Experiences with being diagnosed with and treated for testicular cancer
It is an ordeal to be diagnosed with and treated for testicular cancer. Various resources can help patients to handle the difficult situation more easily.
Background: Men experience receiving the diagnosis of testicular cancer and its treatment as challenging.
Purpose: To explore how individuals experienced and managed the challenges related to being diagnosed with and treated for testicular cancer.
Method: The study comprises five individual qualitative interviews with former patients with testicular cancer.
Result: The men found the time up until diagnosis and during their medical assessment to be difficult. Receiving the diagnosis came as a shock, although they had suspected testicular cancer. They experienced the surgery as uncomplicated, while the chemotherapy was a strain, physically and psychologically. As a resource for coping with the disease the spouse or partner provided the most important support, but also employer, colleagues and health personnel were of great help. Receiving updated information, being physically active, having hope and being open about the disease were central in coping with the difficult times.
Conclusion: The men found receiving the diagnosis of testicular cancer and undergoing chemotherapy quite demanding. Support, physical activity and hope helped improve coping, health and wellbeing, and are therefore important. Health personnel can help improve testicular cancer patients’ ability to cope. They can give early and updated information, act supportively, help give hope and motivate the patients to openness and physical activity.
Testicular cancer is the most common form of cancer among young men aged 15 to 40 years (1, 2). The prevalence of this type of cancer has doubled over the past 50 years (3). Norway has one of the highest prevalences of the disease. Around 300 new cases occur each year (2).
There are two different types of testicular cancer: seminomatous, arising at median age 35 years, and non-seminomatous, arising before 30 years of age and metastasising more frequently. The development of the disease is divided into four stages: In stage I a limited tumour has been located in the patient’s testicle. In stage II the patient has lymph node metastases in the abdomen, while in stage III lymph node metastases occur outside the abdomen. In stage IV there are distant metastases to the lungs and/or the brain. The most common symptom is a lump in the testicle with tenderness and pain (2).
Diagnosis and treatment are a great strain
The patients go through a standardised treatment programme in accordance with THE SWENOTECA- collaboration (Swedish Norwegian Testicular Cancer Group), where the treatment programme is determined based on the type of cancer and the stage of the disease. The first choice of treatment is surgery, removing the testicle and the tumour. The tumour is examined histologically before the patient is referred to further follow-up and treatment.
In stage I the treatment is only surgical but the patient is followed up on a regular basis for up to ten years. Patients in stages II – IV also undergo chemotherapy. In stage IV the distant metastases are surgically removed where this is possible. Total survival is 97 percent, but this depends on when the patient receives the diagnosis. For patients in stage IV survival is 41 percent (2).
Earlier studies show that receiving the diagnosis and undergoing treatment for testicular cancer are a great strain (4, 5, 6, 7, 8). The patients are frequently young, and the diagnosis comes as a shock to many (4, 5, 6). Treatment with chemotherapy can be an ordeal, as it may have tough side effects such as hair loss, nausea, weakened immune system, fatigue and infertility (5, 6, 8, 9). Studies also show that living with the fear of recurrence after treatment is completed can be difficult (4, 5).
Important to learn coping strategies
In order to experience the best possible health and wellbeing in such a difficult situation, coping strategies are important (4, 5, 7, 19). According to Antonovsky, health is not absence of disease, but we move along a continuum of degrees of health. To cope is to handle challenges that are experienced as a threat to health, or that do not have any immediate solution. The concept ”sense of coherence (SOC)” is central to strengthening coping and health. SOC consists of three components:
- comprehensibility
- manageability
- meaningfulness
Coping resources are important to strengthen SOC and may consist of internal as well as external resources. Examples of internal resources are ego identity, values and knowledge. External resources may be social support and material values (11).
Support, physical activity and hope help improve coping, health and wellbeing.
With regard to coping resources during diagnosis and treatment of testicular cancer, an earlier study has found that social support from close ones was important, but that health personnel were also central in giving support (4). A more recent study shows that in addition to support from partner and health personnel, religious faith and knowledge may be of help (5). We have found few studies that address patients’ experiences in connection with diagnosis and treatment of testicular cancer. We also have found few studies on what sustains the ability to cope. There is thus a need for more knowledge. The purpose of this study is thus as follows:
- explore the patients’ experiences with being diagnosed with and treated for testicular cancer
- explore which coping resources are important in strengthening the patients’ ability to cope
Method and sample
The study has a qualitative design with individual interviews.
