Self-evaluation of competence by nurses working offshore
Today, nurses working in the offshore industry include staff who have specialised in intensive care or anaesthetic nursing as well as staff with no particular specialty. Are there differences between their own perceived competence levels?
Background: Nurses who work in the offshore oil and gas industry are usually the only medical staff aboard an installation, which means they are responsible for the medical emergency response. Following a sharp reduction in the number of offshore accidents in the 1980s, the authorities decided to drop the requirement for offshore nurses to have specialised in anaesthetic or intensive care.
Objective: The objective was to investigate how offshore nurses from different backgrounds in terms of education and past work experience evaluate their own competencies in examining, assessing and treating patients.
Method: We drew up a questionnaire designed to establish how offshore nurses evaluate their own level of competence with respect to nursing care, medical assessment and treatment, technical skills, teamworking, decision-making and improvisation, teaching skills and professional development.
Results: A total of 66 offshore nurses took part in the survey. No significant difference was found between specialist anaesthetic nurses, intensive care nurses and nurses with no nursing specialty.
Conclusion: Despite substantial differences in the respondents’ educational backgrounds and work histories, the study found no differences between their self-reported overall competence levels.
Nurses who work in the Norwegian offshore industry are responsible for examining, diagnosing and treating ill and injured patients (1). On most offshore installations, nurses are the only medical staff. Formerly, Norwegian authorities required this group of personnel to have specialised in anaesthetic nursing or intensive care nursing (2). The authorities dropped this requirement in the 1980s after the introduction of stricter health and safety rules, which led to a sharp reduction in the number of accidents involving personal injuries (3).
Norwegian authorities have not investigated whether the changes they introduced to the professional requirements have brought about any changes to the medical emergency response capability on the Norwegian continental shelf, but the Framework Regulations require all offshore health services to be of a high standard (4). This study examines how nurses who work in the offshore industry evaluate their own competence and capability to undertake the activities requested of them on an offshore installation.
We found a number of articles that provided data from patient evacuations in the Norwegian and British sectors (5–7), but we were unable to find studies that looked into the offshore nurses’ autonomous assessments, their treatment results or patient satisfaction. The literature searches were carried out in Norwegian as well as English texts. They included words such as “nurse offshore”, “medic offshore”, “HSE coordinator”, “medevac”, “medical evacuation”, “offshore health”, “offshore competence” and “nursing competence”.
Dissimilar competence requirements
To ensure that the medical emergency response capability holds a consistently high standard, nurses are required to attend mandatory courses in emergency medicine. Courses in medical examination techniques and the follow-up of other diseases and conditions are however not covered by a similar ruling. There has been an increase in the rate of acute medical conditions caused by age and lifestyle related health problems (8) and this is now the most common reason for requisitioning a helicopter to take patients ashore. Some oil companies still prefer specialist nurses who have been trained to provide anaesthetic or intensive care (9). Other oil companies employ nurses without any advanced specialist training and whose experience of clinical and emergency medicine is limited, despite the fact that the petroleum industry’s collective wage agreements (10) ensure that all nurses receive the same rate of pay as the specialist nurses.
“Competence” is this study’s key concept. Cowan et al. (11) investigated how competence has been defined in the nursing sector. They emphasised that a holistic definition, covering knowledge, performance, practical skills and attitudes, was required in order to embrace the full complexity of nursing. Nurses need to be able to transfer knowledge, make thorough assessments and adjust their skills to unexpected and unfamiliar situations (11).
Eraut (12) describes the development of competence as a gradual process: Knowledge and theories are put into a system of standards for each discipline. They are then further developed into general principles, which in turn form the basis for knowledge about procedures and guidelines. He describes the last step as a cognitive process that involves planning, problem solving, analysis, evaluation and decision-making. This last step cannot be achieved by simply following procedures because it requires a robust knowledge base, retrieval of information, recognition of patterns and quick interpretation of data (12). Eraut maintains that experts make decisions intuitively rather than analytically, and that this requires considerable experience. It is generally accepted that competence, as a concept, means to be qualified to do a job, for instance after completing professional training. Expertise, however, is required to deal with the unexpected. (12).
In order to examine how nurses working in the offshore industry evaluate their own capability to examine, diagnose and treat patients, we drew up the following research questions:
- Do specialist anaesthetic and intensive care nurses assess their competence to be different to the competence of nurses with another specialty or with no advanced specialist training?
