Small organisational adjustments can lead to better supervision of clinical practice in intensive care units
Measures such as the ‘getting-to-know-you’ day, the ‘float nurse’ function at an early stage, group meetings and internal training greatly benefitted supervisors and students at Oslo University Hospital.
Background: The education of intensive care nurses in Norway is undergoing continuous change – it is in the process of becoming more academic whilst the requirement for a high proportion of clinical placements is maintained. This change entails challenges for the organisation of practice supervision.
Objective: The objective of the project was to enhance the quality of practice supervision by means of organisational adjustments.
Method: This action research project was a collaboration between an intensive care unit at Oslo University Hospital and Lovisenberg Diaconal University College (LDUC). Six intensive care nurses acting as supervisors for intensive care students in practice participated in the project and supervised a cohort of master’s degree students at LDUC throughout three clinical placements. During the same period, they carried out a training and monitoring programme consisting of a clinical supervision course worth 10 credits, and took part in supervision groups and reflection groups as well as planning and evaluation meetings. We studied the supervisors’ experiences by means of focus group interviews before, during and after the project period.
Results: The supervisors found that the project had positive impacts on the quality of student supervision. The sense of community with other supervisors, competence development and the opportunity to discuss and get advice on issues they encountered in practice were of value in developing the supervisory role. The supervisors were given the opportunity to participate in the development of practice through continuous evaluation of practice and the testing of new measures. We implemented some organisational adjustments to adapt the functioning of the unit to the supervision through close cooperation between management and supervisors.
Conclusion: There will always be a gap between what is desirable and what is possible to achieve at a workplace with high activity, constant changes and limited financial and staffing resources. This project had the goal of implementing measures that were feasible within the ordinary operational framework. We discovered that small adjustments could result in substantial benefits.
The education of intensive care nurses in Norway is undergoing continuous change. It has developed from in-house training via further education at university college level to specialisation as an intensive care nurse at master’s degree level. It is in the process of becoming more academic whilst the requirement for a high proportion of clinical placements is maintained (1).
As the education becomes more advanced, this also increases the demands placed on practice supervisors. If the quality of clinical placements is to keep pace with developments, we must apply new ways of thinking to the organisation of practice supervision.
Previous research
International studies point out that supervision is challenging and that the framework factors are often unsatisfactory. An Australian study showed that the lack of a formal supervision programme resulted in supervisors experiencing high work pressure, a lack of training, little cooperation with other supervisors, and limited time for planning (2).
A Swedish study revealed that training in supervision, feedback about the supervision, preparation time, and support from management were precisely the factors that facilitated supervision (3). Supervisors at a Norwegian intensive care unit reported that sufficient time and involvement on the part of management were key framework factors (4).
Supervisors of Swedish bachelor’s degree students evaluated a supervision model devised for the purpose of remedying deficiencies and facilitating a good academic learning environment. They were of the opinion that the supervision model was useful. A risk factor in clinical placements was that the practice supervisors did not have sufficient academic or pedagogical skills (5). A review of the literature concluded that structured supervision programmes are important in respect of the training, recruitment and satisfaction of nurses (6).
The didactical relationship model
The didactical relationship model is a pedagogical model that can assist in planning, conducting and evaluating teaching and supervision. The model was developed by Bjørndal and Lieberg (7) and elaborated further by Hiim and Hippe (8). The model describes the following six key factors of importance for learning: learning conditions, setting framework, goals, content, learning process and assessment.
The factors are interdependent and comprise a holistic system in which none of the factors actually predominate (8). In this article, we have decided to highlight the organisational framework factors, and to show how these factors affect the participants in the project and therefore play a decisive role in the overall picture.
The objective of the study
This project was a collaborative project between an intensive care unit at Oslo University Hospital and Lovisenberg Diaconal University College (LDUC). We wished to explore new ways of organising practice supervision of intensive care nursing students in the unit. Our motivation was to create parameters for supervision that would offer both supervisors and students a better solution. We therefore formulated the following research question:
How can practice supervision be organised to enhance its quality?
Method
Research design
We considered action research to be a good design for this project since its core idea is that problems in practice can be studied scientifically together with those who are actually familiar with the problems (9). The method entails that solutions come from the lowest level in the organisation, i.e. a bottom-up-perspective (10).
