Deficient reporting of falls in nursing homes
Deficient documentation of falls may stop the implementation of necessary preventive interventions. The nursing homes in the study are nevertheless failing to comply with their own documentation requirements.
Background: Fall prevention in nursing homes is one of the main target areas set out in the Norwegian Patient Safety Programme, and the documentation of fall hazards is a requirement.
Objective: The objective of this study was to investigate whether the nursing homes’ documentation practices with respect to fall incidents comply with their internal documentation requirements and to identify any factors associated with compliance.
Method: This quality improvement project involves a retrospective descriptive study which reviewed the fall documentation practices at three different nursing homes and examined whether these practices were compliant with the nursing homes’ internal documentation requirements.
Results: The total sample included 652 people. Of these, 208 (32 per cent) had experienced a fall. A total of 556 fall incidents were reported for these people. Falls involving injuries (pain, cuts, fractures) accounted for 26 per cent of the reported incidents. Only 10.6 per cent of the falls were reported in accordance with the nursing homes’ internal requirements. There was significant variation between nursing homes with respect to their documentation practices, but fractures were generally associated with correct completion of an injury report form.
Conclusion: The results show that nursing homes fail to comply with their own documentation requirements in connection with falls in general, but that falls involving fractures were associated with correct documentation practices.
Prevention has long been a key target area for Norwegian health authorities; the Coordination Reform has further emphasised the need for prevention and better coordination between the different parts of the health service. Prevention is intended to help avoid unnecessary discomfort for patients and reduce the number of unnecessary hospital admissions (1).
The Norwegian Patient Safety Programme entitled In Safe Hands 24–7has highlighted fall prevention as a particularly important target area. This programme aims to reduce the incidence of patient injuries and increase patient safety in Norway (2). It is a continuation of a comprehensive national patient safety campaign that was run by the Norwegian specialist and primary healthcare services in the period 2011–2013. The campaign was commissioned by the Norwegian Ministry of Health and Care Services, and the primary healthcare services was invited to participate on a voluntary basis. There were three main objectives: to reduce the number of patient injuries, to establish lasting systems and structures for patient safety, and to improve the patient safety culture in the health service. The Patient Safety Programme covers 12 main target areas, two of which include the prevention of falls in nursing homes and the correct use of medication in nursing homes (medication review).
The health and social care services’ quality requirements and improvement strategies are well known, yet it has repeatedly been demonstrated that there is a gap between desired and real practices (3). Nursing documentation requirements are disregarded, or the documentation may be inadequate or of a poor standard (4). The implementation of secondary prevention measures can therefore be deficient. There is a need for more knowledge as to whether the secondary prevention strategies are in fact put in place in connection with fall incidents, and more knowledge about factors that may affect the work involved with implementing fall prevention strategies.
Falls – a serious health problem for the elderly
Falls and fall injuries can be defined in various different ways. One definition used by Norwegian authorities describes a fall as an incident which results in a person coming to rest inadvertently on the ground or floor or other low level, irrespective of the reason and irrespective of whether an injury arises as a consequence of the fall (2). A fall injury is defined as a cut that needs suturing, a graze or abrasion that requires treatment, sprains, suspected fractures, fractures and all head injuries (2).
This article is based on a wider analysis of data collected in connection with a clinical review at three Norwegian nursing homes (5). The study examined the medication assessments associated with falls, which showed that 32 per cent of the 652 residents had experienced at least one fall. Of the 208 residents who had experienced a fall, 46 per cent had fallen once, while 25 and 29 per cent respectively had fallen two times or more. The study further showed substantial deficiencies with respect to the reporting of falls. This was established by identifying considerable under-reporting of falls on injury report forms (non-conformance reports) compared to the number of falls reported in the patient records. This article does not examine and discuss this matter in depth and thus invites further consideration and questioning with regard to whether the documentation practice requirements for fall incidents are being fulfilled.
