Native language nurses and second language nurses document information in patient records differently
Nurses with Norwegian as their mother tongue use a larger, and more nuanced repertoire in handover reports than those with Norwegian as a second language. However, they document numerical information in almost the same way.
Background: In recent decades, there has been an increase in the labour migration of nurses across country borders. Managers have a responsibility for ensuring that staff have the necessary language skills. We have not identified any studies that compare patient records written by nurses who are native language speakers with those written by second language nurses.
Objective: The objective of the study was to explore differences and similarities in the scope and linguistic precision of the handover reports of nurses who are native speakers and those of second language nurses.
Method: We used an exploratory design to assess 113 handover reports, of which 57 were written by 17 nurses with Norwegian as their mother tongue, and 56 were written by 17 nurses with a different mother tongue.
Results: Nurses who are native speakers for the most part documented more information than second language nurses. However, second language nurses documented almost as much numerical information as well as more information about family and relatives. The findings revealed that they had a smaller repertoire and lower linguistic precision.
Conclusion: Nurses who are native speakers and nurses who are second language speakers recorded almost the same amount of numerical information, but there were clear differences between the groups in respect of their language repertoire and register. The former use a larger and more nuanced repertoire than the latter. The study does not provide a basis for concluding that nurses who are native speakers record nursing information flawlessly, but it can help to initiate measures that may make patient record documentation easier for a growing group of nurses that Norway needs.
In this article, we direct our attention to patient record documentation carried out by nurses with Norwegian as their native language and nurses with Norwegian as a second language. Nurses must use clear and succinct language in patient record documentation in order to avoid misunderstandings and errors. Nurses who have been educated in countries other than Norway and nursing students with Norwegian as a second language may face linguistic challenges both during their education and in professional life (1, 2).
Students who pursue a programme of study in a country in which they must use a second language during their education often find that the transition from upper secondary school to nursing studies, for example, is linguistically challenging (1). Nurses using a second language may find the interaction with patients and colleagues challenging, and they may have a different interpretation of the role of the nurse (2).
Studies of patient record documentation
Studies that do not distinguish between native language nurses and second language nurses generally show that the quality of patient record documentation varies (3–5), and that the nurses find that formulating nursing plans is challenging (6). The quality of the patient record may be affected by fragmentary language (7), and the records may be incomplete with, for example, a lack of information about the effect of nursing measures (8).
A study from a German university hospital (9) pointed in part to considerable deficiencies in the patient records. The researchers revealed that there was a lack of correspondence between what was said in the oral report and what was documented in the patient record, and that there were errors in important information, or that this information was lacking altogether.
Advantages and disadvantages for second language nurses
International nurses and second language nursing students who follow a programme of nursing education in a different country may face linguistic, professional and culturally-related challenges. Canadian studies show that internationally trained nurses face challenges in using English as an academic language when they take further education and when they encounter unexpected formal requirements (10).
Various factors, either combined or singly, have a positive impact on nurses’ integration and professional practice. Factors such as financial resources, general language skills and work-related linguistic proficiency are highlighted (11).
An Australian study (12) shows that purposeful enhanced interaction with experienced nurses and with patients helps to improve the communicative skills of second language nurses and their interaction with patients and other nurses. In relation to linguistic adaptation, the study emphasises the importance of how the nurse sees him/herself and how well-prepared he/she is before working in another country. Their manner of communication affects the expectations of patients and other healthcare personnel towards them.
Publications that identify problems linked to communication with second language nurses apparently use the term ‘language’ only in connection with oral communication (2, 13). Written documentation is not discussed even though it has a legal significance which does not apply to oral communication (14).
The objective of the study
In our article, we focus on the fully trained nurse who has completed a course of professional education and who satisfies language requirements. We have not found studies that examine linguistic similarities and differences between documentation recorded by native language nurses and second language nurses, either in Norway or internationally.
The absence of such studies is surprising considering that in some countries, a relatively large proportion of nurses do not speak the country’s official language as their mother tongue. Currently, over 10 per cent of 100 000 nurses, midwives and public health nurses in Norway do not come from Norway originally (15).
In order to ensure quality and continuity, an adequate, relevant, precise and comprehensible language repertoire, that allows for the inclusion of the patient’s views, is essential (16). The aim of the pilot study was to explore differences and similarities in scope and linguistic precision between the handover reports of native language nurses and second language nurses.
Method
We employed an exploratory approach to examine the nurses’ language skills. We identified their linguistic register and use of grammatical structures.
