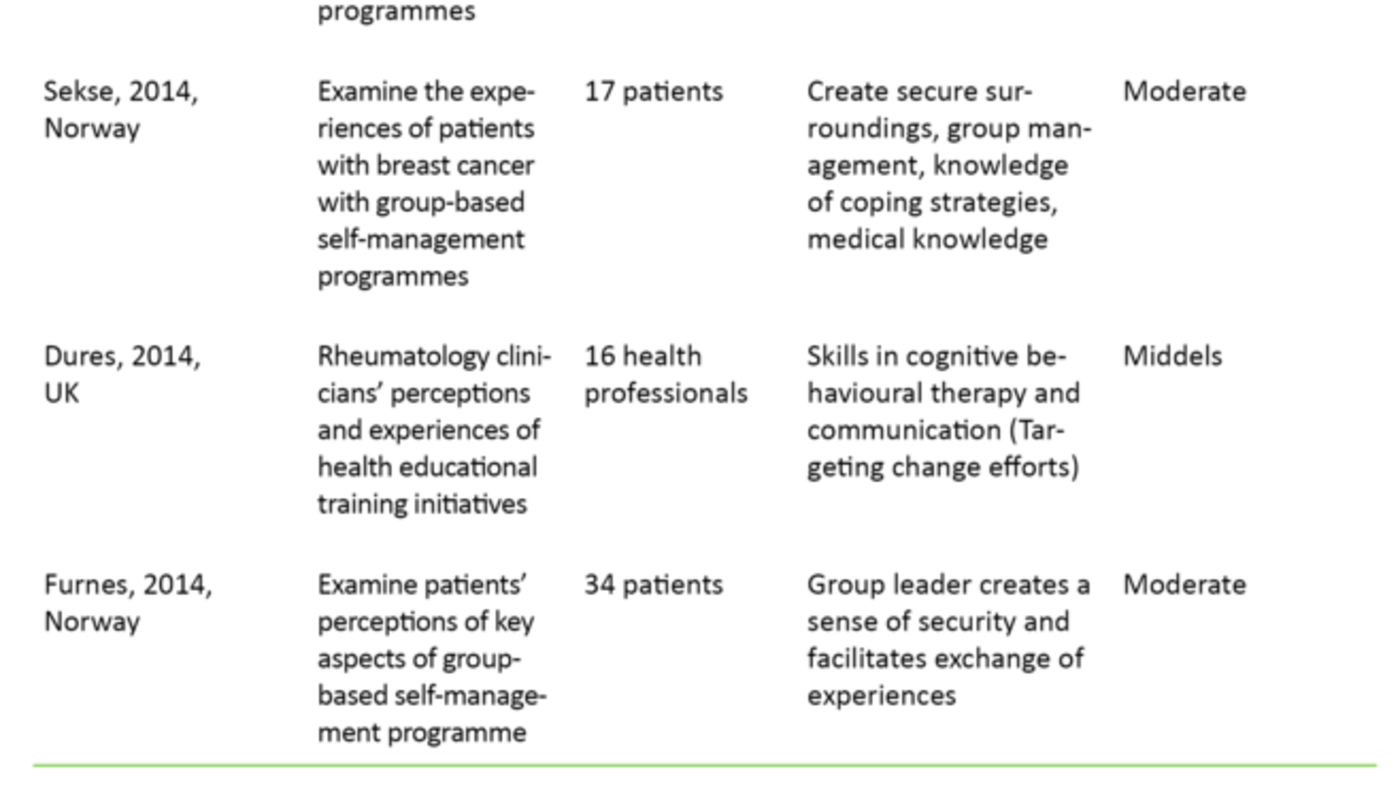
A quantitative and qualitative content analysis of the studies’ descriptions of competence was conducted (21). This entailed recording and enumerating the competencies that the studies explicitly describe. It also involved a process of coding whereby we noted, categorised and systematised the semantic content of sentences and paragraphs that more indirectly describe competence, in overarching categories. We have chosen to present the results of the literature review based on key topics derived from this content analysis. The analysis indicates what forms of competence are highlighted in the literature, cutting across study design and research question. To provide a clearer and uniform presentation, we have grouped the studies by study design in addition to author, purpose, sample, competence and quality assessment (Table 1).
