Use of admission CTG in low-risk parous women: a clinical audit
Quality improvement measures led to midwives reducing the use of cardiotocography (CTG) on admission by 47 per cent. Nevertheless, they continued to use CTG more often than necessary.
Background: Cardiotocography (CTG) as a form of electronic fetal monitoring is widely used in normal labour, despite the lack of association with a better neonatal outcome. Intrapartum care today is characterised by unnecessary use of technology, even though a guiding principle is that interventions should only be undertaken when necessary, and where the benefits outweigh the disadvantages.
Objective: The objective of this quality improvement study was to map the use of admission CTG in low-risk parous women after quality improvement measures were implemented to reduce its use.
Method: Using the clinical audit method, we retrospectively mapped low-risk parous women for four weeks (n = 164). After assessing practice, we implemented several changes together with key personnel in the maternity unit. We then decided to perform a statistical process control over 18 weeks in order to observe the use of admission CTG after the quality improvement measures were implemented (n = 168).
Results: The audit showed that admission CTG was used on 77 per cent of the low-risk parous women. In cooperation with key personnel in the maternity unit and management, we provided feedback to the field of practice and implemented measures tailored to the unit in question. These measures led to an improvement in practice, where the use of admission CTG was reduced to 30 per cent. The statistical process control showed that the change in practice was stable over time.
Conclusion: The audit revealed a discrepancy between actual practice and evidence-based guidelines. The desired standard of practice was not met, but the use of admission CTG was significantly reduced after quality improvement measures were implemented.
A guiding principle in intrapartum care is that interventions during childbirth should only be used when absolutely necessary and where the benefits outweigh the disadvantages (1). One consequence of inappropriate interventions in normal labour is the potential for undesirable variation in practice, which in turn may lead to a poorer quality of intrapartum care (2, 3).
Studies show that intrapartum care today is characterised by unnecessary use of technology, where interventions are generally used too frequently and too extensively in normal labour (2, 4). Electronic fetal monitoring (cardiotocography (CTG)) is an advanced fetal monitoring method that is a useful tool when labour complications arise. Fetal monitoring is not recommended for healthy pregnant women because advanced monitoring can lead to adverse outcomes and unnecessary interventions during the birthing process (2, 5).
Studies have also shown that routine use of admission CTG instead of intermittent auscultation (handheld Doppler or fetal stethoscope) increases the risk of a caesarean section by 20 per cent (6, 7). Furthermore, evidence shows that admission CTG among low-risk women does not reduce the incidence of neonatal deaths, or affect the Apgar score or reduce neonatal intensive care admissions (6, 8, 9).
A systematic literature review of low-risk parous women concluded that admission CTG does not improve the quality or patient safety in intrapartum care compared to intermittent auscultation (7). CTG is nevertheless widely used in normal labour (2).
Objective of the study
Intrapartum care in Norway is of a high standard in international terms (5). Nevertheless, the Norwegian Directorate of Health has conducted a study of the midwifery service, which identified a need for improvement in the evidence-based services in intrapartum care (10). In order to achieve this, the midwifery service needs to have access to and apply the best knowledge that is available.
An evidence-based approach entails making decisions in practice based on reliable research results and applying these results in combination with clinical experience and the patient’s wishes and needs (11). One of the goals of the health service is to reduce the use of interventions in normal labour (12).
A large maternity clinic found that, in practice, admission CTG was often used in normal labour. We therefore wanted to carry out a clinical audit to (i) map the use of admission CTG in normal labour at the clinic, (ii) assess whether the practice was in line with evidence-based recommendations, and (iii) implement quality improvement measures where deemed necessary.
Method
The objective of a clinical audit is to improve the quality of patient care by assessing the extent to which the practice is in line with evidence-based guidelines and improving the quality of the health care (13, 14). The method is a step-by-step, systematic process that consists of preparation, auditing practice, assessing the quality of practice against criteria and standards, implementing change and re-auditing practice (13).
Setting
This clinical audit was conducted at a large maternity clinic in Norway, which has just under 5000 births a year. The clinic consists of a high-risk ward and a midwife-run low-risk ward. Both wards were included in the quality improvement study, which was conducted between autumn 2016 and spring 2018. The inclusion criteria were low-risk parous women.
The criteria for low-risk birth are set according to national standards for intrapartum care and include the following: a healthy woman with a normal full-term pregnancy involving a cephalic presentation and spontaneous labour, where the woman is not known to have an illness that can cause complications, and where she has not previously undergone a complicated pregnancy or birth (5).
Quality measurements
Quality is measured against a criterion and a standard. The criterion represents the ideal quality measurement, while the standard describes the realistic measurement in practice (13). The quality of practice was assessed against one criterion and one standard, which were quantifiable and based on scientific knowledge (Table 1).