- What is the correlation between self-reported competence and past work experience?
- What type of competence do the nurses report that they need most in order to carry out their work?
Method
Design
In order to reach the greatest possible number of nurses we decided on a sample survey design (13). The method is based on information obtained through standardised questions and can be used to gather quantitative data from large groups of people. A self-administered questionnaire with predefined response alternatives is well suited to collect data without the researcher exerting an influence on participants (14). The challenge is to formulate questions that are unambiguous, and response alternatives that reflect the area being investigated (15).
Competence can be investigated in several different ways. According to a systematic literature study that charts instruments used to measure competence, all such instruments include a form of self-evaluation, some of them in combination with other methods such as practice observation, interviews or manager evaluation (15). For reasons of distance and cost we decided to use an online questionnaire.
Drawing up the questionnaire
We drew up a two-part questionnaire. Part 1 was based on a questionnaire developed by Valeberg, Grønseth and Fagermoen (16). Their questionnaire was made for the purpose of studying the perceived competence of specialist nurses on completion of their specialist training. This questionnaire included questions relating to seven different areas of competence: nursing care, medical skills, technical skills, teamworking, teaching skills and professional development, decision-making and improvisation, and liaison with relatives. We adjusted our questions to the most commonplace offshore patient scenarios, excluding liaison with relatives, as this responsibility lies with the oil companies’ onshore management.
Medical competence was split into two skills areas: “Medical treatment” included questions about medication and the ability to make autonomous decisions about initiating treatment, while “medical assessment” included questions concerning anamnesis and examination as a basis for the nurses’ diagnoses. The other areas of competence were adjusted to the nurses’ role as the only health care staff aboard the installation and therefore the leader of the medical emergency response.
The competence part of the questionnaire included 44 questions. The nurses were asked to evaluate themselves on a Likert scale (13) from 1–10 (1 = considerable gap between own competence and the competence required to do the job, 10 = meets the competence requirements for the relevant area in a fully satisfactory way).
Part 2 of the questionnaire consisted of questions concerning age, gender, specialist training, past work experience, and the duration of employment at up to three different places of work. The alternative responses with respect to advanced specialist training were anaesthetic nursing, intensive care nursing, theatre nursing, emergency care nursing, other advanced specialist training and paramedic training (for ambulance crews) (17). The nurses were also asked to indicate what type of clinical experience they felt was the most relevant when they started working offshore. The greater the number of relevant explanatory variables, the stronger a study that investigates correlations is considered to be (13).
Three nurses with different offshore histories took part in a pilot study in order to strengthen the validity of the questionnaire’s content. They were each asked to submit comments in writing on the design of the questionnaire, the phrasing of the questions and their relevance with respect to the areas of competence. Based on their feedback, we added further questions under “medical treatment” associated with acutely ill and seriously injured patients. This was done to reflect the fact that an ability to provide emergency medical care is a requirement relating to the nurses’ emergency medical response provision offshore (4, 18). We also added further questions concerning common offshore health problems, such as skin rashes, eye injuries, ear, nose and throat problems, respiratory problems, musculoskeletal complaints (19).
Under the heading of “Medical assessment” we included questions about infectious diseases, ECG interpretation, neurological examination and the ability to carry out the examinations referred to in the Norwegian Electronic Medical Handbook(NEL) (20). The three nurses completed the questionnaire again, after which some of the questions were rephrased. The nurses felt that the website login procedure and the questionnaire format were satisfactory.
Data collection
We tried to recruit all nurses working in the Norwegian petroleum industry. Twenty oil companies and crewing agents that provide nurses for offshore work, were contacted by email or telephone. The sixteen companies that agreed to assist with the recruitment employed a total of 261 nurses offshore. For this study, we used an online form that had been developed at the University of Oslo. This required the questionnaire and the login and password details to be sent electronically to the informants’ email addresses. The various oil companies operated with different internal standards with respect to handing out the email addresses of employees. Some made their email lists available, while others chose to have their HSE manager, company doctor or coordinator forward the information letter and invitation to the nurses. Those who wished to take part subsequently contacted us direct by email and gave their consent, after which they were sent the form and login details electronically.