The unit leader at a local hospital distributed letters with requests for participation to 22 men who had undergone testicular cancer surgery during the past four years, and who had completed treatment. Of these, five wished to participate in the study.
The informants were 32-51 years of age when the interview took place. The level of education varied from primary school to college, four were in a relationship, three had children, and they had all returned to work.
The informants had had surgical treatment at the local hospital and had received further follow-up and/or treatment at a regional hospital. One informant was followed up with regular check-ups, two had had one chemotherapy cycle, one had had three chemotherapy cycles, while one had had five chemotherapy cycles.
Data collection
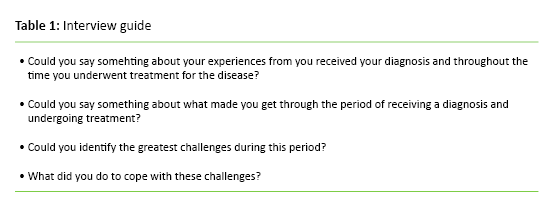
First author carried out the interviews in December 2013 and January 2014. In order to get answers to our questions we used a semi-structured interview guide (Table 1). We had received permission to use an audio recorder during the interviews. The interviews took place in the homes of the informants or in the office of the first author. Each interview lasted 45–60 minutes.
During the interviews it was important to let the informants talk freely about their experiences (12). They had to be able to express their sentiments in their own words and in their own way (13). The informants said that to them it felt right to share their story and they talked openly and trustingly about the time of assessment and treatment. The interviewer presented follow-up questions to gain depth and understanding of the challenges the informants had been through. She also asked the informants what they felt had helped them cope with the challenges they had encountered.
Ethical considerations
The study was carried out in accordance with the Declaration of Helsinki. The informants received written information on the study and signed a written consent statement. Prior to the interview the informants received oral information on the purpose of the study. They also received information that participation was voluntary, and that they were free to withdraw at any time (14). The study was also approved by the hospital administration and Norwegian Center for Research Data (project no 34726).
Analysis
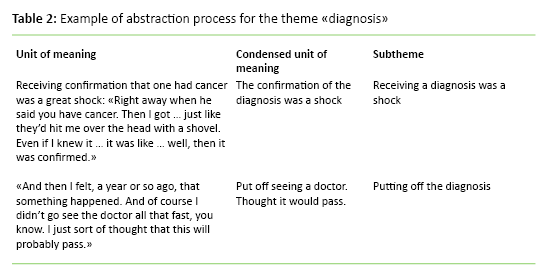
We analysed the printout from the interviews by using systematic text condensation (15). The analysis followed four steps:
- a thorough reading of the printouts from the transcribed interviews to gain an impression of the totality
- identification and coding of units of meaning
- comparison in all interviews of the units of meaning from step two
- condensation and abstraction of the coded units from each category
Findings
The informants yielded good knowledge on the challenges involved in being a patient with testicular cancer and going through receiving a diagnosis and undergoing treatment. Even if testicular cancer is a diagnosis from which the majority recover, it was a great strain to receive the diagnosis and go through the treatment. Below we present the most important themes that emerged in the analysis:
- the diagnosis
- the time from confirmation of diagnosis until information and treatment
- chemotherapy was an ordeal, physically and psychologically
- coping resources that sustained coping
The diagnosis
The theme “diagnosis” comprised two subthemes: “not taking symptoms seriously” and “confirmation of the diagnosis”. The theme “the time from confirmation of diagnosis to information and treatment” had one subtheme: “information”. The theme “coping resources that sustained coping” contained three subthemes: “social support”, “physical activity” and “hope”.
Not taking symptoms seriously
One informant put off seeing a doctor for a long time despite suspecting testicular cancer: “And then I felt, well, a year or so ago, that something happened. And of course I didn’t go see the doctor all that fast, you know. I just sort of thought that this will probably pass.”
Another informant did not at first think that the symptoms were signs of anything serious, while others found that their doctor did not take the symptoms seriously: “And then when I got to the doctor he said he didn’t think it was anything to worry about.” This resulted in it taking a bit longer before the diagnosis could be confirmed.
Confirmation of the diagnosis
Having a cancer diagnosis confirmed was a great shock: “Right away when he said you have cancer. Then I got … just like they had hit me with a shovel. Even if I knew it … it was like … well, then I it was confirmed.”
The time from confirmation of the diagnosis till information and treatment – information
The time between confirmation of diagnosis till information on treatment was the most challenging.
But when the informants received adequate information from a doctor they had come to trust, anxiety was replaced by calm and a belief that all would be well: “And then I was given the prognosis, and I calmed down quite a bit … if you are going to have cancer it is pretty nice to have a kind they have control of.”