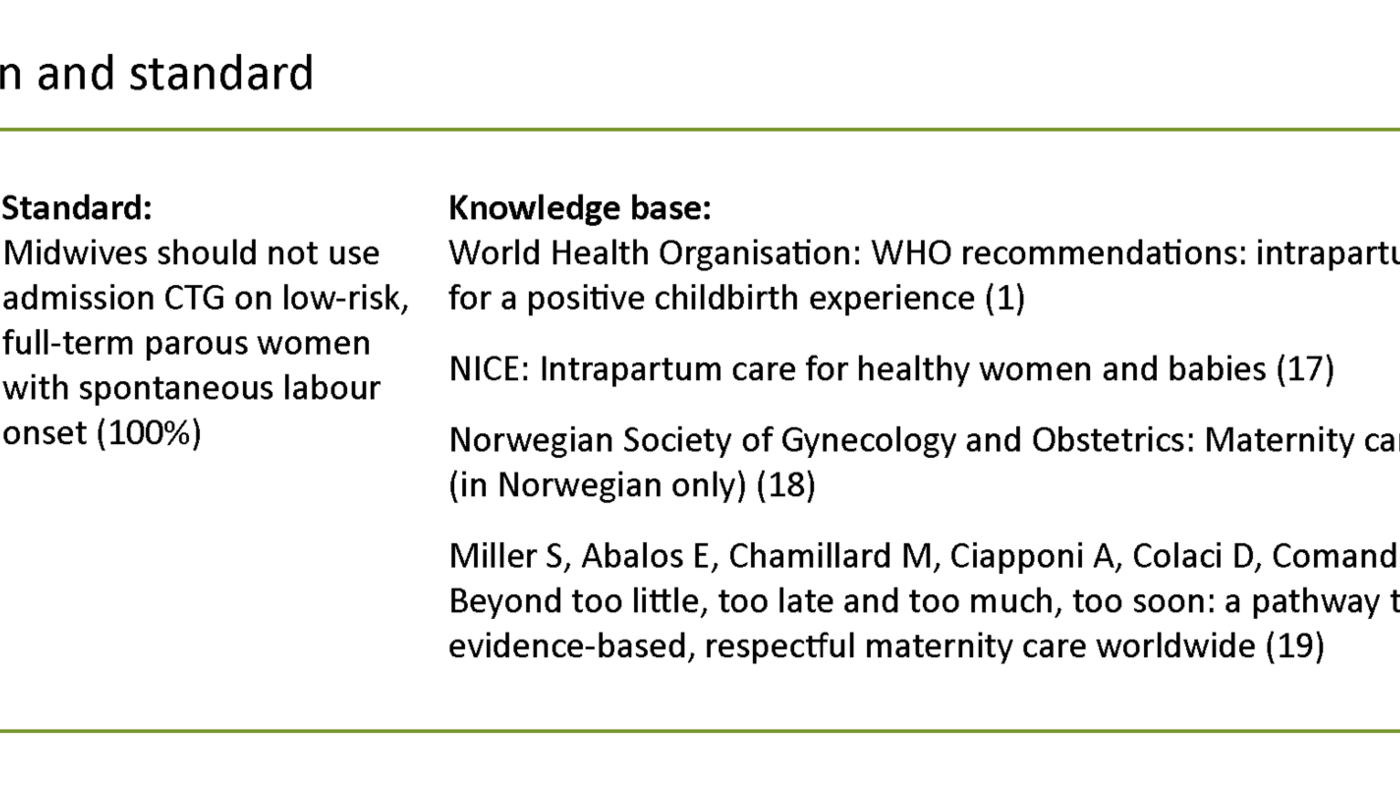
The criterion was defined as ‘admission CTG should only be undertaken based on medical indication’. In order to determine the criterion and standard, we performed a systematic search in various national and international guidelines as well as in databases (Guidelines International Network (G-I-N), the Norwegian Electronic Health Library, WHO, Cochrane Library, Pubmed, Embase, Cinahl and Maternity and Infant Care).
The quality of the various sources was critically assessed before the sources were included in the knowledge base (15, 16). The criterion is based on three guidelines and a systematic literature review (1, 17–19). The expected standard of practice was set to ‘admission CTG should not be undertaken if the labour is considered low risk’ (100 per cent). We determined that there was no reason for the standard to deviate from the criterion, since the knowledge base explicitly states that admission CTG should not be used on low-risk parous women (1, 17–19).
Assessing practice
The quality of practice was assessed in two stages: i) before (audit) and ii) after implementation of quality improvement measures (re-audit). We collected data for the audit and re-audit using the electronic patient record system IMATIS Natus, and a validated mapping tool (audit form) was used to systematically review each patient record (20). The tool was tested on five patient records independently, and was subsequently adapted for the local conditions at the clinic (21).
The finalised tool then underwent an inter-rater reliability test where the first and second authors evaluated five further patient records independently to see if they were reviewed in the same way. The comparison of this test showed consistency in the use of the mapping tool. The patient records were then distributed between the first and second author and assessed manually against the mapping tool.
In the initial audit of practice, we obtained data from the whole of February 2016. In the re-audit, we collected data in the period February to June 2018 in a time series analysis in order to be able to examine change through statistical process control (22).