Setting and sample
Handover reports must help to ensure continuity and teamwork around the patient (4, 14). The charge nurses in four wards collected written, anonymised reports from day shifts at a large hospital in the eastern part of southern Norway. Reports from day shifts are normally more comprehensive than reports from evening and night shifts.
In the hospital’s electronic documentation system, handover reports are referred to as ‘Note/evaluation’, hereinafter referred to as ‘reports’. The inclusion criteria were that the nurses should have Norwegian as their mother tongue or Norwegian as their second language. They could not have any other Scandinavian language as their mother tongue, be permanent employees or have no higher education.
The managers also gathered information about how long the nurses had been employed in Norway, and where they had taken their final nursing examination.
Data collection
A member of hospital management contacted five clinic heads and requested permission to carry out the study. Four agreed to participate and arranged for a contact person for the individual ward. The contact persons received further written and oral information from the first author about the objective of the project and the mode of procedure.
The contact persons obtained written consent from the nurses allowing them to collect the reports the nurses had written and use them in the project. Prior to giving consent, the nurses had received written information about the objective of the project and how the results were to be used. The charge nurse of each individual ward anonymised people and patient-identifying information.
We collected ward reports between June 2015 and January 2016. We sought to ensure that none of the reports covered periods when there are frequently a number of agency nurses on duty or double shifts, such as Christmas, Easter and the summer holidays. We chose the same shift and omitted defined periods in order to prevent imbalances between the two groups of nurses.
Altogether we collected 129 reports written by 20 nurses who were native speakers and 20 nurses who were second language speakers. The material we received from the charge nurses turned out to include reports from evening and night shifts. These reports were removed from the material that finally consisted of reports written by 17 nurses who were native speakers and 17 nurses who were second language speakers, representing 57 and 56 reports respectively.
Ten of the nurses who were second language speakers were educated as nurses in Norway, while the other seven had nursing education from other countries. The majority of nurses who were native speakers had worked from one to three years as nurses. Second language speakers had longer professional experience on average. The majority had worked in a permanent position from two to fifteen years.
For reasons of anonymisation, we do not present the results by ward or place of education, i.e. whether the place of education was in Norway or elsewhere.
Analysis
First we carried out an analysis in order to identify categories across twelve functional areas that the nurses were expected to use in the reports:
- Communication and senses
- Knowledge, development or mental health challenges
- Respiration and circulation
- Nutrition, fluid and electrolyte balance
- Elimination
- Skin, tissue and wounds
- Activity and functional status
- Pain, sleep, rest and well-being
- Sexuality and reproduction
- Social needs
- Spiritual and cultural needs, and lifestyle challenges
- Miscellaneous, doctor-delegated activities and observations
In this phase, we first organised the material on the basis of official expectations regarding patient record documentation (14). Then we used text condensation based on a grounded theory approach (17).
This resulted in the following six cross-cutting categories: 1) Nurse’s assessments and nursing diagnoses, 2) Nurse’s measures and actions, 3) Communication between patient and nurse, 4) Cooperation and communication with other healthcare personnel, 5) Notes that related to family, relatives and friends, and 6) Number-related information units such as blood pressure, fever, degree of pain and time.
In order to facilitate a comparison of the two groups of nurses, we summarised the number of times each nurse recorded information in each category, and then calculated the average number of information units per report. For example, nurses who were native speakers recorded 108 cases of ‘Communication between patient and nurse’ in the 57 reports. We calculate this as an average of 1.9 per report. The group of nurses who recorded most information in each category was set at 100 per cent, making it possible to show the relative difference between native speakers of Norwegian and speakers of Norwegian as a second language.
In-depth analysis of skin, tissue and wounds
Hospital patients are vulnerable to infections (18) and wounds (19). Both professional and linguistic competence is needed to be able to express precisely how a wound appears along a timeline, i.e. the past and present state of the wound, what action has been taken in the preceding shift(s), and also reference to any follow-up that is necessary in the ensuing shift(s).
Consequently, we conducted an in-depth analysis of the functional area ‘Skin, tissue and wounds’ in order to examine the linguistic level of precision through the use of nuanced language. We investigated expressions used to describe variation in different assessments, measures and actions, descriptions of time and changes as well as communication and cooperation.