It also emerged that medical information, given in a proper manner, should not be underrated: “It was pretty good to get information about … You do wonder how the rest of your body will work after something like that. When you have lost a testicle I mean. How your sex life will work and all that, afterwards, but all that has been just normal.” “They said it was more or less a 50-50 … could become sterile too, and don’t really know that yet. So you froze … had an offer of that. So I did that before starting on the chemo.”
The information is related to knowledge and safety and is important for trust in the health services. Informants who experienced a shortage of information or who had to keep asking for such information related that to the hospital not having enough knowledge on diagnosis and treatment.
Chemotherapy was an ordeal – physically and psychologically
All informants found the surgery uncomplicated and simple. Undergoing chemotherapy on the other hand was a great strain both physically and psychologically. The informants had felt fairly healthy until the chemotherapy, but the moment they were given chemotherapy, they had issues that made them feel really ill. Nausea and vomiting and a feeling of physical and mental fatigue were challenging: “Was totally in the basement after these treatments.” Those who had the most cycles emphasised this strain the most, but also those who had only one cycle of chemotherapy experienced it as a physical and psychological ordeal. The informant who did not undergo chemotherapy, found the thought of doing so very frightening.
Coping resources that contributed to coping – social support
It emerged in the analysis that a spouse or partner was the most important support during the period of illness, and this was seen as a determining factor for getting through the challenges in an adequate way. Also own parents, adult children and understanding from employer and colleagues were emphasised. The informants described it as an advantage to not have to work and to be on sick leave with a good conscience. Also feeling safe and cared for in the health services was central to coping with the challenges throughout the cancer treatment: “A pure success story I think. Impressed by the control the regional hospital had.”
All informants had been open about their disease and had had positive experiences with being so. They emphasised that in being open it was easier to get support. Openness would also hinder speculation and get the patient help to work through his own thoughts and feelings: “It is better to be able to talk about it than have people just sit and wonder, and then make up their own thoughts and opinions. Being open has been a help. The more people who know what you suffer from, the greater is the chance of getting the help you need.”
Coping resources that contributed to coping – physical activity
Several informants emphasised that physical activity was important for coping. Doing something physical signalled that the body functioned, and one could think of other things. Through physical activity they saw progress, and they felt that they did something to move forward: “The best way to get on was when I started to exercise. That felt good, I felt things were working.”
Coping resources that contributed to coping – hope
The informants further emphasised the importance of being positive and have hope that all would be well. The informants gave the doctor and nurses at the regional hospital much of the credit for this hope: “I guess I hoped I would be among those percentages, I don’t remember, it was some 95 percent or whatever she said. Then I thought, oh well, I do think this is going to go well … and then I did relax a bit more.” “When I heard the possibilities or prognoses then I thought that this, this is probably going to turn out really well.” Believing that it would be all right made it easier to grit your teeth and go through the treatment. In addition professionalism, care and cheerfulness from the health personnel were emphasised as important.
Discussion
This study shows that the men find it demanding to be a patient, receive the testicular cancer diagnosis and go through the treatment. Various coping resources such as social support, physical activity and hope may help patients cope with the difficult life situation.
The findings show that some do not see a doctor despite suspecting that they may have cancer. Some put off seeing a doctor because they do not think the symptoms signal anything serious. Earlier studies show that putting off seeing a doctor in the case of cancer may be due to uncertainty regarding whether the symptoms are serious enough. Some also deny the fact that the symptoms may signal a serious disease (4, 6, 7, 16).
To many the diagnosis comes as a shock.
The informants emphasised how difficult the time was before they received proper information on the diagnosis. The difficulty of going through a time of medical assessment has also emerged in other studies (4, 10, 16). This points to the importance of attending to the patients when they have received the diagnosis. A study on patients with breast cancer shows that early information on a specific treatment plan gives them a feeling of control. They also feel they belong to a trustworthy health service (10). It is important that patients experience predictability and knowledge so that they may more easily manage the challenges the disease brings (5, 10, 11) and feel that the treatment is meaningful, something necessary for full recovery (5, 10, 11). The informants also pointed out that having hope is important for coping during the difficult time that accompanies confirmation of diagnosis and treatment. Hope may give a feeling that there is a way out or the difficulties and that challenges can be managed (10, 17).