Our focus on fall prevention is also based on our current knowledge of the considerable negative consequences that falls may have for the elderly. Falls represent a serious health problem among the elderly, whether they live in a nursing home (6, 7) or in their own home (8). Studies show that more than a third of the elderly population experience a fall every year, that the risk of falling increases after the age of 75, and that 50 per cent of elderly individuals over the age of 80 has at least one fall per year (7, 9). A systematic review article showed that 10 to 20 per cent of falls in the elderly population gave rise to serious injuries such as head traumas or fractures (7).
Our focus on falls is also based on the fact that there is considerable documented potential for improvement if preventive interventions are implemented in healthcare institutions (2). Norway has seen the introduction of a special intervention package for fall prevention (2). Risk assessments of falls and medication reviews make up two of the most important fall prevention interventions.
Prevention and risk factors
Secondary prevention strategies have now been proposed in order to reach the goal of reducing the incidence of falls and falls that cause injury in healthcare institutions (10). Secondary fall prevention involves, among other things, the identification of individuals with an increased risk of falling. Documenting the risk of falling is needed to ensure that individuals who have had a fall will have their medical prescriptions re-assessed (5), that all people with an increased risk of falling are identified, and that other interventions can be implemented in order to prevent further falls.
Today we have a great deal of knowledge about factors that influence the risk of falling (7, 11, 12). A previous fall is a key risk factor for further falls (2), combined with internal risk factors such as health and level of functionality (13), and external environmental factors (11). This means that the patients’ risk of falling must be assessed if they have already had a fall (2).
It is recommended that this type of risk assessment is carried out as a secondary prevention intervention for all patients over the age of 65 and other adults with neurological or cognitive disorders or considerable visual impairments. This should take place no later than 24 hours after admission to hospital, or after the first meeting with the patient. The assessment must be conducted by a nurse or healthcare worker. The risk of falling must be re-assessed if the patient’s general level of fitness should change or if the patient has a fall, and at least once a year for any long-stay patients. The risk of falling must be documented in the patient records (2).
This study’s objective was therefore to describe documentation practices in connection with falls in nursing homes and discuss the degree to which these coincided with the nursing homes’ internal documentation requirements. We also wanted to investigate whether the age and gender of residents, the location of the nursing home, the type of fall and whether or not the resident was admitted to hospital were factors associated with the completion of injury report forms.
Method
This quality improvement project was conducted as a retrospective descriptive study of patient records and injury report forms in the period 1 August 2010 to 31 July 2011 at three nursing homes in a large Norwegian municipality. According to the nursing homes’ written procedures and explicit documentation requirements for fall incidents at the time of data collection, all falls had to be documented in accordance with the institution’s current documentation procedures. This means that falls had to be documented as an undesirable incident, in the patient records as well as on an injury report form. All staff were made aware of this requirement during their training. The injury report form that was used by all the nursing homes takes the form of an electronic document in which all data about the fall should be recorded, such as the date of the incident and a description of it, the consequences of the fall and any further follow-up measures.
During the survey period a total of 652 individuals over the age of 65 were admitted to the three nursing homes included in the survey, and all falls that were documented in patient records, on injury report forms or both, were registered. The nursing homes all used the same IT system for documentation purposes and to follow up each individual resident.
Data collection and variables
Data were collected by gathering information about falls from anonymised patient records and injury report forms; free text searches of patient records were carried out for the words ‘fell’ and ‘tripped’. The patient records and injury report forms were carefully reviewed and checked against each other. This registration exercise resulted in an overview of all the falls suffered per person, and this enabled us to establish whether falls appeared in both sets of records or in only one of them.
Each fall incident was listed and recorded as having been documented in the patient records only, on the injury report form only, or in both places. The date of the fall was registered, as well as the age and gender of the patient. The consequences of the falls were listed against the following variables: ‘injury’ and ‘hospitalisation’. The following values were assigned to the ‘injury’ variable: ‘fall without injury’, ‘fall with non-fracture injury (pain and cuts)’ and ‘fall with fracture’. The ‘hospitalisation’ variable was assigned the values ‘admitted to hospital’ or ‘not admitted to hospital’.