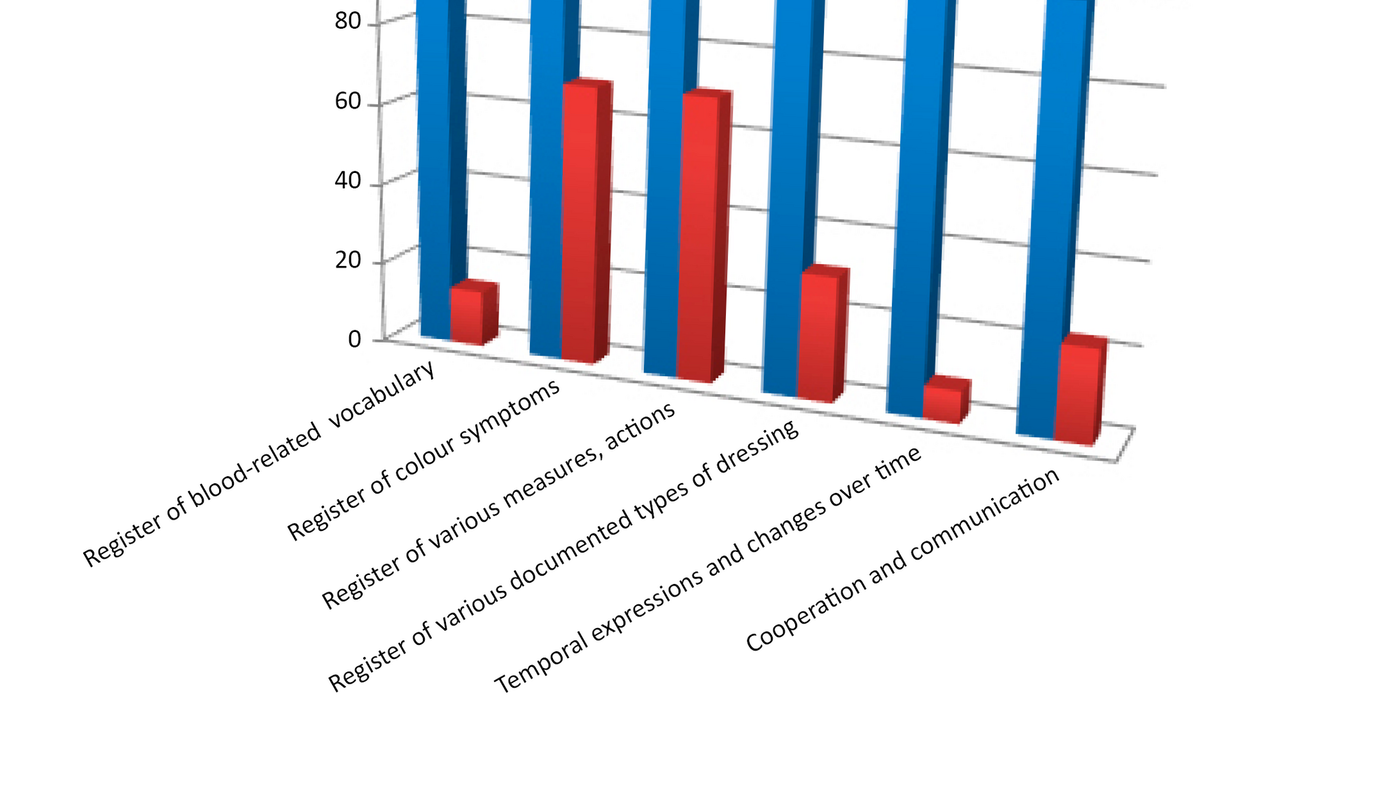
We decided to compare the patient record documentation of the two groups of nurses based on: 1) Register of blood-related vocabulary, 2) Register of colour symptoms ranging from light to dark, 3) Register of various documented measures or actions, 4) Register of various documented types of dressings, 5) Terms expressing condition of patient and changes over time, and 6) Cooperation and communication with other healthcare personnel and the patient.
Category 6 was included since cooperation and communication are intended to strengthen the quality of patient follow-up as well as including one-way communication in the form of direct messages to the next shift.
Ethics
The project was quality assured and was assessed and approved by the hospital’s data protection official for research. The nurses consented to our use of the reports they had written in the analysis. They had removed all patient-identifying information from the reports we received.
We informed the nurses that it would not be possible to identify individual wards in publications. The same applied to individual nurses and groups of nurses as well as to their national or cultural background.
Results
A main finding is that native language nurses record more information than second language nurses in the following categories: ‘Nurse’s assessments and nursing diagnoses’, ‘Nurse’s measures and actions’, ‘Communication between patient and nurse’, and ‘Interaction with other healthcare personnel’.
