Oxygen therapy for children in hospitals
The current practice of using oxygen therapy has proven to be incomplete.
Background: The lack of clinical guidelines for oxygen therapy leads to different treatments depending on the health personnel’s own experiences and competence.
Objective: The aim of this study was to examine 1) the current practice of using oxygen therapy 2) the written documentation of administering and monitoring oxygen therapy and 3) to consider the need for improvement.
Methods: We did a retrospective examination of patient records that included a written prescription for oxygen, administration and monitoring of oxygen therapy and documentation of treatment for patients. This was done in the period 01/01/14 to 05/31/14 and in the period 01/01/15 to 31/05/15. A quality improvement plan was introduced after the first examination.
Results: In the first period, 135 patient records were reviewed and 29.6 percent of those patients needed oxygen. In the second period, 202 records were reviewed and 31.2 percent of those patients had received oxygen therapy. After the first period, written prescriptions of oxygen increased from 25 percent to 46 percent, and the documentation increased from 15 percent to 46 percent between periods.
Conclusion: This project based on the health personnel’s own practice has contributed to the development of new and better procedures and the work to develop new clinical procedures for oxygen therapy has begun.
Keywords: Oxygen, infant, observation, documentation, quality improvement
Introduction
Bronchiolitis is the most common cause of hospitalisation in children under 12 months of age in many countries. A Norwegian study has shown a prevalence of 21.7 per 1000 with regard to hospitalisations of children under one year of age (1). Around 20 per cent of all children contract bronchiolitis during the first year of life. Bronchiolitis is caused mainly by Respiratory S Virus (RS virus), which appears seasonal during the winter months. The infection starts in the upper respiratory tract and may spread to the lower respiratory tract, causing pneumonia and atelectasis (2). The infection leads to breathing problems such as wheezing, coughing, congested nose, increased respiratory rate, sleep apnoea, use of supportive muscles, increased mucus production in the lesser airways, and reduced nutritional intake (1,3,4). The main treatment principles are sustained oxygen saturation and appropriate fluid and nutritional balance. Another therapeutic option is inhalation of adrenalin and saline water, but the effect is uncertain (1).