Implementing change
We conducted a barrier analysis to identify the barriers to following the recommended practice. The barriers were identified through interviews with midwives, discussions in an interdisciplinary working group as well as informal conversations and discussions in the workplace.
Following this process, a fish-bone analysis (Figure 1) was undertaken to identify possible links in the failure to adhere to guidelines in practice, and to identify the barriers that had the most significance for changing practice (23). The fish-bone analysis showed that the greatest barriers to reducing the use of admission CTG were the working environment and the staff.
There was professional uncertainty among the midwives about the use of admission CTG. The midwives were uncertain and insecure about their own knowledge. This lack of confidence and apprehension led to them using interventions such as admission CTG as a way of ensuring they would not miss signs of fetal stress and that the birth would not end with a negative outcome.
The obstetric environment at the clinic was characterised by a risk perspective, where there was a strong culture for using admission CTG. A hallmark of this culture was that different occupational groups, such as midwives and obstetricians, had different expectations and views on when admission CTG should be used. The midwives believed that the obstetricians expected admission CTG to be used on all women, and therefore complied with this. In addition to unclear understandings of when to use admission CTG, the professional procedure for using admission CTG at the clinic was ambiguous and difficult to interpret.
The results from the fish-bone analysis were used to adapt quality improvement measures to the clinic in question (24). Several measures were implemented, which proved to be more effective in changing behaviour than one measure alone (25). Systematic literature reviews on the measures that have proven to be effective in changing practice represented the knowledge base for the measures implemented (14, 26, 27).
Study participants
We recruited six midwives from both maternity wards as opinion leaders for the project prior to the re-audit. During the process, these key personnel were updated and encouraged to monitor the problem area in the clinic (26). The second measure in the project was feedback to the wards (14, 28). The management, key personnel and authors of the article provided feedback orally and in writing several times during the process on various platforms. The feedback included preliminary results.
The feedback was conveyed shortly after the initial audit, prior to the implementation of the quality improvement measures and two months after implementation. The management and the first and second authors provided the feedback at local workshops, at obstetricians’ meetings, in monthly information letters from management and via email.
The last quality improvement measure to be implemented was written educational material in the form of posters, which were displayed in all admission rooms where midwives use admission CTG (27). The posters were put up at the start of the re-audit.
Assessing new practice (re-audit)
In the re-audit, we collected data every four weeks over a period of 18 weeks. The data collection therefore consisted of five measurement points between February 2018 and June 2018. Each measurement point in the time series lasted for one week. We used statistical process control to monitor and analyse how the change developed during the process (29).
Data analysis
The data were plotted and analysed in the Statistical Package for the Social Sciences (IBM SPSS) version 24.0 (IBM Corp., 2016). All data were plotted independently by two people to ensure correct data entry (30). Discrepancies between actual practice and ideal practice (criterion) were presented as absolute numbers and percentages. We calculated the confidence interval of the percentage estimates to be 95 per cent (31, 32).
In order to compare the measurements in the audit and the re-audit, we used Pearson’s chi-squared test (32). Two-tailed confidence intervals were used to calculate confidence intervals for the change between the audit and the re-audit (31). A significance level of 0.05 was applied in all tests (32).
A percentage diagram was created to show the development of change over time, before and after implementation (29). The diagram shows changes during the re-audit period. The diagram also shows the repeat measurements of the practice that were taken between February and June 2018; a total of five measurements. In order to compare the time series in the re-audit with the audit, we calculated the average from all five measurements. This enabled us to assess whether the practice had improved.
The quality improvement study was reported to and approved by the local data protection officer. All data were treated confidentially and stored on the hospital’s quality server.
