A survey of clinical competence among health personnel in care homes: a pilot study
The registered nurses demonstrated a higher level of competence than the nursing associates and healthcare assistants. However, scores were too low in all three groups in response to emergency scenarios.
Background: The clinical competence of health personnel affects the health care provided for elderly patients. It is therefore important that the personnel have a level of knowledge that fulfils the requirements set by the institution they work for. The interdisciplinary clinical competence available in Norwegian municipal healthcare has not been surveyed to any appreciable degree.
Objective: To survey the clinical competence of health personnel who work on care home wards with a locked-door policy, and to identify any need for competence enhancement they may have in responding to clinical incidents. We also sought to investigate how parts of the survey instrument could be improved.
Method: The questionnaire included ten demographic questions and 19 clinical questions for which correct answers had been set for each occupational group. Data were collected in October 2018 and statistically processed in SPSS using parametric analyses, Spearman’s Rho and Cronbach’s alpha.
Results: There were 56 participants. The average percentage of correct answers among the registered nurses (n = 15) was 59%. This percentage was 53% among the nursing associates (n = 31) and 41% among the healthcare assistants (n = 10). The number of correct answers was only influenced by occupational background (p-value 0.018), with the healthcare assistants’ level significantly lower compared to the registered nurses (p-value 0.013). Overall, the health personnel gave the highest number of correct answers in response to clear symptoms of new disease, and the most incorrect answers in response to vague, complex conditions and two emergency scenarios. As many as 62 per cent reported a need to enhance their own clinical competence.
Conclusion: The health personnel demonstrated varying levels of clinical competence, with the registered nurses achieving the highest scores. The study highlights the importance of positive and well-defined interaction between the different categories of staff. The results indicate that all occupations have a need for competence enhancement in responding to serious, often complex clinical situations. The questionnaire should be developed further in order to minimise the scope for interpretive differences in respect of response alternatives. We recommend trialling open-ended text responses to allow for explanations of the clinical judgement on which the choice of answer is based. Future surveys of competencies using the same instrument should involve a larger sample.
Frail elderly patients in the care of the municipal health service need to be looked after by health personnel with sufficient clinical competence, particularly if they are also suffering from a dementia disease. Whenever the patient’s ability to communicate is impaired, there is an increased risk that signs of disease, symptoms and problems are under-communicated, misunderstood or remain unidentified (1).
Early identification of new and worsening symptoms is crucial for the individual patient’s quality of life and sickness load, and prevention of premature death (1 – 6).
Status after the introduction of the Care Coordination Reform
After the introduction of the Norwegian Care Coordination Reform, the specialist health service has been reserved for the most seriously ill patients who cannot receive satisfactory treatment locally (7). This arrangement has raised the bar in respect of the clinical competence that is required in the primary health care system.
Over the last ten years, researchers have been describing an existing competence gap and the consequences of insufficient competence (8–10). Any patient transfer from a care home to treatment in hospital can cause severe distress in geriatric patients, particularly in cases of cognitive failure (11).
Unnecessary hospitalisations are associated with fundamental uncertainty and a lack of clear procedures in assessing vulnerable care home patients, which may be caused by insufficient clinical competence (12).
Health personnel are meant to be in possession of several types of competence to be able to deal with different, often complex pathological pathways as well as the patient’s relatives (13, 14). The legislation requires the health services to offer a safe level of competence (15). However, international and Norwegian research can demonstrate that the health services are often found wanting when it comes to standards and competency targets (2, 8, 12, 14, 16).
A survey of staff competence may improve our knowledge of whether the health service provides the desired quality of care, and will be helpful when planning future competence enhancement initiatives. This study focuses on personnel who work on wards with a locked-door policy because patients on these wards are particularly vulnerable and because more knowledge has been called for about the competence of health personnel who work in dementia care (3, 4, 14).
What is clinical competence, and how can this be measured?
Clinical competence is an aspect of practical nursing which is defined in the literature as a mix of skills, knowledge, attitudes and ability to perform a technique (13).
Although all health personnel by definition represent clinical competence (15), it is unreasonable to expect the same level of competence from different occupations due to their dissimilar qualifications, responsibilities and functions. Clinical competence will inevitably be reflected by level of education, but the individual’s knowledge and experience will also come into play (17). Consequently, the competence available on a ward will depend on who is on duty.
Unskilled workers (healthcare assistants) tend to have no healthcare training. Statistically, they make up approximately 20 per cent of the health personnel that work in Norway’s municipal health services (18). Few studies have investigated how employing this proportion of unskilled labour impacts on the quality of care and the standard of patient safety (19), and more information about this group of workers has been called for (8, 19).