Oxygen therapy by Heated Humidified High Flow Nasal Cannula (HHHFNC) therapy and Continuous Positive Airways Pressure (CPAP) reduces the need for invasive ventilation (1,3,5). HHHFNC therapy is a well-tolerated treatment alternative that lowers the respiratory rate (6). HHHFNC can in some cases replace CPAP. It is user friendly and well tolerated by the patient (1). The patient receives heated and humidified air that reduces the injuries to the mucus membranes in the upper respiratory tract (7) and is thus a viable treatment option for patients with acute respiratory tract infection (8).
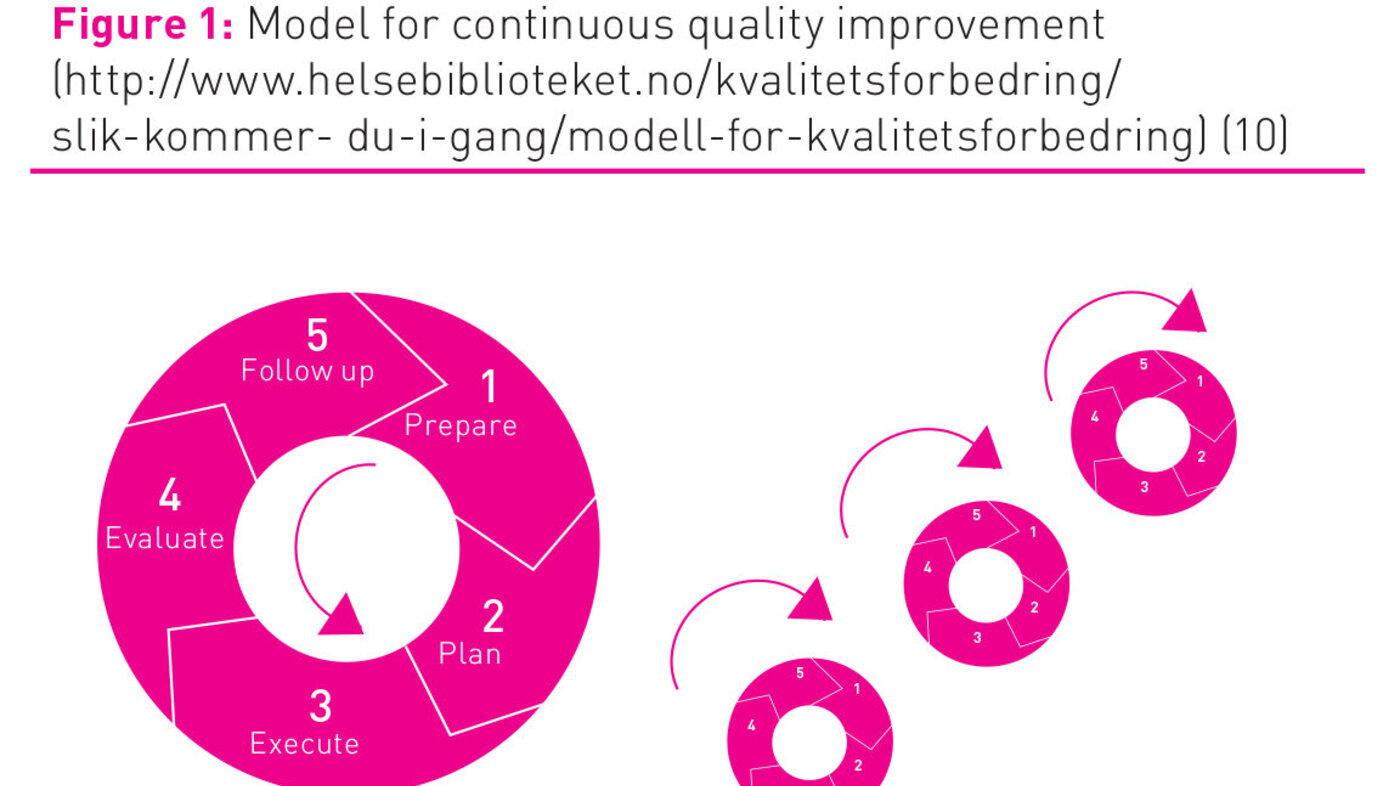
According to the National Strategy for Quality Improvement in Health and Social Services (2005-2015), practice should be systematically evaluated to assess the need for improvement (9). The department for quality development in The Norwegian National Knowledge Centre for the Health Services has developed a model for quality improvement (figure 1), illustrating that systematic quality work is a continuous process through which improvement of services may be achieved by systematically working through five phases (prepare, plan, execute, evaluate, follow up) (10). Improvement work may be time-consuming, necessitating testing, adjusting, and repeating measurements and reflecting on the results several times.
The lack of clear clinical guidelines for oxygen therapy leaves room for nurses and doctors to handle the treatment according to their own experience and competence. Although guidelines and administrative routines in and of themselves do not ensure quality in the treatment of patients, clear guidelines and recommendations will be of support when qualified assessments of individual patients are made. Practice has shown that there is great variation as to whether oxygen is prescribed and documented (11). Oxygen is a medication (11, 12) which reduces the respiratory effort (13) and should be prescribed in writing in accordance with desired oxygen concentration in the blood measured peripherally (SpO2-values), fraction of oxygen in inspiration air (FiO2), and administration method (12,14).
In this project we have worked in accordance with the Norwegian Knowledge Centre for the Health Services model for quality improvement (10). The model may be used in improvement work for both small and large projects. The complexity determines how long an improvement process takes. The purpose has been to examine current practice of using oxygen therapy, to examine the written documentation of administering and monitoring oxygen therapy, and to consider the need for quality improvement.