Result
Most studies included deal with the perceptions held by health professionals (15, 22–27) and patients (28–34) of key competencies in health professionals offering self-management programmes. One study deals with both groups (33). The studies of patient perceptions refer to a total of 398 patients. The patients have type 2-diabetes (34), chronic pain (25, 28), cancer (31), COPD (29, 33), irritable bowel syndrome (32) and hypertension (30). Altogether 252 healthcare professionals are mentioned in the studies on how competence is perceived. The professions most often described in these studies are doctors, nurses, physiotherapists, ergonomists and nutritionists.
The majority of the studies are qualitative empirical studies (22–28, 31–34). One study is a systematic review of qualitative studies (29), and three have a mixed method-design (15, 30, 36). Using quantitative data, two studies examine the impact of health education training programmes on the acquisition of knowledge, skills and attitudes by those who are planning to provide instruction, and self-management programmes (35, 36). The 16 studies included shed light on competence from different angles. The research issues in the studies did not all focus on competence as a topic, but included it when presenting the results of the study.
Competence areas
The content analysis of the 16 studies show that there are six competence areas that are considered to be of key importance for health professionals. These areas are highlighted across the various study designs and research issues. The six competence areas are as follows:
- Group management
- Medical expertise on diagnosis and treatment
- Communication
- Coping and coping strategies
- Education
- Personal qualities and attitudes
Group management
Altogether twelve out of the 16 studies stress the importance of being able to manage groups of patients and service users in order to make adequate provision for self-management (15, 22, 24, 25, 27–34, 36). For the most part the studies describe two dimensions of group management. The first concerns the ability of health professionals to create safe and supportive environments for group participants in self-management programmes. One example is encouraging participation and making patients feel welcome, recognised and heard (15, 24).
The second dimension applies to health professionals’ ability to inspire active group participation, learning and exchange of experience using various tools and methods. For example, this might include questions and comments that encourage the individual and the group as a whole to share thoughts and feelings linked to their own life situation. Several studies of patient experiences confirm the importance of active group discussions. A diabetes patient said: ‘Being able to hear how they [other diabetes patients] experience their disease, the tricks and solutions they have for food and exercise, it is so important’ (34). Meanwhile several studies point out that health professionals find that they lack competence in managing this type of group processes in a proficient manner.
Professional expertise
Eight studies underlined that it is vital that health professionals have professional medical knowledge. They must also be updated regarding research and knowledge of specific diagnoses, treatment and self-treatment for people with long-term health challenges (15, 24–27, 29, 31, 32, 35). The main reason given in the studies for claiming that professional knowledge plays an important role is that patients, service users and next of kin should be able to acquire basic knowledge about their own illness. One nurse describes it as follows: ‘Of course the patients need medical knowledge. Knowledge they can hopefully use as a driver in the process of getting a healthier lifestyle’ (24). At the same time, several health professionals in the studies report challenges adapting the language they use and the professional knowledge level they communicate to a variety of patient groups with different backgrounds and needs.
Knowledge about communication
Eight studies mentioned knowledge and skills in communication as an important area of competence (15, 23, 26, 30, 32, 33, 35, 36). The studies describe general communication skills that are often employed in interaction between health workers and patients, such as active listening and speaking in an understandable manner. In addition, they describe skills that are more closely linked to initiating, directing and concluding group discussions among patients or service users. Examples of this can be how to communicate verbally to create a secure atmosphere and safe surroundings, how to enable people to reflect on and discuss habits and thought patterns, and how to handle negative group dynamics. In this respect, there is a close association between knowledge and skills in communication and group management.
