Evaluation of research investment in nurses and allied health professionals in the Northern Norway Regional Health Authority area
The Northern Norway Regional Health Authority has specifically focused over time on enhancing health-related competence and research. This has resulted in a greater number of researchers and research fellows, and an increase in the number of published articles.
Background: At the beginning of the 2000s, Norwegian research in nursing and allied health disciplines was described as weak. Since 2007, the Northern Norway Regional Health Authority has had a strategic focus on enhancing health research.
Objective: The objective of this project was to evaluate whether the Northern Norway Regional Health Authority’s research investment has given results. We have examined research activity, the allocation of research funding, research outputs and facilitating factors for research to be conducted by health researchers (excluding doctors and dentists) in the health trusts.
Method: The survey took place in four health trusts under the Northern Norway Regional Health Authority. In the survey, we used a multi-method approach and a variety of data sources. Quantitative mapping based on research administrative data and systematic searches for published scientific output registered in journal databases were used together with data from a survey conducted among health researchers and research fellows in 2015.
Results: In the period 2008–2015, there was an increase in the number of research fellows, researchers and published scientific output in the health trusts. Competence enhancement has been greatest in nursing and physiotherapy. Researchers and research fellows have contributed to multi-disciplinary research, using a broad range of methodological approaches with a preponderance of qualitative methods. On average, 29 per cent of the articles published in the period were published in level 2 journals. The Northern Norway Regional Health Authority has been the main funding source for the research. The respondents reported time pressure, lack of funding, research culture and adaptation for research as obstacles to conducting research.
Conclusion: There has been a positive development in and strengthening of health research and research-based competence in the Northern Norway Regional Health Authority during the relevant period of time. The results indicate that strategic investment in health research has had a positive effect, and that a similar focus is also recommended for other health authorities.
In 2003, the Research Council of Norway evaluated medical and health research in Norway, mainly research carried out at universities (1).
The report concluded that research in nursing and allied healthcare disciplines could be described as weak and lagging behind other countries such as Sweden and Finland in relation to the development of research programmes and use of resources. The recommendations included greater investment in health research funding (1).
On the basis of the evaluation and identification of health research, i.e. research by nurses and allied health professionals, as a weak area of research nationally, several regional health authorities, including in the north and west of Norway, developed strategic measures to strengthen health research (2, 3).
A strengthening of research in the Northern Norway Regional Health Authority
In order to strengthen such research in the area covered by the Northern Norway Regional Health Authority (NNRHA below), USAM, the advisory body for cooperation between the NNRHA and the universities in Northern Norway, granted funding for a three-year project position of health research manager in 2007.
Moreover, in the new research strategy plans for the University Hospital of North Norway (UNN)(4) and the NNRHA (5), healthcare was designated as one of several priority areas where research was weak.
The purpose of the NNRHA’s investment has been to boost research among staff with a bachelor’s degree in one of the healthcare professions, such as nursing, midwifery, physiotherapy, occupational therapy, bio-engineering, radiography and social work.
Implemented measures
Specific measures that have been implemented include the position of health research manager and the prioritisation of health research in the NNRHA’s allocation of research funding.
The tasks of the health research manager have included the provision of research supervision and advice, establishing support functions, developing courses or seminars, and developing research networks among health researchers from both the somatic and psychiatric fields.
No individual allocation for health research has been announced as part of the research funding. However, if projects have been deemed worthy of support, funding has been granted annually to at least one health researcher’s doctoral or post-doctoral project.
Evaluation of research investment
As part of their work on a new research strategy for the NNRHA applicable from 2016, Sirona Health Solutions (Sirona) was tasked with evaluating the NNRHA’s research investment in the period 2002–2013 (6).
The final report in March 2015 concluded that both research activity and research competence in the NNRHA have increased in line with the strategic investment (6). In relation to health research, Sirona concluded that it was not possible to analyse allocations in this area in greater depth on the basis of the data collected (6, p. 73).
The objective of the study
The objective of this study was to evaluate the NNRHA’s health research investment in the period 2007–2015. The following research questions were explored:
- What characterises health research activity in the period?
- To what extent has research funding been granted to health researchers?
- To what extent have health researchers contributed to the NNRHA’s research output?
- How do health researchers regard the conditions for research in the health trusts?