Method
During the period January 1 2014 to May 31 2014, a retrospective examination of patient records was done for hospitalised patients at the Infection, lung, and emergency care unit at the Children’s Clinic at Haukeland University Hospital. The patients’ diagnoses were bronchiolitis and pneumonia. We registered current practice for written prescription of oxygen, administration method, observations, and documentation of oxygen therapy and whether use of monitoring equipment was documented. Patients with serious chronic diseases were excluded from the review. After an assessment of whether current practice was in line with current recommendations on oxygen therapy for children in hospitals described in the literature, we have acknowledged a need for improvement and have developed improvement actions to accommodate for new practice. A new examination of corresponding data for hospitalised patients during the period January 1 2015 to May 31 2015 was subsequently done.
Planning
In the first data collection 135 patient records were reviewed. Of these, 40 (29.6 per cent) patients needed oxygen. In the second data collection 202 records were reviewed and 63 (31.2 per cent) patients had received oxygen therapy. We registered data on age, gender, diagnosis, and number of hospital bed days. We also registered whether oxygen therapy was prescribed in writing, whether administration method was prescribed and documented, and whether use of monitoring equipment was documented. Data were collected from the patient chart (main chart, medication chart, charts for prescriptions, and observation sheets), as well as nursing documentation in DIPS. Prior to starting the first data collection, a pilot study was done in which we read seven patient records. We wanted to test if the registration form layout was suitable for capturing the necessary and relevant data for the study.
In the Norwegian Knowledge Centre for the Health Services’s model for quality improvement (10) it is important that as many as possible, in the physician group and nursing group, are informed and involved in mapping and discussion on current practice. Involving all relevant parties will give all ownership to the project, resulting in a greater commitment. Prior to starting the project information on the project was communicated to the nursing group through intranet, personnel meetings, and daily ten minutes of professional information at the start of each shift (figure1)
Accommodating new practice
Summed up findings from the first data collection were presented at a professional seminar for nurses and physicians. The findings lead to discussions in the nursing and physician groups as current practice did not quite correspond with recommendations for oxygen therapy to children in hospitals as described in the literature. Through our findings we saw that we were not necessarily bad at what we did, but we wanted to get better by introducing new measures and routines. National Strategy for Quality Improvement in Health and Social Services (2005-2015) states that services shall be safe and secure (9). A plan was developed for quality improvement. The research nurse had an active role as supervisor responsible for the project’s progress and implementation of actions. The following actions were implemented:
- Training in setting up and reading manometer
- New observation sheets for patients treated with CPAP and HHHFNC
- Revised guide for filling in charts
- New instructions to the physician group describing oxygen as a medication to be prescribed in writing
- New procedures for HHHFNC treatment
The Helse Bergen Data Protection Officer has evaluated and approved the study. The regular hospital insurance is valid for the patients. A separate folder was made for each patient for the data collections. The paper forms were stored locked up on the ward, and the information was later transferred to an electronic database in accordance with the security routines of the Western Norway Regional Health Authority. We applied for disk space on the quality server for storing the data. All information was handled without name and national identification number or any other immediately recognizable information. A code linked the patient to the information through an identifier list. The reference number followed the patient and was used again in case of rehospitalisation. Only authorised personnel were included in the project, had access to the identifier list, and could retrace the patient.
The results are presented descriptively with frequency count and percentagewise distributions. For each time period we made frequency counts of the diagnosis distribution (bronchiolitis/pneumonia), gender distribution, age distribution, number of hospital bed days, number of patients with written prescription for oxygen, number of observations per shift, frequency of registration on chart, and frequency of use of separate observation sheets. We tested for significant differences between the two time periods with Pearson’s Chi-square test. In cases with expected cell-frequencies less than five, Fisher’s exact test was used. We used spreadsheets in Excel and Stata IC version 14 to analyse the data.