Second language speakers recorded more information in the ‘Family, relatives and friends’ category than native speakers. In the ‘Number-related information units’ category, native speakers documented slightly more. Table 1 shows the differences in the scope of the information with examples of how the two groups of nurses record patient information.
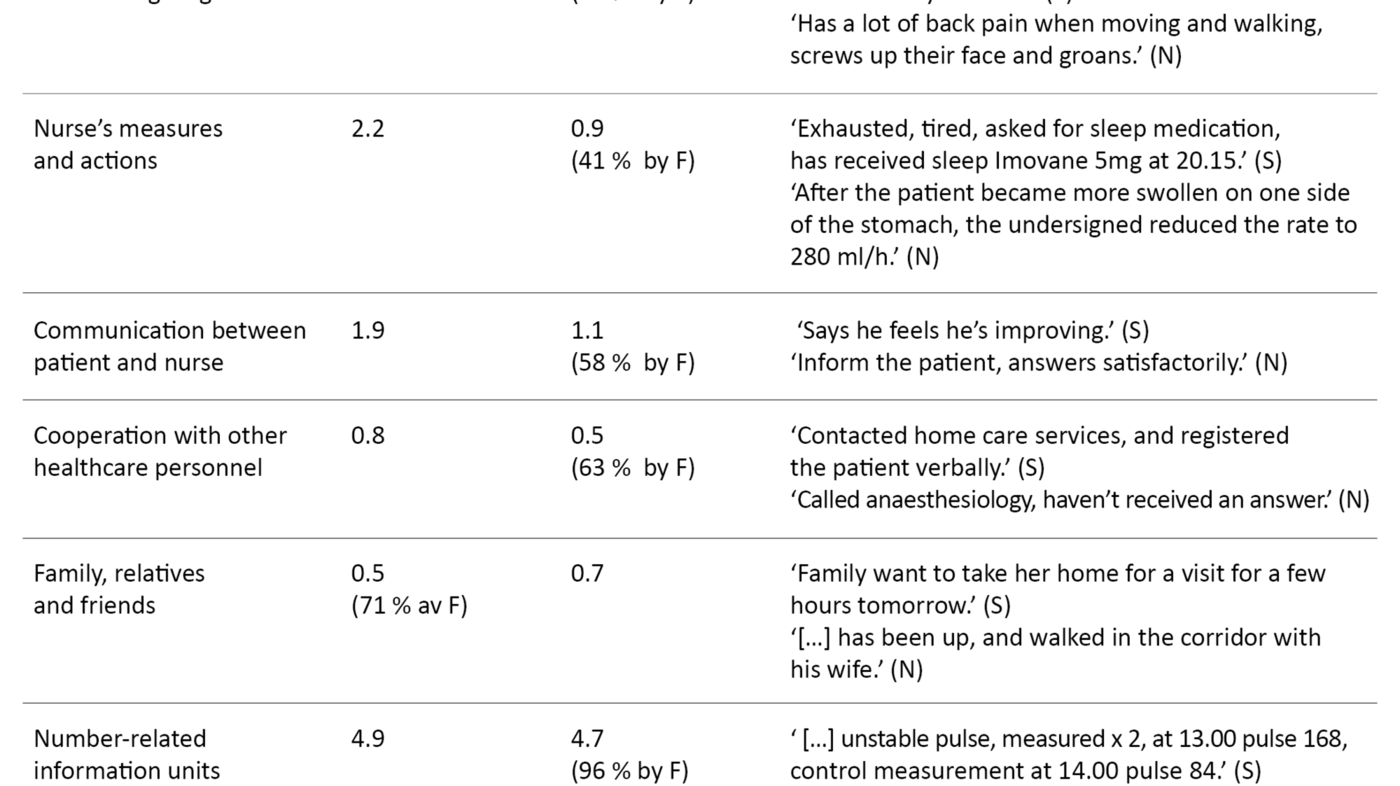
Figure 1 shows the relative difference in the scope of the main categories between the two groups’ patient record documentation.

Second language speakers have lower linguistic precision
In a detailed analysis of linguistic precision, we found that second language speakers recorded information in 37 out of the 56 reports (66 per cent), but that native language speakers had provided documentation in 51 out of the 57 (89 per cent). Second language speakers have less linguistic precision with fewer nuances. This is, for instance, revealed when they document observations of wound care and change of dressing. Native speakers use a register of ten different words related to observation of dressings, while we identified only one description among second language speakers.