It has been demonstrated that the make-up of staff categories, the proportion of registered nurses (RNs) and the interaction between the different occupations impact significantly on the quality of the work (2, 4, 8, 9). This is why our study’s target group is health personnel with a range of different qualifications: RNs, nursing associates and healthcare assistants.
The NOP-CET competence evaluation tool
Previously, there was no validated survey instrument for measuring the competence of several different categories of heath personnel in the municipal health service (20). The Nursing Older People – Competence Evaluation Tool (NOP-CET, 2015) was therefore developed specifically for this purpose (20). NOP-CET includes a description of 19 clinical scenarios concerning a fictitious patient, ‘Ms Olsen’. These descriptions were used to formulate the survey questions in this pilot study.
The survey questions were intended to collect statistically measurable data concerning the judgement that health personnel make when confronted with ill health: ‘What action will you take when vulnerable Ms Olsen, who is 90 years old, develops new symptoms …?’. The participants were asked to choose one of six response alternatives (Figure 1).
The questions establish whether the patient will receive the right healthcare assistance. The competence that is surveyed, requires respondents to have knowledge of symptoms and awareness of their own personal experiences and occupational role (17). NOP-CET has previously been used with only one set of correct answers applicable across different categories of health personnel (8).
By differentiating the correct answers according to occupation, representatives of the different occupations can give different answers, which are nevertheless correct, based on their personal responsibilities and qualifications. A pilot study such as this can help to improve the instrument for future use.
The study’s objective
The study’s objective was to survey the level of clinical competence among an interdisciplinary group of health personnel from care home wards with a locked-door policy. We also wanted to identify any need for clinical competence enhancement. Parts of the survey instrument were investigated with a view to improvement.
Method
Design
The pilot study had a quantitative cross-sectional design. We used a questionnaire with descriptions of clinical scenarios taken from the NOP-CET instrument, plus ten demographic questions.
NOP-CET consists of 365 questions, of which we used 19. These relate to clinical judgements and decision-making in scenarios that involve common acute symptoms in elderly patients who are cared for by the municipal health service.
NOP-CET was developed by experts in geriatrics using a Delphi process. It was tested on a sample of more than 1000 community-based healthcare personnel. The instrument has been evaluated for validity and reliability and has been recommended for further use (20).
Based on earlier experience of the questionnaire (8) and input from the care home management, we introduced everyday Norwegian terminology in addition to medical terminology in order to promote the inclusion of unskilled workers, e.g. dyspnoea at rest (shortness of breath).
Due to the limited scope of the study and the need to preserve anonymity, the Norwegian Centre for Research Data (NSD) recommended that we replace background data questions that might elicit exact numbers with questions about categories. We were also advised to avoid questions about gender and cultural background.
In this study, selected parts of the NOP-CET questionnaire were changed by introducing a new set of correct answers based on the care home’s guidelines for acute and critical illness. According to these guidelines, the different occupations carry different responsibilities and need to take different actions.
The guidelines use ‘all other health personnel’ as a generic term to include both nursing associates and healthcare assistants. These are all expected to report any serious observations to the RNs. Nursing associates and healthcare assistants would give a right answer to all questions by opting for ‘initiate nursing measures’ whenever symptoms arise.
They will also be deemed to give the right answer if they recognise the most serious scenarios and choose ‘request same-day doctor’s assessment’ or ‘call for emergency help’. RNs are expected to undertake independent examinations, notify a doctor or call for emergency assistance depending on the seriousness of the situation. This is why the correct responses expected from RNs were different to the correct responses expected from both nursing associates and healthcare assistants (Table 1).
Ethical considerations
The questionnaire was approved by care home manager. The heads of each ward informed staff by talking to them and by putting up posters about the study’s objective, consent, the right to withdraw responses, anonymity, storage, and time of data destruction. This information was also printed on the questionnaire. NSD approved the project in advance on 29 September 2018 (reference number 934395).
Data collection
We recruited participants from nine wards with a locked-door policy at a care home with 110 staff. The care home’s health personnel (the population) consisted of 19 RNs, social educators or other staff with higher education, 56 nursing associates, auxiliary nurses or carers and 35 healthcare assistants with a contract of employment.
In the dataset, the survey participants are categorised as RNs, nursing associates and healthcare assistants, while managers and doctors were excluded. The participants could choose whether to answer the questions in an online Questback questionnaire over the phone or on paper.
They also received two reminder text messages ahead of the submission deadline. The data were collected in October 2018.