Results
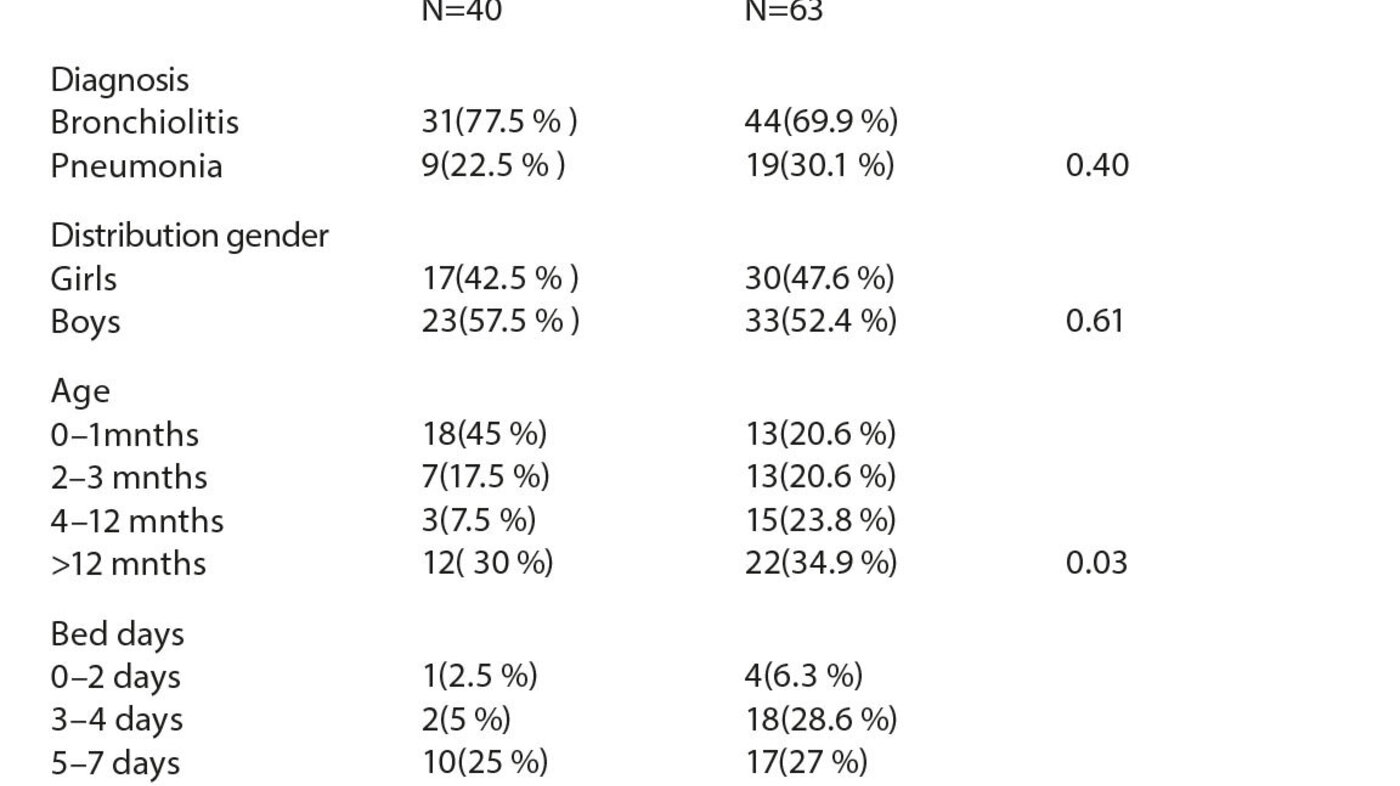
There was a significant difference in the age distribution between the two time periods (table 1). In the first data collection there were more children aged 0-1 month (45 per cent), whereas the second data collection had more children aged 2 – 12 months (54.4 per cent). There was a significant difference in the distribution of number of hospital bed days between the two time periods. The number of children with more than seven hospital bed days was significantly higher in the first mapping. There was a small overweight of boys at both registration points, but no significant difference in gender distribution between the two time periods. The first data collection showed a slightly higher percentage of patients diagnosed with bronchiolitis than the second data collection, but the difference in diagnosis distribution was not significant (table 1).