We collected data in the period between November 2013 and March 2014. We issued two reminders – after four weeks and then again after eight weeks. The responses were recorded in a closed database. Data were electronically transferred to SPSS following closed inclusion. The study has been approved by the Data Protection Official at the Norwegian Centre for Research Data (NSD). The participants’ email addresses have since been deleted, and the data have been anonymised.
Analysis
All data were transferred electronically to IBM SPSS Statistics 22, which was the software used for our analyses. All education and past work experience data were summarised in groups and analysed by means of descriptive statistics: frequencies, percentages, mean scores and standard deviations. When an analysis involves several independent variables, we need to carry out multiple comparisons. We conducted an analysis of variance (one-way ANOVA) to establish whether there were significant differences between the distribution of responses within each group and between groups. We also used one-way ANOVA to study the effect of several factors at the same time.
Levene’s test is included in the SPSS analysis and is used to test the null hypothesis that there is homogeneity of variance, so that the groups are statistically comparable. The significance testing was corrected using the Bonferroni and T2 methods in order to avoid any type 1 errors that would lead to incorrect rejection of the null hypothesis. The significance value was set to p <0.05.
We recoded the respondents into three educational groups: The first two groups consisted of anaesthetic nurses and intensive care nurses. Anaesthetic nurses who had also specialised in intensive care nursing, were nevertheless categorised as anaesthetic nurses because prehospital acute medical services are defined as the remit of anaesthetic nurses (21). The remaining educational groups were too small to warrant separate analyses; they were therefore combined into a single educational group.
