Communication training course with simulation
Simulation based communication courses can give improved communication skills and increased understanding of how the communication model may be used.
Background: Patients hospitalised in acute care settings are vulnerable and may experience not being confirmed as a person. If the nurses possess good communication skills, that might have a great significance for the patients. Communication courses have been shown to enhance health care professionals’ communication skills, when simulation based learning have been applied.
Objective: To describe how nurses in a postoperative care department evaluated a simulation based communication course.
Method: We developed a simulation based communication course consisting of a theoretical lecture about a confirming communication model and simulation. A survey was conducted 6 months after the course.
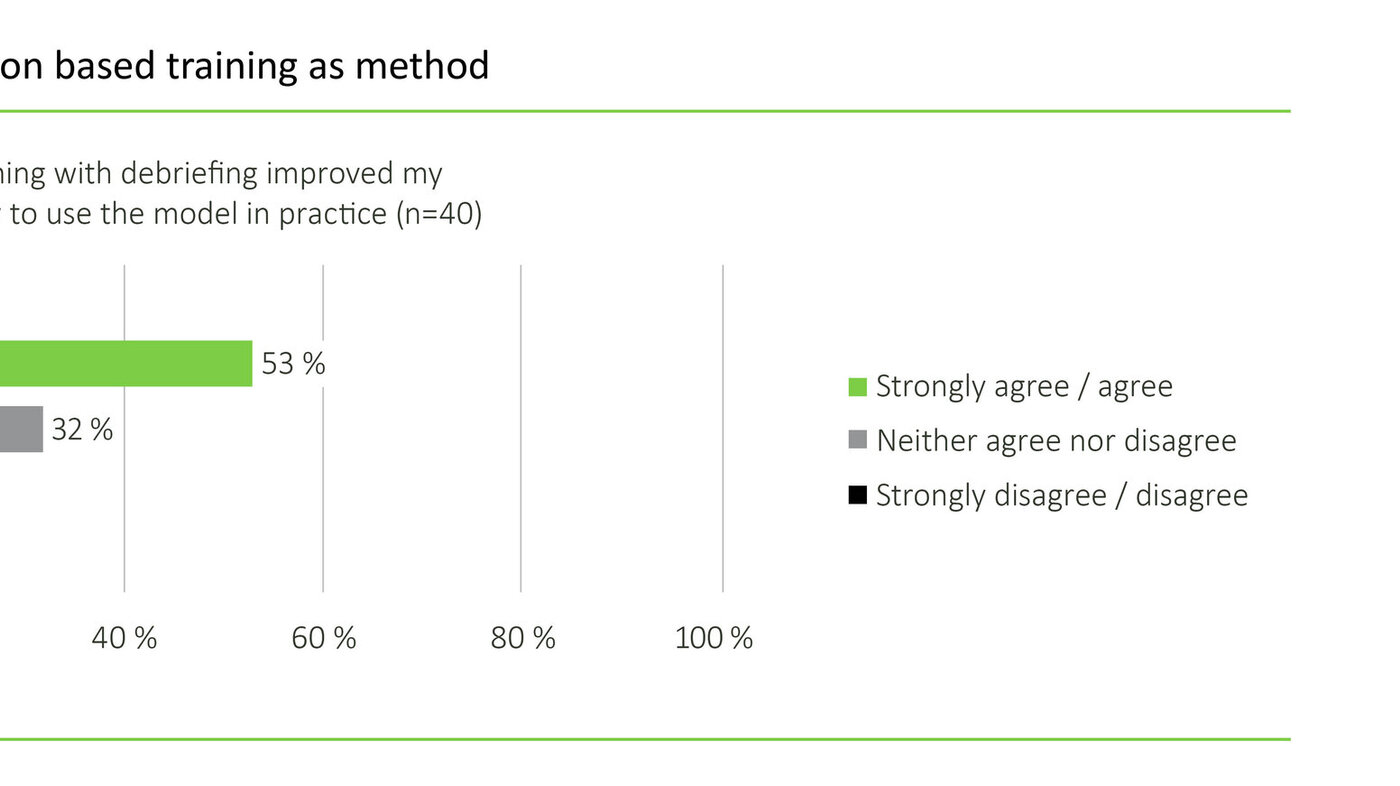
Results: 49 nurses attended the course and 40 responded to the questionnaire. 53 % reported that the simulation improved their comprehension about how to use the model. 33 % reported their communication skills improved after the course.
