Encountering parents of a sick newborn child
When nurses encounter parents with a sick newborn child, it is vital that they see them as individuals and establish a relationship based on empathy.
Background: Parents often experience stress when their newborn child is admitted to a neonatal intensive care unit (NICU)ward. Nurses who meet parents must have knowledge about communication and relational competence to provide support based on the parents’ experiences and needs.
Objectives: To describe a group of nurses’ experiences of what is important in the encounters and conversations with parents of a sick newborn child.
Method: The study has a qualitative design with a phenomenological approach, where the aim is to obtain an accurate description of the informants’ experience of a phenomenon. Individual interviews were conducted with five nurses at an NICU. The interviews were analysed according to a descriptive phenomenological research method.
Results: When meeting the parents, the informants described it as crucial to establish a relationship based on empathy, to see the individual parent, to facilitate the mutual exchange of information and to foster parents’ sense of coping. When these aspects were present, the informants experienced a good encounter and conversation with the parents, but if these aspects not were present, the encounters and conversations were described as less successful.
Conclusion: The results emphasize that when encountering parents of a sick newborn child, nurses have a responsibility to establish a relationship based on empathy and to treat each parent according to their own situation in order to help them cope with their vulnerable situation.
Having a newborn baby admitted to a neonatal intensive care unit (NICU) is a frightening experience for most parents. All parents react differently, but many experience anxiety, powerlessness, loss of control, guilt and shame (1). Parents’ reactions do not necessarily correspond to the degree of severity of the child’s diagnosis (2). Stress, anxiety and suppressed grief can be obstacles to forming a parental attachment to the child and to a natural parent-child interaction (3).
In order to prevent parents’ emotional strain from becoming a protracted burden, and to foster an attachment between the parent and child, it is essential that nurses have relational competence, as well as good communication skills and effective methods for conveying information. Relational competence is the set of skills, abilities, knowledge and attitudes needed to establish, develop and repair relationships between people (4).
Communication tools
There is much to suggest that communication tools based on empathy, such as the Empathetic Communication principle, boost nurses’ skills and confidence in conversations with parents (5, 6). Empathetic Communication was devised by Lisbeth Holter Brudal and entails the gradual building of dialogue. The method is a process in which the nurse becomes attuned to the parents and tries to understand their inner lives. The core elements of the method are the parents’ narrative and their mental reality as well as their need for existential validation.
Empathetic Communication as a tool has an overarching goal to promote health, and it is partly based on Aaron Antonovsky’s sense of coherence theory. The goal is for the parents to achieve a sense of coherence that is characterized by three dimensions: comprehensibility, manageability and meaningfulness (6).
Open communication in family-centred care
Communication is also an essential aspect of family-centred care. Family-centred care is recognized as a fundamental approach to care for families with sick children. The core elements are the family’s right of access to care, and the parents’ abilities and emotional well-being. Parents’ perceptions of the efficacy of the care and of themselves as the child’s most important care person are also important elements of family-centred care (7, 8).
Communication between nurses and parents in an NICU poses special challenges due to the stressful situation in which the parents find themselves. Another element that represents a challenge is the complexity of the high-tech environment of the unit (9). Open communication is a fundamental principle for successful family-centred care. Achieving open communication is a challenge (10), and research shows that there is a need to foster the communication between nurses and parents (9, 11, 12).
Qualitative research has been conducted both in Norway and internationally on mothers’ and fathers’ experiences with and perceptions of their stay in an NICU (13, 14). There are studies of nurses’ and parents’ experiences of the relationship in the cooperation (15, 16) and the importance of a supportive relationship (17). However, we have not found any phenomenological studies that focus on nurses’ descriptions of what is important in the encounters and conversations with parents of a sick newborn baby who is admitted to an NICU.