Method
The survey took place in four of the five health trusts in the NNRHA, with the exception of the Northern Norway Pharmaceutical Trust. We used a multi-method approach with various kinds of data and data sources.
Through searches in the Pubmed and Cristin databases, we identified research articles published by health researchers with an affiliation to or address at the health trusts. The searches were limited to published articles in the period from 2008 up to and including 2014 for which health researchers were the first, last or co-author.
We used administrative data from research allocations in the period 2008–2015 to map the award of PhD fellowships and research funding to health researchers.
The NNRHA’s secretariat for advertised research funding provided data on the number of applications and awards. The number of PhD degrees completed in the period was derived from annual reporting on the NNRHA’s research funding (2008–2015) (7) as well as the University of Tromsø’s (UiT) overview of completed doctoral degrees (8).
The questionnaire was sent to researchers
We used snowball sampling or network sampling in order to gain an overview of health researchers and research fellows (PhD candidates) as of June 2015 (9). In short, we asked each of the researchers or research fellows identified whether they knew of others who were not included on our list.
Our starting point was researchers who had been identified on the basis of data from a former health research manager in the NNRHA. All health researchers and research fellows employed in main or additional positions in the NNRHA’s health trusts (n = 42) were sent an electronic questionnaire developed specifically for this survey.
Content of the questionnaire
The questionnaire contained both individual questions from similar research surveys at UNN (10, 11) and questions developed specifically for this project.
The questionnaire contained the following questions with pre-coded responses on a nominal or ordinal scale: gender, place of work (health trust), affiliation to health trust in a main or additional position, affiliation to the university or university college in a main or additional position, number of years since completion of first degree, background in healthcare, number of years employed in the health trust in the period 2008–2015, PhD qualification, year of completion of PhD, PhD funding, work tasks in clinical practice, time allocated to research, methodological approaches in own research, and partners in research.
In addition, we asked the following open-ended question: ‘Mention up to three factors that can hinder or assist your research.’
Implementation of questionnaire survey
The questionnaire was reviewed and piloted at a meeting between three health researchers and a research fellow at UNN, all of whom were registered nurses (RNs). No changes were found necessary. The questionnaire survey was carried out using Questback.
We reported the project to UNN’s data protection officer before commencing, and the data protection officer had no objections to the planned implementation of the questionnaire survey. An ICT colleague in the clinical research department administered the questionnaire in Questback, and sent a selective reminder after two weeks.
On completion of the data collection, the ICT colleague submitted a de-identified dataset to the researcher. The data were stored in compliance with UNN’s routines for handling research data.
The information letter informed the survey participants that the data would be handled confidentially and would be de-identified. A total of 30 – 14 researchers and 16 research fellows – answered the questionnaire (response rate: 71).
Data analysis
We carried out descriptive statistical analyses using SPSS, version 20 (IBM SPSS Statistics), and present summary measures such as number, percentage, average, median and dispersion in this article.
We used Microsoft Excel to group the results in figures and tables. Responses to the open-ended questions were analysed and categorised using summative content analysis (12).
In the presentation of results, we use the term ‘researcher’ of staff with a professional healthcare background and PhD qualifications, and ‘research fellow’ of healthcare staff who are in the process of enhancing their competence at PhD level.
Results
Research competence and professional background
When the strategic investment in health research was introduced in 2008, there were altogether seven health researchers with PhD qualifications and four research fellows in the NNRHA’s health trusts.
Snowball-sampling in the middle of 2015 identified a total of 19 researchers and 23 research fellows in the health trusts. Of these, three researchers and three research fellows were men. Most were employed at UNN – 15 researchers and 17 research fellows respectively.
The nineteen health researchers had the following professional backgrounds: eleven RNs, two midwives, four physiotherapists, one bio-engineer and one occupational therapist. The professional background of the 23 research fellows was similar: twelve RNs, six physiotherapists, two bio-engineers, one social educator, one occupational therapist and one social worker.
Research funding
As regards the allocation of research funding to health researchers and research fellows, a total of 17 currently employed research fellows had received funding from the NNRHA in 2015. Over time, research funding allocations have varied from zero to five PhD fellowships per annum awarded to people with a professional healthcare background.
The NNRHA was the most important funding source for research fellows.