Knowledge of coping resources
Eight studies refer to knowledge of coping and coping processes as of key importance in ensuring that patients and service users benefit from participating in self-management programmes (15, 23, 25, 30, 31, 35, 36). The studies discuss the benefits arising from health professionals’ and course leaders’ dissemination of practical knowledge about coping, coping strategies, and how to solve every-day practical challenges. In addition, they point to the importance of course leaders being able to apply methods and techniques that initiate and support changes in mind-set and behaviour patterns among patients and service users. Examples are building and acknowledging group participants’ own coping resources, or creating reflection and discussion among the participants. One cancer patient commented on how important this was: ‘I don’t think the outcome would have been the same if we had just sat and talked with each other [without nurses] … That would have been more of a self-pitying group’ (31).
Educational competence
Six of the studies point out that educational competence and skills are a basic area of competence for health professionals who offer self-management programmes (15, 24, 26, 35–37). The studies emphasise two main dimensions of such knowledge and skills. Firstly, we need knowledge about learning as a phenomenon and about how to apply theoretical knowledge in self-management programmes. We also need to know how to adapt and adjust teaching or learning activities to the knowledge and teaching needs of the participants. Moreover, several stress that it is necessary to have basic practical knowledge and skills in planning, organising, implementing and evaluating courses and programmes for patients and service users.
Personal qualities and attitudes
Patients, health professionals and researchers indicate that the personal qualities, attitudes and values of health personnel are important for how patients and service users perceive participation in self-management programmes, whether in a positive or negative light. This is discussed by two studies (26, 35). The patients in these studies describe such qualities as prerequisites for the way health personnel act and meet them. Patients and users stress health personnel’s ability to show care, empathy, interest, and respect and to exhibit non-judgmental attitudes towards people with long-term health challenges. These qualities are described as important for several reasons. They have a positive influence on the relations established between the health worker and the patient, patients’ motivation to take part in such programmes and their feeling of receiving support and understanding in terms of their health-related challenges.
Discussion
Educational institutions, health professionals, service user representatives and patients have long emphasised that competence and the personal qualities of health professionals who provide self-management programmes are of prime importance for the quality of such programmes (39). Nevertheless, it has been unclear what competence is most relevant in facilitating the best possible outcome from participation in such a programme.
Based on systematic searches of the literature, in this review we have described the literature available in respect of the competence deemed most important for health professionals who provide self-management programmes to patients and service users with long-term health challenges. In the literature, the health professionals, the patients and service users all stress that certain features are decisive for a positive outcome from training and self-management programmes. The quality deemed most essential in health professionals is the ability to manage and contribute to good group processes. Moreover, it is vital to have professional and updated medical knowledge about diagnoses and treatment, communication skills, coping skills and educational skills. Personal qualities and attitudes are also important (see fact box).
The results naturally reflect nursing, medical and psychological literature on patient–therapist communication but also reveal knowledge that is easy to overlook. A good example is research in psychotherapy and therapeutic methods. Several decades of research have shown that differences between the personal qualities of therapists are more important for the outcome in terms of the mental health of clients or patients than differences between the methods therapists use (12–14). Research with and without an experimental design supports this. This problem was long disregarded by a professional field dominated by impact studies, and which largely concealed underlying variables (14).
The quality deemed most essential in health professionals is the ability to manage and contribute to good group processes.
However, there is a lack of studies on the significance of health professionals’ personal qualities for the outcome of participation in self-management programmes (user impacts). Moreover, studies that indirectly thematise the practitioner impact factor by examining health professionals’ key competencies have not attracted much attention (9). In this systematic review, we found 16 studies that satisfied the inclusion criteria and described different areas of competence. Some of these did not focus on competence as a research question but instead raised the topic when discussing the results. The review further shows that most are qualitative studies. One limitation of these is that the findings cannot be generalised to other populations. The authors of the articles also discuss this.
Moreover, most of the studies we have described were based on qualitative interviews. Such data are little suited to elucidating how knowledge, skills and attitudes are specifically put into practice by those providing self-management programmes. Nor do the data give any information about how various types of competence are combined and integrated in the individual programmes, and what impact competence has on the different outcome goals (26). There is a need for more ethnographic studies and impact studies with an experimental design to shed light on these questions. Moreover, most of the studies we assessed were of moderate quality. We assessed twelve of the 16 studies as being of moderate quality, three studies were of high quality, and one was of poor quality. The Knowledge Centre for the Health Service defines ‘moderate quality’ as meaning that there is little likelihood that the conclusion of the study is affected by deficiencies in the study, but that we must nevertheless be cautious about drawing clear conclusions.