A phenomenological approach is appropriate when trying to gain an understanding of individual experiences of people that cannot be measured or understood through causal relationships. The aim is to develop knowledge about people’s experiences within a particular field (18). The purpose of our study was to describe a group of nurses’ experiences of what is important in the encounters and conversations with parents of a sick newborn child. The research question presented in the study was as follows:
‘What do nurses consider to be important in the encounters and conversations with parents of a sick newborn child?’
Method
Design
The study has a qualitative design with a phenomenological approach, and data were obtained through individual interviews. According to phenomenological philosophy, our consciousness is always directed towards something. This means that we experience different phenomena based on how they present themselves to us. The descriptive phenomenological research method aims to gather accurate descriptions of how a person experiences a phenomenon. Here, the phenomenological reduction is an important prerequisite. Prior knowledge of the phenomenon being studied must therefore be set aside in order to produce an unbiased description. This requires the researcher to describe the experiences of the informants without interpreting them based on his or her own experiences (18).
Sample
The criteria for inclusion in the study were that informants had to be a paediatric nurse or a nurse with at least two years’ experience from an NICU. Recruitment took place from September to November 2013 at an NICU in Southeast Norway. Five female nurses between the ages of 30 and 50 reported an interest in participating, and all were included. Four of these nurses had further education in paediatric nursing.
Data collection
We conducted individual interviews in the autumn of 2013 at the informants’ workplace. The informants were asked two open-ended questions:
- Can you give as detailed a description as possible of an encounter in which you felt you had a good conversation with parents of a sick newborn child?
- Can you describe an encounter where you did not have such a successful conversation?
In order to obtain as rich descriptions as possible, we asked questions like ‘Would you like to tell me more about it?’, ‘Can you give a reason for it?’ and ‘What did you think then?’. The interviews lasted up to 47 minutes. We made audio recordings of the interviews and transcribed the data verbatim shortly after each interview.
Analysis
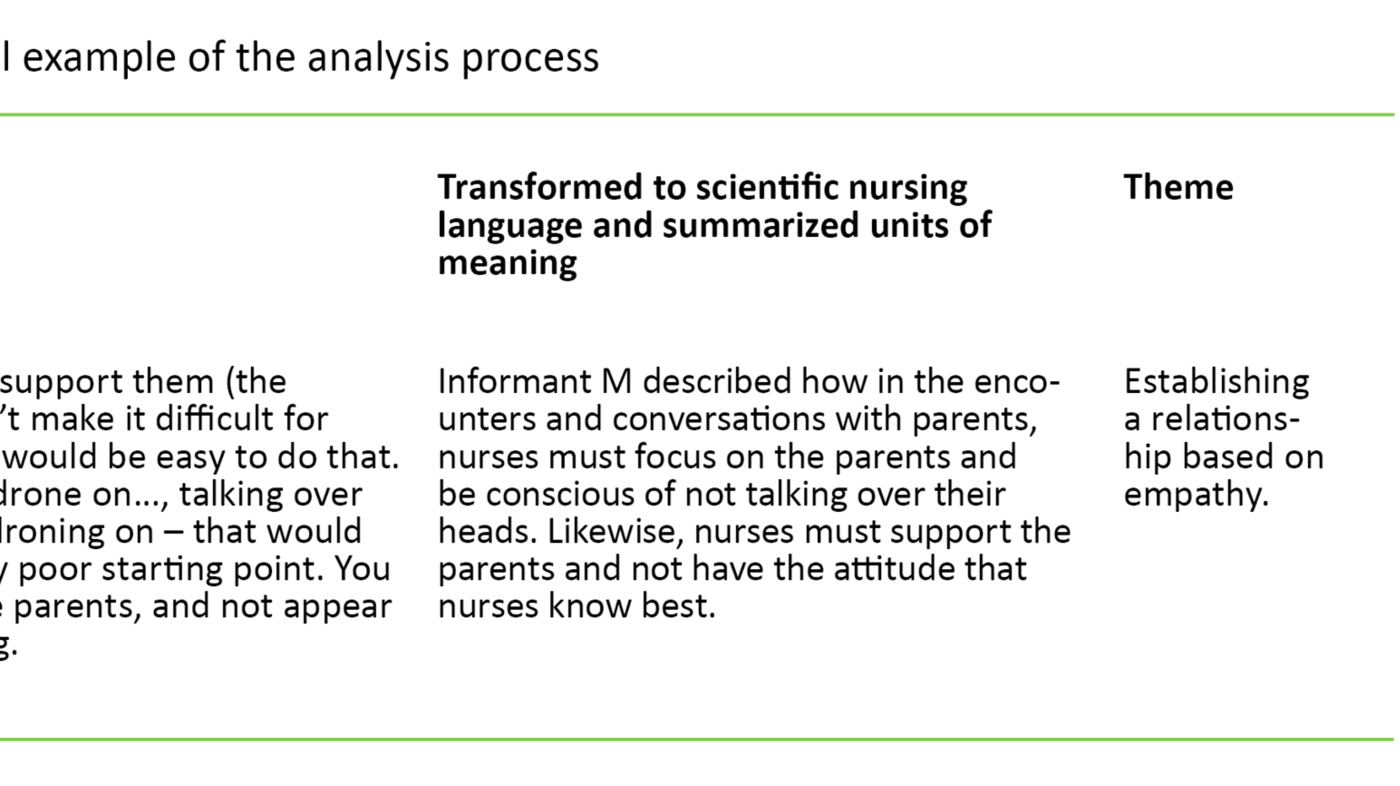
We carried out the analysis process according to the four steps in Giorgi’s (18) descriptive phenomenological research method. The interview text was read several times with a phenomenological reduction in order to gain an overall impression. In order to make the data more manageable for further analysis, we identified units of meaning in which there was a natural division in content. The everyday language in the units of meaning was transformed into scientific nursing language. We transformed the text using imaginary variations, where the aim was to establish as exact a description of the units of meaning as possible, with correct scientific language.