The doctor's communication is significant
Several informants emphasised the first doctor who gave them faith that the treatments would succeed. The informants had a clear memory of this conversation, both regarding the words used by the doctor and the emotions they induced. Studies show that the personal interest a doctor shows when communicating a diagnosis is a factor that determines whether the patient will trust or mistrust the doctor (4, 8, 18). Earlier studies also point out how significant trust is, as the disease strengthens the need to trust others (4, 5, 19, 20, 21, 22).
A central finding is that some informants found the information they received in the local hospital to be out-dated. Such incidents weaken the trust in the health services. When the informants felt their lives were under threat when they developed cancer, it became even harder when they experienced that some health professionals did not merit their trust. Earlier studies also show that some health personnel may greatly influence how the patients cope with challenges when ill (4, 8, 10, 23). Health personnel must be aware of this when encountering patients with testicular cancer.
Support from close ones is important for coping
The informants felt that support from family, friends, colleagues and health services was the most important reason for their ability to cope with the illness. This is also in line with earlier studies of patients with testicular cancer (4, 5, 6, 7, 24). The positive effect of social support on health is relatively well documented (25) and that help and support from health personnel is invaluable (10, 19). Having at least one confidant enables resistance and strength and helps give meaning to life (26). This is important for the ability to cope and for the improvement of health and wellbeing (11).
In addition to support from family and health personnel there is much one can do to regain health, according to the informants. Health is not what we are subjected to in life, but our ability to use our coping resources in such a way that one copes with the challenges (11). Focusing on the patients’ coping resources, such as social support, knowledge and hope, thus becomes important. The patient thus gets help to keep his or her place along the continuum between health and non-health, or to move towards better health. By supporting the patient and advising him to use his coping resources, he can more easily manage the situation.
Physical activity yields many benefits
The informants emphasised that how the body functioned was important for their mental health. By using the body physically they had a feeling of being in recovery and on the way back to a better health and existence. The days they felt physically low, they also became psychologically broken down. This is in line with an earlier study that shows that physical activity and being preoccupied with other things may be of help in coping with daily life (4). An earlier review article on cancer patients also suggests that physical activity during treatment may lead to a higher survival rate and an improved quality of life (27).
An interesting finding is that the informants pointed out that openness was an important help for support and coping. This finding is not in line with earlier studies that show that a male approach is to be independent and manage problems alone (6, 7). They also show that it is difficult to talk about one’s own illness (5, 6), and that silence keeps any difficult emotions at bay (28). Our findings are thus an important contribution to research, as they show that openness may lead to more support from others. Such support may also contribute to increased understanding and manageability. According to Antonovsky, comprehensibility and manageability are important in strengthening SOC, which again will improve coping, health and wellbeing (11).
The study's strength
Interviewer had long clinical experience with cancer patients, both from hospital and municipal health services. This experience provides a solid basis for understanding the challenges the informants have had in connection with cancer diagnosis and treatment. Interviewer can ask informed follow-up questions, and the men feel safe when speaking openly of their experiences in the difficult situation (12).
The study's weakness
The study has a small number of informants, and all participants emphasised being open about their illness. It is possible that some of those who did not participate would not have been equally open. Interviewer’s preunderstanding may result in preconceived notions, which may influence the questions asked in the interview and the result of the analysis (14). Interviewer was aware of these issues and attempted to make sure that her own knowledge, experiences and events should not influence the result.
Conclusion
Receiving the testicular cancer diagnosis and chemotherapy was a physical and psychological ordeal for the informants. The stages from suspecting testicular cancer to seeing a doctor, receiving the diagnosis and the treatment were marked by challenges that put life at risk and tested the ability to cope with the challenges. The analysis shows that support, physical activity and hope contribute to improved coping, health and wellbeing. It is also important to be open about the disease so that the network may give support. Early and up to date information was also important, as having one’s life threatened feels even harder when the trust in health personnel is weakened.
References
1. Frøen H, Brennhovd B, Abeler VM, Lehne G. Ung mann med sterke ryggsmerter. Tidsskrift for Den norske legeforening 2012;132:1626–9.
2. Helsedirektoratet (2015). Nasjonalt handlingsprogram med retningslinjer for diagnostikk, behandling og oppfølging for testikkelkreft. Available at: https://helsedirektoratet.no/retningslinjer/nasjonalt-handlingsprogram-med-retningslinjer-for-diagnostikk-behandling-og-oppfolging-av-testikkelkreft(Downloaded 26.10.2015.)
3. Berg A, Fosså SD. Kreft i mannlige kjønnsorgan. In: Reitan AM, Schjølberg TK (ed). Kreftsykepleie. Pasient-utfordring-handling. Akribe forlag, Oslo. 2010.