Practitioners participate actively in order to perform a critical assessment of current practice and find opportunities for improvement. Action research is a dynamic process, and practice can be changed throughout the data collection, and new measures implemented (11). The research and changes in practice took place in parallel, and we collected and analysed the data on an ongoing basis.
The research group
Two intensive care nurses from the intensive care unit, both with a master’s degree, took part. One of them was project manager. In addition, the head of unit participated as well as an assistant professor from the university college and the head of studies and the head of research. The two intensive care nurses also held part-time positions at the university college during the project period. The group held regular meetings from the time we started planning the project in May 2016 until we published the results.
Ethical considerations
We obtained approval for the project from the data protection officer at the hospital, and informed nurses in the unit about the project via circular letters and oral communication.
We informed them that participation was voluntary, and that they could withdraw at any point in the process. Intensive care nurses who were particularly interested in supervision were encouraged to participate. The participants gave written, informed consent prior to the start of the project.
Sample
Six intensive care nurses took part in the project. They had from 2–16 years of experience as intensive care nurses and a range of supervisory experience as well as a common interest and involvement in student supervision.
Project activities
The project participants were offered a study programme in clinical supervision at the university college. The course was worth 10 credits and was organised in three modules. At the beginning of each period of practice, an information meeting was held for students, supervisors, the project manager and the teacher. These meetings functioned as an arena for participants to get to know each other and exchange experiences, and for expectations to be clarified. The assistant professor from the university college presented the syllabus and plan for the clinical practice period.
Prior to the second and third clinical practice period, the supervisors, project manager, teacher and unit management held planning meetings to discuss experiences from the previous period of practice, and make plans for the ensuing period. During all practice periods, we arranged supervision group meetings for the supervisors, at which they had the opportunity to raise issues from practice and receive advice on these.
We also arranged two reflection group meetings for supervisors and students together, allowing time for them to reflect on patient situations and supervision methods.
Data collection
We chose focus group interviews as the principal method of data collection. In addition, we wrote field notes during the supervision and reflection groups and the planning meetings. A focus group interview is a research interview in which the participants discuss a pre-determined topic as freely as possible (12).
The challenge consists of creating dynamics in the group that help to elicit different perspectives that provide diversity and breadth, and that can answer the research questions. The aim is that no one dominates the group and that the group is not too homogenous (13, 14).
We conducted five focus group interviews with the supervisors in the period from September 2016 to October 2017, with the first taking place prior to the start of the project and the last after the end of the project. All the focus group interviews began with a presentation of the research question. Then we posed open-ended questions about the supervisors’ experiences of student supervision and the organisation of the supervision. We expanded and concretised the open-ended questions by asking how the supervisors collaborated, and how interaction with management helped to facilitate student supervision.
The supervisors could discuss and share their experiences of new supervision methods in the focus groups, and suggest changes in the project. We discussed the results of each individual interview in the research group. The results formed the starting point for new questions if relevant and the need for further elaboration in the next focus group.
Analysis
We transcribed the audio tapes from the focus group interviews and analysed them together with the field notes from the group meetings. In order to ensure reflexivity, relevance and validity (15), the entire research group was involved in the analysis process. We carried out Brinkmann and Kvale’s (16) five-step method for qualitative content analysis. We extracted and condensed the meaning-bearing units from the text, and preliminary topics were then formulated.
In the next phase, we condensed the meaning units further, with some degree of interpretation. Subsequently, the topic was formulated with an overarching, abstract content. We discussed the results in the research group before further processing of the dataset. After analysing the interviews, we summarised the results and applied them in the ongoing evaluation of changes implemented in the project.
Results
Before the project started, the supervisors described deficiencies in the organisation of the practice supervision. For example, they believed that much was governed by sheer chance: ‘There probably hasn’t been all that much follow-up and so on. It’s been left to us supervisors to find our way.’
The unit received many students, and because of different working time arrangements, the responsibility for the students often fell on the same nurses. The supervisors called for greater understanding from management and colleagues regarding the considerable demands of supervisory responsibility: ‘It is essential that management takes on board that having a student entails planning and a lot of extra work during the course of the day. They say they understand, but that doesn’t quite tally with what they do in practice.’
The supervisors acknowledged that they themselves had a responsibility to communicate their needs to management: ‘I also think we’re not good enough at speaking up. We must make it clearer what having students demands.’