Results
Quality of practice measured against criteria for practice (audit)
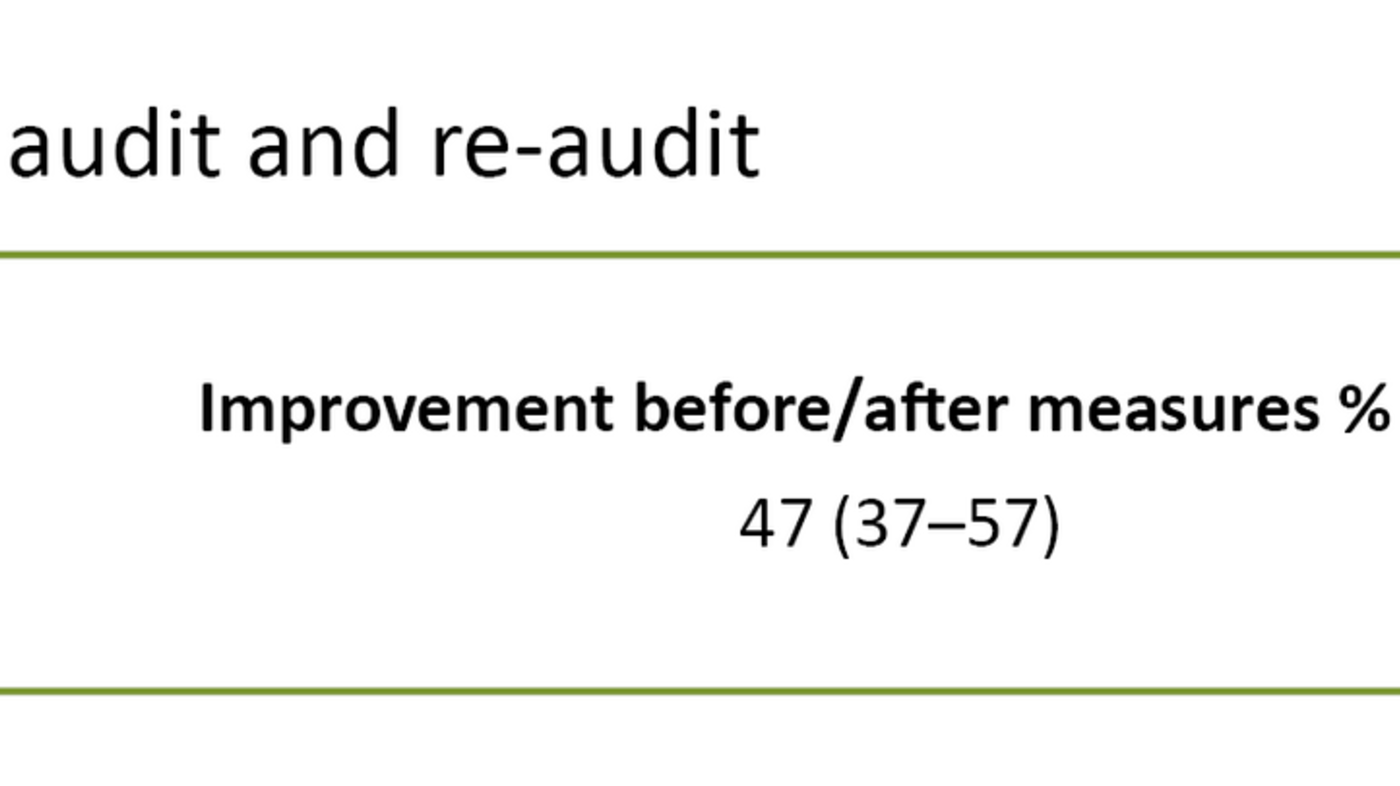
A total of 395 women gave birth during the audit in February 2016, 164 of whom met the inclusion criteria. Admission CTG was used in 77 per cent (n = 126) of the patient records (95%, CI 70–83) (Table 2). In the audit, 90 per cent (n = 147) of the women were admitted to the low-risk ward and 10 per cent (n = 17) were admitted to the high-risk ward.
The breakdown of admission CTG in the different wards showed that in the high-risk ward the use of admission CTG was 88 per cent (n = 14) (95%, CI 73–104), and in the low-risk ward the use was 76 per cent (n = 111) (95%, CI 69–82).
Re-assessing practice (re-audit)
When re-auditing the practice, we performed a statistical process control of the change in practice, with five repeated measurements. The time series showed a stable change over time with little variation, where the lowest observed use of admission CTG was 24 per cent (week 6), and the highest was 41 per cent (week 10).
There was no evidence of an increase in the use of admission CTG beyond the months measured, and in the last measurement from practice, the use of admission CTG was down to 26 per cent (week 22) (Figure 1).
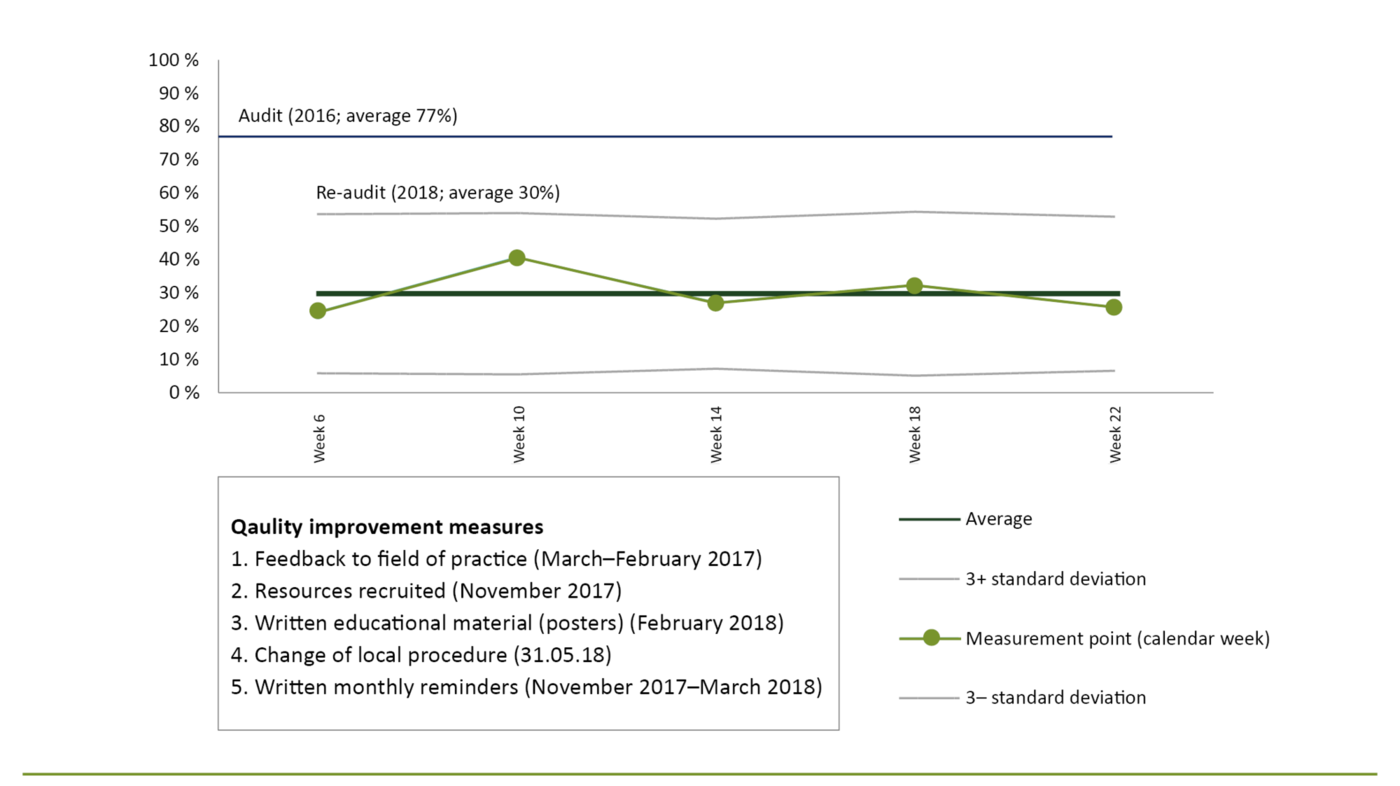
A total of 168 women were included in the re-audit. Of the sample, 13 per cent (n = 23) were admitted to the high-risk ward and 86 per cent (n = 145) were admitted to the low-risk ward. The average of the measurements from the re-audit showed that admission CTG was used in 30 per cent (95%, CI 23–37) of the women. There was a significant reduction in the use of admission CTG of 47 per cent (95%, CI 37–57) between the initial audit and the re-audit (Table 2).
Admission CTG was used in 25 per cent (n = 36) (95%, CI 18–32) of the women in the low-risk ward and 61 per cent (n = 14) (95%, CI 41–81) in the high-risk ward. The use of admission CTG fell in both wards, but the greatest reduction was seen in the low-risk ward, with an improvement of 51 per cent versus 27 per cent in the high-risk ward.
Discussion
Admission CTG was used in 77 per cent of cases, which did not match the standard defined for the practice. After implementing tailored measures, the practice improved over time, and the use of admission CTG was reduced to an average of 30 per cent.
Strengths and weaknesses of the study
The quality improvement study is a local project, and the population is from the maternity clinic in question. The results of the study can only be interpreted in a local context and are not transferrable to anywhere else. Nevertheless, it is reasonable to assume that admission CTG is often used unnecessarily on low-risk parous women at other maternity wards in Norway, as there has long been a strong tradition for this in intrapartum care (33). This clinical audit can therefore serve as a guide for practice.