According to Giorgi (18), imaginary variations entail a given phenomenon being varied freely in its possible forms. The constant in the different variations is the essence of the phenomenon. We also rewrote the text from first to third person in order to create greater distance to the data material. Finally, we summarized transformed units of meaning that addressed the problem, and related them to each other, i.e. we identified common features of the interviews. These common features formed the general structure of the phenomenon. Table 1 shows a practical example of the analysis process.
Research ethics
The Norwegian Centre for Research Data (NSD) was notified of the study. We were given permission to carry out the study by the R&D unit at the hospital in question. The informants received oral and written information about the study, and were informed about voluntary participation and the option to withdraw. We also obtained written informed consent.
Results
General structure
In the informants’ encounters with parents, the informants considered it essential to establish a relationship based on empathy, where the parents were treated as individuals, where the mutual exchange of information was facilitated, and where the parents’ sense of coping was fostered. When these aspects were present, the informants perceived the encounters and conversations as good. Where these aspects were absent, the encounters and conversations were described as less successful.
Establishing a relationship based on empathy
The informants emphasized that the relationship aspect was a core element of the encounter with the parents. They believed that the parents appreciated the empathy they were shown, and that it gave the parents the courage to confide in them. In order to establish an empathetic relationship, the informants pointed out that nurses must be attentive to the parents and not have the attitude that nurses know best. They must also take care not to talk over the parents’ heads. They must show understanding for the parents being in a difficult situation.
Furthermore, they must know that crisis and stress reactions can manifest themselves in different ways, and that being separated from the child is often extremely challenging. These factors were particularly applicable when the parents felt they were in a crisis under circumstances that the informants considered to be straightforward and which they knew would have a good outcome. The informants also emphasized that adopting an empathetic approach would stop the nurses from having unrealistic expectations of the parents and regarding the parents as difficult. Where there was no such comprehension, the relationship could be adversely affected. Accepting and being open to and tolerant of the different reactions of the parents were considered important for establishing a relationship based on empathy.