We recoded age and experience into three groups of near-equal size. We recoded clinical experience into little experience (≤8 years), moderate experience (9–14 years) and long experience (≥15 years). Offshore experience was recoded into little experience (≤4 years), moderate (5–14 years) and long experience (≥15 years). Age was recoded into youngest (≤44 years), middling (45–53 years) and oldest (≥54 years).
Results
A total of 89 nurses reported that they wanted to take part, but only 66 completed the questionnaire, which gave a take-up rate of 25.3 per cent of the 261 nurses working offshore. Table 1 presents the sample’s demographic data.
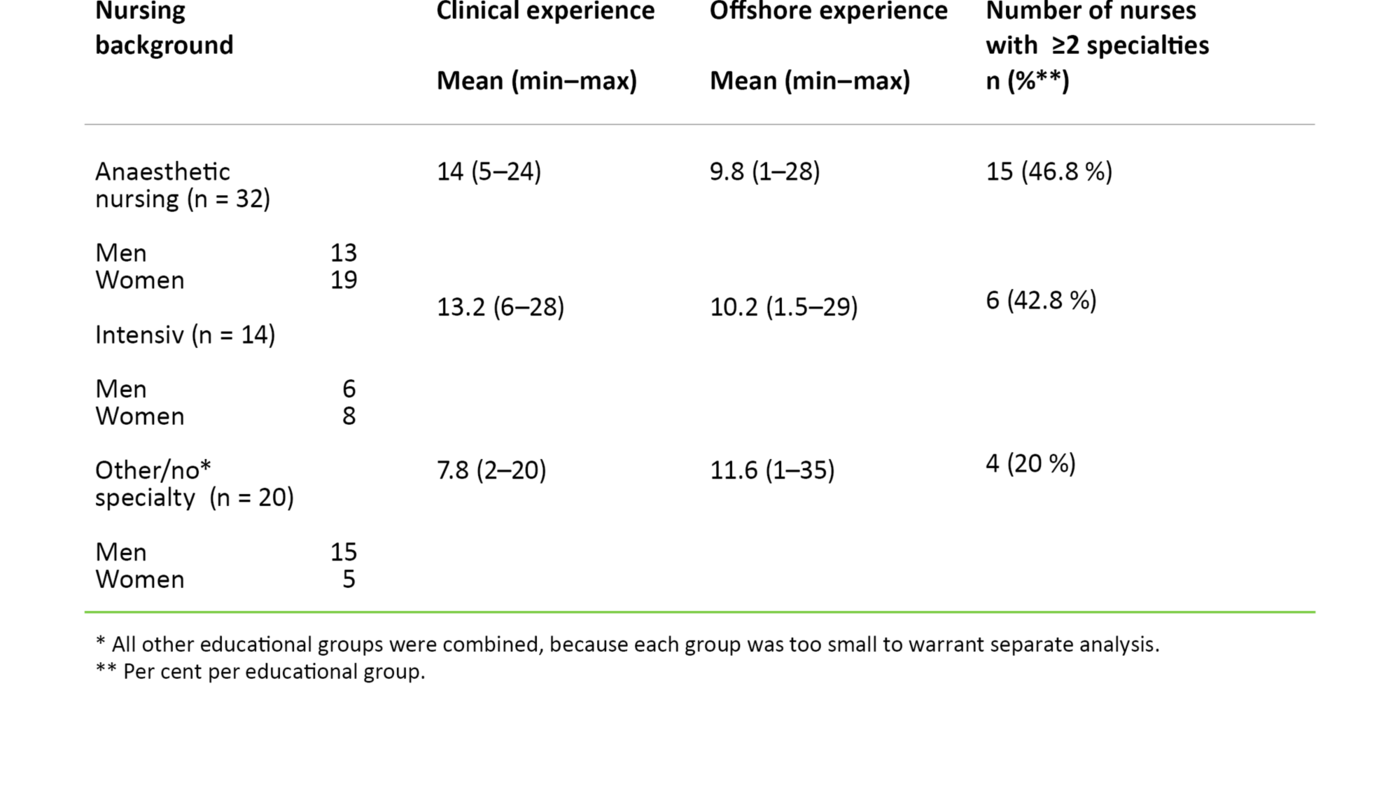
The sample consisted of 34 (51.5 per cent) men and 32 (48.5 per cent) women. Men and women had the same number of specialties, but men had significantly less clinical experience than women (p = 0.002). Table 1 shows that the group with either no specialty or with a different specialty had less clinical experience, and included fewer nurses with multiple specialties, than the groups with anaesthetic or intensive care training.
A few of the nurses had advanced specialist training in theatre nursing, acute care nursing or paramedic training, but many of them had specialist training in anaesthetic nursing or intensive care nursing as well. Twenty-three nurses reported that they had a different specialty, which may have referred to other healthcare disciplines, a master’s degree or possibly healthcare management. The responses for clinical experience indicated that 59.1 per cent had worked in an Accident & Emergency department in the past, 48.5 per cent in anaesthetic departments, 47 per cent in an intensive care unit and 27.3 per cent in the ambulance service.
The first variance analysis showed that no age group, educational group or past work experience group was significantly different from the others. To facilitate further analyses, we recoded all of the competence-related questions into seven variables, each corresponding to one of the seven areas of competence referred to in the questionnaire. Table 2 shows each of the educational groups’ results in all seven areas of competence.