From and including the 2009 allocation, a total of three health researchers have received post-doctoral funding. Two out of a total of 55 researchers with post-doctoral fellowships in the period 2010–2015 were health researchers (excluding doctors and dentists) from the NNRHA.
Numbers given by survey respondents (n = 30) showed that the NNRHA was the most important funding source for research fellows. A total of twelve out of 16 research fellows had received a PhD grant from the NNRHA, three had a university grant and one had a grant from the Research Council of Norway.
A greater proportion of the research fellows (75 per cent) had received their PhD fellowship from the NNRHA compared with the researchers (36 per cent).
Research output
In the period 2008–2015, ten PhD degrees were completed by candidates with a healthcare background receiving full or part funding from the NNRHA. In addition, five PhD degrees completed by healthcare staff in the health trusts had been funded by a different funding source (7).
Figure 1 shows the number of scientific articles published per annum in the period 2018 up to and including 2014 where one of the authors was a health researcher or research fellow employed in a health trust.
Over time, the number of published articles has increased annually and in 2014, altogether 31 research articles by an author with a nursing or allied healthcare background were published (Figure 1). The percentage of level 2 articles (light green column) has remained stable at over 25 per cent annually from 2011.
Moreover, the figure shows a steady increase in the number of articles where authors employed in a health trust were first or last author (grey column). In 2014, these articles represented 68 per cent of the total (21 out of 31 articles).
Characteristics of health research activity in the NNRHA
By means of the questionnaire, we identified the characteristics of and conditions applying to health research. The responses to the question on how long ago the researchers and research fellows had completed their first degree showed that the median (minimum–maximum) age was 30 (10–35) years for researchers and 28 (11–36) years for research fellows.
In response to the question on research partners, ten out of 14 researchers (71 per cent) stated that they had regional partners and ten out of 14 researchers (71 per cent) stated that they worked with international partners or co-authors in their research.
Most stated that their partners were doctors.
Of the research fellows, twelve out of 16 (75 per cent) stated that they had regional partners and ten out of 16 (62 per cent) stated that they had international partners or co-authors in their own research. To a considerable extent, the research cooperation was interdisciplinary.
Most stated that their partners were doctors (70 per cent), while RNs were the second most common partner followed by physiotherapists.
In response to the question ‘What methodological approaches do you use/have you used in your research?’, 20 out of 30 researchers and research fellows (67 per cent) reported that they had used qualitative methods. Figure 2 presents the methodology used by researchers and research fellows.
The following areas were included among the responses to the open-ended question on the subject area in which researchers and research fellows carried out their research: child/adolescent health, e-health/e-records, refugee health, public health, gastrology, immunology, intensive care medicine, cardiology, clinical ethics, cancer, chronic somatic symptom disorder, women’s health, neurology, obstetrics, mental health, rehabilitation and rheumatology.
Conditions for health researchers in the health trusts
Of the 14 health researchers in the health trusts participating in the survey, five (36 per cent) reported that no working time was set aside for research in their current position.
The median time set aside for research was ten per cent, varying from 0–100 per cent, and three people were employed in 100 per cent research positions. Eight out of 16 research fellows (50 per cent) had 100 per cent research fellow positions.
We also asked researchers about the work tasks their job in the health trust covered, using the following pre-coded response alternatives: clinical patient/client work, management, teaching/supervision of students/staff, research and quality work/professional development.
Multiple alternatives could be chosen. The results are presented in Figure 3. The figure shows that 50 per cent had clinical work tasks, and that around 60 per cent worked with research.