Conclusion: The study indicates that simulation improved the comprehension about how to use the communication model.
Introduction
Advanced communication skills are considered fundamental to the intensive care nurse’s competence (1, 2). Purposeful communication is one of several topics in the development of nurses’ clinical competence (3). Patients, nurses, and family members have described the importance of good communication skills for nursing quality and patient satisfaction (4–6).
Little research has been done on communication methods or models to guide health care professionals in their interaction with critically ill patients. However, some studies have shown improvement of the quality of communication between intensive care nurses and patients and family members in end-of-life care (7). Patients are at their most vulnerable when admitted to an intensive care unit (8, 9). The result of surgery may be uncertain, and the patient may experience loss of personal control (10). Several studies show that various measures may improve intensive care nurses’ communication skills, and the target group is the voiceless mechanically ventilated patient (11, 12), rather than the conscious and alert postoperative patient who is able to express his or her needs.
Acute, critically ill patients are to a greater extent awake and communicative when they receive non-invasive mechanical ventilation or invasive mechanical ventilation and this demands greater attention the patient’s communication needs. These patient groups are present in Post-anaesthesia care units as well. If health personnel do not communicate well, the patients may experience this as not being taken seriously and feel that their psychosocial needs are not met, which may cause experiences of worthlessness, patient dissatisfaction, and depression (8, 13–15). However, not much knowledge is available on how nurses achieve communication competence within the professional field of intensive care nursing.
Confirming patients’ communication may further health and improve the patients’ possibilities for collaboration (14, 15). Confirming communication skills is one way of recognising the patient (16). Listening, understanding, acceptance, respect and tolerance are, in addition to confirmation, ingredients in the concept of recognition, which is philosophically anchored in existentialism. Recognition is intersubjective, as it has the experience of the other as its basis (17). Eide and Eide (16, p.220) define confirming skills as «skills that communicate in words that one has seen and understood the core of what the other communicates. Being seen and understood are confirming in themselves». The aim is to communicate immediate, confirming, and recognising answers to what the patient expresses (16).
In order to develop communication skills further, simulation or a traditional academic didactic approach may be used, although much seems to indicate that simulation based learning is preferable (18–20). Simulation as a way to learn communication has resulted in improved skills for students at basic level nursing (21, 22), for health personnel on oncological wards (23), and for nurses in psychiatric wards (24).
Nurses with good communication skills may be of great importance to the patients.
Simulation based learning may be divided into two main categories: for use in developing technical skills and for use in developing non-technical skills (25). Examples are treating traumatised patients (26, 27), advanced emergency heart and lung resuscitation (28), and to further patient safety in intensive care nursing (29, 30). Communication skills also entail awareness in relation to other types of simulation – such as training to achieve ethical competence and to develop communication skills needed in complex patient situations (31). We have been unable to find simulation used to further develop verbal and non-verbal communication skills in Post-anaesthesia care units.
Simulation based learning as method is anchored in learning theories such as Kolb’s circle and Bloom’s taxonomy; these theories can shed light on why simulation is considered an effective learning method (32). Knowledge and understanding resulting from simulation are basic measures of competence. If the participants are able to use and analyse what they have learned, this is a better measure of competence. The way the participants use former experience and integrate the new into their thinking is of importance to the learning outcome (32). Simulation consists of the phases briefing, scenario training, and debriefing, and is a challenging way to learn (33). The aim of simulation is to achieve a change in practice, sustained over time (32–34).
Simulation based learning turns out to be a method for improving patient outcomes (35). Participants have demonstrated skills in emergency procedures that they have learned in simulation, up to one year later (36). This suggests that simulation is an appropriate method for achieving quality improvement in practice.
We were inspired to strengthen the professional practice on the ward by adapting confirming skills to a communication model for patients on a Post-anaesthesia care unit. On the unit in question, there were no specific methods implemented for communicating with the awake and communicable patient or with the awake patient receiving invasive mechanical ventilation. We were recommended to use simulation rather than traditional teaching methods (19, 23), and we developed a one day simulation-based course for teaching confirming communication skills. The course consisted of a theoretical introduction to the communication model, and scenario training in the use of confirming skills.
The purpose of the study is to describe how nurses on a postoperative ward assessed the utility of a simulation-based communication course in which the aim was practical use of confirming communication skills in the encounter with the postoperative patient.
In this article, we want to explore whether the simulation helped the nurses gain increased understanding of how the communication model may be used in practice, and whether the nurses’ communication skills improved after the simulation.