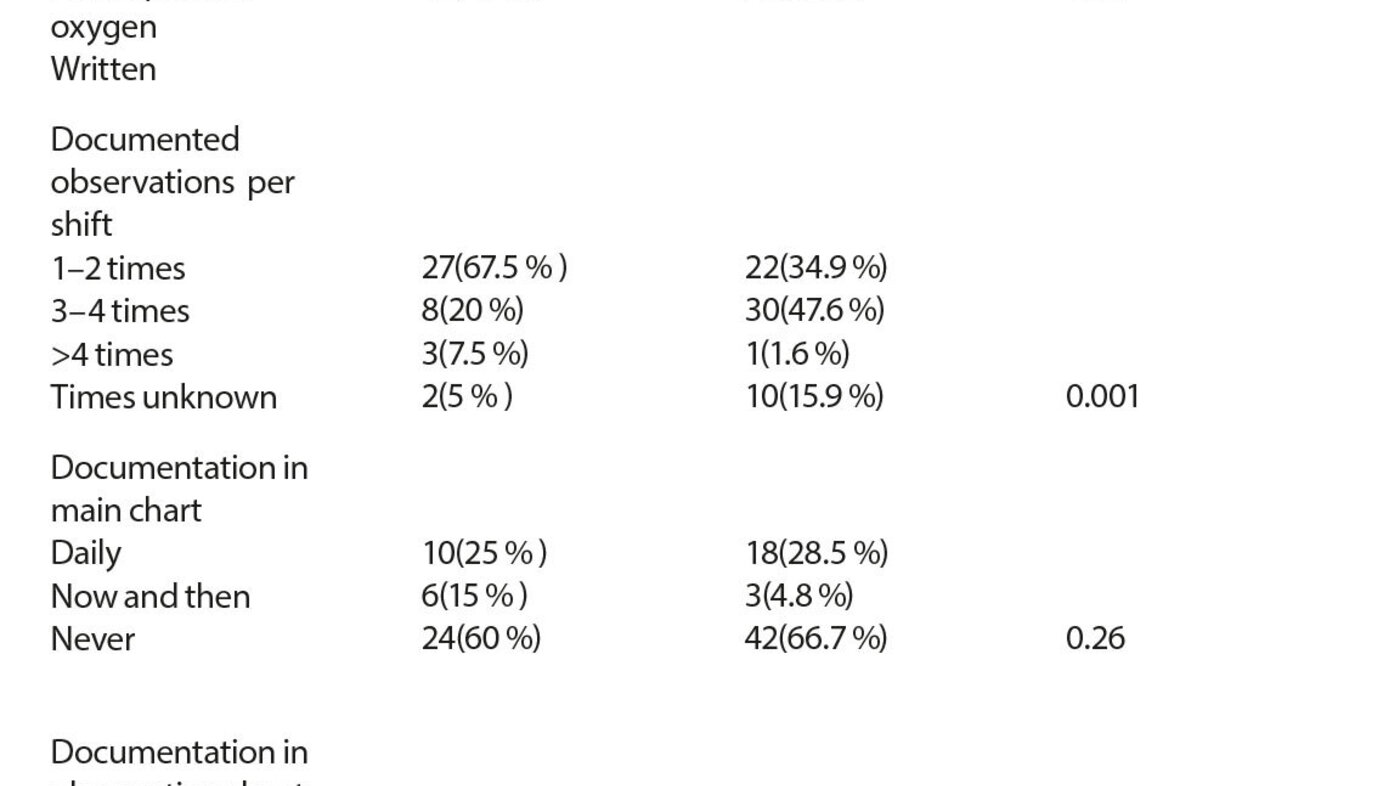
Observations were documented in main chart, observation sheets, or in written report. In the first data collection ten (25 per cent) journals had daily documentation of administration method for oxygen therapy in the chart, such as two litres by nose catheter. In 24 (60 per cent) journals documentation in the chart was missing. In some patient charts the SpO2 values were documented, but not that oxygen had been administered. In the second data collection there was a small improvement, 18 (28.5 per cent) patient records showed daily documentation in the charts (table 2).