Analyses
The data were processed using IBM SPSS Statistics for Macintosh, version 24.0. We conducted a descriptive frequency analysis and a cross-tabulation analysis of the demographic data. A near to normal distribution of data allowed us to use parametric analyses such as a t-test and One-way ANOVA (21), including chi-square testing.
If an outcome was found to be significant, we used a post-hoc Tukey HSD test in order to establish which group was statistically different. We considered p-value ≤ 0.05 to be statistically significant.
The observations were analysed in accordance with the correct answers set for the different occupations. We coded the answers as incorrect = 0 or correct = 1. In this way, the level of clinical competence was defined by the number of correct answers, with 19 correct answers giving a score of 100 percent.
No limit was set for an acceptable level of competence, but scores below or above 50 percent may illustrate a lower or higher competence level.
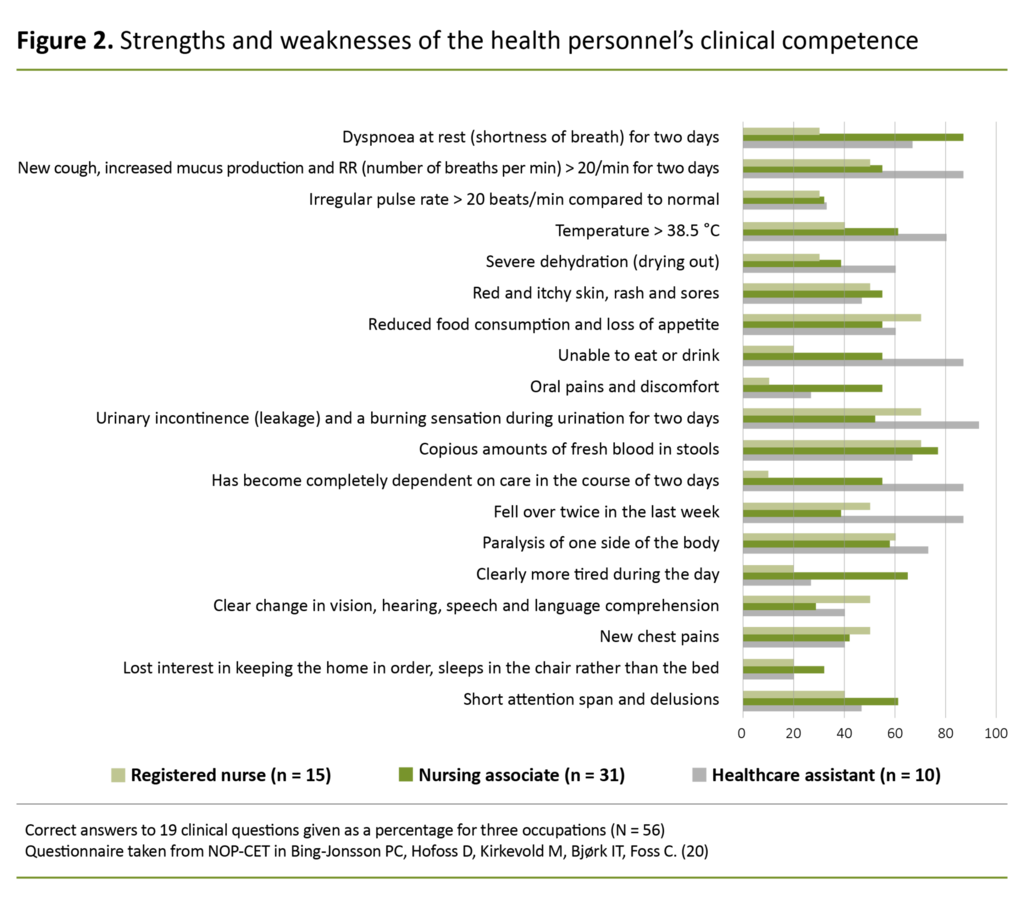
We added up the variables to find a total score for the number of correct answers (%) given by each occupation to each question (coded 0–1). The average value for each occupation was calculated on the basis of these results (Figure 2).
We then investigated whether there was a correlation, and what correlation there was between the number of correct answers and the background variables. For this purpose we used parametric analyses for categoric variables, and the Spearman’s Rho correlation coefficient for graded alternatives.
Significant outcomes were tested in a linear regression analysis. The questionnaire was checked using Cronbach’s alpha on the combined responses as well as on responses per occupation. Cronbach’s alpha measures the stability of a Likert scale questionnaire by testing it for systematic error and bias, and whether the results are reliable (22).