Treating the parents as individuals
Another important aspect of the encounters and conversations with the parents was to make them feel that they were ‘seen’, for example by showing them that they cared about their child and the particular situation of that child. The informants considered it essential to act according to the individual situation and reactions of the parent, since all parents differ and have different needs that change during the hospital stay. The opportunity to focus fully on the parents is a prerequisite for being able to treat the parents as individuals. When the nurses also had to concentrate on other work at the same time, giving their full attention to the parents often presented a challenge. For example, other tasks sometimes had to be prioritized over the sick child or other acute events.
Other challenges to the nurses’ time included where the nurses were responsible for several children and parents or where they had different procedures or documentation to adhere to. In order to be able to give their full attention to the parent, there was occasionally a need to move the setting from the incubator or the child’s bedside in the unit. The informants said it was important to take the parents out of the unit to a suitable room with comfortable chairs, for example, in order to allow them to focus on the parents as individuals.
Facilitating the mutual exchange of information
The informants felt that it was crucial to facilitate the mutual exchange of information in order to adapt the information to the individual’s aptitudes and needs, and to show understanding for the child’s situation in the conversations with the parents. The informants wanted to keep the parents informed of the child’s situation and development from their first meeting right up until the child was discharged.
They told of the child’s need to have the parents with them at the hospital, and what they thought was best for the child. The informants often found that the parents did not take on board all of the information they were given. They therefore recognized the importance of identifying how they could best provide the individual parent with explanations that he or she could understand. In order to identify what was important to the individual, it was crucial to listen actively and make sure they understood the parents. The informants wanted to find a balance so that they could facilitate the best possible overall situation for the whole family.
Helping parents to cope
The informants described how when the child was admitted to the NICU, the parents entered an unknown world that could feel confusing and unmanageable. They felt it was important to facilitate conversations about the parents’ experiences and perceptions. They could, for example, encourage the parents to share their stories and versions of what had happened, and then ask follow-up questions about how they felt or what they thought about this. The informants felt that this could help the parents to express their emotions and thoughts.
In the conversation with the parents, the nurses discussed how the parents could take part in the care, and provided information and guidance. Everyone agreed that involving the parents in the care of their child helped parents to feel that they were coping and helped them to form an attachment to their child. They pointed out that it had to be on the parents’ terms. When the informants were unable to meet the parents’ needs and do what was right for them, it sometimes led to insecurity, stress and a negative experience for both the parents and the informants.
Discussion
All of the informants described how it was crucial to establish a relationship based on empathy in the encounter with parents. Earlier research confirms this, and highlights the importance of nurses showing empathy towards the parents (19, 20). The experience of being met with empathy fosters and strengthens the individual’s mental resources in a difficult situation (21). Empathy gives parents the resolve to continue and a zest for life (6). New knowledge about mirror neurons and the mirror neuron system has introduced new aspects to the concept of empathy. Evidence suggests that empathy is an innate ability to recognize the emotions and intentions of other people (22).
Empathy has both a cognitive and emotional aspect. Based on the principle of Empathetic Communication, it may be said that through a process characterized by mutual reflection and dialogue, the nurse can start to comprehend what the parents are going through by recognizing their feelings and intentions. Only when the nurse recognizes the parents’ inner world does he or she have the opportunity to understand the parents. This recognition adds a distinctive quality to the relationship and dialogue between nurses and parents, which gives a sense of cohesion and equality. Both have the same experience simultaneously (6).
The informants describe how they met the parents with an open, empathetic and receptive attitude. The parents are the key figures in the relationship, and as such will sense the intention to help, which is implicit in such behaviour. Empathy can arise as a result of such a process because, in practice, it is about the nurse attuning to the parents and taking part in their reality (6).