On the basis of the prior situation and experiences we gained during the project period, we identified three main topics that were of significance for how practice supervision at the unit was organised. These topics were supervisors’ sense of community, adaptation of the operation of the unit,and building a supervisory culture.
Supervisors’ sense of community
The project participants felt positive about being included in a group in which they could share responsibility for the students, exchange experiences, and give each other feedback: ‘We’re a fixed group of supervisors who will work together. We’ll have the same teaching and we can discuss things, cooperate and ask each other for advice.’
Several people had experienced challenging situations where they had been able to utilise their colleagues’ expertise to improve student performance. The supervisors said that having their own forums for discussing and exchanging experiences allowed them to cooperate and exploit each other’s competence.
We held the group meetings on days when the staffing situation made it possible for the supervisors to leave the unit at the time scheduled. Those who attended in their free time were given extra time off. The supervisors said as follows: ‘The group discussions with and without students have been fine. You are away from the unit and you have the opportunity to talk and discuss things.’
Even though the supervisors talked together about supervisory tasks in the course of the working day, the supervision groups gave them more leeway to look at issues in depth. They agreed that it would be wise to continue the supervisor groups even after the end of the project period.
Adaptation of the operation of the unit
The project participants emphasised the importance of good cooperation between the supervisors and unit management to permit the adaptation of the operation of the unit to the supervision. The supervisors hoped that the project would be positive in that respect: ‘I feel that supervision is given a higher priority now, and that the students are more in focus.’
One of the main challenges the supervisors highlighted was caring for the interests of both the student and the intensive care patient simultaneously. It was preferable to work with complex cases to allow students to achieve their learning outcomes, but performing all the tasks and finding time for supervision and reflection at the same time was a challenge:
‘I find I’m often a bit short of time. Because it’s not a ward patient who’ll be going home soon. It’s a patient with complicated multi-organ dysfunction, and any change you make will impact on something else. So you’re supervising, and something happens, and you have to provide care, and then there’s the doctor’s round and then the day’s over.’
In a busy everyday situation, it was difficult for the supervisors to take the student aside to reflect on learning situations.
In order to strengthen the cooperation between management and supervisors, we held planning meetings for supervisors and management prior to the practice periods. We agreed on several measures to meet the wishes of the supervisors. To ensure good learning situations for the students, the supervisors themselves would take greater responsibility for communicating specific wishes regarding patient allocation and learning situations.
To allow the supervisor and the student time to get to know each other and plan their cooperation, they were to have a ‘float nurse’ function for their first shift together, i.e. have no specific patient responsibility but help where needed if required.
We set aside time for an extra follow-up conversation between the supervisor and student one week after the conversation about expectations in order to evaluate at an early stage whether the plans developed at that time were appropriate. The supervisors greatly appreciated these measures: ‘I think it’s good that we’ve been allowed to have a ‘floating’ role on the first day. And that has become the standard. That we’re together the first day, that we go around and look at things, and as long as it doesn’t affect the functioning of the unit, it’s really good to do this. Get to know each other and show the student round. That means that there’s a better flow of communication later.’
Having time to lay a good foundation for the clinical practice period proved to be valuable for both student and supervisor, and they benefitted from this later on: ‘I think I’ve become more conscious of the importance of informing administration that “my student needs this and that”, and in fact we’ve had very good cooperation with administration, so we’ve really achieved what we wanted to.’
During the project period, the supervisors became more aware of their own responsibility for facilitating good learning situations for the students. They found that management paid attention when they expressed their wishes and needs related to practice supervision.
Building a supervisory culture
The supervisors were concerned that the students should be made to feel welcome. At the start of the project period, a ‘getting-to-know-you’ day for students, the teacher and the supervisor group was held on the first day of clinical practice. The assistant professor presented the learning outcomes of the study, and the students and supervisors exchanged thoughts about their expectations.
The ‘getting-to-know-you day’ received positive evaluations and created a common understanding of the objectives of the clinical practice period. Moreover, this measure functioned as an arena for exchanging information about students’ learning in practice.
The supervisors felt that the ICU staff did not really understand that having a student could be an arduous task. They wanted their colleagues to demonstrate greater recognition of these supervisory tasks.