Results
Description of the sample
The survey achieved a response rate of 51. The sample (N = 56) consisted of nursing associates (n = 31), registered nurses (n = 15) and healthcare assistants (n = 10) (Table 2). One person with no specified occupation was excluded from the study. The sample represented 79 percent of RNs, 55 percent of nursing associates and 29 percent of healthcare assistants working at the care home.
The number of years since acquiring a qualification varied from zero to more than ten, and over half had been working in healthcare for more than ten years. Of the respondents with healthcare qualifications, 67 percent were working a full-time equivalent of 75 percent, and more than 90 percent were making use of Gerica for patient documentation.
Moreover, 69 percent had attended some form of training in the last 12-month period, and 30 percent had completed a programme of further study. The majority (62 percent) wanted to enhance their competence in dealing with similar clinical scenarios.
Survey results
The participants (N = 56) demonstrated varying levels of clinical competence, as shown in Figure 2. More than 50 percent of respondents gave the right answer in scenarios with clear symptoms of disease: abnormal respiration, signs of infection, copious amounts of blood in stools, sores, a change in levels of functioning, falling, refusal to eat, paralysis of one side of the body and symptoms of urinary infection and delirium.
Fewer than 50 percent of the respondents gave correct answers in scenarios that may be considered vague: elevated irregular pulse rate, loss of interest in keeping the home in order and sleeping in a chair rather than a bed, clearly more tired during the day, and severe dehydration.
Fewer than 50 percent of the respondents gave correct answers in scenarios that may be considered vague.
Additionally, fewer than 50 percent of the answers were correct in response to two emergency scenarios – one involving chest pains, the other involving a clear change in sensory responses and language. On average, response option 4 (initiate nursing measures as soon as possible) was chosen more often than any of the other five possible answers.
The RNs (n = 15) achieved an average score of 59 percent correct answers. The lowest score was 7 and the highest 14 of the 19 possible. Figure 2 shows that in response to eleven questions, more than 50 percent of the RNs gave a correct answer, while in response to eight questions, fewer than 50 percent gave the correct answer.
Compared to the other staff categories, the RNs gave the largest number of correct answers to nine questions, but for the remaining ten questions their scores were below that achieved by the nursing associates and the healthcare assistants. In respect of these ten questions, the guidelines expected RNs to conduct independent examinations and to initiate measures, or there was a need for a doctor’s assessment or emergency help.
The nursing associates (n = 31) achieved an average score of 53 percent correct answers. The lowest score was 6 and the highest 19 out of 19. The healthcare assistants (n = 10) achieved an average score of 41 percent correct answers, the lowest score being 2 and the highest 14.
Compared to the other staff categories, the RNs gave the largest number of correct answers to nine questions.
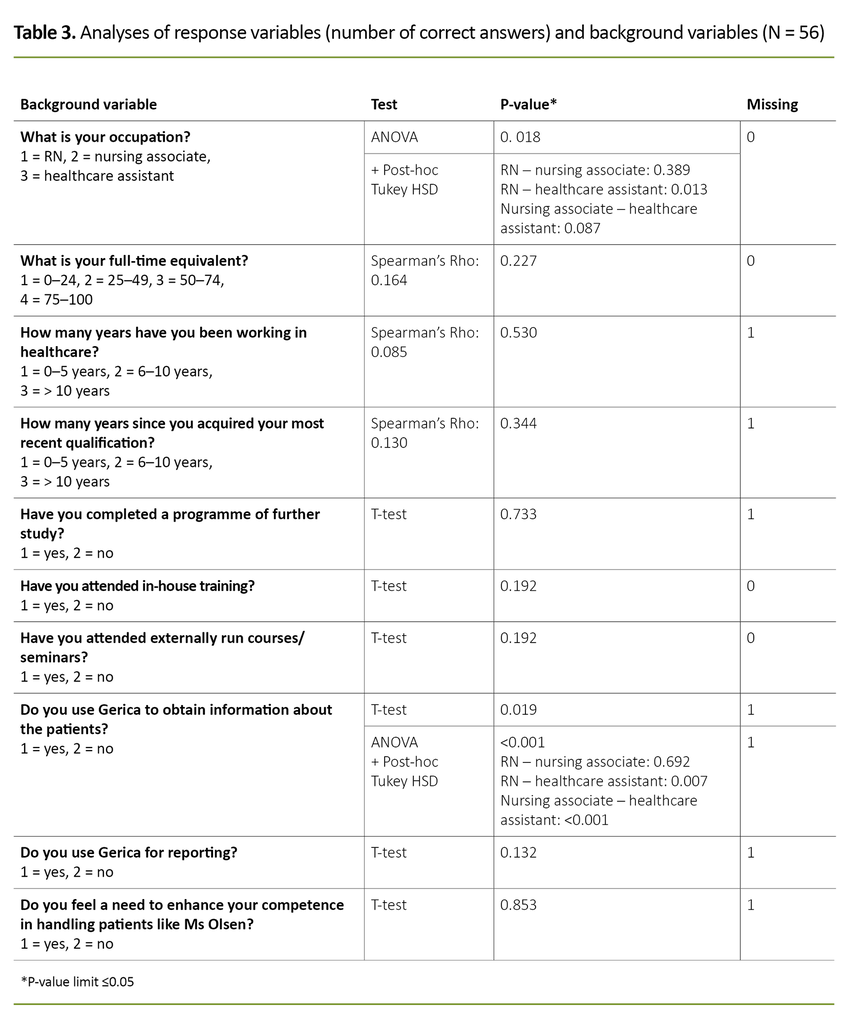
Extended ANOVA analyses showed that the number of correct answers given by the RNs and the nursing associates was not significantly different (p-value 0.389), nor was there a significant difference between the nursing associates and the healthcare assistants (p-value 0.087). However, the analysis showed a significant difference (p-value 0.013) between the number of correct answers given by the RNs and the healthcare assistants.