Analysis
Categorical variables are expressed as absolute numbers and percentages, while continuous variables are expressed as the mean and standard deviation. Multiple logistic regression was used to establish whether age, gender, practice location (the nursing homes), fall with injury and hospital admission were factors associated with non-completion of an injury report form following a fall. Odds ratio (OR) > 1 indicates an increased risk of not completing an injury report form. A two-sided P-value < 0.05 suggests statistical significance. SPSS version 20 was used for the statistical analyses.
Ethical considerations
The Regional Committees for Medical and Health Research Ethics (REC) considered the project to be exempt from any obligation to seek their approval under the Norwegian Health Research Act, but because this was an internal quality improvement project conducted by an external person, the project was submitted to the Norwegian Data Protection Authority for clarification of the legal aspects. The Data Protection Authority recommended that the matter be submitted to the Norwegian Directorate of Health, which granted approval for the project, provided that all health information was anonymised. This condition was met by collecting all data from an anonymised version of the nursing homes’ databases.
Results
Of the 652 individuals in the sample, 208 (32 per cent) had experienced a fall; a total of 556 fall incidents had been reported (Table 1). This shows that many residents had fallen more than once. The average age of individuals who had experienced a fall was 85.5 years. The majority of falls were reported to involve women (60.8 per cent).
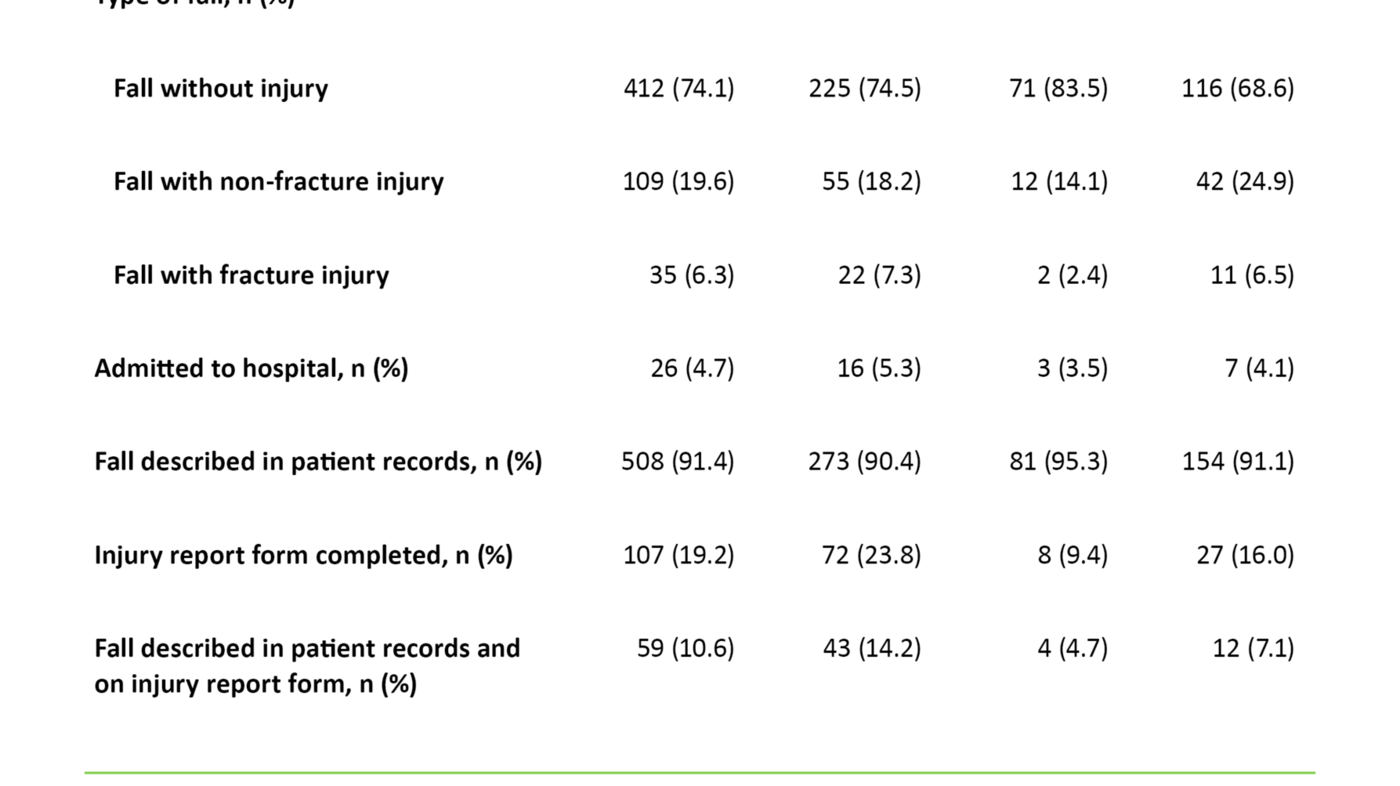
Falls without injury accounted for 74.1 per cent of the falls. Falls with non-fracture injuries (pain and cuts) accounted for 19.6 per cent, while 6.3 per cent of the falls resulted in a fracture. Twenty-six of the fall incidents resulted in the patient being admitted to hospital (4.7 per cent).