Design and method
The study has a quantitative design and the method used was a survey by questionnaire. This method is recommended for gaining knowledge of a larger group’s opinions and behaviour in encountering a phenomenon (37).
The study is part of a collaborative project between a Post-anaesthesia care unit at a university hospital and the postgraduate education in intensive care nursing at a university college in Eastern Norway. The collaborative project aimed to strengthen the students’ practice supervision and strengthen the professional practice at the unit. The communication course was held in February 2013.
Population and sample
The population consisted of 60 nurses on a Post-anaesthesia care unit, of which around 80 per cent are intensive care nurses. The sample in this survey consisted of 49 nurses participating in the communication course.
Context
The postoperative ward treats and nurses patients after planned and acute operations and traumas. The majority of patients stay for less than one day before they are transferred to a general ward or other surveillance or intensive care unit in the hospital.
The communication course
Simulation-based learning was used, and the course day started with 60 minutes of theory presented by third author. The communication model was based on Eide and Eide’s (16) description of confirming skills in communication, with examples from postoperative practice (table 1).
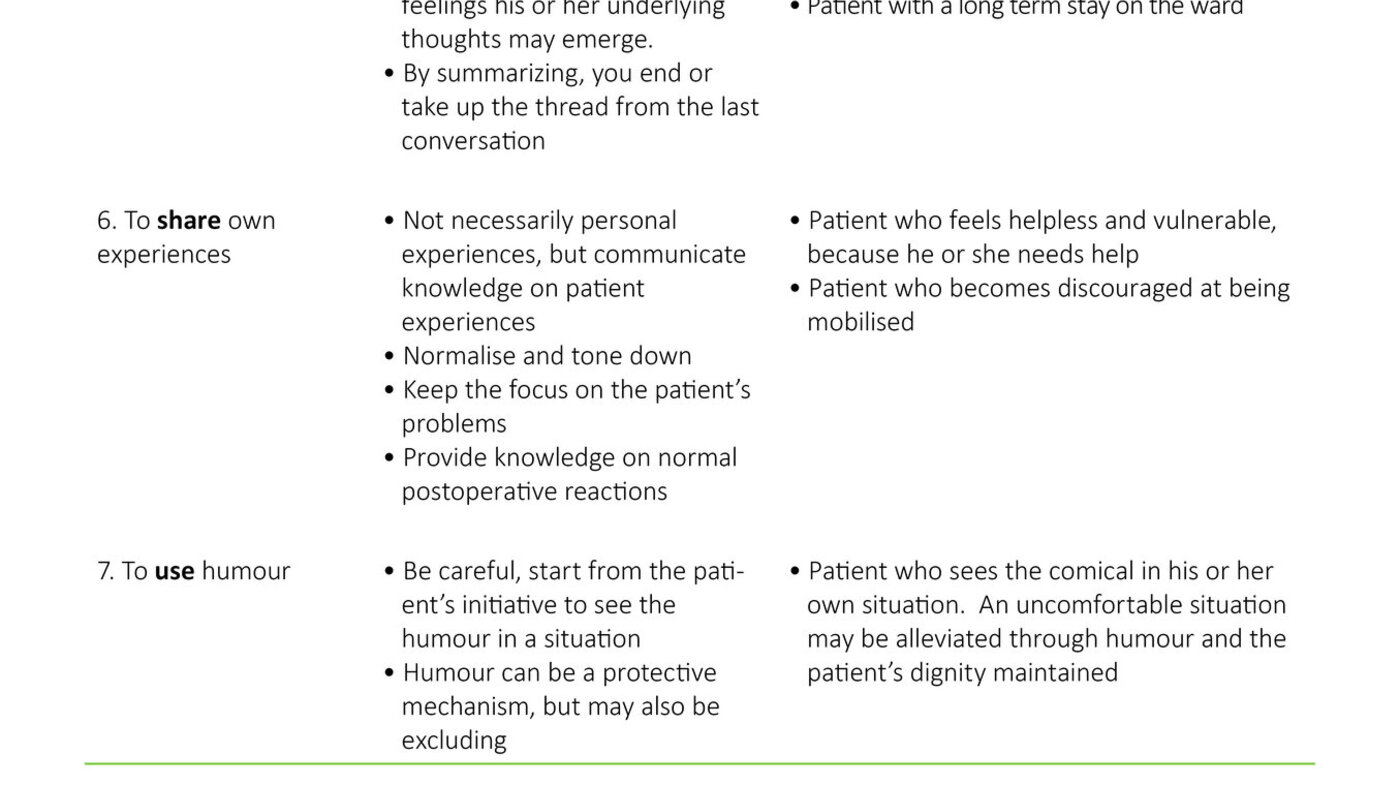
The theory lecture was followed by video recorded simulation with debriefing, lead by facilitators. The desired learning outcome from the simulation was the ability to use confirming communication skills. Following recommendations that smaller groups may increase the participants’ engagement, the nurses were divided into groups of 6 – 8 during the simulation (18). The course lasted four days, with two groups on each course day. One and a half group had scenario training in training areas with video recording. The observers were present in the same room. The other groups had scenario training in a simulation laboratory, with a separate room for the observers. The scenarios were created from a postoperative context and lasted 5-8 minutes.