The correlation analysis of graded response options showed that the Spearman’s Rho coefficient was between 0.085 and 0.164, which suggests a weak correlation between the number of correct answers and the background variables.
Parametric testing of the remaining categoric response alternatives gave two significant outcomes: occupation (p-value 0.018) and the use of Gerica for information retrieval (p-value < 0.001). Regression analysis showed that the number of correct answers was influenced only by occupational background.
Cronbach’s alpha for all occupations combined was 0.788 (N = 56). For the registered nurses (n = 15), Cronbach’s alpha was 0.618, and for the nursing associates (n = 31) and healthcare assistants (n = 10) Cronbach’s alpha was 0.796. The results therefore demonstrated relatively good internal consistency.
Discussion
All occupations demonstrated clinical competence, but to varying degrees. An earlier study (8) also found a difference between the competence levels established by survey and the expected competence levels, as in our study. However, the results show no statistical difference between RNs and nursing associates, even if the RNs answered more questions correctly.
In respect of ten questions, a larger proportion of the nursing associates and healthcare assistants gave more correct answers than the RNs.
Because the health personnel who took part in this pilot study were measured against a differentiated scale, all respondents had the same opportunity to achieve a maximum score. The lack of a difference between the scores achieved by RNs and nursing associates may suggest that an equal proportion of RNs and nursing associates gave correct answers, although the bar was set higher for the RNs in terms of their expected clinical competence.
The results also show that in respect of ten questions, a larger proportion of the nursing associates and healthcare assistants gave more correct answers than the RNs. These findings are also considered to be an effect of tailoring the set correct answers to different categories of staff.
The level of competence among health personnel
Figure 2 is a bar chart showing the number of correct answers given by each occupation as a percentage. The chart is a visual representation of the strengths and weaknesses of the measured levels of competence.
Overall, the respondents gave the greatest number of correct answers when there were clear symptoms of worsening illness, and the greatest number of incorrect answers in scenarios that may be considered complex or vague. The score achieved by all occupations must be said to be too low in two out of three emergency scenarios.
It is to be expected that clear symptoms elicit the greatest number of correct answers while vague conditions increase the number of incorrect answers due to the high level of complexity and difficulty involved. Symptoms of disease in the elderly are often camouflaged by comorbidity and polypharmacy (23, 24). If new, vague symptoms occur on top of this, a higher level of competence is required to judge what is the correct action.
For patients with dementia, these are important matters because cognitive impairment and geriatric psychiatric diagnoses may camouflage symptoms of worsening illness and make it more difficult to make a clinical assessment (1, 4). Vague symptoms require a broad nursing approach involving screening and pre-examination of the patient, often before contacting a doctor (23, 24).
It is also essential that emergencies are recognised and handled as such. When team members make good observations and report these to an RN, it tends to be the RN’s level of competence that determines what further assistance is provided.
RNs make up a minority staff group in care homes, but they carry the greatest responsibility for clinical assessments and initiating correct measures. The study may help to highlight not only the RNs’ dependency on the competence of co-workers, but also the importance of their presence on every ward, as demonstrated by other research on competence levels in the municipal health service (9).
The number of RNs in the study is too low for the results to be of transferable value, but RNs are sufficiently well represented for the care home to consider the results to be valid for this occupational group.