We found that 91.4 per cent of the fall incidents were described in patient records, while 19.2 per cent of the falls were documented on injury report forms. In total, 10.6 per cent of the falls were documented in both the patient records and on an injury report form.
Factors associated with injury reporting
The logistic regression analysis showed that there were statistically significant differences between the nursing homes in terms of how frequently an injury report form was completed after a fall (P = 0.008) (table 2).
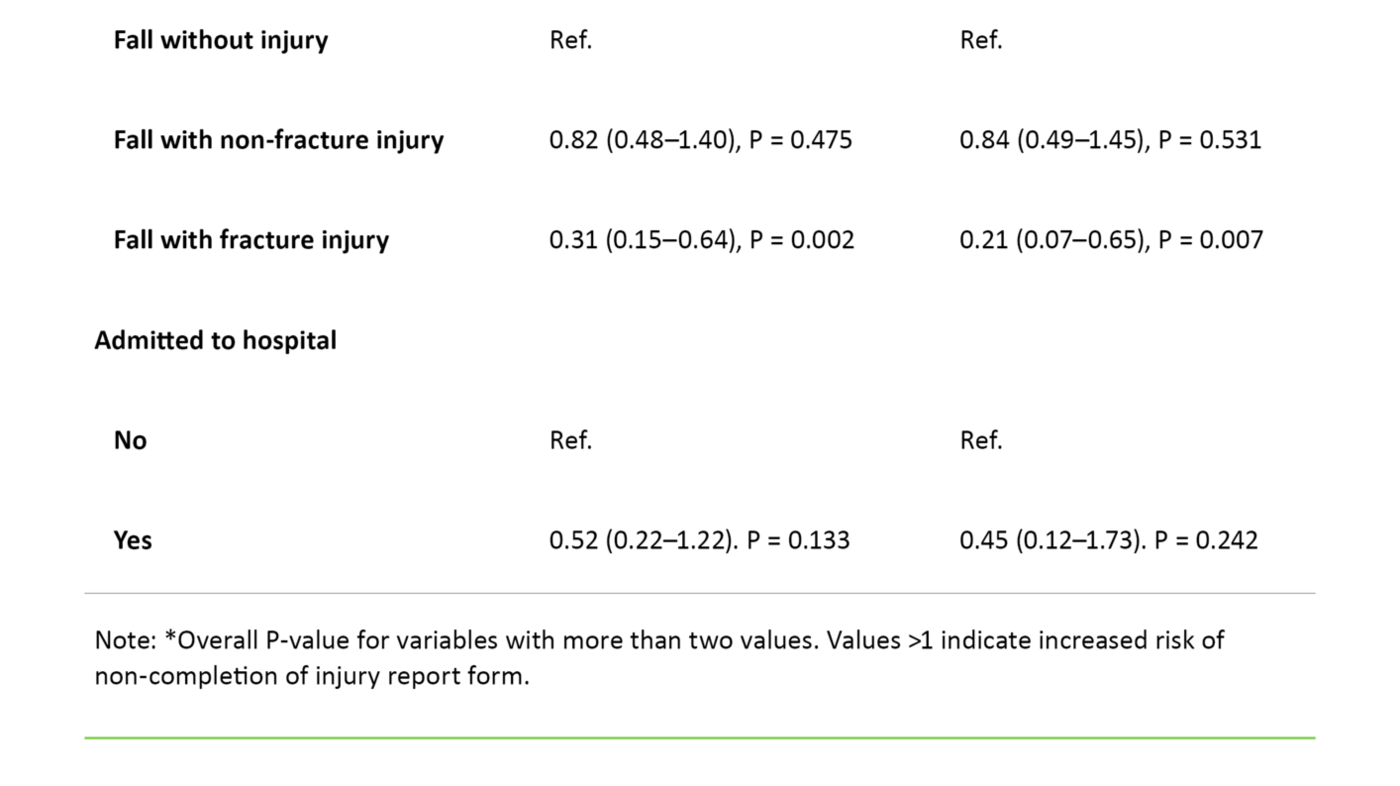
Moreover, there was a clear correlation between the severity of the injury caused by the fall and whether an injury report form was completed (P = 0.026). The relative probability of non-completion of an injury report form was lower when the fall resulted in a fracture than when the fall did not cause an injury (OR = 0.21; P = 0.007).
Whether or not the fall caused the individual to be hospitalised did not produce a significant difference with respect to the relative probability of non-completion of an injury report form (OR = 0.45; P = 0.242).
Discussion
This study’s objective was to examine the extent to which the nursing homes’ practices comply with their own internal requirements with respect to falls, and to identify any associated factors.
We found that most falls involve women. This must be seen in the light of the large percentage of female residents in nursing homes. The risk of falling increases after the age of 75, and 50 per cent of those over the age of 80 fall at least once a year (9). Similar figures are brought out by this study. Average age at the time of the fall incidents was 85.5, which suggests that this may be a high-risk group and therefore that there is a need for follow-up measures.