Table 2 shows differences in nuances and specificity in the documentation. There are also differences between the two groups when describing symptoms using colour and nuanced conditions – native speakers use twice as many descriptions. The register of different measures and actions shows that native language speakers use twice as many descriptions – altogether twelve as opposed to six for second language speakers.
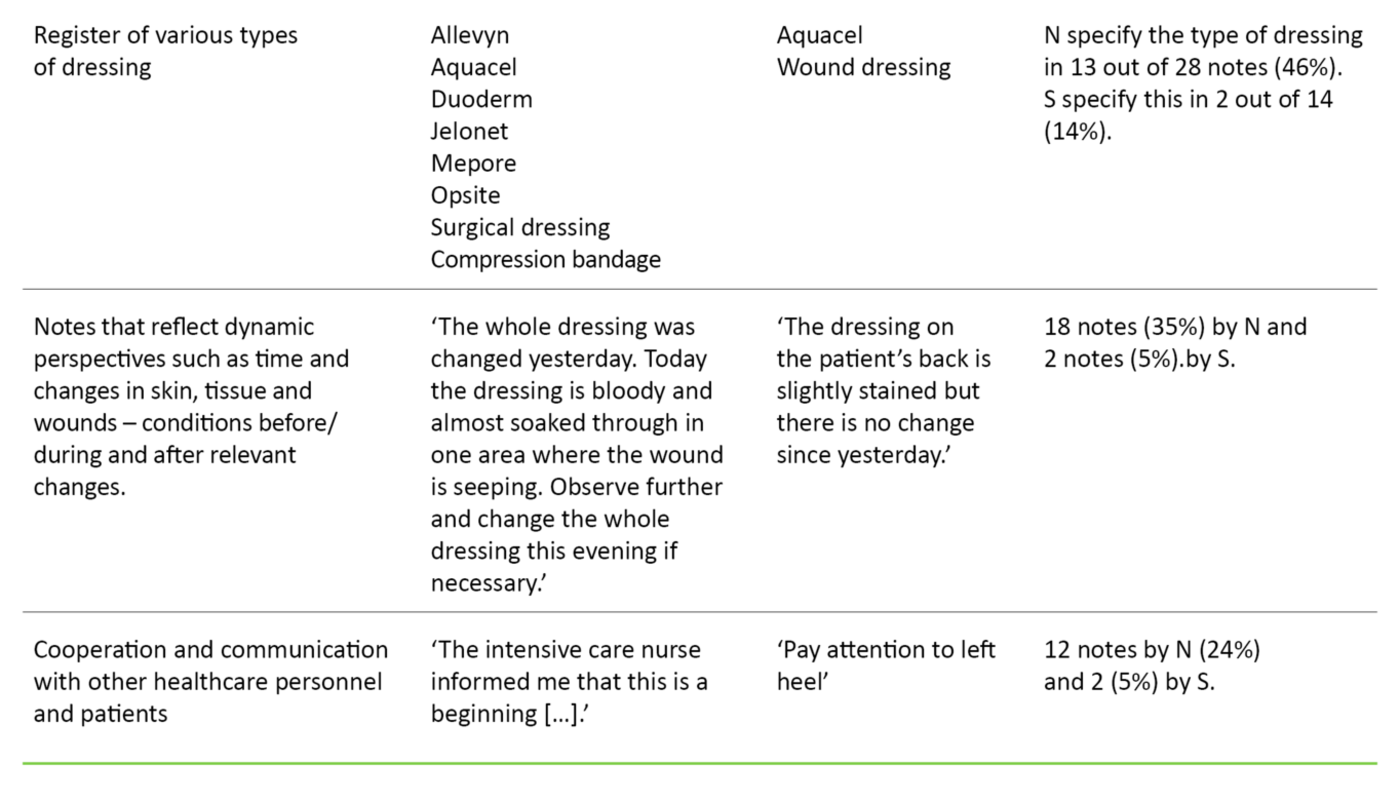
Nurses who are native language speakers document cooperation to a greater extent
The type of dressing gives additional information about the wound and the treatment given. Second language speakers specify this in two out of 14 notes that include dressings, in contrast to 13 out of 28 notes made by native speakers. The notes of the former reflect to a minimal degree the change and development aspect that is critical to the skin, tissue and wound category, for example the condition of the skin or the wound during the previous shift and the type of change prior to the shift in question.
Native language speakers document far more on cooperation and communication with other healthcare personnel and with patients. We identified twelve notes with documentation of various forms of communication and cooperation. In contrast, second language speakers had two notes in this category and both were direct requests to future shifts and did not concern communication with patients.