One of the supervisors expressed this as follows: ‘It’s not easy for the rest of the staff, like today with eight patients and the nurses running around […] It’s not as if we can just go and say “good luck”. And when you also get comments along the lines of “When will you be back?” it doesn’t feel good at all.’
In order to create a common understanding and culture for student supervision in the group of personnel, the supervisors took the initiative to hold internal tutorials about supervision. The project participants wanted to give something back in connection with the study. They also saw it as an advantage that their colleagues learned more about supervision. In addition, the project participants invited colleagues to participate in a discussion about the challenges and opportunities arising from having students in the unit.
The supervisors found that it was vital that the entire group of staff assumed collective responsibility for the students, including colleagues who had no specific supervisory responsibility. They emphasised that they themselves could help to build a supervisory culture by sharing their knowledge and experience, and by including colleagues in their work with students.
Discussion
The idea for the project stemmed from a desire to make practice supervision more attractive for intensive care nurses at the unit. There is evidence that supervisors need good support from management, and that good supervision can best be carried out if the supervision situation is well organised (3, 17).
The didactical relationship model stresses that all factors affect each other, i.e. the supervisory framework will influence how the supervisor and the student are able to work, etc. The framework will also affect the content that the supervisor manages to include in the supervision, in other words the areas in which supervision is possible (8). Framework factors are therefore crucial for the scope offered to both students and supervisors.
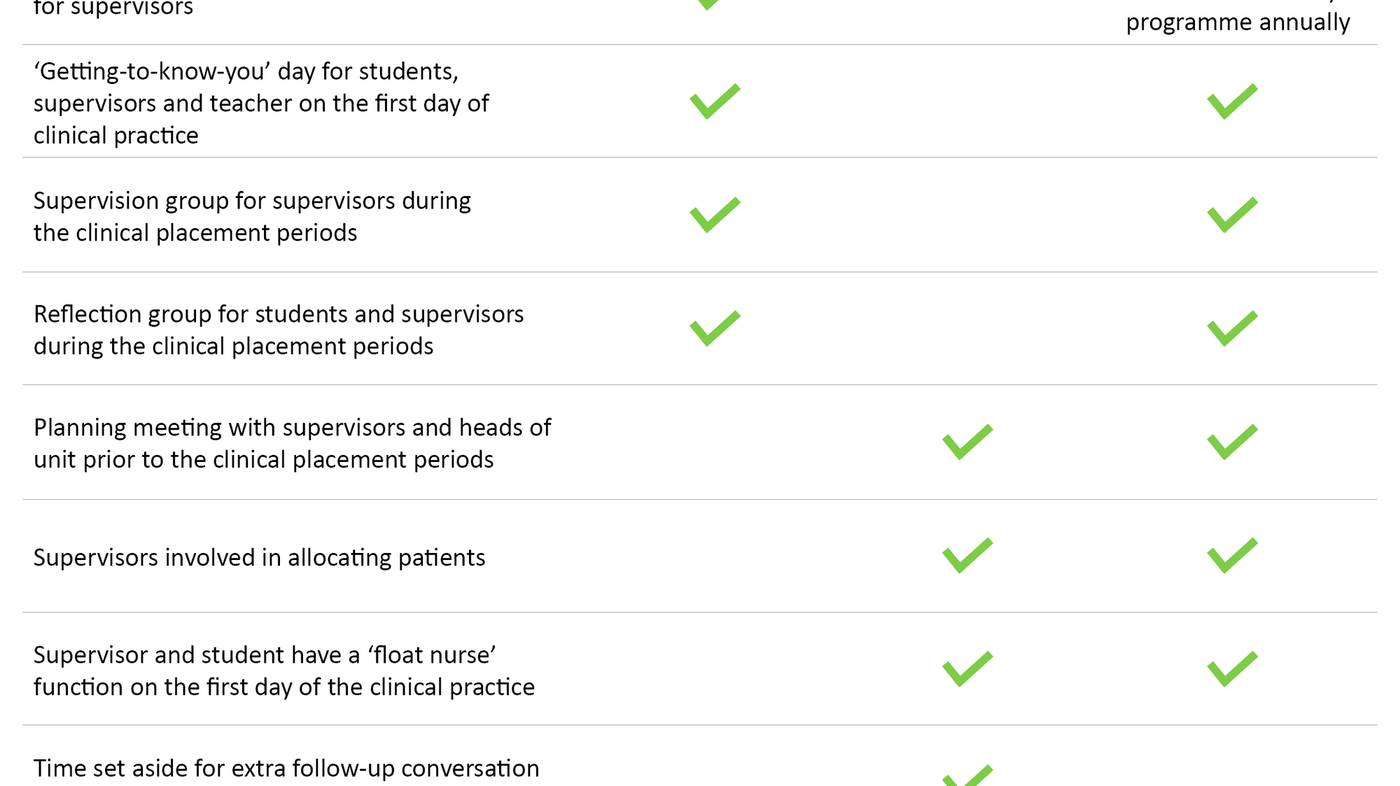
The changes implemented were partly introduced at the start of the project and partly during the project (Table 1). The first changes were a result of our assumptions about what would enhance the quality of supervision. We based these assumptions on research and experience from the unit. During the project, we assessed both established practice and the recently introduced activities, and made further changes on this basis.