The results of this study show that the nursing homes in practice do not comply with their own documentation requirements in connection with falls. Only 10.6 per cent of the falls were documented in both the patient records and on an injury report form, even though the nursing homes’ own requirements expressly state that that these forms must be completed when a fall occurs. However, the study also shows that nursing homes vary in their compliance with fall documentation requirements, and that more serious falls are associated with better compliance.
Deficient reporting of falls
There are several reasons why the current rule is to report any fall by an elderly person, and why a risk assessment must be carried out after an elderly person has experienced a fall. First and foremost, this practice provides an opportunity to implement preventive interventions. A risk assessment involves a systematic review of various factors, both external and internal, that increase the risk of falling, including the prescription of medication for the elderly person (5). Deficient reporting may mean that no such risk assessment is conducted, so that necessary preventive measures cannot be implemented. Deficient reporting of falls also means that we cannot gain more knowledge about the extent of the problem and the consequences to society.
There may be several reasons why falls are not documented in compliance with the nursing homes’ requirements. Research on risk factors gives us knowledge about preventive interventions. One reason may be that this knowledge is not passed on to staff. The personnel may have insufficient knowledge about the fall documentation requirements and about the potentially serious negative consequences of a fall for the elderly person (14). Consequently, they will not appreciate the need for documentation, which is why they fail to comply faithfully with the reporting requirements.