In the first data collection the observations sheets showed daily documentation in six (15 per cent) records, whereas the observation sheet was never used in 24 (60 per cent) records. In the second data collection the observation sheet was used daily in 29 (46 per cent) records, while it was never used in 29 (46 per cent) records. There was a significant difference between the two time periods. In the case of HHHFNC treatment in particular the observation sheet was not used, while we saw more frequent use in the case of CPAP treatment (table 2). We found a significant change in the number of documented observations from the first to the second time period. In the first data collection the frequencies of documentation 1 – 2 times per shift and 3 – 4 times per shift were 27 (67.5 per cent) and eight (20 per cent) respectively. In the second data collection this had changed to 22 (34.9per cent) and 30 (47.6 per cent) respectively (table 2).
Discussion
During the two time periods in which we registered oxygen therapy to hospitalised children with bronchiolitis and pneumonia, 40 of 135 children and 63 of 202 children respectively, received oxygen. The bronchiolitis season varies from year to year. Studies show that the majority of patients with this diagnosis are hospitalised during the winter months. RS-bronchiolitis appears from October to May in the northern hemisphere (1). At the first data collection we had a peak of patients in March. The first part of the registration period was quiet with few patients. At the second data collection there were many patients in January and fewer during the rest of the registration period. A long and varied bronchiolitis season challenges the health services economy, hospital space, and the employee situation in paediatric wards (1).
In the first data collection 45 per cent of patients receiving oxygen were in the 0-1 month age group, while in the second registration the majority of children with a need for oxygen were in the 2-12 months group. Experience tells us that such variations arise from year to year. Children under six weeks and premature children are at high risk for becoming seriously ill with bronchiolitis (15). Our experience shows that many of these patients often need CPAP treatment, and will thus remain in hospital longer; we see this in the first data collection period as well.
Current practice
Nurses need to be able to initiate acute oxygen therapy. To achieve safe administration of oxygen, clear routines are needed for the prescription of administration method, flow, and desired saturation value (14). The findings from our project showed that oxygen to a greater extent is prescribed in writing at the second registration point (25 per cent and 46 per cent at first and second registration respectively).
There was only a small degree of change in written prescription of oxygen therapy by nasal catheter and steam, but the registration shows a trend where oxygen to a greater extent is prescribed in the case of HHHFNC and CPAP and for unstable patients. After the new procedure for HHHFNC treatment was ready, better routines were initiated for this treatment (16). In one study we see significant improvement in prescription of oxygen by using guidelines from clinical interdisciplinary collaboration (14). An interdisciplinary focus and close collaboration with the ward’s head physisian was emphasised in our project with revised guide for updating charts and new instructions to the physician group describing oxygen as a medication for which prescription in writing is needed.
In the second data collection, in the case of prescription of oxygen, a desired SpO2 value for start-up of oxygen therapy was more often specified. Listing clear criteria and standards for when and how oxygen therapy shall be administered will enable us to secure better quality oxygen therapy. At HHHFNC and CPAP treatment, desired SpO2 value was more often defined. Several studies have recommended monitoring the patient’s SpO2 value, respiratory rate, heart rate, and respiratory rate (1). However, no clear consensus exists with regard to evaluations of SpO2 value and start-up of oxygen therapy in the case of bronchiolitis (1). As a result, oxygen therapy is administered on varying SpO2 values. In Great Britain, a SpO2 value between 92-95 is recommended for initiating oxygen therapy, while the corresponding SpO2 limit in the US is 90 (1).
As described in the Norwegian Knowledge Centre for the Health Services’s model for quality improvement, anchoring all quality improvement work in leadership is essential (10). It is also vital that time is spent on information and discussion with all involved. During the work process we wished to focus on prescription of oxygen therapy in the whole personnel group and to discuss current practice for written documentation of administration method and observations related to oxygen therapy. We had an inkling that we were not implementing this treatment in line with recommended criteria and standards, and this has been confirmed by the registrations.
Feedback, written and oral, is a common strategy for quality improvement. It is most effective when clear goals and action plans are made, and when the improvement work is carried out by a supervisor or colleague (17). Data from the patient records with registration of current practice for written prescription of oxygen, administration method, and observations and documentation have been presented and evaluated in seminars and teaching sessions for the whole personnel group. This gave impetus to interdisciplinary discussions on the ward. We have increased the awareness around the use of oxygen and the respect for oxygen therapy. A new procedure for HHHFNC treatment has been implemented. Several studies have identified guidelines as an important tool to support good oxygen management (11). We will keep working on a general clinical guideline for oxygen therapy.