Implications
The results of this study describe key competence areas for health professionals who provide self-management programmes. To our knowledge, no systematic search of such literature has previously been undertaken.
However, the literature review shows that more research on the topic is needed. We need more types of qualitative studies in order to increase understanding of how competence areas relate to each other and are linked in specific self-management programmes. In addition, quantitative studies are required in order to understand how the competence of health professionals affects different patient outcomes. We also need to undertake studies of important knowledge, skills and attitudes in service user representatives, who are often co-providers of self-management programmes. Such studies are necessary to enhance the relevance of the research in a Norwegian context. The competence of service user representatives will overlap that of health professionals in some areas, especially regarding the skills necessary for good cooperation with patients and service users (39).
The studies included also show that health professionals are uncertain about their own competence.
A better insight into the competence areas required in training and self-management programmes can provide key input to those responsible for courses in health education for professionals in the specialist health service and the municipal health and care services. This would also give vital input to the health professionals and service user representatives who offer self-management programmes for patients and service users (26).
The studies included also show that health professionals are uncertain about their own competence (15, 24). Several therefore underline the importance of improving health education programmes. The purpose of such programmes is to provide health professionals and service user representatives offering self-management programmes with knowledge of how to make provision for self-management in patients, service users and next of kin (39).
Methodological criticism
The self-management programmes on which the studies are based are offered by health professionals. Thus the studies do not necessarily describe competence linked to making provision for real service user involvement, or for cooperation with service user representatives in the planning, implementation and evaluation of measures or initiatives. In a Norwegian context, this cooperation model constitutes a key framework for self-management programmes (39).
In addition, the studies describe a fairly limited number of diagnosis groups. It is reasonable to assume that the competence required will vary among different initiatives and diagnosis groups (26). The studies are based on various types of self-management programmes for different diagnosis groups, and elucidate the question of competence from various angles. Nevertheless, to a considerable degree they highlight the same competence areas.
One of the advantages of a systematic literature study is that it applies a systematic, and accurately described procedure to identify and give an overview of relevant research. A weakness of the studies we have summarised is that most are qualitative studies with a limited number of patients and diagnoses. Furthermore, they vary in quality. Nor do all the studies examine competence as their primary research objective. An important goal in this systematic review has, however, been to gain an overview of what kind of studies do exist within this area of scant research.
The review also shows that a number of joint competence areas are highlighted across study design, diagnosis groups and interventions, indicating that the areas described may constitute the basic components of health education competence. A weakness of the literature review is that only one person – the first author – reviewed and excluded potentially relevant articles in full text in addition to extracting information from the 17 studies that were included at the start. Since the selection process and the procurement of data were not conducted by at least two persons independently of each other, the likelihood of bias increases. This may therefore have impacted on the interpretation of the results.
Conclusion
Our literature review indicates that health personnel need knowledge and skills in group management, diagnoses, coping skills and education as well as appropriate personal qualities and attitudes in order to provide good group-based self-management programmes. There are relatively few studies of the competence held by health professionals who provide training and self-management programmes, and there has been a lack of systematic literature reviews. Our study should therefore make this knowledge more accessible.
Nonetheless, the results should be applied with caution. Most of the studies discussed are of moderate quality, which indicates that it is not very likely that the conclusions of the studies have been affected by their deficiencies. However, we must be cautious about drawing clear conclusions. We need a greater number of high-quality studies of the topic with a larger sample and with an experimental design. We also need to boost the quality of health education training measures and the education of students, health professionals and service user representatives.