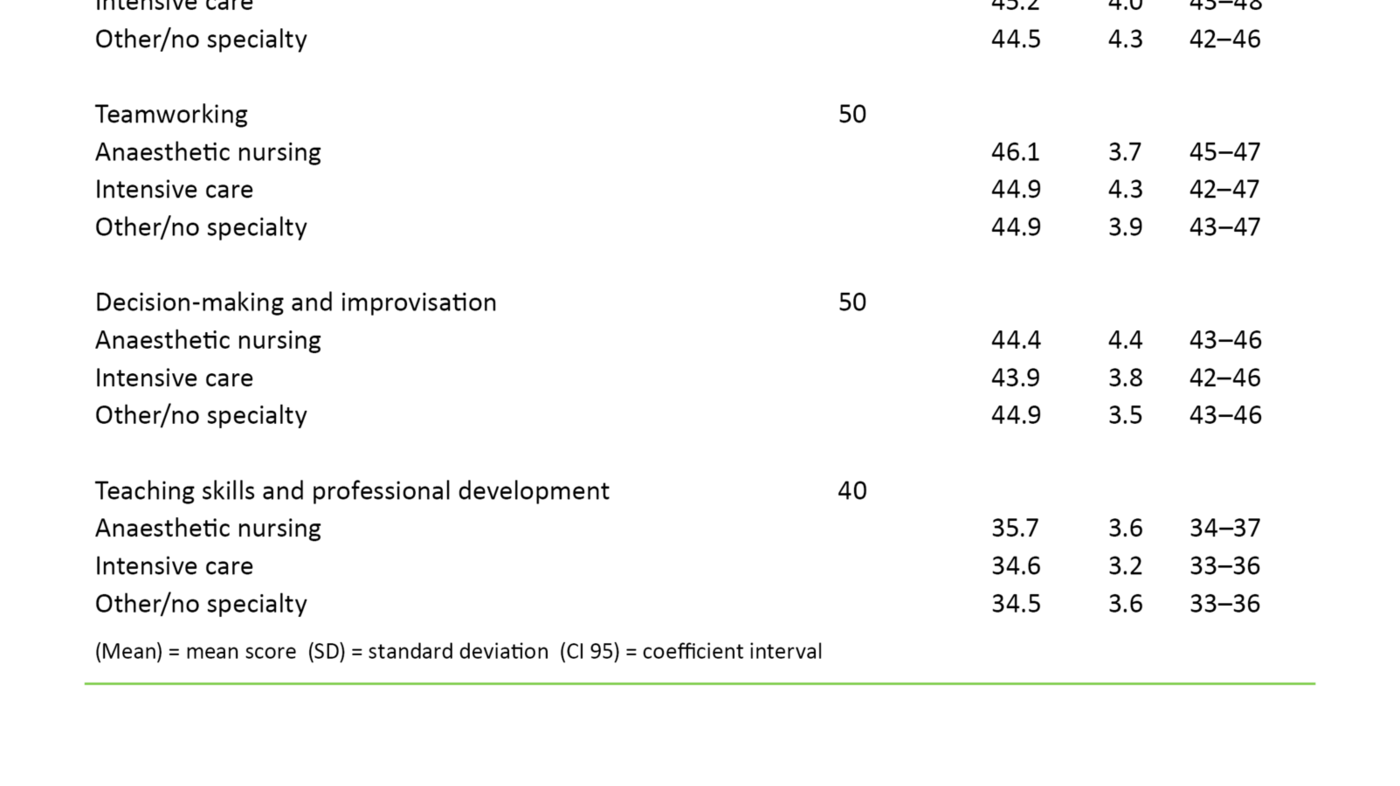
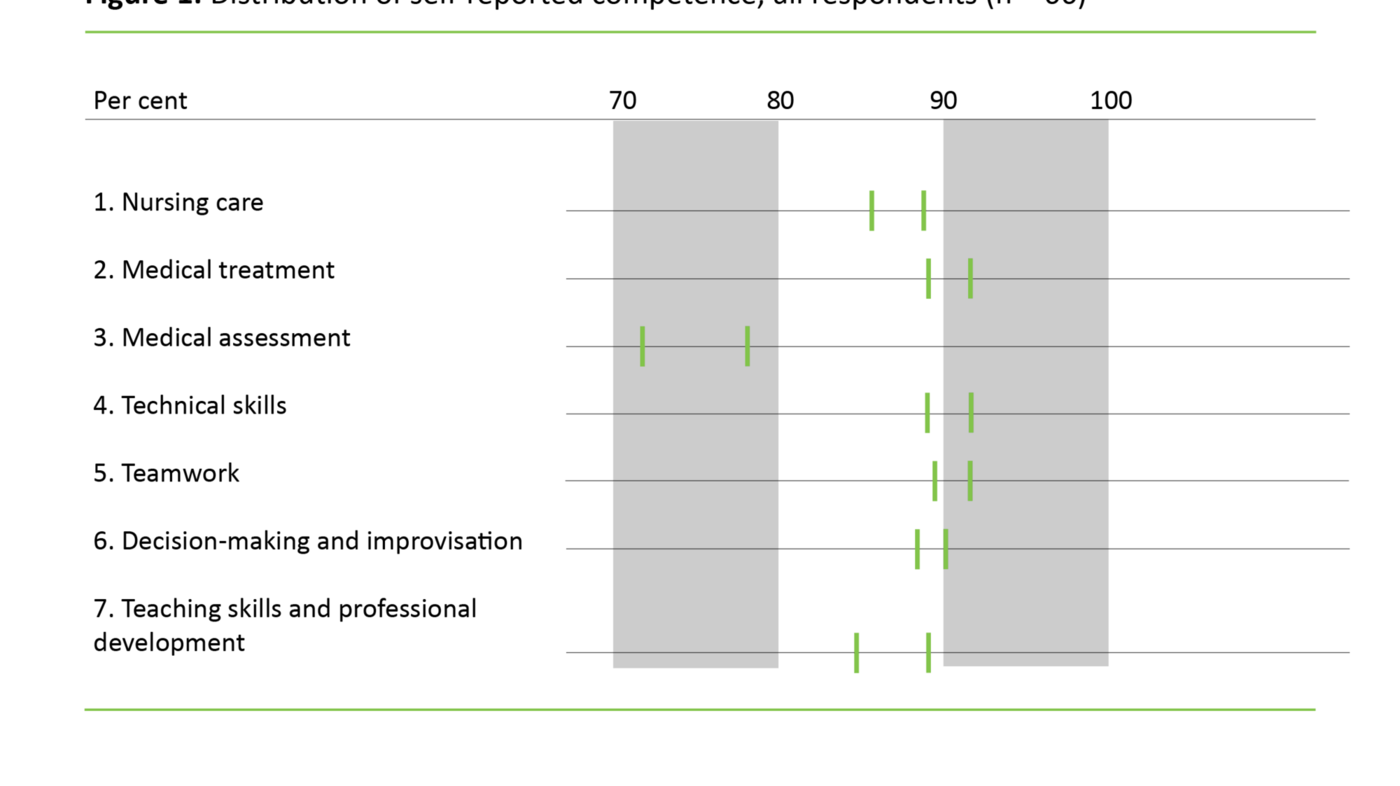
Our analysis of the variance showed no significant differences between educational groups (p values between 0.498 and 1.0). In all educational groups, the standard deviation was greatest for medical assessment, which suggests that this was the skills area with the greatest distribution of responses. The respondents considered their own competence to be somewhat lower in this area than within the other areas.
Figure 1 clarifies the difference in distribution by showing the responses as percentages.
We also investigated whether the reported types of past work experience, or the length of clinical experience, the length of offshore experience, or multiple specialties influenced the self-reported competence levels. The variance analysis showed that nurses with less than four years’ clinical experience considered themselves to be just as competent in all seven areas as the specialist nurses with more than 20 years’ clinical experience. Responses to each of the 44 competence-related questions in the three educational groups were compared. Only one of ten questions under the Medical treatment heading showed a significant difference: The intensive care nurses considered that they were less capable of implementing emergency medical procedures than what anaesthetic nurses did (p = 0.037).
When asked what clinical experience was most relevant to their work offshore, the highest scorers were out-of-hours primary care (92.3 per cent), Accident & Emergency departments (87.2 per cent) and surgical wards (83.3 per cent).
The respondents were asked to indicate up to three areas of healthcare competence which they felt were required for their work. The highest scorer was the ambulance service (17.6 per cent), followed by Accident & Emergency departments (15.6 per cent) as second choice and out-patient clinics (12.6 per cent) as third choice. Past work experience did not influence the respondents’ ratings.
Discussion