Figure 2 shows graphically the difference in register of the two groups of nurses’ descriptions and actions.
Discussion
A main finding is that nurses who are native speakers and nurses who are second language speakers record information to a different degree, and the linguistic precision differs. In four out of six categories, the latter document less than the former. In one category, second language speakers document more, and in one category the amount of documentation is relatively similar.
The detailed analysis of skin, tissue and wounds shows that native language nurses consistently use more detailed and more nuanced language in all categories.
However, the findings also reveal that the documentation of native language nurses can also be deficient, as other studies have also shown (20). Competence and cultural circumstances that are significant for how second language speakers regard their roles and responsibilities may explain some of the differences we uncovered (2).
Second language speakers have a narrower linguistic register
Nurses who are second language speakers have a narrower linguistic register when it comes to using nouns, adjectives and verbs in their descriptions of symptoms and actions. They include little information from before or after the shift on which they report.
There is a comprehensive body of research on second languages, i.e. learning, acquisition and application. This is not uniform, but it confirms that developing a richer linguistic register in terms of mastering good oral and written communication is a process that takes many years (21).
Henriksen (22) refers to such differences between the language acquisition and learning of native and non-native speakers, and provides an explanation. When learning a second language, a number of people can function well after a short time when using everyday language, but it can take several years to acquire a functional, professional language. These experiences also tally with the experiences of nurses in Norway who are second language speakers (2).
Refer to time differently
We revealed differences when it came to expressing time factors, sequence and changes in the condition of skin, tissue and wounds. There may be various reasons for the differences. They may be associated with the fact that second language nurses record less information than native language nurses, and therefore refer less to time-related factors.
Another possibility is that the differences may be linked to professional competence, but they may also be connected to the linguistic background of the nurse. The tense of a verb depends on whether it refers to something which has happened or something which is happening now, whether it describes an actual condition or is something the nurse must take into account in the future – for example during the next shift.
The recording of information that concerns the current shift largely requires verbs in the present simple, present perfect or past simple tenses, i.e. ‘eats’, ‘has eaten’ or ‘ate’ respectively, and adverbs of time such as ‘this morning’ and ‘12 noon’ and the like. Notes intended for the next nurse on duty make it natural for the reporting nurse to express the future using verbs such as ‘shall’, ‘can’, ‘must’ and ‘should’, and expressions of time such as ‘this evening’ or ‘next week’.
Notes that refer to the preceding shift require the nurse to use past forms such as the past simple ‘ate’ or the past perfect tense to show that something happened before something else, for example, ‘had just eaten when he felt pain’. The verb tense used in this example was previously referred to as the pluperfect. Even foreign languages that are closely related to Norwegian, such as English, German, French and Spanish, express the past fairly differently.
Languages such as Vietnamese and Chinese (Mandarin) do not express the past by means of different verb endings like Norwegian ( åpner – åpnet/åpna) or changes in the vowel ( stå – sto), but use time markers, for example ‘this morning’ and ‘during the visit’ (23). Such language differences can explain some of the findings. Therefore, the linguistic challenges we have revealed may vary according to the native language of the nurse, or where he/she completed their nursing education.
The fact that Norwegian is a foreign language not spoken by many people may make a difference for nurses who have probably learned it as adults. They have been exposed to Norwegian for a far shorter length of time and to a lesser degree than to world languages such as English and Spanish. This may lead to considerable challenges in communication with patients and in interaction with other healthcare personnel. However, on the basis of the findings in the study, we have no evidence to comment on such challenges.
The employer is responsible for the training
We cannot draw conclusions as to whether there is any correlation between language skills and possible deficiencies in the direct treatment and follow-up of patients. The objective of the study has not been of a normative character – i.e. meant to evaluate whether one group of nurses is better than the other. We have focused on describing linguistic similarities and differences.
There may be reason to reflect on the findings in a broader cultural context, with information culture in the foreground (16). Precision in descriptions and a smaller register of words and expressions to describe professional assessments, actions and measures may then be significant.
Regardless of the reason for these linguistic challenges, the employer has a duty to ascertain that the language skills of second-language speakers are on a level that ensures that they can record information accurately and succinctly so that nursing services are sound (24).
Developing nursing terminology
International efforts have been made to develop terminology for use in nurses’ patient record documentation, which may alleviate some of the challenges (25, 26). Efforts are being made nationally to develop and introduce nursing terminology, and the Norwegian Directorate of eHealth recommends the use of the ICNP (International Classification for Nursing Practice). When the nurses used specialist terminology, the content was more complete (27).