RNs who work in the primary health service find that their competence needs to meet a high level of requirements (14, 16, 24–26). Japanese researchers have showed that the competence level of RNs does not rise linearly with experience; instead, the curve rises steeply in the first five years.
After ten years, the level stabilises unless a change is introduced, such as completing a programme of further study, taking on new tasks or other career-related matters (27). This is supported by international and Scandinavian research (25, 26, 28).
All studies stress the employer’s responsibility for giving RNs competence enhancement opportunities in accordance with the health service’s expectations of them. The International Council of Nurses defines the specific role and function of RNs as a lifelong dynamic process: ‘Nurses require appropriate initial and ongoing education and training as well as lifelong learning to practice competently within their scope of practice’ (29, p. 2).
The expected responses from nursing associates were the same as those for healthcare assistants.
In our study, the expected responses from nursing associates were the same as those for healthcare assistants because the guidelines refer to both occupations as ‘all other health personnel’. This synthesis of expectations relating to two different occupational groups in care homes can be perceived to downgrade the nursing associates’ responsibilities and functions, as they are certified skilled workers, which is not the case for the healthcare assistants.
However, according to the guideline criteria for reporting to an RN, nursing associates and healthcare assistants have the same responsibility, and the set correct answers for these occupations are therefore the same. The Norwegian Health Personnel Act refers to healthcare assistants simply as ‘assistants’, and they are subject to the control and supervision of medically qualified personnel (15).
The study’s results may, even if the number of healthcare assistants is low, serve as a reminder that healthcare assistants should learn about the symptoms of disease and be told what to do when such symptoms arise, so long as they are a part of a healthcare team.
A need for competence enhancement
The results of the pilot study may suggest a need for competence enhancement among the participating healthcare personnel. Most of them wanted such enhancement.
The results suggest that the care home management should invest in competence enhancement initiatives for all occupations, focusing on observation, judgement, and taking correct action when patients experience worsening illness.
What background data affected the level of competence?
The level of competence was only impacted by the participants’ occupational background. The outcomes of our analyses were not affected by age or the number of years working in the health service, nor by attending courses or completing a programme of further study. We may assume that the small size of our sample was the reason why no statistical correlations were identified, and the results can therefore not be considered to be of great value.
The study’s strengths and weaknesses
We used a validated high-quality instrument in order to avoid errors that might affect the results. Most instruments that are available for measuring competence levels include an element of self-assessment (20).
The tool we used gives a score based on correct or incorrect answers to clinical questions, thus providing an objective measure of competence. This avoids the tendency for respondents to either overestimate or underestimate their own level of competence (30). Objective measurements are recommended, and they strengthen the reliability of the results (22, 30).
Cronbach’s alpha tested the internal consistency of the scale, and the values were sufficient to establish good reliability, even if the number of participants was small.
The questionnaire listed response alternatives that may have given scope for interpretive differences, thereby introducing a risk of bias and error. For example, the questionnaire did not explain what ‘initiate nursing measures’ or ‘consult with a colleague’ involved.
Similarly, the exact implication of ‘call for emergency help’ could be open to interpretation: immediately call a nurse/doctor/A&E department or request an ambulance? Consequently, there is room for improvement with respect to the questionnaire.
Working up a new set of correct answers may give rise to systematic errors. We tried to reduce this risk by obtaining input to the questions from the ward management, and by basing the correct answers on the care home’s own guidelines for each occupation.
The study’s objective was to survey the clinical competence level of a specific care home. Because the care home had a specific number of employees, this was reflected in the size of the study. A limited number of participants (N = 56) gave rise to research-related challenges. A response rate of over 50 is considered satisfactory for a study, although it should ideally have been higher (22).
One reason for the low participation rate may be that one of the wards had only recently opened, and the timing of the data collection was therefore less than ideal. No-one withdrew at any stage, and there were few omissions in the completed questionnaires.
Nevertheless, a small sample involving a small number of participants in each group, combined with the dropout rate, reduced the quality of the statistical analyses and the transferable value of the results.
Conclusion
The health personnel at the care home demonstrated varying levels of clinical competence, and the RNs represented the highest level of competence. The study highlights the importance of positive and well-defined interaction between different categories of staff. The results indicate a need for competence enhancement across all occupations with respect to several serious and often complex clinical situations, including emergency scenarios.
The survey that was conducted is an example of how municipal health care agencies can define, measure and evaluate clinical competence.
By conducting a similar survey it is possible to check existing levels of competence and provide a basis for planning competence enhancement initiatives in order to meet the requirement for safe and caring services (24, 31). Defined competency plans can have a positive effect and clarify the interaction between occupational groups.