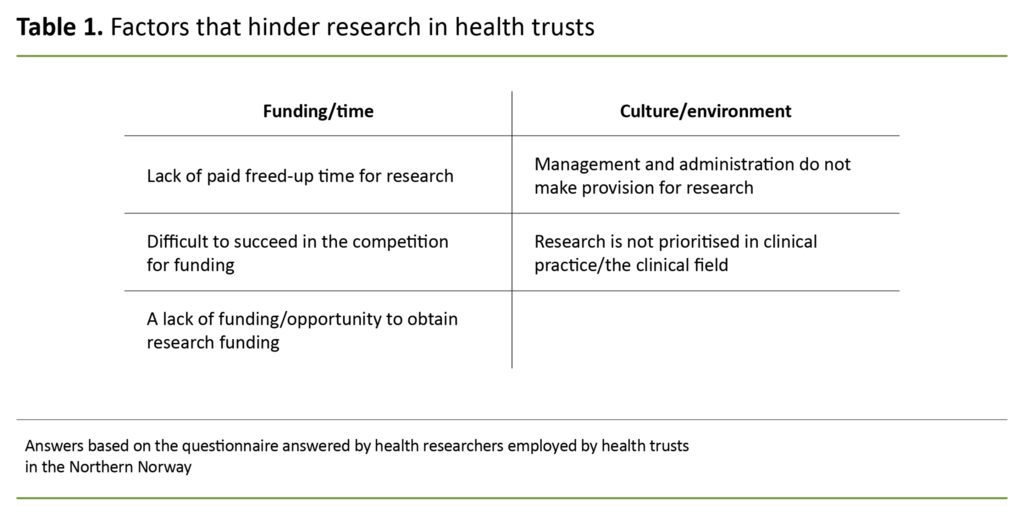
In an open-ended question, we asked the researchers to give their views on the three most important factors that hindered research. These were divided into the following categories: funding/time and culture/environment, although these overlap to some extent. The categories and sub-groups are presented in Table 1.
The researchers specified the following concrete examples: ‘Not enough time due to other work tasks’, ‘Lack of help in conducting research and lack of funding’, ‘Finding a good combination of research and other tasks in clinical practice’, and ‘Lack of additional positions at UiT so that I can’t be a main supervisor’.
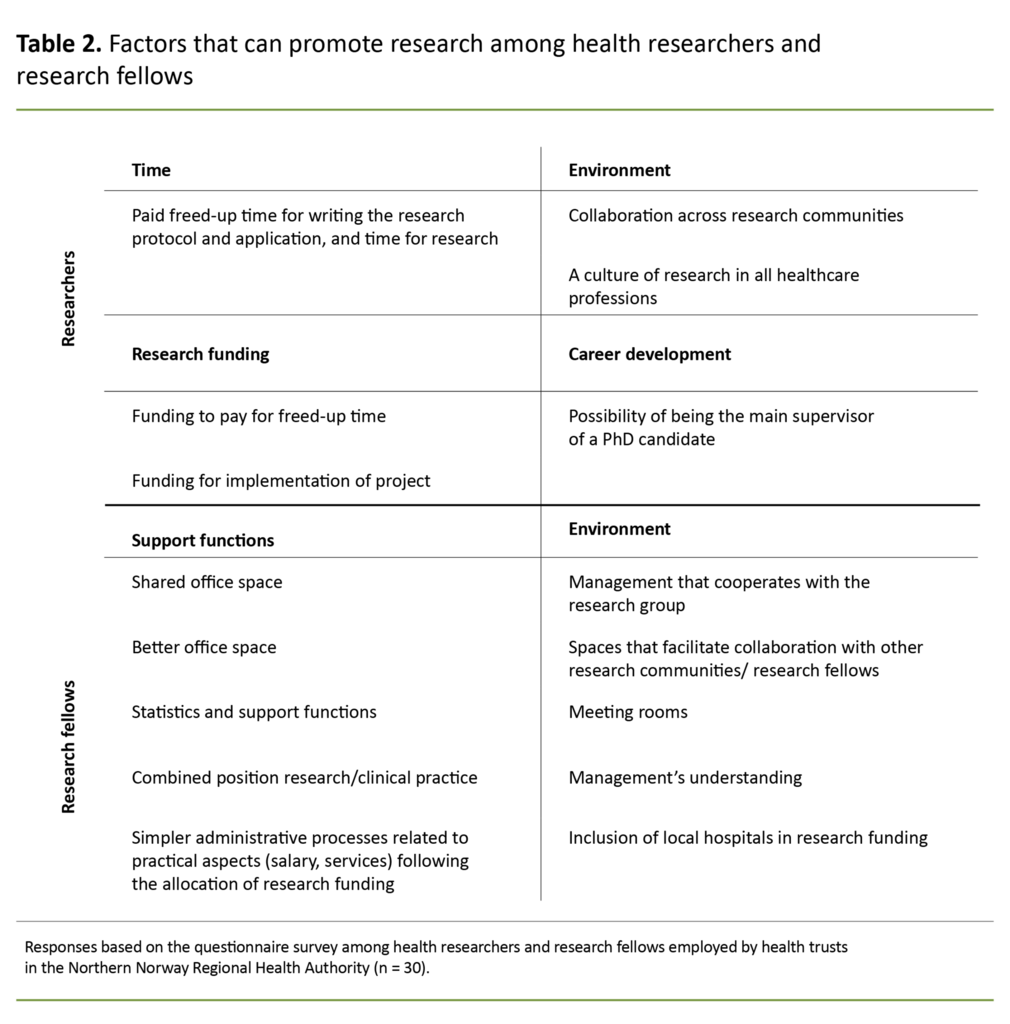
The researchers and research fellows were also asked in an open-ended question to describe the three most important factors that can assist their own research.