However, nursing diagnoses can be seen as enriching, linguistic constructions (6). Therefore, we need studies that address whether the use of specialist terminology helps to support nurses who are second language speakers.
Limitations of the study
The study has several limitations. We do not know if the differences are caused by language proficiency alone or by nursing competence and cultural background in addition (1). More knowledge is needed about the actual quality of patient record documentation through more comprehensive and robust studies. An interview survey giving more in-depth insight is also recommended.
Our study builds on a limited number of handover reports. Since we found no previous studies on this topic, we used a method that enabled us to compare the scope and linguistic nuances of the two groups. The fact that we analysed the material across functional areas is a strength because it gives a deeper understanding of the nuances.
Ten of the second-language speakers had completed their nursing education in Norway while the remaining seven were educated in other countries. We found small differences when comparing these groups so we chose to include them in the same group. However, the findings must be seen in light of the fact that we were unable to control for the characteristics of the informants. The body of material was too small.
The findings must also be considered in light of the fact that we have no information about how many patients were represented in the reports. In addition, we had to take ethical considerations into account. Since the number of informants in the sample is small, we cannot state the country of origin of nurses with Norwegian as a second language due to anonymity requirements.
The fact that nurses who are second language speakers have a smaller vocabulary in writing does not mean that we can draw conclusions about the quality of their direct patient care or their competence as nurses. We do not know whether there was an oral information transfer between the shifts and whether this helps to compensate for deficiencies in written information. However, an oral report does not necessarily solve all the language challenges (9).
Nor do we know whether the participants in this study felt pressurised to participate. If cultural factors indicate that they feel inferior (2), this may mean that our group is not representative. Furthermore, we have no information about the content or quality of the reports written by the nurses who chose not to participate, and this may affect the results.
Conclusion
Native language nurses and second language nurses record almost the same amount of numerical information but there are clear differences between the groups in terms of their language repertoire and register. Nurses who are native speakers use a larger and more nuanced repertoire than those who are second language speakers. The study does not provide a basis for concluding that nurses who are native speakers record nursing information flawlessly.
The study should be followed up by a larger and more broadly based study in the specialist and primary health services and in the education sector. It is a managerial responsibility to ensure that employees receive language and professional follow up to prevent risk to patients. The study can help to implement relevant measures that may make patient record documentation easier for a growing group of nurses that Norway needs.
Thanks to quality assurance staff at the hospital for their help in the implementation of the project, and to Else Ryen for vital input in the final phase.
Lasse Morten Johannesen died before the article was published. The article is published in agreement with his family.
References
1. Jonsmoen K, Greek M. Studenter med norsk som andrespråk mangler nødvendige språkferdigheter. Sykepleien. 2018;106(72471)(e-72471). DOI: 10.4220/Sykepleiens.2018.72471.
2. Dahl K, Dahlen KJ, Larsen K, Lohne V. Conscientious and proud but challenged as a stranger: Immigrant nurses’ perceptions and descriptions of the Norwegian healthcare system. Nordic Journal of Nursing Research. 2017;37(3):143–150.
3. Ehrenberg A, Ehnfors M, Smedby B. Auditing nursing content in patient records. Scand J Caring Sci. 2001;15(2):133–41.
4. Gjevjon ER, Hellesø R. The quality of home care nurses' documentation in new electronic patient records. J Clin Nurs. 2009;19(1–2):100–8.
5. Saranto K, Kinnunen UM, Kivekas E, Lappalainen AM, Liljamo P, Rajalahti E, et al. Impacts of structuring nursing records: a systematic review. Scand J Caring Sci. 2014;28(4):629–47.
6. Nöst TH, Blekken LE, Andre B. Nurses’ experiences with introduction of nursing diagnoses. Nordisk tidsskrift for helseforskning. 2015;11(1):89–103.
7. Jefferies D, Johnson M, Nicholls D. Nursing documentation: how meaning is obscured by fragmentary language. Nurs Outlook. 2011;59(6):e6–e12.
8. Jefferies D, Johnson M, Nicholls D, Langdon R, Lad S. Evaluating an intensive ward-based writing coach programme to improve nursing documentation: lessons learned. Int Nurs Rev. 2012;59(3):394–401.
9. Lauterbach A. … da ist nichts, ausser dass das zweite Programm nicht geht Dienstübergaben in der Pflege. ff. 204–24 Reihe Pflegewissenschaft Norderstedt, Books on Demand GmbH; 2008. ISBN: 9-783-8370-43556.