The results show that the quality of practice has improved and that midwives are working more in line with evidence-based recommendations (1, 17–19). However, it is unknown whether the improvement is a result of the quality improvement measures alone, as there may be other factors that have contributed to the change in practice. A stronger focus on admission CTG by management may be one such factor.
The ward managers sought change and took an active part in the audit process. The obstetric staff at the clinic were also involved in parts of the process. In addition, key personnel at the maternity clinic, such as the manager of the low-risk ward, the midwife responsible for professional development, a senior consultant, and the midwives at the clinic helped to draw up the quality improvement measures. Modifications to the working environment and management support make it more likely that the change will be sustained over time (14, 34, 35).
In the re-audit, the data were collected in parallel with the implementation of the quality improvement measures. The measurements were therefore taken during a period when there was a greater focus on reducing admission CTG, which may have had a positive impact on the results (35).
In the re-audit, the staff were also aware that they were being assessed, which may have led them to perform better than they would normally. However, a steady improvement in practice was observed in our repeat measurements. There was no sign that the use of admission CTG increased over time, which may indicate that the practice has improved.
The measurements were thus carried out during a period where there was a greater focus on reducing admission CTG, which may have had a positive impact on the results (35). The field of practice is constantly changing, and it is therefore not inconceivable that the time that passed between the first and second quality improvement measures (two years) may have had an unknown impact on the results. It remains to be seen whether the positive effect we have shown will diminish if the various wards do not continue to highlight the use of admission CTG after the end of the project (30).
Midwives overestimate the risk of fetal stress
Evidence shows that using admission CTG during normal labour does not lead to a better fetal and neonatal outcome (7). The initial audit of the field of practice showed that the use of admission CTG was high, despite the fact that evidence-based guidelines do not recommend this (1, 7, 17, 18). The quality of patient treatment and failure to apply the best knowledge available is a well-known challenge in several areas of health care (10, 11, 14, 36).