Following the content analysis, we categorised factors that can promote research among the researchers into two categories: support functions and environment. Table 2 shows the combined results.
Discussion
Characteristics of health research activity in the NNRHA
In the period from 2008 to 2015, there was a steady increase in the number of health researchers and research fellows in the NNRHA, especially at UNN. Competence enhancement has been greatest within nursing and physiotherapy. In the smaller health trusts and in some healthcare disciplines such as radiography, research competence has not been strengthened to the same extent.
The research covers a broad range of disciplines. In the case of the NNRHA, there has been an annual award of from one to five new PhD or post-doctoral fellowships to candidates with a professional healthcare background. In this period, 15 doctoral degrees were completed where the candidate had a professional healthcare background and received funding from the NNRHA and/or employment in the health trust.
In step with an increasing number of researchers and research fellows, there was also a steady increase in the number of published articles in the period, and on average 29 per cent of these were published in level 2 journals. Only two out of altogether 55 postdoctoral fellowships were awarded to health researchers in the period 2010–2015.
In step with an increasing number of researchers and research fellows, there was also a steady increase in the number of published articles in the period.
The research investment in the period 2008–2015 has helped to build research competence among own staff who have largely chosen to stay on in the health trusts. However, there are considerable differences between the health trusts.
As yet, the Helgeland Hospital Trust has not succeeded in building or recruiting health research competence, while UNN has recruited more people with such competence externally while also successfully building competence internally.
The NNRHA is aware that increasing research activity at the smaller health trusts is more challenging than at UNN (6).
The median age since completion of the first degree was 28 years among research fellows and 30 years among researchers. The Nordic Institute for Studies in Innovation, Research and Education (NØverst i skjemaetIFU)’s survey of research carried out by RNs reported an average of 18 years since the research fellows had completed their first degree (13). The average age among candidates in the NNRHA can therefore be said to be high.
Aamodt et al. also found that the average age among research fellows in nursing was considerably higher than in the entire research fellow population per 2017 (13). In the future, efforts should be made to recruit younger candidates in order to promote a longer career pathway within research, including healthcare disciplines.
In recent years, several specialist nursing and physiotherapy programmes have been converted to master’s degree programmes, and the prerequisites for building competence and recruiting younger researchers now exist if this opportunity is exploited (13).
The results we have achieved in the NNRHA correspond to the results described by the Western Norway Regional Health Authority where in the period 2009–2013, a total of NOK 8.5 million was allocated in strategic research funding to boost health research (14).
A summary of the research investment concludes that the funding has promoted regional research networks, increased research activity and production among health researchers, and not least has helped to boost more evidence-based health services in the Western Norway Regional Health Authority (14).
Competence enhancement and research improve hospitals
In order to build up and retain research competence, good candidates with master’s degree competence are of key importance in recruiting the best students to the PhD pathway.
It is challenging for clinics to set aside time and funding to educate healthcare staff to the master’s degree level, while there is a continuing need for clinical competence in practice.
Healthcare personnel gain knowledge of research through acquiring competence at master’s degree level. This can strengthen clinical practice in that they promote the use of research results in practice. According to Sirona’s (6) evaluation, linking research and clinical practice remains a challenge for the NNRHA.
Via the National Institute for Health Research, the UK health authorities have invested in enhancing RNs’ competence to master’s degree level by means of a dedicated clinical, academic study programme in the health trusts (15).
Through the programme, earmarked funding is allocated to competence enhancement at master’s degree level. In addition, clinical, academic positions have been created for experienced researchers. The programme enables RNs to increase their competence in research at the same time as they increase their clinical expertise.