Easy to implement the ‘float nurse’ function at an early stage
The relevant framework factors for good supervision of students in an intensive care unit encompass supervisory competence, daily work tasks and available resources in the form of time and organisation (17). The parameters in the project did not permit an increase in staffing or other resource-intensive measures to free up time for supervision.
However, we identified several minor adjustments that were feasible within the applicable financial and staffing parameters. The ‘float nurse’ function early in the practice period gave the supervisor and the student time to get to know each other and to put in place parameters for the cooperation between them. Although the ‘float nurse’ function was a simple change, it required planning and cooperation between the supervisors and management.
The change was made because the supervisors had been made responsible and had been challenged to suggest improvements themselves, while managers saw opportunities to make changes within the existing framework. Active and cooperative management was of key importance in implementing the measures. In earlier studies, the supervisors sought support from management and clear parameters (4).
Barriers to good supervision
The students’ learning process was a motivating factor for the supervisors, whilst framework factors that disturbed the learning process were demotivating. Factors such as time pressure, uncertainty about own competence and a feeling of being alone with responsibilities for students were highlighted as barriers to taking on supervisory tasks. These findings are supported by other research, which shows that ad hoc solutions in the organisation of supervision give poor results (2, 17).
The supervisors found that neither management nor colleagues understood how resource-intensive having supervisory responsibility was, a finding which is supported by several international studies (18, 19). Having supervisory responsibility together with responsibility for patients with complex needs was described as a challenging combination.
Impacts of changed framework factors
Even before any changes were implemented, the supervisors asserted that they felt positive about the efforts now being made to put in place a better framework for clinical practice supervision. During the project, the supervisors became more aware of their role. They took more responsibility, suggested improvements and participated actively in testing out changes. In line with the presentation in the didactical relationship model, we saw that when the framework factors changed, this had ripple effects on other factors of importance for supervision (8).
Even though the operational framework did not always permit the implementation of the supervisors’ suggestions for improvement, we found that the close dialogue between management and the supervisor group made it easier to find good solutions. Several studies show that uncertainty about the parameters and the content of the supervisory role represents a barrier to good supervision that makes the supervisors’ position more difficult (17, 20).
In our project, we highlight the responsibility embedded in the supervisory role, and clarify the opportunities supervisors have to influence their role. When supervisors took on more responsibility themselves, we found that they had more influence on their own work situation.
Supervisory responsibility became less lonely
The sense of community in the supervisor group also made supervision less lonely. It became a forum for learning in that supervisors shared their experiences and gave each other feedback on practical issues. Several studies have pointed out that supervisors feel lonely when they have sole responsibility for a student. They sought opportunities for greater cooperation and shared responsibility (4, 18).
Towards the end of the project period, the supervisors also emphasised the value of including other colleagues in student supervision through internal training and by utilising colleagues’ expertise. The supervisors themselves thus assumed responsibility for building a supervisory culture at the unit that could form a better framework for the practice supervision.
In the didactical relationship model, the framework is composed of given conditions that limit or facilitate learning (21). The changes that we have made in the framework factors (Table 1) are adjustments that we have good experiences of, and that promote a good learning process in line with the didactical relationship model.
Conclusion
There will always be a gap between what is desirable and what is feasible at a workplace with high activity, constant changes and limited financial and staffing resources. In this project, it has been important for us to adhere to measures that are feasible within the ordinary operating framework.