The scenarios had as their basis the adult, alert and orientated patient. All participants participated in one scenario, and acted either the patient or the nurse. A «timeout» was possible for conferring with the facilitator during the scenario training. The observers were in a separate room with video transmission and were asked to observe the use of specific confirming communication skills. The debriefing was about the nurse’s and the patient’s experience. The participants did not have to watch the video playback of themselves during the debriefing, which lasted around 30 minutes. The course was pilot tested with an evaluation that resulted in a better flow in the scenarios, among other things.
Confirming communication skills are one way of acknowledging the patient.
The questionnaire
The theoretical foundation used to develop the questionnaire, in collaboration with a statistician, was communication theory, theory on use of simulation, and research theory (38,39). To operationalise the research questions we developed a form with 33 questions, of which one was open. A variable is a characteristic of a phenomenon and may have various measurement levels (40). The variables were on the nominal level and the ordinal level. The nominal variables were: nurse/intensive care nurse, experience as nurse/intensive care nurse, and prior participation in communication courses. The ordinal variables were: use of confirming skills, improvement of communication skills, utility for supervision of students, utility value in typical patient situations, and increased understanding of the model learned through simulation training.
The ordinal variables were measured with a 5 point Likert scale (37), where agreement on statements are graded from «strongly disagree» (one), «disagree» (two), «neither disagree nor agree» (three), «agree» (four) and «strongly agree» (five). We chose gradation three as a neutral answer alternative on recommendation from the statistician. The questionnaire was tested in a pilot test (n=5) and revised based on feedback received. The questionnaire was distributed to the nurses six months after the communication course, in September 2013.
Ethical considerations
Simulation is a method in which nurses are observed by colleagues, and this was used as learning arena. Having one’s behaviour and actions evaluated leaves the participant vulnerable, and this must be taken into consideration. We thus tried to establish a caring atmosphere for the participant all through the process. The communication course was obligatory for the nurses. We informed them that the video recording would be erased immediately following debriefing.
The ward administration gave permission to evaluate the collaborative project. The Data Protection Officer at the hospital approved the project as a quality improvement study. The data from the survey were stored on the hospital’s research server in accordance with guidelines from the Data Protection Officer. Data were anonymised and will be erased after the data have been used. The nurses were informed orally and in writing on the purpose of the survey and that participation was voluntary. Returning the questionnaire was considered as consent from the respondents. It was not possible to withdraw the questionnaire, as it was impossible to trace it back to the individual participant. This was considered the most «secure» way of anonymising the findings in an ethically responsible manner.
Analyses
We used the programme Statistical Packages for Social Sciences (SPSS) version 18 to register the data. We did frequency analyses to show the distribution of the nurses’ answers on each individual variable (40). The frequency distributions are shown in Figures 1-3. In the figures the Likert scale values are combined from five to three categories to simplify the presentation. We did the analyses and the presentation of the results in text and figures in accordance with advice from the statistician.
Results
Demographic data
Forty-nine nurses participated in the communication course, and 40 nurses (82 per cent) responded to the questionnaire (n=40). Twenty-nine nurses (74 per cent) were intensive care nurses, and 33 (83 per cent) had participated in a communication course earlier in their education.
Simulation as learning method
53 per cent of the nurses strongly agreed or agreed with the statement that the simulation improved their understanding of how to use the communication model in practice (see Figure 1).