Failing to recognize that the parents are having a crisis
The informants’ descriptions of the significance of the relationship concur well with other studies (15-17). Several studies have, for instance, shown that parents of sick newborn babies have a crisis reaction to childbirth and the post-natal period (1, 23). Hillgaard et al. (2) examine whether some crises are not discovered because health professionals consider the behaviour to be normal for that particular person. They interpret the situation as having to do with difficult parents, and fail to recognize that the parents are having a crisis. In order to be able to provide effective help for the parents, the nurse must have knowledge of the parents’ reactions in connection with having a sick newborn baby (24). The nurse must also use a communication tool, such as Empathic Communication (5, 6).
All of the informants emphasized the importance of making parents feel that they are seen. Being seen gives an immediate sense of being understood and validated (25). When the nurse starts to comprehend the parents’ understanding, the parents can feel valued. This strengthens their resolve and self-esteem (6). Earlier research suggests that nurses who are sensitive and supportive to parents’ needs can foster parents’ self-confidence and strengthen their response to the child’s needs (26). This is because when parents have self-confidence and are able to cope they can more quickly adapt their response to the child’s signals (27).
The informants also emphasized that giving their full attention to the parents was a prerequisite for identifying the individual’s needs. Such attention to the parents requires the ability and capacity to be present and mindful (6). When the nurse focuses on the parents’ thoughts and perceptions, they are signalling that the parents are important. The role the parents have as a caregiver for the child is asserted (28).
Information both ways
Enabling the mutual exchange of information between parents and nurses was emphasized as a key aspect of the conversations. Through the mutual exchange of information, the nurse gains a better understanding of the parents’ reality and what is important for the individual (6). Such understanding of the parents’ problems, resources and needs thus makes it possible for the nurse to adapt the amount and type of information that is preferred by the parents (29, 30). In this way, an empathetic dialogue is created (6). Duncan (31) refers to this as client-directed and outcome-informed practice. Attention is directed to the information shared by the parent, and to giving professional feedback based on the fact that the parents are the key figures in the dialogue.
In order to foster the parents’ sense of coping, it was important for the informants to encourage the parents to share their stories and ask follow-up questions about what the parents felt and thought. This is also in line with the communication tool Empathetic Communication. Parents are given the opportunity to express and convey their own feelings and thoughts in an empathetic relationship that can foster a sense of coping. By mirroring what the parent says, the nurse can create a valuable process in which tension and stress are dampened, and mental strength is further developed (6).
Parents need to express their perceptions and be heard in order to be able to process impressions and reactions in relation to what has happened (32). They can receive information and concentrate on caring for the child more effectively once they have processed their own perceptions. Such processing may affect how they bond and interact with the child (33, 34).
All the informants felt that involving the parents in the care of the child helped give the parents a sense of coping and helped them bond with the child. Informants described how they talked to and guided the parents in what was best for the child and how they could take part in the care. Research shows that early intervention aimed at learning parental interaction and sensitivity to the child’s signals can foster good mental development in the sick newborn child and a sense of coping in the parents (3, 23, 34-36).
Methodological considerations
One weakness of the study is that we only have five informants. The ideal would have been to include more informants from more NICUs. According to Giorgi (18), however, three in-depth interviews can be sufficient for a phenomenological study. Thus, five informants in the study can be a sufficient basis for illuminating the phenomenon.
A researcher will always have a certain influence on the data material, and it may, therefore, be unrealistic to assume that all prior knowledge will be set aside. The first author has an understanding of the phenomenon as she has the same professional background as the informants. She also works in the same type of unit, and has opinions about the phenomenon being investigated. It is thus important for the authors to have a reflective relationship to their own preconceptions and to try to use solely the informants’ experiences.
The convergence of findings from the various interviews helps to enhance the reliability of the study. The findings also concur with other research in the field. The reliability of the study is further enhanced by the fact that all of the authors have been involved in the analysis. The first author conducted the analysis in close collaboration with the co-authors. We followed the analytical steps carefully, which is essential for obtaining valid findings, according to Giorgi (18).