10. Covell CL, Neiterman E, Bourgeault IL. Scoping review about the professional integration of internationally educated health professionals. Human resources for health. 2016;14(1):38.
11. Lum L, Dowedoff P, Bradley P, Kerekes J, Valeo A. Challenges in oral communication for internationally educated nurses. J Transcult Nurs. 2015;26(1):83–91.
12. Philip S, Woodward-Kron R, Manias E, Noronha M. Overseas Qualified Nurses (OQNs) perspectives and experiences of intraprofessional and nurse-patient communication through a Community of Practice lens. Collegian. The Australian Journal of Nursing Practice, Scholarship & Research. 2019;26(1):86–94. DOI: 10.1016/j.colegn.2018.04.002.
13. Norsk Sykepleierforbund. Språkproblemer truer pasientsikkerheten, 2015. Available at: https://www.nsf.no/vis-artikkel/2354192/539355/Spraakproblemer-truer-pasientsikkerheten(downloaded 05.01.2018).
14. Ot.prp. nr. 13 (1998–99). Om lov om helsepersonell mv. Oslo: Sosial- og Helsedepartementet; 1998.
15. Statistisk sentralbyrå. Innvandrere og ikke-bosatte 15–74 år med helse- og sosialfaglig utdanning sysselsatt i helse- og sosialtjenester, etter landbakgrunn, 2015. Available at: https://www.ssb.no/270655/innvandrere-og-ikke-bosatte-15-74-ar-med-helse-og-sosialfaglig-utdanning-sysselsatt-i-helse-og-sosialtjenester-etter-landbakgrunn.per-4.kvartal.prosent-endring-siste-ar(downloaded 07.05.2018).
16. Jylha V, Mikkonen S, Saranto K, Bates DW. The impact of information culture on patient safety outcomes. Development of a structural equation model. Methods Inf Med. 2017;56(Open):e30–e38.
17. Malterud K. Shared understanding of the qualitative research process. Guidelines for the medical researcher. Fam Pract. 1993;10(2):201–6.
18. Helsedirektoratet. Meldeordningen for uønskede hendelser i spesialisthelsetjenesten. Oslo, Helsedirektoratet; 2016. Available at: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/1365/%C3%85rsrapport%202016%20meldeordningen%20for%20u%C3%B8nskede%20hendelser%20i%20spesialisthelsetjenesten.pdf(downloaded 20.01.2018).
19. Knudsen CW, Tonseth KA. Pressure ulcers – prophylaxis and treatment. Tidsskr Nor Laegeforen. 2011;131(5):464–7.
20. Wang N, Yu P, Hailey D. The quality of paper-based versus electronic nursing care plan in Australian aged care homes: A documentation audit study. Int J Med Inform. 2015;84(8):561–9.
21. Chenu F, Jisa H. Reviewing some similarities and differences in L1 and L2 lexical development. Aile Acquisition et interaction en langue étrangère. 2009;1:17–38. Available at: https://journals.openedition.org/aile/4506(downloaded 15.04.2018).
22. Henriksen B. Research on L2 learners' collocational competence and development – a progress report. In: Bardel C, Lindqvist C, Lauffer B, eds. L2 vocabulary acqusition, knowledge and use – new perspectives on assessment and corpus analysis 2: Eurosla Monographs series. Italia: University of Modena and Reggio Emilia; 2013. p. 11–29.
23. Chan L. Tense-aspect processing in second language learners. Pittsburgh, Pennsylvania, Faculty of the Dietrich School of Arts and Sciences, University of Pittsburgh; 2012.
24. Statens helsetilsyn. Arbeidsgiver har ansvar for å ansette helsepersonell med språkferdigheter [internet]. Oslo: Statens helsetilsyn; 2015. [updated 23.01.2015, cited 20.01.2018]. Available at: https://www.helsetilsynet.no/presse/nyhetsarkiv/2015/arbeidsgiver-har-ansvar-for-a-ansette-helsepersonell-med-sprakferdigheter/.
25. Hardiker N. Harmonising ICNP and SNOMED CT: A model for effective collaboration. Stud Health Technol Inform. 2016;225:744–5.
26. Hardiker NR, ed. Developing standardized terminologies in nursing informatics. Sudbury, MA: Jones and Bartlett Publisher; 2009.
27. Thoroddsen A, Ehnfors M, Ehrenberg A. Content and completeness of care plans after implementation of standardized nursing terminologies and computerized records. Computers, Informatics, Nursing: CIN. 2011;29(10):599–607.










Comments