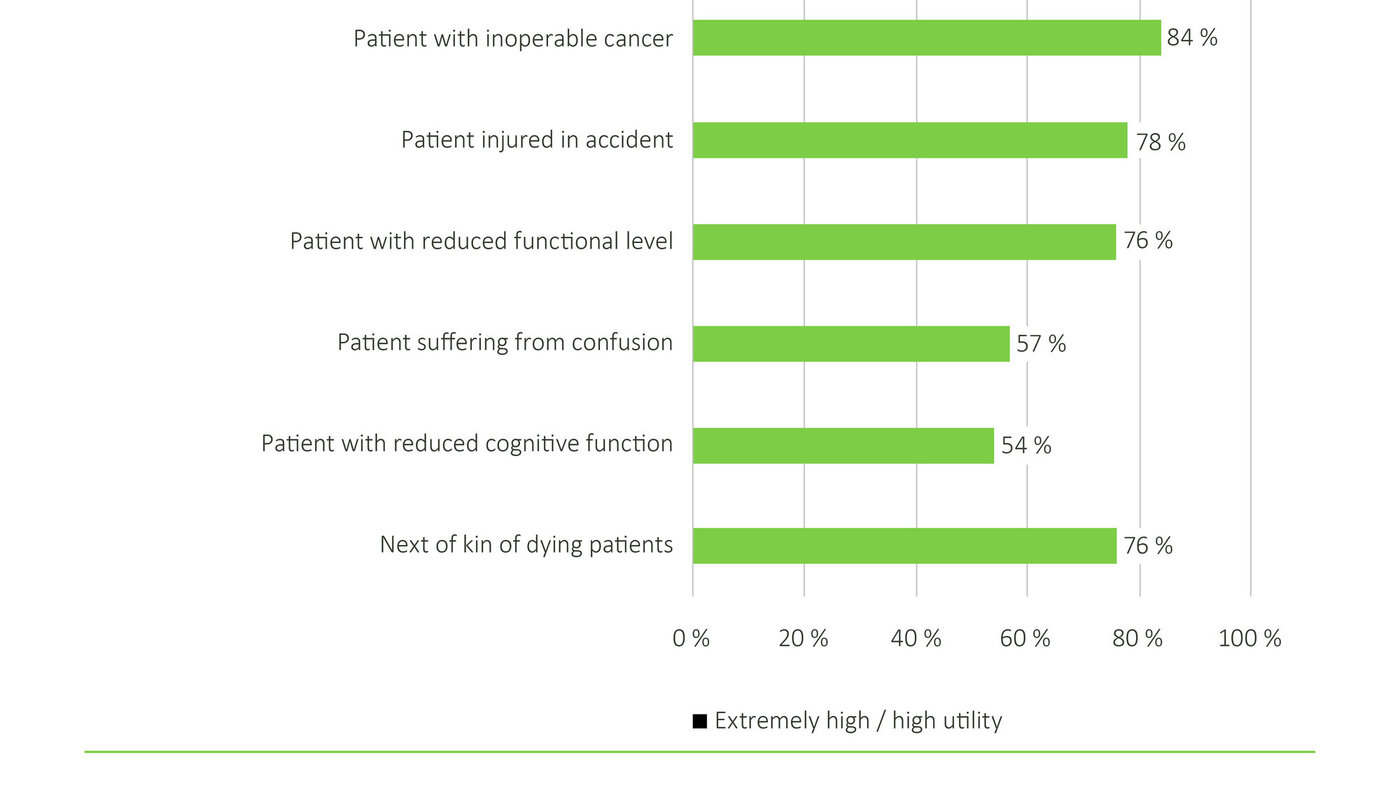
The communication model had highest utility for the nurses in their encounter with patients with inoperable cancer, and patients injured in an accident (see Figure 2).
Communication skills following the course
33 per cent of the nurses strongly agreed or agreed that their communication skills had improved after the course, while 47 per cent neither agreed nor disagreed with the claim (see Figure 3).

Discussion
Simulation as learning method
53 per cent of the nurses reported that the simulation improved their understanding of how to use the communication model in practice. Several factors may have influenced this result, such as aspects of simulation as learning arena and how nurses later integrate what they have learned in concrete patient situations.
Experience with simulation training generally suggests that some will find the method somewhat uncomfortable. After completion of the scenario it is subject to reflection in a debriefing session to bridge the gap between knowledge achieved through simulation and its use in practice (33,34). The facilitator has an important role in making such learning through simulation comfortable and useful to the participants (34). In our study experienced facilitators lead the debriefing, and they were related to the ward. We focused on that the participants were there to learn, not to be evaluated. Security was an important factor in the learning environment and in making the participants feel comfortable. To protect the participants we emphasised confidentiality in the groups, assuring the participants that what happened there would not be communicated to the ward.