The results of the initial audit concur with a previous study showing that midwives prefer to use admission CTG instead of intermittent auscultation. The study also showed that midwives overestimate the risk of fetal stress upon admission to the labour ward and therefore use admission CTG (37). The midwives’ overestimation of the risk of fetal stress is consistent with the findings in our barrier analysis, which showed that midwives were particularly focused on fetal stress and how this could be detected at an early stage using admission CTG.
Intentions are inconsistent with practice
Several studies show that midwives have a fundamental belief in natural childbirth without interventions, but this does not reflect the midwives’ actions in practice (37–39). Midwives appear to overestimate the risk of adverse events during childbirth for low-risk women. Taking a risk approach to childbirth out of fear of what might happen to the mother and the fetus can lead to unnecessary monitoring and use of technology, which in turn reduces the quality of patient care (39–41).
If we let the risk perspective govern us, intrapartum care will become based on the worst-case scenario approach. In terms of health promotion, it is important that patients receive good-quality services without being exposed to risk or injury as a result of treatment (3, 42, 43). One indicator of good quality in intrapartum care is childbirth without major interventions and complications (12). By reducing the use of admission CTG on low-risk parous women, the use of intrapartum interventions such as continuous CTG and fetal blood tests can also be reduced (7).
Improvements after feedback
The re-audit of practice showed that the standard had improved significantly and that the change was stable over time. The lowest measurements were observed during the implementation of the quality improvement measures. These findings are also consistent with another study showing that the field of practice performs best immediately after receiving feedback (44).
One consequence of midwives adhering more closely to evidence-based guidelines is that it reduces an undesirable variation in practice, where the treatment patients receive differs depending on who treats them (10). An equal health provision to all patients helps to raise the standard of health care. It also strengthens the quality requirements for intrapartum care, which stipulate that the provision should be equal for all women and children, regardless of where the birth takes place (5).
The use of admission CTG was reduced in both low-risk and high-risk wards. The greatest change of practice occurred at the low-risk ward, where admission CTG was used on 25 per cent of low-risk parous women, compared to 61 per cent in the high-risk ward. One possible explanation may be that midwives who work in high-risk wards with high-risk parous women have a greater risk perception in general during the birthing process than those who work in low-risk units with more normal births without complications.
One study shows that midwives who work in high-risk wards are more exposed to interventions, resulting in a higher perception of risk in childbirth (39). The study also shows that low-risk women are more likely to be subjected to interventions during childbirth if they give birth in a high-risk ward (39). Further measures should be implemented in the high-risk ward to reduce the use of admission CTG during normal labour.
Quality standard not met
In this audit, the defined standard of practice was not met, despite the reduction in the use of admission CTG. The time period for measuring practice is crucial to the result. Measuring practice immediately after the quality improvement measures have been implemented may not allow sufficient time for the measures to take effect. Waiting too long may result in measures losing their effect and staff falling back into old habits (35, 45).
New measurements should also be taken to ensure that the quality is maintained (35). The failure to meet the quality standard indicates that further measures should be taken to improve practice. The reason why the standard of practice was not met may be due to changes in the structure of the organisation. Evidence shows that organisational changes can impact on the results in a clinical audit (35).
During the period of our clinical audit, the selection criteria at the hospital changed, such that the ward that is referred to as a low-risk unit now also includes women whose labour is induced. As a result of this restructuring, the staff were dealing with more high-risk pregnancies than previously. Coupled with a change in ward management, this new structure may also have affected the operation and thus the use of intrapartum interventions (39).
Conclusion
The first round of the clinical audit revealed a discrepancy between preferred practice and evidence-based recommendations in the use of admission CTG. After implementing quality improvement measures, the use of admission CTG fell significantly, but the defined standard for practice was still not met. The quality associated with the use of admission CTG was improved in the maternity clinic in question, and the midwives there are now working more in line with evidence-based recommendations for admission CTG in normal labour.
In light of the results of the midwifery audit, the spotlight should continue to be directed towards the problem area through close follow-up and further measurements of practice.
Kristina Jørandli and Ada Kristine Nese are both first authors of this article.
References
1. Verdens helseorganisasjon. WHO recommendations: Intrapartum care for a positive childbirth experience. Genève: Verdens helseorganisasjon; 2018. Available at: http://www.who.int/reproductivehealth/publications/intrapartum-care-guidelines/en/ (downloaded 02.02.2018).
2. Renfrew MJ, McFadden A, Bastos MH, Campbell J, Channon AA, Cheung NF, et al. Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. The Lancet. 2014;384(9948):1129–45.
3. McDougall L, Campbell OMR, Graham W. Maternal health an executive summary for The Lancet’s Series. The Lancet; 2016. Available at: http://www.thelancet.com/pb/assets/raw/Lancet/stories/series/maternal-health-2016/mathealth2016-exec-summ.pdf (downloaded 16.03.2018).