Competence enhancement measures are justified by research evidence showing that health trusts that engage in research offer their patients better quality nursing and treatment (15–17). To ensure the recruitment of younger researchers, it is important to continue efforts to award PhD fellowships to new health researchers.
Other measures recommended include boosting the ability to write good research applications and building research networks to share competence. The objective of these measures is to increase the quality of projects and applications and the allocation of research funding to healthcare projects.
The questionnaire survey showed that health researchers and research fellows contributed to interdisciplinary research, with research in several disciplines and in a broad range of subject areas.
Research funding and research output
Even though there has been a positive development, mainly at UNN, health research competence is vulnerable. The allocation of research funding to health researchers apart from those at PhD level remains very modest.
Consequently, in the NNRHA’s research strategy for the period 2016–2020, investment in health research has been further strengthened with an annual post-doctoral fellowship, with the proviso that the applications merit support (18). Extensive clinical experience gives researchers fewer opportunities for an academic career pathway.
Short academic careers mean that fewer will become experienced researchers that establish large research projects or groups involving several research fellows and post-doctors. We therefore recommend continuing the NNRHA’s strategic investment in health research.
Conditions for health research in the health trusts
The median time set aside for research was 10 per cent, and 36 per cent of the health researchers had no time whatsoever for research. Research was mainly hindered by lack of time, funding, culture and facilitation.
A lack of time for research due to other work tasks corresponds with earlier reported findings on obstacles to research experienced by doctors and psychologists (10, 11).
On the basis of the feedback we received, possible measures in future strategic research investment may be as follows:
- make use of ordinary research funding
- continue the position(s) of health research manager(s)
- earmark funding for master’s degree, PhD and post-doctoral grants
- develop career pathways for health researchers in the health trusts
- provide a facilitating environment and shared office space for research fellows at the health trusts
- create additional positions by health trusts partnering with universities or university colleges
In order to retain competence in the health trusts, it seems important to develop career pathways for health researchers so that they can combine clinical work and research after completing a PhD degree to a greater extent than today. Positions combining clinical practice and research are most often the model followed by doctors and psychologists in the health trusts (10, 11).
In order to retain competence in the health trusts, it seems important to develop career pathways for health researchers.
On account of the anticipated need to replace staff in senior academic positions in the university sector in the coming years (13), it is essential for health trusts to offer attractive positions on competitive terms to avoid unintended competence drain.
Aamodt et al. found that the most common career aims of research fellows in nursing were either to have a senior academic position in nursing education or a combined clinical and research position in the specialist health service.
It was also common to want to continue a career as a post-doctor or researcher (13). Therefore, there is probably a basis for retaining health researchers in the health trusts if the conditions are right.
The health researchers and research fellows also sought infrastructure and support functions for research, for example office space, meeting rooms and a good environment, and statistics help. Such support functions were also mentioned in a survey of doctors and psychologists in 2001 and 2006 (10, 11).
The strengths and weaknesses of the study
Due to small-scale and transparent conditions in the NNRHA’s health trusts, we have a good overview of staff with a doctoral degree and the research fellows. A response rate of 71 per cent is regarded as satisfactory.
We cannot rule out that the restriction of the literature search to only the Pubmed and Cristin databases has meant that the number of published articles in the period has been underreported.
Conclusion
On the basis of the results, we can conclude that a positive development has taken place over time in the NNRHA, with a strengthening of health-related competence and research in most healthcare professions.
The NNRHA’s specific investment through a separate position for a health research manager and searchable research funding can therefore be described as successful.
Experiences from the NNRHA concur with the results achieved in the Western Norway Regional Health Authority, and indicate that a strategic investment in health research has a positive effect and can also be recommended for other health authorities.
Thanks to: Inger Sperstad, IT consultant at the clinical research department, UNN, Tromsø for compilation and distribution of the Questback questionnaire; Professor Ellen Blix, Oslo Metropolitan University and former health research manager in the NNRHA 2007–2014 for help with lists of names of relevant researchers in the NNRHA; Tove Klæboe Nilsen, head of research in the quality and research department, NNRHA, Bodø for input and discussion of the results.
Both authors had held or held the position of health research manager and health research supervisor respectively when the article was written. Consequently, both authors had an interest in the thematic area and the results. In our opinion, this has not influenced the results or our conclusions.