The offshore nurses in this sample rated their respective competencies to be at the same level, irrespective of their past work experience and nursing specialties. No correlation was found between the nature and duration of past work experience and self-reported competence levels within any of the areas we looked at. We had expected to find greater variance among the groups of nurses in terms of how they evaluated their own competence, with a lower score achieved by those whose experience was less varied and of short duration. One explanation may be that offshore nurses have to attend the same mandatory type of course, irrespective of their past experience, and they have to attend regular onshore practice sessions. Also, limited practice in emergency care offshore is compensated for by frequent training in standardised emergency medical protocols.
Protocols and manuals work well in practical training situations for people with little experience (12), and the less experienced nurses may thus have rated their own competence highly because they mastered every part of the protocol. It is likely that the sample’s high scores in all areas better reflect the competence levels of experienced nurses. The scores suggest a competence level that requires a unique combination of theoretical knowledge, situation awareness and professional assessment (11, 12).
The only significant finding, then, was the fact that the intensive care nurses’ rating of their own ability to implement emergency medical procedures was lower than the rating reported by the anaesthetic nurses. Emergency medical procedures form a part of both groups’ specialist training and job descriptions (21, 22). One possible explanation may be the fact that anaesthetic nurses are trained to establish a secure airway and intravenous access within and outside their own place of work, while intensive care nurses often treat patients who have already been intubated and have cannulas and a central venous catheter. Moreover, different criteria for competence attainment are clearly defined in the framework plans for both nursing specialties (21, 22).