There is a need to conduct similar surveys involving larger samples, in order to test the validity and reliability of the questionnaire and the new set correct answers, and to establish whether other types of background data will have an impact on the results.
By explaining the implications of each response alternative, continuing the use of simplified terminology and expanding the questionnaire to include open-ended text responses, it may be possible to profile the participants’ own observations and judgements in greater detail. The set correct answers should be based on valid competence targets and be defined as such.
In future research on competence levels, healthcare assistants should be encouraged to take part in order to boost our knowledge of this group of workers.
We are grateful to statistician Leiv Sandvik from the University of South-Eastern Norway for his quality assurance of our statistical work. Thanks also to the care home management for authorising the study and for assisting with the recruitment of survey participants. We also wish to extend our sincere thanks to the healthcare staff who took part.
References
1. Eskeland KO. Alderspsykiatri og omsorgsarbeid. Oslo: Cappelen Damm Akademisk; 2017.
2. Recio-Saucedo A, Dall'Ora C, Maruotti A, Ball J, Briggs J, Meredith P et al. What impact does nursing care left undone have on patient outcomes? Review of the literature. Journal of Clinical Nursing. 2017;27(11-12):2248–59. DOI: 10.1111/jocn.14058
3. Mjørud M, Engedal K, Barca ML, Ytrehus S. Livskvalitet, depressive symptomer og funksjonssvikt hos personer med demens. Sykepleien Forskning. 2011;6(2):178–86. DOI: 10.4220/sykepleienf.2011.0101
4. Kovach CR, Logan BR, Joosse LL, Noonan PE. Failure to identify behavioral symptoms of people with dementia and the need for follow-up physical assessment. Research in Gerontological Nursing. 2012;5(2):89–93.
5. Bauer M, Fetherstonhaugh D, Haesler E, Beattie E, Hill KD, Poulos CJ. The impact of nurse and care staff education on the functional ability and quality of life of people living with dementia in aged care: a systematic review. Nurse Education Today. 2018 aug.;67:27–45. DOI: 10.1016/j.nedt.2018.04.019
6. Neerland B, Watne LO, Wyller TB. Delirium hos eldre pasienter. Tidsskrift for Den norske legeforening. 2013;133(15):1596–600.
7. St.meld. 47 (2008–2009). Samhandlingsreformen – Rett behandling – på rett sted – til rett tid. Oslo: Helse- og omsorgsdepartementet; 2009. Available at: https://www.regjeringen.no/no/dokumenter/stmeld-nr-47-2008-2009-/id567201/sec1 (downloaded 31.10.2019).
8. Bing-Jonsson PC, Hofoss D, Kirkevold M, Bjork IT, Foss C. Sufficient competence in community elderly care? Results from a competence measurement of nursing staff. BMC Nursing. 2016;15:5. DOI: 10.1186/s12912-016-0124-z
9. Ugreninov E, Solstad Vedeler J, Heggebø K, Gjevjon ER. Konsekvenser av sykepleiermangel i kommunene fra et pasient- og pårørendeperspektiv. Oslo: Norsk institutt for forskning om oppvekst, velferd og aldring; 2017. Rapport 7. Available at: https://www.nsf.no/Content/3545405/cache=20171809144820/NOVA-Rapport-7-17-Konsekvenser-av-sykepleiermangel-i-kommunene-web.pdf (downloaded 30.01.2019).
10. Husebø B, Erdal A, Kjellstadli C, Bøe J. Leve hele livet – en kvalitetsreform for eldre. Helsehjelp til eldre: kunnskapsoppsummering. Begen: Universitetet i Bergen, Det medisinske fakultet; 2017. Delrapport. Available at: https://www.regjeringen.no/globalassets/departementene/hod/fellesdok/levehelelivet/kunnskapsoppsummering/011017_kunnskapsoppsummering_helsehjelp_sefas.pdf (nedlastet 30.01.2019).
11. Morphet J, Innes K, Griffiths DL, Crawford K, Williams A. Resident transfers from aged care facilities to emergency departments: can they be avoided? Emergency Medicine Australasia. 2015;27(5):412–8.
12. Ågotnes G. The institutional practice: on nursing homes and hospitalizations. Oslo: Cappelen Damm Akademisk; 2017.
13. Cowan DT, Norman I, Coopamah VP. Competence in nursing practice: a controversial concept – a focused review of literature. Nurse Education Today. 2005;25(5):355–62.