This study has investigated whether falls are documented in compliance with the guidelines established by the nursing homes themselves. We cannot therefore rule out the possibility that risk assessments and necessary changes are introduced without this being documented. If so, the documentation will be deficient due to insufficient knowledge about quality-enhancing efforts and documentation, not insufficient knowledge about the risk of falling and fall prevention. We have little knowledge of how nursing home staff might assess and consider the need to report non-conformances. It may well be that non-conformance reporting is felt to constitute extra work or to be onerous in other ways, if no positive culture has been established around doing so.
Reasons for deficient documentation
The correlation between the severity of the fall and whether an injury report form was completed may indicate that nursing home staff are insufficiently acquainted with their institution’s internal documentation requirements when it comes to reporting incidents (non-conformances). However, we have also found that it was not until the fall caused an injury that it was satisfactorily documented. This may suggest that one contributory explanation is insufficient understanding of the importance of prevention and the link between non-conformance reporting and quality improvement (15).
The significant difference between the nursing homes with respect to the probability of completing an injury report form may be caused by cultural differences. The Patient Safety Programme is also conscious that patient safety is affected by various employment issues, and patient safety culture is therefore one of its three main objectives (2). Different knowledge levels may also be a reason associated with, for example, the difficulty of recruiting staff with relevant skills and expertise, or associated with the management’s focus on fall prevention, as this differs between institutions. All of the nursing homes included in the study were located within the same municipality, which suggests that they all have the same opportunity to recruit qualified staff. It is therefore reasonable to assume that the differences between them were caused by cultural differences and by their respective managements’ different focus on fall prevention.
Another potential reason why the reporting is deficient is that inadequate attention is paid to the overall implementation process. When it comes to fall prevention practice, documentation requirements and risk assessments are innovations that may represent new ways of working. Implementing new practice is never easy. Research on fall incidents has given us knowledge about risk factors and fall prevention, but this research provides no knowledge about how to implement the interventions. A transfer of knowledge may, on its own, not necessarily be enough to change practice (16-18). When introducing fall prevention interventions the organisation will need to focus on the overall implementation process (19).
A change of practice may require the introduction of a competence development regime adjusted to the specific context, including provision of follow-up and guidance, and involving and supporting the people who will be implementing the intervention (16, 17, 20). Adjusting the implementation to the specific practical context (21) will be important. The management of the institutions will play a key role throughout this process. Insufficient attention from management to the overall implementation process may be a contributing factor to deficient documentation (22). Time pressure, large workloads and insufficient knowledge about nursing documentation will of course play a part (23, 24). Further obstacles to good nursing documentation include frequent interruptions while writing the report and insufficient guidance (25). It is important to be aware of these barriers so that the initiatives put forward as part of quality improvement strategies can be targeted towards them (26).
The study’s limitations and weaknesses
The results from this study describe the current practice at three Norwegian nursing homes over a specific period of time. This suggests that we need to be careful not to generalise the results and assume they also apply to other nursing homes. Furthermore, it is reasonable to believe that the results may have been different had the study been conducted after the implementation of the Patient Safety Programme. The IT system used by the nursing homes is very well suited for retrieving data, and many data were imported directly from the database and into the analysis tool. Reporting errors that might have been caused by manual input of data were therefore avoided.
This article is based on information obtained from patient records. There may have been reporting errors, or reports may have been based on an incorrect definition of a fall. Some may have defined a fall as a fall resulting in an injury, and falls may have been described by using words other than ‘fell’ or ‘tripped’. These are possible sources of error that may account for under-reporting of fall incidents. Furthermore, the non-significant association between hospitalisation and completion of an injury report form (OR = 0.45) (Table 2) may be a type II error caused by low statistical power.
The road ahead
The results of this study show that there is great potential for improvement in nursing homes when it comes to their documentation of fall incidents. There is reason to believe that training in how to follow documentation procedures may help to improve the documentation practice, since several systematic overviews show that training interventions can improve the quality of nursing documentation (4, 27). Furthermore, feedback may form part of the training intervention, thereby ensuring that the results of research into current practice are communicated to staff to boost their motivation to try to close the gap between current practice and what research has shown to constitute high-quality nursing documentation (28, 29).