4. Kristjanson LJ, Ng C, Oldham L, Wilkes L, White K, Maher L. The impact and responses of men who have experienced testicular cancer. Australian Journal of Cancer Nursing, 2006;7(1):10–7.
5. Saab M, Noureddine S, Abu-Saad H, DeJoung J. Surviving testicular cancer: The Lebanese lived experience. Nursing Research 2014; 63(3):203–10.
6. Brodsky MS. The young male experience with treatment for nonseminomatous testicular cancer. Sexuality and Disability 1999;17(1):65–77.
7. Mason OJ, Strauss K. Testicular cancer: Passage through the help-seeking process for a cohort of U.K. men (part 1). International Journal of Men’s Health 2004; 3(2):93–110.
8. Johansson S, Steineck G, Hursti T, Fredrikson M, Furst CJ, Peterson C. Aspects of patient care: interviews with relapse-free testicular cancer patients in Stockholm. Cancer Nursing 1992; 15(1):54–60.
9. Dahl O, Lehne G. Cancer testis. In: Dahl O, Lehne G, Baksaas I, Kvaløy S, Christoffersen T (ed.). Medikamentell kreftbehandling. Cytostatikaboken. Haukeland universitetssykehus, Bergen. 1995.
10. Drageset S, Lindstrøm TC, Underlid K. Coping with breast cancer: between diagnosis and surgery. Journal of Advanced Nursing 2009;66(1):149–58.
11. Antonovsky A. Helsens mysterium. Gyldendal Norsk Forlag, Oslo. 2012.
12. Kvale S, Brinckmann S. Det kvalitative forskningsintervju. Gyldendal Akademisk, Oslo. 2012.
13. Jacobsen DI. Forståelse, beskrivelse og forklaring. Innføring i metode for helse- og sosialfagene. Høyskoleforlaget, Oslo. 2010.
14. Malterud K. Kvalitative metoder i medisinsk forskning. Universitetsforlaget, Oslo. 2011.
15. Malterud M. Systematic text condensation: A strategy for qualitative analysis. Scandinavian Journal of Public Health 2012;40:795–805.
16. Sandén I, Larsson US, Eriksson C. An interview study of men discovering testicular cancer. Cancer Nursing 2000;23(4):304–9.
17. Rustøen T. Håp og livskvalitet – en utfordring i sykepleien? Gyldendal Akademisk, Oslo. 2001.
18. Myskja A. Leve med kreft. Hvordan styrke håp og livsmot. Cappelens forlag, Oslo. 2005.
19. Giske T. Sårbarheit, makt og tillit: Tillit – den gode bru mellom sårbarheit og makt, eksemplifisert med pasientar innlagde på sjukehus til utgreiing. Michael 2010;7:254–61.
20. Fugelli P. Tillit. Tidsskrift for Den norske legeforening 2001;30(121):3621–4.
21. Giddens A. Modernitetens konsekvenser. Pax forlag, Oslo. 1997.
22. Grimen H. Tillit og makt – tre sammenhenger. Tidsskrift for Den norske Legeforening, 2010;30(121):3617–9.
23. Ekeland T-J. Kommunikasjon som helseressurs. In: Heggen K, Ekeland T-J. (ed). Meistring og myndiggjering – reform eller retorikk. Gyldendal Akademisk, Oslo. 2008.
24. Fleer J, Sleijfer D, Hoekstra H, Tuinman M, Klip E, Hoekstra-Weebers J. Objective and subjective predictors of cancer-related stress symptoms in testicular cancer survivors. Patient Education & Counceling 2006;64:142–50.
25. Dalgard OS, Ystgaard M, Brevik JI. Sosiale miljøfaktorer og psykisk helse. I: Dalgard OS, Døhlie E, Ystgaard M (red.). Sosialt nettverk – helse & samfunn. Universitetsforlaget, Oslo. 1995.
26. Reitan AM. Krise og mestring. In: Reitan AM, Schjølberg T.K. (ed.). Kreftsykepleie – pasient, utfordring, handling. Akribe forlag, Oslo. 2010.
27. Galvâo DA, Newton RU. Review of exercise intervention studies in cancer patients. Journal of Clinical Oncology 2005;23(4):899–909.
28. Lien MI. Syke menn skyr moderlig omsorg. Available at: http://www.sykepleien.no/nyhet/1197229/syke-menn-skyr-moderlig-omsorg(Downloaded 29.04.2013.)










Comments