4. Hoope-Bender Pt, Bernis Ld, Campbell J, Downe S, Fauveau V, Fogstad H, et al. Improvement of maternal and newborn health through midwifery. The Lancet. 2014;384(9949):1226–35.
5. Helsedirektoratet. Et trygt fødetilbud. Kvalitetskrav til fødselsomsorgen. Oslo; 2010. IS-1877. Available at: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/245/Et-trygt-fodetilbud-kvalitetskrav-til-fodselsomsorgen-IS-1877.pdf (downloaded 01.10.2016).
6. Bhartiya V, Sharma R, Kumar A, Srivastava H. Admission cardiotocography: a predictor of neonatal outcome. J Obstet Gynaecol India. 2016;66(1):321–9.
7. Devane D, Lalor JG, Daly S, McGuire W, Cuthbert A, Smith V. Cardiotocography versus intermittent auscultation of fetal heart on admission to labour ward for assessment of fetal wellbeing. (Review.) Cochrane Database Syst Rev. 2017;(1):1–46.
8. Impey L, Reynolds M, MacQuillan K, Gates S, Murphy J, Sheil O. Admission cardiotocography: a randomised controlled trial. The Lancet. 2003;361(9356):465–70.
9. Mires G, Williams F, Howie P. Randomised controlled trial of cardiotocography versus Doppler auscultation of fetal heart at admission in labour in low risk obstetric population. BMJ. 2001;322(7300):1457–562.
10. Helsedirektoratet. Utviklingsstrategi for jordmortjenesten. Tjenestekvalitet og kapasitet. Oslo; 2010. IS-1815. Available at: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/265/Utviklingsstrategi-for-jordmortjenesten-tjenestekvalitet-og-kapasitet-IS-1815.pdf (downloaded 22.09.2015).
11. Sosial- og helsedirektoratet. Nasjonal strategi for kvalitetsforbedring i Sosial- og helsetjenesten … Og bedre skal det bli! Oslo; 2005. IS-1162. Available at: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/233/Og-bedre-skal-det-bli-nasjonal-strategi-for-kvalitetsforbedring-i-sosial-og-helsetjenesten-2005-2015-IS-1162-bokmal.pdf (downloaded 04.06.2016).
12. Helsedirektoratet, Medisinsk fødselsregister. Kvalitetsindikatorer for graviditet og fødsel. Oslo: Direktoratet for e-helse; 2016. Available at: https://helsenorge.no/Kvalitetsindikatorer/graviditet-og-fodsel (downloaded 19.01.2018).
13. NICE. Principles for best practice in clinical audit. Oxford; 2002. Available at: http://www.uhbristol.nhs.uk/files/nhs-ubht/best_practice_clinical_audit.pdf (downloaded 03.06.2016).
14. Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback: effects on professional practice and healthcare outcomes. (Review.) Cochrane Database Syst Rev. 2012;(6):1–229.
15. The AGREE Collaboration. Evaluering av faglige retningslinjer. Oslo: Sosial og-helsedirektoratet; 2003. Available at: http://www.agreetrust.org/wp-content/uploads/2013/06/AGREE_Instrument_Norwegian.pdf (downloaded 15.02.2018).
16. Nasjonalt kunnskapssenter for helsetjenesten. Sjekkliste for vurdering av en oversiktsartikkel. Oslo; 2014. Available at: https://www.fhi.no/globalassets/kss/filer/filer/verktoy/sjekkliste-oversikt-sr-2014.pdf (downloaded 15.02.2018).
17. NICE. Intrapartum care for healthy woman and babies. Oxford; 2017. CG190. Available at: https://www.nice.org.uk/guidance/cg190/evidence/full-guideline-248734765 (downloaded 01.06.2016).
18. Norsk gynekologisk forening. Veileder i fødselshjelp. Tromsø/Oslo/Bergen; 2014. Available at: http://legeforeningen.no/Fagmed/Norsk-gynekologisk-forening/Veiledere/Veileder-i-fodselshjelp-2014/ (downloaded 02.02.2018).
19. Miller S, Abalos E, Chamillard M, Ciapponi A, Colaci D, Comandé D, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. The Lancet. 2016;388(10056):2176–92.
20. Fadnes H. Jordmorfagleg audit av innkomst CTG. Korleis praktiseres innkomst CTG på ei fødeavdeling for selekterte friske gravide? (Fordypningsoppgave.) Bergen: Høgskolen i Bergen, Institutt for sykepleiefag, Avdeling for helse- og sosialfag; 2015.
21. Boynton PM, Greenhalgh T. Selecting, designing, and developing your questionnaire. BMJ. 2004;328:1312–5.
22. Carey RG, Lloyd RC. Measuring quality improvement in healthcare: a guide to statistical process control applications. Milwaukee, Wisconsin: ASQ; 2001.
23. Helsebiblioteket. Fiskebeinsdiagram: Folkehelseinstituttet. Oslo; 2010. Available at: www.helsebiblioteket.no/kvalitetsforbedring/metoder-og-verktoy/fiskebeinsdiagram (downloaded 18.01.2018).