The sense of community and organisation have been the success factors for improving conditions for student supervision at the unit. Strengthening training and follow-up have increased the supervisors’ competence and commitment to student supervision. Closer cooperation between the supervisors and management has enabled us to see new opportunities to adapt the operation of the unit to supervision.
Through this project, we have found that small adjustments can provide substantial benefits that entail a higher quality of supervision in intensive care units.
References
1. Utdannings- og forskningsdepartementet. Rammeplan for videreutdanning i intensivsykepleie. Oslo; 2005. Available at: https://www.regjeringen.no/globalassets/upload/kilde/kd/pla/2006/0002/ddd/pdfv/269388-rammeplan_for_intensivsykepleie_05.pdf(downloaded 20.04.2018).
2. Trede F, Sutton K, Bernoth M. Conceptualisations and perceptions of the nurse preceptor's role: A scoping review. Nurse Education Today. 2016;36:268–74.
3. Martensson G, Engstrom M, Mamhidir AG, Kristofferzon ML. What are the structural conditions of importance to preceptors' performance? Nurse education today. 2013;33(5):444–9.
4. Hansen BS, Gundersen EM, Bjorna GB. Improving student supervision in a Norwegian intensive care unit: a qualitative study. Nursing & Health Sciences. 2011;13(3):255–61.
5. Hall-Lord ML, Theander K, Athlin E. A clinical supervision model in bachelor nursing education – purpose, content and evaluation. Nurse education in practice. 2013;13(6):506–11.
6. Nash DD, Flowers M. Key elements to developing a preceptor program. Journal of Continuing Education in Nursing. 2017;48(11):508–11.
7. Bjørndal B, Lieberg S. Nye veier i didaktikken? En innføring i didaktiske emner og begreper. Oslo: Aschehoug; 1978.
8. Hiim H, Keeping D, Hippe E. Undervisningsplanlegging for yrkesfaglærere. 3. ed. Oslo: Gyldendal Akademisk; 2009.
9. Hummelvoll JK. Kunnskapsdannelse i praksis : handlingsorientert forskningssamarbeid i akuttpsykiatrien. Oslo: Universitetsforlaget; 2003.
10. Sjøvoll N. Aksjonsforskning i sykepleie : en kommunikativ utfordring : en litteraturstudie av utviklingen i aksjonsforskning i sykepleien etter 1994. Bodø: Høgskolen i Bodø; 2002.
11. McNiff J. Action research : principles and practice. 3. ed. London: Routledge; 2013.
12. Wibeck V. Fokusgrupper : om fokuserade gruppintervjuer som undersökningsmetod. Lund: Studentlitteratur; 2000.
13. Kvale S, Brinkmann S, Anderssen TM, Rygge J. Det kvalitative forskningsintervju. 2. ed. Oslo: Gyldendal Akademisk; 2009.
14. Malterud K. Fokusgrupper som forskningsmetode for medisin og helsefag. Oslo: Universitetsforlaget; 2012.
15. Malterud K. Kvalitative metoder i medisinsk forskning : en innføring. 3. ed. Oslo: Universitetsforlaget; 2011.
16. Brinkmann S, Kvale S. InterViews : learning the craft of qualitative research interviewing. 3. ed. Thousand Oaks, California: Sage; 2015.
17. Williams L, Irvine F. How can the clinical supervisor role be facilitated in nursing: a phenomenological exploration. Journal of Nursing Management. 2009;17(4):474–83.
18. Valizadeh S, Borimnejad L, Rahmani A, Gholizadeh L, Shahbazi S. Challenges of the preceptors working with new nurses: A phenomenological research study. Nurse Education Today. 2016;44:92–7.
19. McCarthy B, Murphy S. Preceptors' experiences of clinically educating and assessing undergraduate nursing students: an Irish context. J Nurs Manag. 2010;18(2):234–44.
20. Omansky GL. Staff nurses' experiences as preceptors and mentors: an integrative review. J Nurs Manag. 2010;18(6):697–703.
21. Hiim H, Hippe E. Læring gjennom opplevelse, forståelse og handling : en studiebok i didaktikk. Oslo: Universitetsforlaget; 1993.









Comments