Simulation may be used to further develop communication skills.
The participants played the parts of both nurses and patients, and the learning effect of simulation may depend on how good an actor one plays against (41). Half of the nurses were unable to try out the nursing role, for practical reasons. This may have yielded a lower learning outcome for those who played only the patient role. On the other hand, it is recommended that the participants do play the patient in scenario training. That enables them to take on the patient’s perspective and may add greater realism to the scenario (41).
To watch a part of the video during debriefing has a learning effect and has been considered the «gold standard» of simulation (33, 34). However, a more recent review article points out that debriefing without a video playback may be equally effective (42). The video recording was shown with both observers and scenario participants present. The participants were free to not watch the video of themselves during the debriefing in the communication course, and several did so. Using video playback during debriefing may distract the participants from focussing on the scenario’s learning goals (42). It is therefore important, according to our experience, that judgement is used in using video playback during debriefing, especially with regard to what sequences are used for learning purposes.
Developing communication skills further
Thirty-three per cent of the nurses reported improved communication skills following the course. This may be interpreted as a low result, but 47 per cent answered «neither nor» to this question. A weakness in the study’s design is that we did not measure communication skills prior to the course. We had no control questions in the questionnaire about knowledge on confirming communication or other communication skills prior to the course. It is therefore difficult to say whether the course has resulted in improved communication skills. A pretest-posttest design could have shown a real change in, or effect on, the nurses’ skills following the communication course. A critique of this kind of design is that the effect is not necessarily caused by the intervention, but by other causal effects that cannot be controlled (37).
Being as the course was developed for students as well as nurses at the unit, the patient scenarios in the simulation may not have been sufficiently challenging for the experienced nurses. Researchers emphasise that theories such as social learning theory and adult learning theory may shed light on the way experienced persons learn, as opposed to students, in a basic training programme (43). Elements of the theories state that experienced persons are problem-focussed and use their experience to assess the new material that is presented to them. They learn based on what is useful to them in their practice, and inner motivation is important for learning. The question is whether we were able to motivate the nurses to use the skills in practice. We did, however, assess the communication model as useful in encounters with postoperative patients, such as patients with inoperable cancer, and patients injured in accidents. The participants acknowledged the utility of the skills, but maybe not of the simulation staged to learn them.
Even if the communication course turns out to improve communication skills, there is little evidence that skills learned in simulation are maintained over time in clinical practice (20,44,45). Whether great resources should be used to teach communication skills through simulation may be questioned.
However, clinical supervision has proved to maintain communication skills in oncological nursing practice (46). A resource group was established at the unit after the course to help maintain knowledge acquired in the simulation. One of several interventions was that third author was attentive to communication skills in clinical supervision with both a group of nurses with special competence in such skills and students in post graduate education. The hope is that confirming communication skills were implemented at the unit in more than one way.
The communication course is now obligatory for students in postgraduate education in intensive care nursing when in practice at the Post-anaesthesia care unit. Newly employed nurses are given an introduction to the communication model as part of their introductory programme.
The study’s weaknesses
One of the weaknesses of the study is that we used a self-developed questionnaire. We did, however, not find any already constructed questionnaire that suited our purpose, and the questionnaire was developed in collaboration with the statistician and then pilot tested. A survey like this yields knowledge of the nurses’ opinion at one point in time. One challenge with self-report studies may be a possible discrepancy between the skills the respondents report having and the skills they do in fact use in practice (37). The nurses received the questionnaire six months after the communication course. They may thus have had too little time to develop their communication skills.
Conclusion
The study suggests that simulation increased the participants’ understanding of the possible uses of the communication model, but no more than 33 per cent of the nurses considered their communication skills to have improved after the simulation. Communication, however, is very complex and encompasses more dimensions than merely confirming communication skills. In the study we chose to focus on this one communication model. The study’s design does not measure the effect on patient care directly, as this was not the purpose of the study.
There is a need for more knowledge on simulation-based communication courses to evaluate their effect and whether such courses may yield lasting improvement in communication skills.
Acknowledgments
We are very grateful to the Post-anaesthesia care unit’s nurses who took the time to answer the questionnaire. We also want to thank the Simulation Centre at Oslo University Hospital and department manager Lasse Schmidt for the use of facilities and personnel during the course. We also want to thank the facilitators. Professor Leiv Sandvik at Oslo Centre for Biostatistics and Epidemiology has guided us in the development of the questionnaire. The project is financed through collaboration funds from the University College of Oslo and Akershus.