References
1. Kamper-Jørgensen F, Eriksson C, Starfield B, Ahlbom A, Andersen PK, Jensen UJ, et al. Evaluation of clinical, epidemiological, public health, health-related and psychological research in Norway. Public health and health services research – Panel 2. Oslo: Norges forskningsråd; 2004.
2. Universitetssykehuset Nord-Norge HF. Helsefaglig forskning ved Universitetssykehuset Nord-Norge HF. Forslag til plan. Tromsø; 2006.
3. Helse Vest RHF. Strategi for styrking av helsefaglig forskning i Helseregion Vest 2007–2010. Arbeidsgruppens rapport. Bergen; 2007. Available at: https://docplayer.me/820080-Strategi-for-styrking-av-helsefaglig-forskning-i-helseregion-vest-2007-2010-arbeidsgruppens-rapport.html (downloaded 15.05.2020).
4. Universitetssykehuset Nord-Norge HF. Forskningsstrategi Universitetssykehuset Nord-Norge 2008–2012. Tromsø; 2007.
5. Helse Nord RHF. Forskningsstrategi Helse Nord 2010–2013. Bodø; 2009.
6. Sirona Health Solutions. Evaluering av forskningssatsingen i Helse Nord RHF perioden 2002–2013. Sluttrapport. Stockholm: Sirona Health Solutions; 2015. Available at: https://docplayer.me/13088133-Evaluering-av-forskningssatsingen-i-helse-nord-rhf-perioden-2002-2013.html (downloaded 15.05.2020).
7. Helse Nord RHF. Årlig rapportering på forskning og innovasjon. Faglig rapportering. Hovedrapport forskningsaktivitet. Bodø: Helse Nord RHF; 2008–2015. Available at: https://helse-nord.no/forskning-og-innovasjon/arlig-rapportering-pa-forskning-og-innovasjon (downloaded 16.04.2019).
8. UiT Norges arktiske universitetet. Doktorgrader ved UiT Tromsø 2015. Available at: https://uit.no/om/enhet/artikkel?p_dimension_id=88199&p_document_id=256499 (downloaded 16.04.2019).
9. Polit DF, Hungler BP. Nursing research: principles and methods. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 1999.
10. Eriksen BO, Evensen E. Hvilke tiltak kan øke forskningsaktiviteten ved universitetssykehusene? Tidsskr Nor Legeforen. 2001;121:2960–3.
11. Eriksen BO, Evensen E. Endringer i forskningsaktiviteten ved Universitetssykehuset Nord-Norge. Norsk Epidemiologi. 2006;16(2):67–72.
12. Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
13. Aamodt PO, Nesje K, Olsen BM. Rekruttering til forskning i sykepleie: en kartlegging av rekrutteringsbehov, rekrutteringsgrunnlag og stipendiatenes karriereplaner. Oslo: NIFU; 2018. NIFU report; 2018:28.
14. Hope I, Frisk B, Myklebust H, eds. Helsefaglig forskning. Regional helsefaglig forskningssatsing i Helse Vest. Regional helsefaglig forskningssatsing i Helse Vest; 2013.
15. National Institute for Health Research. Building a research career. A guide for aspiring clinical academics (excluding doctors and dentists) and their managers. Leeds; n.d. Available at: https://www.clahrc-eoe.nihr.ac.uk/2016/02/building-a-research-career-a-guide-for-aspiring-clinical-academics-and-their-managers-from-the-nihr/ (downloaded 22.05.2020).
16. Ozdemir BA, Karthikesalingam A, Sinha S, Poloniecki JD, Hinchliffe RJ, Thompson MM, et al. Research activity and the association with mortality. PLoS One. 2015;10(2):e0118253.
17. Hanney S, Boaz A, Soper B, Jones T. Engagement in research: an innovative three-stage review of the benefits for health-care performance. Health Services and Delivery Research. 2013;1(8):2050–4349.
18. Helse Nord RHF. Strategi for forskning og innovasjon i Helse Nord 2016–2020. Bodø: Helse Nord RHF; 2016. Available at: https://helse-nord.no/Documents/Forskning/Strategi%20for%20forskning%20og%20innovasjon%202016-2020.pdf (downloaded 22.05.2020).













Comments