Conclusion
This study has thrown light on a group of nurses’ experiences in terms of what is important in the encounters and conversations with parents of sick newborn children in an NICU. The results emphasize that the nurses are responsible for establishing an empathetic relationship with the parents and treating each parent according to their own situation in order to help them cope with the vulnerable situation in which they find themselves.
The informants’ descriptions indicate that nurses at NICUs can benefit from adopting the communication tool Empathetic Communication. The method is in many ways consistent with the findings of the study: information must be adapted to the parents, the parents are the real experts on themselves, there is no such thing as ‘difficult parents’, and coping gives parents a sense of security.
Further research is needed to investigate whether training in the communication tool Empathetic Communication can help develop nurses’ relational competence and communication skills, thereby facilitating good encounters and conversations with parents of a sick newborn child.
References
1. Turan T, Basbakkal Z, Özbek S. Effect of nursing interventions on stressors of parents of premature infants in neonatal intensive care unit. J Clin Nurs 2008;17(21):2856–66.
2. Hillgaard L, Ravn L, Keiser L. Sorg og krise. Gyldendal, Copenhagen. 1999.
3. Kaaresen PI, Rønning JA, Ulvund SE, Dahl LB. A randomized, controlled trial of the effectiveness of an early-intervention program in reducing parenting stress after preterm birth. Pediatrics 2006;118(1):9–19.
4. Spurkeland J. Relasjonskompetanse som grunnlag for å skape resultater i arbeid og på skole. Available at: http://forebygging.no/Artikler/2015/Relasjonskompetanse/(downloaded 16.05.2017).
5. Nerdrum P. Training of empathic communication for helping professional. (Dissertation). University of Oslo, Oslo. 2000.
6. Brudal L. Empatisk Kommunikasjon – Et verktøy for menneskemøter. Gyldendal Akademisk, Oslo. 2014.
7. Johnson, BH. Family-centered care: Four decades of progress. Families, Systems & Health: The Journal of Collaborative Family HealthCare. 2000;18(2):137–56.
8. Griffin T. Family-centered care in the nicu. J Perinat Neonatal Nurs. 2006;20(1):98–102.
9. Wigert H, Dellenmark MB, Bry K. Strengths and weaknesses of parent-staff communication in the NICU: a survey assessment. BMC Pediatr. 2013;13:71.
10. Johnson AN. Promoting maternal confidence in the nicu. Journal of Pediatric Healthcare. 2008;22(4):254–7.
11. Boss RD, Urban A, Barnett MD, Arnold RM. Neonatal Critical Care Communication (NC3): training NICU physicians and nurse practitioners. Journal of Perinatology: Official Journal of The California Perinatal Association. 2013;33(8):642–6.
12. Griffin T. A family-centered «visitation» policy in the Neonatal Intensive Care Unit that welcomes parents as partners. J Perinat Neonatal Nurs. 2013;27(2):160–7.
13. Fegran L. Parents and nurses in a neonatal intensive care unit: the development of a mutual beneficial partnership in the care of the infant. (Dissertation). University of Oslo, Oslo. 2009.
14. Wigert H, Johansson R, Berg M, Hellström AL. Mothers' experiences of having their newborn child in a neonatal intensive care unit. Scand J Caring Sci. 2006;20(1):35–41.
15. Fegran L, Fagermoen MS, Helseth S. Development of parent-nurse relationships in neonatal intensive care units – from closeness to detachment. J Adv Nurs. 2008;64(4):363–71.
16. Reis M, Rempe G, Scott S, Brady-Fryer B, Van Aerde L. Developing nurse/parent relationships in the NICU through negotiated partnership. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2010;39:675–83.