References
1. Boykins AD. Core communication competencies in patient-centered care. ABNF J 2014;25(2):40–5.
2. Mullan BA, Kothe EJ. Evaluating a nursing communication skills training course: The relationships between self-rated ability, satisfaction, and actual performance. Nurse Educ Pract 2010;10:374–8.
3. Aari RL, Tarja S, Helena LK. Competence in intensive and critical care nursing: a literature review. Intensive Crit Care Nurs 2008;24:78–89.
4. Broyles LM, Tate JA, Happ MB. Use of augmentative and alternative communication strategies by family members in the intensive care unit. Am J Crit Care 2012;21:e21–e32.
5. Finke EH, Light J, Kitko L. A systematic review of the effectiveness of nurse communication with patients with complex communication needs with a focus on the use of augmentative and alternative communication. J Clin Nurs 2008;17:2102–15.
6. Happ MB, Garrett K, Thomas DD, Tate J, George E, Houze M, et al., Nurse-patient communication interactions in the intensive care unit. Am J Crit Care 2011;20(2):e28–40.
7. Shannon SE, Long-Sutehall T, Coombs M. Conversations in end-of-life care: communication tools for critical care practitioners. Nurs Crit Care 2011;16:124–30.
8. Almerud S, Alapack RJ, Fridlund B, Ekebergh M. Of vigilance and invisibility – being a patient in technologically intense environments. Nurs Crit Care 2007;12:151–8.
9. McKinley S, Nagy S, Stein-Parbury J, Bramwell M, Hudson J. Vulnerability and security in seriously ill patients in intensive care. Intensive Crit Care Nurs 2002;18:27–36.
10. Havik O. En generell modell for psykologiske reaksjoner ved somatisk sykdom. Nordisk Psykologi 19891;3:161–76.
11. Happ MB, Garrett KL, Tate JA, DiVirgilio D, Houze MP, Demirci JR, et al., Effect of a multi-level intervention on nurse-patient communication in the intensive care unit: results of the SPEACS trial. Heart Lung 2014;43:89–98.
12. Radtke JV, Tate JA, Happ MB. Nurses’ perceptions of communication training in the ICU. Intensive Crit Care Nurs 2012;28:16–25.
13. Eriksson U, Svedlund M. Struggling for confirmation – patients’ experiences of dissatisfaction with hospital care. J Clin Nurs 2007;16:438–46.
14. McCabe C. Nurse-patient communication: an exploration of patients’ experiences. J Clin Nurs 2004;13:41–9.
15. Naden D, Saeteren B. Cancer patients’ perception of being or not being confirmed. Nurs Ethics 2006;13:222–35.
16. Eide H, Eide T. Bekreftende ferdigheter. I Kommunikasjon i relasjoner. 2. utg. Gyldendal Norsk Forlag, Oslo. 2007.
17. Løvlie-Schibbye AL. Hva sier jeg til klienten i psykoterapi. Noen sammenfatninger mellom et filosofisk grunnsyn, relasjonsteori og vårt terapeutiske språk. Impuls 2004;2:20–6.
18. Gysels M, Richardson A, Higginson IJ. Communication training for health professionals who care for patients with cancer: a systematic review of training methods. Support Care Cancer 2005;13:356–66.
19. Kruijver IP, Kerkstra A, Francke AL, Bensing JM, van de Wiel HB. Evaluation of communication training programs in nursing care: a review of the literature. Patient Educ Couns 2000;39:129–45.
20. Lane C, Rollnick S. The use of simulated patients and role-play in communication skills training: a review of the literature to August 2005. Patient Educ Couns 2007;67:13–20.
21. Sleeper JA, Thompson C. The use of hi fidelity simulation to enhance nursing students’ therapeutic communication skills. Int J Nurs Educ Scholarsh 2008;5:Article 52.
22. Tosterud R, Hedelin B, Hall-Lord ML. Nursing students’ perceptions of high- and low-fidelity simulation used as learning methods. Nurse Educ Pract 2013;13:262–70.
23. Gysels M, Richardson A, Higginson IJ. Communication training for health professionals who care for patients with cancer: a systematic review of effectiveness. Support Care Cancer 2004;12:692–700.