14. Bing-Jonsson PC. Forskning på kompetanse i helse- og omsorgstjenester i kommunene i Norge: Hva bør vi egentlig kunne og hvordan finne ut av det? Demens & Alderspsykiatri. 2017;21(1).
15. Lov 2. juli 1999 nr. 64 om helsepersonell m.v. (helsepersonelloven). Available at: https://lovdata.no/lov/1999-07-02-64 (downloaded 03.10.2019).
16. Stanyon MR, Goldberg SE, Astle A, Griffiths A, Gordon AL. The competencies of Registered Nurses working in care homes: a modified Delphi study. Age and Ageing. 2017;46(4):582–8.
17. Nortvedt P, Grimen H. Sensibilitet og refleksjon: filosofi og vitenskapsteori for helsefag. Oslo: Gyldendal Akademisk; 2004.
18. Helsedirektoratet. Nasjonale kvalitetsindikatorer (NKI). Årsverk med fagutdanning i de kommunale pleie- og omsorgstjenestene. Oslo: Helsedirektoratet; 2020. Available at: https://www.helsedirektoratet.no/statistikk/kvalitetsindikatorer/kommunale-helse-og-omsorgstjenester/fagutdanning-i-pleie-og-omsorgstjenesten (downloaded 13.12.2020).
19. Flodgren GM, Bidonde J, Berg RC. Konsekvenser av en høy andel ufaglærte på kvalitet og pasientsikkerhet i helse- og omsorgstjenestene: en systematisk oversikt. Oslo: Folkehelseinstituttet; 2017. Available at: https://www.fhi.no/publ/2017/konsekvenser-av-en-hoy-andel-ufaglarte-pa-kvalitet-og-pasientsikkerhet-i-he/#resultat (nedlastet 14.02.2019).
20. Bing-Jonsson PC, Hofoss D, Kirkevold M, Bjørk IT, Foss C. Nursing older people-competence evaluation tool: development and psychometric evaluation. Journal of Nursing Measurement. 2015;23(1):127–53. DOI: 10.1891/1061-3749.23.1.127
21. Fagerland MW, Sandvik L, Mowinckel P. Parametric methods outperformed non-parametric methods in comparisons of discrete numerical variables. BMC Med Res Methodol. 2011;11(1):44. DOI: 10.1186/1471-2288-11-44
22. Polit DF, Beck CT. Nursing research: generating and assessing evidence for nursing practice. 9th ed. Philadelphia: Wolters Kluwer Health; 2012.
23. Wyller TB. Geriatri. En medisinsk lærebok. 2nd ed. Oslo: Gyldendal Akademisk; 2015.
24. Meld. St. 15 (2017–2018). Leve hele livet. En kvalitetsreform for eldre. Oslo: Helse- og omsorgsdepartementet; 2018. Available at: https://www.regjeringen.no/no/dokumenter/meld.-st.-15-20172018/id2599850/sec1 (downloaded 15.09.2019).
25. Cooper E, Spilsbury K, McCaughan D, Thompson C, Butterworth T, Hanratty B. Priorities for the professional development of registered nurses in nursing homes: a Delphi study. Age and Ageing. 2017;46(1):39–45.
26. Miraglia R, Asselin EM. The Lasater Clinical Judgment Rubric as a framework to enhance clinical judgment in novice and experienced nurses. Journal for Nurses in Professional Development. 2015;31(5):284–91.
27. Takase M. The relationship between the levels of nurses’ competence and the length of their clinical experience: a tentative model for nursing competence development. Journal of Clinical Nursing. 2013;22(9–10):1400–10.
28. Karlstedt M, Wadensten B, Fagerberg I, Poder U. Is the competence of Swedish Registered Nurses working in municipal care of older people merely a question of age and postgraduate education? Scand J Caring Science. 2015;29(2):307–16.
29. International Council of Nurses (ICN). Position statement. Scope of nursing practice. Genève; 2013. Available at: https://www.icn.ch/sites/default/files/inline-files/B07_Scope_Nsg_Practice.pdf (downloaded 10.01.2019).
30. Schlösser T, Dunning D, Johnson KL, Kruger J. How unaware are the unskilled? Empirical tests of the «signal extraction» counterexplanation for the Dunning-Kruger effect in self-evaluation of performance. Journal of Economic Psychology. 2013;39:85–100. DOI: 10.1016/j.joep.2013.07.004
31. Forskrift 28. oktober 2016 nr. 1250 om ledelse og kvalitetsforbedring i helse- og omsorgstjenesten. Available at: https://lovdata.no/forskrift/2016-10-28-1250 (downloaded 30.01.2019).












Comments