References
1. Folkehelserapporten 2014. Helsetilstanden i Norge. Nasjonalt folkehelseinstitutt.
2. Meld. St. 26 (2014-–2015). Fremtidens primærhelsetjeneste – nærhet og helhet.
3. Fønhus M, Stenberg U, Hafstad E. Mestringstiltak med brukermedvirkning for personer som har langvarige helseutfordringer. Oslo: Nasjonalt kunnskapssenter for helsetjenesten. 2015.
4. Zwerink M, Brusse-Keizer M, van der Valk PD, Zielhuis GA, Monninkhof EM, van der Palen J et al. Self management for patients with chronic obstructive pulmonary disease. The Cochrane database of systematic reviews. 2014;3:Cd002990.
5. Ahn S, Basu R, Smith M, Jiang L, Lorig K, Whitelaw N et al. The impact of chronic disease self-management programs: healthcare savings through a community-based intervention. BMC Public Health 2013;13(1).
6. Fønhus M, Dahm K. Cochrane: mestringstiltak for personer med kols. Sykepleien Forskning 2015;10(2):110–1. Available at: https://sykepleien.no/forskning/2015/07/mestringstiltak-personer-med-kols. (Downloaded18.11.2016).
7. Fønhus M. Mestringskurs – hva har form og innhold og si for utbyttet? Oslo: NK LMH. 2013.
8. Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Education and Counseling. 2002;48(2):177–87.
9. Anderson RM, Funnell MM. The art and science of diabetes education: a culture out of balance. Diabetes Educ. 2008;34(1):109–17.
10. Koster T, Granum V. Lærer å formidle kunnskap. Sykepleien 2009;10:64–7. Available at: https://sykepleien.no/forskning/2009/06/laerer-formidle-kunnskap. (Downloaded18.11.2016).
11. Hvinden K. Etablering av lærings- og mestringssentra – Historie, grunnlagstenkning, innhold og organisering. In: Lerdal A, Fagermoen M (ed.). Læring og mestring – et helsefremmende perspektiv i praksis og forskning. Oslo: Gyldendal Akademisk. 2012. p. 48–62.
12. Silverman J, Kurtz, S., Draper, J. Skills for communicating with patients. Oxford: Radcliffe Publishing. 2005.
13. Bramhall E. Effective communication skills in nursing practice. Nursing standard (Royal College of Nursing (Great Britain): 1987). 2014;29(14):53–9.
14. Rønnestad M. Evidensbasert praksis i psykologi. Tidsskrift for Norsk Psykologforening 2008;45(4):444–54.
15. Butow P, Ussher J, Kirsten L, Hobbs K, Smith K, Wain G et al. Sustaining leaders of cancer support groups. Social Work in Health Care 2006;42(2):39–55.
16. Håndbok for Nasjonalt kunnskapssenter for helsetjenesten. Slik oppsummerer vi forskning. 2015. Available at: http://www.kunnskapssenteret.no/verktoy/slik-oppsummerer-vi-forskning(Downloaded 01.02.2016).
17. Hatlevik I. Meningsfulle sammenhenger. En studie av sammenhenger mellom læring på ulike arenaer og utvikling av ulike aspekter ved profesjonell kompetanse hos studenter i sykepleier-, lærer- og sosialarbeider- utdanningene. Oslo: Høgskolen i Oslo og Akershus. 2014.
18. Skau G. Gode fagfolk vokser. Personlig kompetanse i arbeid med mennesker. 4. ed. Oslo: Cappelen Damm Akademisk. 2011.
19. Henriksen J, Vetlesen A. Nærhet og distanse. Grunnlag, verdier og etiske teorier i arbeid med mennesker. Oslo: Gyldendal. 2000.
20. Grabowski D, Brun Jensen B, Willaing I, Zoffmann V, Schiøtz M. Sundhedspædagogik i patientutddannelse. En litteraturbaseret gennemgang af udvalgte sundhedspædagogiske begrebers anvendelse i patientuddannelse. Steno Center for sundhedsfremme. 2010.
21. Wilkinson S. Focus group research. In: Silverman D (ed.). Qualitative research Theory, Method and Practice. 2. ed. London: Sage. 2006. p. 177–99.