24. Guise V, Chambers M, Conradi E, Kavia S, Valimaki M. Development, implementation and initial evaluation of narrative virtual patients for use in vocational mental health nurse training. Nurse Educ Today 2012;32:683–9.
25. Fox-Robichaud AE, Nimmo GR. Education and simulation techniques for improving reliability of care. Curr Opin Crit Care 2007;13:737–41.
26. Westli HK, Johnsen BH, Eid J, Rasten I, Brattebo G. Teamwork skills, shared mental models, and performance in simulated trauma teams: an independent group design. Scand J Trauma Resusc Emerg Med 2010;18:47.
27. Wisborg T, Brattebo G, Brattebo J, Brinchmann-Hansen A. Training multiprofessional trauma teams in Norwegian hospitals using simple and low cost local simulations. Educ Health (Abingdon) 2006;19(1):85–95.
28. Husebø SE, Rystedt H, Friberg F. Educating for teamwork – nursing students’ coordination in simulated cardiac arrest situations. J Adv Nurs 2011;67(10):2239–55.
29. Ballangrud R, Hall-Lord ML, Hedelin B, Persenius M. Intensive care unit nurses’ evaluation of simulation used for team training. Nurs Crit Care 2014;19:175–84.
30. Ballangrud R, Hall-Lord ML, Persenius M, Hedelin B. Intensive care nurses’ perceptions of simulation-based team training for building patient safety in intensive care: a descriptive qualitative study. Intensive Crit Care Nurs 2014;30:179–87.
31. Buxton M, Phillippi JC, Collins MR. Simulation: a new approach to teaching ethics. J Midwifery Womens Health 2015;60:70–4.
32. Zigmont JJ, Kappus LJ, Sudikoff SN. Theoretical foundations of learning through simulation. Semin Perinatol 2011;35(2):47–51.
33. Arafeh JM, Hansen SS, Nichols A. Debriefing in simulated-based learning: facilitating a reflective discussion. J Perinat Neonatal Nurs 2010;24:302–9.
34. Zigmont JJ, Kappus LJ, Sudikoff SN. The 3D model of debriefing: defusing, discovering, and deepening. Semin Perinatol 2011;35(2):52–8.
35. Orledge J, Phillips WJ, Murray WB, Lerant A. The use of simulation in healthcare: from systems issues, to team building, to task training, to education and high stakes examinations. Curr Opin Crit Care 2012;18:326–32.
36. Boet S, Borges BC, Naik VN, Siu LW, Riem N, Chandra D, et al., Complex procedural skills are retained for a minimum of 1 yr after a single high-fidelity simulation training session. Br J Anaesth 2011;107:533–9.
37. Polit DF, Beck CT. Nursing Research. Generating and assessing evidence for nursing practice. 9. utg. Lippincott Williams and Wilkins, Philadelphia. 2012.
38. Boynton PM, Greenhalgh T. Selecting, designing, and developing your questionnaire. BMJ 2004;328:1312–5.
39. Fallowfield L, Saul J, Gilligan B. Teaching senior nurses how to teach communication skills in oncology. Cancer Nurs 2001;24:185–91.
40. Johannesen A, Tufte PA, Christoffersen L. Introduksjon til samfunnsvitenskapelig metode. 4. utg. Abstrakt forlag, Oslo. 2010.
41. Bosse HM, Schultz JH, Nickel M, Lutz T, Moltner A, Junger J, et al. The effect of using standardized patients or peer role play on ratings of undergraduate communication training: a randomized controlled trial. Patient Educ Couns 2012;87:300–6.
42. Levett-Jones T, Lapkin S. A systematic review of the effectiveness of simulation debriefing in health professional education. Nurse Educ Today 2013;15:e58–e63.
43. Knowles MS, Holton EF, Swanson RA. The adult learners. The definitive classic in adult education an human resource development. Elsevier Butterworth Heinemann, San Diego. 2005.
44. Laschinger S, Medves J, Pulling C, McGraw DR, Waytuck B, Harrison MB, et al. Effectiveness of simulation on health profession students’ knowledge, skills, confidence and satisfaction. Int J Evid Based Healthc 2008;6(3):278–302.
45. Moore PM, Rivera MS, Grez AM, Lawrie TA. Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database Syst Rev 2013;3:CD003751.
46. Heaven C, Clegg J, Maguire P. Transfer of communication skills training from workshop to workplace: the impact of clinical supervision. Patient Educ Couns 2006;60:313–25.









Comments