Intensive care nurses are not normally part of trauma teams, which is why we expected to see differences between the anaesthetic and intensive care nurses and the other nurses in terms of their own perceived ability to treat seriously injured patients. The fact that there was no difference may be due to the fact that all nurses who work offshore train to provide the same trauma care. Research has shown that it is more difficult to evaluate knowledge than practical skills, and findings have suggested that respondents evaluate their own potential performance rather than their true performance, or they put an emphasis on their own effort rather than their own results (15).
Medical assessment
The results relating to “medical assessment” were slightly different to the results relating to other areas of competence in that there was greater distribution of responses and a lower mean score, although none of the results were significant. The questions focused on the ability to examine patients and make assessments in various fields of medicine. These tasks are included among the core competencies of doctors, for example the ability to carry out an eye examination or a neurological examination according to the guidelines provided by the Norwegian Electronic Medical Handbook. Awareness that such examinations or assessments come within the remit of doctors, may have meant that the nurses evaluated their own competence to be lower. Several researchers have suggested that when respondents measure their own competence against a given standard, in this case the competence of doctors, they give themselves a lower score (23, 24).
Research has shown that it is difficult for the least competent individuals to evaluate what constitutes a high level of competence within a discipline. Individuals with less education and experience of a certain discipline cannot fully appreciate the level of their own abilities within a wider context (24). At the same time, more competent individuals have a tendency to believe that a task that they find easy, will also be easy for others. Furthermore, they may have experienced a number of situations where they found their own competence to be lacking. Such situations may have led them to underestimate their own competence compared to that of colleagues with less education and experience (23, 25).
The respondents reported that the need for past experience of work in out-of-hours primary care and Accident & Emergency departments was greater than the need for experience of work in specialist emergency medical wards, such as anaesthetic and intensive care units. One of the reasons may be that the majority of offshore patients are people that need treatment for less serious conditions (5, 19). However, the respondents’ wish for more experience of work in emergency medicine does not match up with the fact that all respondents rated their own emergency medical competence as being very good. The offshore companies expect the nurses they employ to be fully skilled in emergency medicine, and offshore jobs are highly desirable. We can only speculate as to the reasons for the discrepancy, as we have found no research that fully elucidates the matter. Some literature has however established that there is a gap between assumed and real learner needs among health care personnel (23).
The study’s limitations
Some of the advantages of a questionnaire survey of perceived competence are the possibility of recruiting more respondents, generating large volumes of first-hand data and receiving standardised response alternatives that are easy to analyse (13, 15). The disadvantage is low reliability, particularly in the case of respondents whose level of competence is low. There is also a greater likelihood that those who feel the least competent, refrain from taking part, or that they award themselves a higher score because the results may affect their opportunity of future employment (15). Our questionnaire was based on a validated template, but we have made a few adjustments to the instrument that have yet to be validated.
The recruitment procedure via companies in the petroleum sector is the study’s weakest factor, and the low response rate may have affected the results. Sending out the questionnaire during the nurses’ off-duty periods, the login procedure and the use of an online questionnaire are other factors that may have had an adverse effect on the rate of participation.
Conclusion
This survey found no differences among the overall self-reported competence levels of offshore nurses despite there being great differences among the respondents with respect to their educational background and past work experience. Nor was it established whether past experience impacted on the self-reported competence levels. Due to the low response rate, the survey findings cannot be generalised, but they may nevertheless be of interest since there is no previous research in this field.
References
1. Tronsmoen S. Helsetjenesten offshore. Sykepleien 1992;80(3):20–1.
2. Sosialdepartementet. Norm for midlertidig instruks for sykepleier ansatt på anlegg for produksjon m.v. i petroleumsvirksomheten på kontinentalsokkelen [fastsatt av Sosialdepartementet 11. mai 1978]. 1979.
3. Ulven J. Medical and psychological challenges in the offshore petroleum industry. Int Marit Health 2009;60:40–2.
4. Forskrift av 12. februar 2010 nr. 158 om helse, miljø og sikkerhet i petroleumsvirksomheten og på enkelte landanlegg (rammeforskriften). Available at: https://lovdata.no/dokument/SF/forskrift/2010-02-12-158(downloaded 21.01.2016).