22. Jormfeldt H, Brunt DA, Rask M, Bengtsson A, Svedberg P. Staff’s experiences of a person-centered health education group intervention for people with a persistent mental illness. Issues in Mental Health Nursing. 2013;34(7):488–96.
23. Dures E, Hewlett S, Ambler N, Jenkins R, Clarke J, Gooberman-Hil R. Rheumatology clinicians' experiences of brief training and implementation of skills to support patient self-management. BMC Musculoskeletal Disorders. 2014;15(108).
24. Andersen TH, Hempler NF, Willaing I. Educator challenges using participatory methods in group-based patient education. Health Education 2014;114(2):152–65.
25. Dysvik E, Stephens P. Conducting rehabilitation groups for people suffering from chronic pain. International Journal of Nursing Practice. 2010;16(3):233–40.
26. Svavarsdottir MH, Sigurethardottir AK, Steinsbekk A. Knowledge and skills needed for patient education for individuals with coronary heart disease: The perspective of health professionals. European Journal of Cardiovascular Nursing : Journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology 2014.
27. Costello JF. Roles and strategies of diabetes support group facilitators: An exploratory study. The Diabetes Educator 2013;39(2):178–86.
28. Furnes B, Natvig G, Dysvik E. Therapeutic elements in a self-management approach: experiences from group participation among people suffering from chronic pain. Patient Preference and Adherence 2014;8:1085–92.
29. de Sousa Pinto JM, Martin-Nogueras AM, Morano MT, Macedo TE, Arenillas JI, Troosters T. Chronic obstructive pulmonary disease patients’ experience with pulmonary rehabilitation: a systematic review of qualitative research. Chronic Respiratory Disease. 2013;10(3):141–57.
30. Scala D, D’Avino M, Cozzolino S, Mancini A, Andria B, Caruso G et al. Promotion of behavioural change in people with hypertension: an intervention study. Pharm World Sci. 2008;30(6):834–9.
31. Sekse RJT, Blaaka G, Buestad I, Tengesdal E, Paulsen A, Vika M. Education and counselling group intervention for women treated for gynaecological cancer: does it help? Scandinavian Journal of Caring Sciences. 2014;28(1):112–21.
32. Hakanson C, Sahlberg-Blom E, Ternestedt BM, Nyhlin H. Learning to live with irritabel bowel syndrome. The influence of a group-based patient education programme on peoples' ability to manage illness in everyday life. Scandinavian Journal of Caring Sciences 2011;25(3):491–8.
33. Wilson JS, O’Neill B, Reilly J, MacMahon J, Bradley JM. Education in pulmonary rehabilitation: The Patient’s Perspective. Archives of Physical Medicine and Rehabilitation 2007;88(12):1704–9.
34. Adolfsson ET, Starrin B, Smide B, Wikblad K. Type 2 diabetic patients’ experiences of two different educational approaches – A qualitative study. International Journal of Nursing Studies 2008;45(7):986–94.
35. Gagliardino JJ, Malbrán MdC, Clark C. Development and implementation of advanced training course for diabetes educators in Argentina. Diabetes Spectrum 2007;20(1):24–30.
36. Jones JM, Papadakos J, Bennett C, Blacker S, Catton P, Harth T et al. Maximizing your Patient Education Skills (MPES): A multi-site evaluation of an innovative patient education skills training course for oncology health care professionals. Patient Education and Counseling 2011;84(2):176–84.
37. Rodgers J. Guidance on delivering effective group education. British Journal of Community Nursing 2006;11(11):476–82.
38. Lawn S, Schoo A. Supporting self-management of chronic health conditions: Common approaches. Patient Education and Counseling 2010;80(2):205–11.
39. Hvinden K. Etablering av lærings- og mestringssentra – Historie, grunnlagstenkning, innhold og organisering. In: Lerdal A, Fagermoen M (ed.). Læring og mestring – et helsefremmende perspektiv i praksis og forskning. Oslo: Gyldendal Akademisk. 2012. p. 48–62.










Comments