Observations and documentation
A significant change in daily documentation in observation sheets was registered (15 and 46 per cent respectively) between the two data collection points. Cardioscope, continuous pulse oximetry, or occasional checking of pulse oximetry is used to monitor the oxygen therapy. Studies have shown that the patient to a varying degree is monitored in connection with oxygen therapy. This is unfortunate, as inappropriate administration of oxygen may have serious consequences (11). When going through the records it was hard to find precise information of which monitoring method was used, as this was frequently not documented. With CPAP and HHHFNC treatment we assume that the patient was monitored by cardioscope, which is common practice. Prescription of monitoring and method was not a registration parameter in the project, but we noticed that in some instances “’scope, checks” were specified by physician. The value of having the nurse continuously monitoring the effect of oxygen therapy by using pulse oximetry has been described earlier (11). Earlier research has recommended that all oxygen therapy be monitored with pulse oximetry (18).
It has earlier been shown that documenting monitoring on the observation sheet and interpreting vital signs have a significant effect on optimal oxygen therapy (11,13). At the time of the first registration period the observation sheet used did not have any space for entering important observations or to document respiratory effort. The observation sheet was also used in CPAP and HHHFNC treatment, but lacked space for documenting these administration methods. Documentation has, from the time of Florence Nightingale, been one of the nurse’s most important functions (19). The existing sheet’s lack of suitable space may explain why it was not used much. After professional feedback and discussions with nurses and physicians on the ward, we decided to start using a more suitable observation sheet. The new observation sheet, with ample space for documenting both the administration method and the effect of the oxygen therapy, made using the sheet much more practicable. At the second registration we noticed a clear improvement in documentation; the observation sheet was more frequently used. Earlier studies have shown that good monitoring and interpretation of vital signs give a more certain effect of the oxygen therapy (11). The frequency of documentation of observations has varied at the two times of measurement in our project. According to Australian recommendations all settings and values should always be documented at the shift change-over or in case of any changes (13).
We have not seen any significant improvement in the documentation of administration methods in the main charts despite having communicated back to personnel on the results of the first data collection, which showed incomplete chart completion. The main chart gives a good overview, such as for instance of how many days the patient has received oxygen therapy.
Strengths and limitations
A strength of the project is that patient records of all hospitalised patients with bronchiolitis and pneumonia were read in a limited time period with a one year interval. The implementation was anchored in leadership and involved both physicians and nursing groups. A weakness of the project may have been that we used only data from the patient chart (main chart, medication charts, charts for prescriptions, observation sheets) and nursing documentation in DIPS as a basis for reviewing if oxygen was prescribed in writing. The reason for choosing to register data solely from the patient record is that this document is what nurses first and foremost use to initiate further observations and interventions. We considered including physician’s memo in the patient record in the study, but as such data did not supply any new information to the review, this information was not systematically read and registered. Another weakness of the project may be that only the patients’ diagnosis at admission was registered at the two data collection times. Some of the patients admitted with diagnosis bronchiolitis received an additional diagnosis of viral pneumonia. Experience has shown that these patients will need oxygen for a longer time period. Registering any additional diagnoses would have been an advantage as such diagnoses may result in a longer stay.
Conclusion
The project has shown that current practice concerning prescription of oxygen therapy was unsatisfactory. The study also shows that documentation practice for administering and monitoring was significantly different in the second data collection period. The findings from the first registration have resulted in the development of new local policy for written prescription of oxygen, and a systematic effort to work out new clinical guidelines for oxygen therapy has been initiated.
We want to thank section head physician Asle Hirth, statistician Jannicke Igland, nurse Jennifer Cairncross, and the personnel group on ward 4 for good discussions, commitment, and ideas during the implementation of the project.










Comments