5. Evensen AMC, Brattebø G. The use of integrated operations in order to improve quality of health care and medical evacuations from offshore installations. [presentation] SPE Intelligent Energy Conference and Exhibition, Amsterdam; 2008.
6. Duffy B. Dental problems in the offshore oil and gas industry: A review. Occup Med 1996;46:79–83.
7. Ponsonby W, Mika F, Irons G. Offshore industry: medical emergency response in the offshore oil and gas industry. Occup Med 2009;59:298–303.
8. Gilja A. For syke til å jobbe offshore. Available at: https://sysla.no/offshore/for_syke_til_229_jobbe_offshore/(downloaded 07.08.2017).
9. Statoil.com. HMS-koordinator/leder (sykepleier) (7725). Available at: https://jobb.tu.no/jobb/hms-koordinatorleder-offshore-sykepleier-7725/20519(downloaded 07.08.2017).
10. Industri Energi. Lønns og arbeidsvilkår. Tariffavtaler. Flyteriggavtalen NR. Available at: http://www.industrienergi.no/lonns-og-arbeidsvilkar/tariffavtaler/flyterigg-norsk-samleversjon-sokie-2014/(downloaded 18.05.2015).
11. Cowan DT, Norman I, Coopamah VP. Competence in nursing practice: a controversial concept – A focused review of literature. Accid Emerg Nurs 2006;15:20–6.
12. Eraut M. Developing professional knowledge and competence. London: Routledge; 1994.
13. Polit DF, Beck CT. Nursing research (int. ed., 9. ed.) Philadelphia: Lippincott Williams & Wilkins; 2012
14. Lund T, Haugen R. Forskningsprosessen. Oslo: Unipub forlag; 2006.
15. Bing-Jonsson P, Bjørk IT, Hofoss D, Kirkevold M, Foss K. Instruments measuring nursing staff competence in community health care: a systematic literature review. Home Health Care Management Practice 2013;25:282–94.
16. Valeberg BT, Grønseth R, Fagermoen MS. Spesialsykepleieres opplevde kompetanse etter endt utdanning. Sykepleien Forskning 2009;4:206-213. Available at: https://sykepleien.no/forskning/2009/10/spesialsykepleieres-opplevde-kompetanse-etter-endt-utdanning(downloaded 01.08.2017).
17. Høgskolen Betanien. Studietilbud, paramedic. Available at: http://www.studiesok.no/paramedic-hogskolen-betanien/(downloaded 08.08.2017).
18. Forskrift av 29. april 2010 nr. 613 om utføring av aktiviteter i petroleumsvirksomheten (aktivitetsforskriften). Available at: https://lovdata.no/dokument/SF/forskrift/2010-04-29-613(downloaded 21.01.2016).
19. Parkinson G. Working as a medic on an offshore oil rig. Intervju av Clare Lomas. Nursing Times 2005;101:76–7.
20. Norsk Helseinformatikk. Norsk Elektronisk Legehåndbok. Available at: https://legehandboka.no/(downloaded 18.08.2017).
21. Kunnskapsdepartementet. Forskrift til rammeplan for videreutdanning i anestesisykepleie. 2005. Available at: https://lovdata.no/dokument/SF/forskrift/2005-12-01-1388 (downloaded 01.08.20.17).
22. Kunnskapsdepartementet. Forskrift til rammeplan for videreutdanning i intensivsykepleie.2005. Available at: https://lovdata.no/dokument/SF/forskrift/2005-12-01-1389 (downloaded 01.08.20.17).
23. Colthart I, Bagnall G, Evans A, Allbutt H, Haig A, Illing J, McKinstry B. The effectiveness of self-assessment on the identification of learner needs, learner activity, and impact on clinical practice: BEME Guide no. 10. Med Teach 2008;30:124–45.
24. Jensen, R. Clinical reasoning during simulation: comparison of student and faculty ratings. Nurs Educ Pract 2013;3:23–8.
25. Schlosser T, Dunning D, Johnson Kl, Kruger J. How unaware are the unskilled? Empirical tests of the «signal extraction» counterexplanation for the Dunning-Kruger effect in self-evaluation of performance. J Econ Psych 2013;39:85–100.










Comments