Research has highlighted that reviews and feedback can serve as effective tools for improving current practices if there is a significant gap between real and recommended practice (30), which is the case in this study. In addition, it will be important that further fall prevention initiatives focus on the overall implementation process, so as to create a culture of patient safety within the health service. We need more research on the actual implementation practices in nursing homes, both in terms of fall prevention and other interventions, and we need research on the characteristics of successful implementation processes.
Conclusion
By measuring the quality provided at three nursing homes in Norway, this study has demonstrated that there is a large gap between requirements and actual practice. Only 10.6 per cent of reported falls had been documented in accordance with the nursing homes’ internal requirements. Some improvements may already have been introduced as a consequence of the Patient Safety Programme, but this nevertheless suggests that there is a need for training, for a revision of requirements and procedures, and for feedback on the level of compliance in addition to a cohesive implementation process.
This study is based on a master’s thesis on evidence-based practice within the health and social sciences at Bergen University College, Centre for Evidence-based Practice. The author wishes to thank Monica W. Nortvedt, Birgitte Espehaug and Katrine Aasekjær, the thesis supervisors, for their assistance with project implementation. The author also wishes to thank the software developer and IT administrator for the nursing homes, Magne Rekdal of Emetra AS, for providing training in the use of the software and for his assistance with data retrieval.
References
1. Helse- og omsorgsdepartementet. Samhandlingsreformen. Helse- og omsorgsdepartementet, Oslo. 2008.
2. Helsedirektoratet. Forebygging av fall i helseinstitusjoner 2015. Available at: http://www.pasientsikkerhetsprogrammet.no/no/I+trygge+hender/Innsatsomr%C3%A5der/forebygging-av-fall-i-helseinstitusjoner;jsessionid=72C5D43A140951BDD3263E6C10BCE32A. (downloaded 21.12.2015.)
3. Sosial- og helsedirektoratet. ... OG BEDRE SKAL DET BLI!: nasjonal strategi for kvalitetsforbedring i Sosial- og helsetjenesten (2005–2015). Sosial- og helsedirektoratet, Oslo. 2005.
4. Saranto K, Kinnunen UM. Evaluating nursing documentation – research designs and methods: systematic review. J Adv Nurs. 2009;65(3):464–76.
5. Øygard SH, Nortvedt MW, Espehaug B, Aasekjær K. Samsvar mellom praksis og retningslinje for førebygging av fall og vurdering av medikamentordinasjon på sjukeheim. Sykepleien Forskning. 2013;8(3):242–8.
6. Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006;12(5):290–5.
7. Sterke CS, Verhagen AP, van Beeck EF, van der Cammen TJ. The influence of drug use on fall incidents among nursing home residents: a systematic review. Int Psychogeriatr. 2008;20(5):890–910.
8. Boyé ND, Van Lieshout EM, Van Beeck EF, Hartholt KA, Van der Cammen TJ, Patka P. The impact of falls in the elderly. Trauma. 2013;15(1):29–35.
9. Helsedirektoratet. Fallforebygging i kommunen. Kunnskap og anbefalinger. Helsedirektoratet, Oslo. 2013. Available at: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/98/Fallforebygging-i-kommunen-kunnskap-og-anbefalinger-IS-2114.pdf. (downloaded 25.06.2017).
10. Cameron ID, Gillespie LD, Robertson MC, Murray GR, Hill KD, Cumming RG et al. Interventions for preventing falls in older people in care facilities and hospitals. The Cochrane Library. 2012. Available at: http://www.cochrane.org/CD005465/MUSKINJ_interventions-for-preventing-falls-in-older-people-in-care-facilities-and-hospitals. (downloaded 26.06.2017).
11. Kenny RA. Mobility and falls. The Cambridge handbook of age and ageing. Cambridge University Press, Cambridge. 2005. (s. 131–40).
12. Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Archives of Internal Medicine. 2009;169(21):1952–60.
13. Bergland A. Fall risk factors in community-dwelling elderly people. Norsk epidemiologi. 2012;22(2):151–64.
14. Phillips VL, Roberts DY, Hunsaker AE. Certified nursing aides’ and care assistants’ views on falls: Insight for creation and implementation of fall prevention programs. Journal of the American Medical Directors Association. 2008;9(3):168–72.
15. Wagner LM, Capezuti E, Taylor JA, Sattin RW, Ouslander JG. Impact of a falls menu-driven incident-reporting system on documentation and quality improvement in nursing homes. The Gerontologist. 2005;45(6):835–42.
16. Fixsen D, Scott V, Blase K, Naoom S, Wagar L. When evidence is not enough: The challenge of implementing fall prevention strategies. Journal of Safety Research. 2011;42(6):419–22.
17. Etheridge F, Couturier Y, Denis J-L, Tremblay L, Tannenbaum C. Explaining the success or failure of quality improvement initiatives in long-term care organizations from a dynamic perspective. Journal of Applied Gerontology. 2014;33(6):672–89.
18. Fretheim A, Flottorp S, Oxman A. Effekt av tiltak for implementering av kliniske retningslinjer. Rapport fra Kunnskapssenteret nr. 10−2015. Oslo: Nasjonalt kunnskapssenter for helsetjenesten; 2015.
19. Wagner LM, Dionne JC, Zive JR, Rochon PA. Fall risk care processes in nursing home facilities. Journal of the American Medical Directors Association. 2011;12(6):426–30.
20. Szczerbinska K, Zak M, Ziomkiewicz A. Role of method of implementing multi-factorial falls prevention in nursing homes for elderly persons. The EUNESE Project. Aging Clinical and Experimental Research. 2010;22(3):261–9.
21. Neyens JC, van Haastregt JC, Dijcks BP, Martens M, van den Heuvel WJ, de Witte LP et al. Effectiveness and implementation aspects of interventions for preventing falls in elderly people in long-term care facilities: a systematic review of RCTs. Journal of the American Medical Directors Association. 2011;12(6):410–25.
22. Rask K, Parmelee PA, Taylor JA, Green D, Brown H, Hawley J et al. Implementation and evaluation of a nursing home fall management program. Journal of the American Geriatrics Society. 2007;55(3):342–9.
23. Björvell C, Wredling R, Thorell-Ekstrand I. Improving documentation using a nursing model. Journal of Advanced Nursing. 2003;43(4):402–10.
24. Naustdal A-G, Netteland G. Sjukepleiedokumentasjon i eit elektronisk samhandlingsperspektiv. Sykepleien Forskning. 2012;7(3):270–7.
25. Paans W, Sermeus W, Nieweg RM, van der Schans CP. Prevalence of accurate nursing documentation in patient records. J Adv Nurs. 2010;66(11):2481–9.
26. Burgess R. New principles of best practice in clinical audit. 2. edition. Radcliffe Publishing, Oxford. 2011.
27. Wang N, Hailey D, Yu P. Quality of nursing documentation and approaches to its evaluation: a mixed-method systematic review. Journal of Advanced Nursing. 2011;67(9):1858–75.
28. Straus S, Tetroe J, Graham ID, red. Knowledge translation in health care: moving from evidence to practice. Wiley-Blackwell, Oxford. 2009.
29. Flottorp S, Jamtvedt G, Gibis B, McKee M. Using audit and feedback to health professionals to improve the quality and safety of health care. World Health Organization, København. 2010. Available at: http://www.euro.who.int/__data/assets/pdf_file/0003/124419/e94296.pdf?ua=1. (downloaded 20.12.2015.)
30. Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD et al. Audit and feedback: effects on professional practice and healthcare outcomes. The Cochrane database of systematic reviews. 2012;6:Cd000259.










Comments