17. Gooding J, Cooper L, Blaine A, Franck L, Howse J, Berns S. Family support and family-centered care in the neonatal intensive care unit: origins, advances, impact. Semin Perinatol. 2011;35:20–8.
18. Giorgi A. The descriptive phenomenological method in psychology: a modified Husserlian approach. Duquesne University Press, Pittsburgh, PA. 2009.
19. Nordby H, Nøhr Ø. Communication and empathy in an emergency setting involving persons in crisis. Scand J Trauma Resusc Emerg Med. 2008;16:5–11.
20. Ammentorp J, Kofoed P, Laulund L. Impact of communication skills training on parents’ perceptions of care: intervention study. J Adv Nurs. 2011;67:394–400.
21. Snyder CR, Lopez SJ. Handbook of positive psychology. Oxford University Press, New York. 2002.
22. Rizzolatti G, Sinigaglia C. Mirrors in the brain – how our minds share actions and emotions. University Press, Oxford. 2008.
23. Mazurek MB, Feinstein NF, Alpert-Gillis L, Fairbanks E, Crean HF, Sinkin RA et al. Reducing premature infants’ length of stay and improving parents mental health outcome with the Creating Opportunities for Parent Empowerment (COPE) Neonatal Intensive Care Unit Program: A Randomized, Controlled Trial. Pediatrics. 2006;21:1414–27.
24. Wakely LT, Rae K, Cooper R. Stoic survival: the journey of parenting a premature infant in the bush. Rural & Remote Health. 2010;10(3):1–10.
25. Stern DN. Det nuværende øjeblik i psykoterapi og hverdagsliv. Hans Reitzel, Copenhagen. 2004.
26. Flacking R, Ewald U, Nyqvist KH, og Starrin B. Trustful bonds: A key to «becoming a mother» and to reciprocal breastfeeding. Stories of mothers of very preterm infants at a neonatal unit. Soc Sci Med. 2006;62(1):70–80.
27. Karl DJ, Beal JA, O'Hare CM, Rissmiller PN. Reconceptualizing the nurse's role in the newborn period as an «attacher». MCN Am J Matern Child Nurs. 2006;31(4):257–62.
28. Tandberg BS. Møtet med familien på nyfødtavdelingen. In: Tandberg BS, Steinnes S. (eds). Nyfødtsykepleie 1. Syke nyfødte og premature barn. Cappelen Damm, Oslo. 2009. s.224–43.
29. Jones L, Woodhouse D, Rowe J. Effective nurse parent communication: a study of parents’ perceptions in the NICU environment. Patient Educ Couns. 2007;69(1-3):206–12.
30. Bruns DA, McCollum JA. Partnerships between mothers and professionals in the NICU: caregiving, information exchange, and relationships. Neonatal Netw. 2002;21(7):15–23.
31. Duncan B. The Heroic Client. Jossey-Bass, San Francisco. 2004.
32. Orapiriyakul R, Jirapaet V, Rodcumdee B. Struggling to get connected: The process of maternal attachment to the preterm infant in the neonatal intensive care unit. Thai J Nurs Res. 2007;11(4):251–63.
33. Eriksson BS, Pehrsson G. Evaluation of psycho-social support to parents with an infant born preterm. J Child Health Care. 2002;6(1):19–33.
34. Kaaresen PI, Rønning JA, Tunby J, Nordhov SM, Ulvund SE, Dahl LB. A randomized controlled trial of an early intervention program in low birth weight children: outcome at 2 years. Early Hum Dev. 2008;84(3):201–9.
35. Rauh V, Achenbach T, Nurcombe B, Howell C, Teti D. Minimizing adverse effects of low birthweight: four year results of an early intervention program. Child Dev. 1988;59(3):544–53.
36. Ravn I. The effects of an early intervention on outcomes in mothers, fathers and moderately and late preterm infants during the infants’ first year of life – A randomized controlled trial. (Dissertation). University of Oslo, Oslo. 2011.










Comments