24. Baker R, Camosso-Stefinovic J, Gillies C, Shaw EJ, Cheater F, Flottorp S, et al. Tailored interventions to address determinants of practice. Cochrane Database Syst Rev. 2015;(4):1–118.
25. Ashmore S, Ruthven T, Hazelwood L. Stage 3: Implementing change. In: Burgess R, ed. NEW principles of best practice in clinical audit. 2. ed. Oxford: Radcliffe Publishing; 2011. s. 81–92.
26. Flodgren G, Parmelli E, Doumit G, Gattellari M, O’Brien MA, Grimshaw J, et al. Local opinion leaders: effects on professional practice and health care outcomes. (Review.) Cochrane Database Syst Rev. 2011;(8):1–69.
27. Giguère A, Légaré F, Grimshaw J, Turcotte S, Fiander M, Grudniewicz A, et al. Printed educational materials: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;(10):1–197.
28. Flottorp S, Jamtvedt G, Gibis B, McKee M. Using audit and feedback to health professionals. Copenhagen: Verdens helseorganisasjon; 2010. Available at: http://www.euro.who.int/__data/assets/pdf_file/0003/124419/e94296.pdf (downloaded 25.10.2016).
29. Nyen B. Forbedringsarbeid og Statistisk Prosesskontroll (SPC). Porsgrunn: Nasjonalt kunnskapssenter for helsetjenesten; 2009. Available at: https://www.fhi.no/globalassets/kss/filer/filer/publikasjoner/seksjonsvis-inndeling/seksjon-for-kvalitetsutvikling/kompendium-spc-v2-0.pdf (downloaded 20.10.2017).
30. Ashmore S, Ruthven T, Hazelwood L. Stage 2: Measuring performance. In: Burgess R, ed. NEW principles of best practice in clinical audit. 2. ed. Oxford: Radcliffe Publishing; 2011. s. 59–79.
31. Ubøe J. Statistikk for økonomifag. Oslo: Gyldendal Akademisk; 2015.
32. Polit DF, Beck CT. Essentials of nursing research: appraising evidence for nursing practice. 8. ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2014.
33. Blix E. Innkomst-CTG. En vurdering av testens prediktive verdier, reliabilitet og effekt. Betydning for jordmødre i deres daglige arbeid. (Doktoravhandling.) Gothenburg: Nordiska högskolan för folkhälsovetenskap; 2006.
34. Aasekjær K, Waehle HV, Ciliska D, Nordtvedt MW. Management involvement—a decisive condition when implementing evidence-based practice. Worldviews Evid Based Nurs. 2016;13(1):32–41.
35. Ashmore S, Ruthven T, Hazelwood L. Stage 4: Sustaining improvement. In: Burgess R, ed. NEW principles of best practice in clinical audit. 2. ed. Oxford: Radcliffe Publishing; 2011. s. 93–106.
36. Aasekjær K. Klinisk audit av avnavlingspraksis: Arbeider jordmor kunnskapsbasert? Sykepleien Forskning. 2012;7(3):214–22. DOI: 10.4220/sykepleienf.2012.0127
37. Mead M, Bogaerts A, Reyns M. Midwives’ perception of the intrapartum risk of healthy nulliparae in spontaneous labour, in The Flanders, Belgium. Midwifery. 2007;23(4):361–71.
38. Scamell M, Alaszewski A. Fateful moments and the categorisation of risk: Midwifery practice and the ever-narrowing window of normality during childbirth. Health Risk Soc. 2012;14(2):207–21.
39. Healy S, Humphreys E, Kennedy C. Midwives’ and obstetricians’ perceptions of risk and its impact on clinical practice and decision-making in labour: An integrative review. Women Birth. 2016;29(2):107–16.
40. Blåka G. Grunnlagstenkning i et kvinnefag – teori, empiri og metode. Bergen: Fagbokforlaget; 2002.
41. Blåka G, Eri TS. Doing midwifery between different belief systems. Midwifery. 2008;24(3):344–52.
42. Verdens helseorganisasjon. Patient safety: making health care safer. Genève; 2017. Available at: http://apps.who.int/iris/bitstream/handle/10665/255507/WHO-HIS-SDS-2017.11-eng.pdf?sequence=1 (downloaded 10.10.2017).
43. Verdens helseorganisasjon. Quality of care: a process for making strategic choices in health systems. Geneva; 2006. Available at: http://www.who.int/iris/handle/10665/43470 (downloaded 19.10.2016).
44. Sjøbø B, Graverholt B, Jamtvedt G. Kunnskapsbasert vurdering av delirium hos intensivpasienten. Sykepleien Forskning. 2012;7(4):358–68. DOI: 10.4220/sykepleienf.2012.0155
45. Grol R, Wensing M. Implementation of change in healthcare: a complex problem. In: Grol R, Wensing M, Eccles M, Davis D, eds. Improving patient care: the implementation of change in health care. 2. ed. Chichester: Wiley-Blackwell BMJ Books; 2013. s. 3–17.









Comments