Inadequate documentation of nutritional practice in the specialist health service
Many medical records lacked information about nutritional risk, and few patients at nutritional risk were followed up.
Background: With few exceptions, all adult patients admitted to somatic departments must be screened for nutritional risk. Nutritional risk is associated with a reduced nutritional status resulting from increased nutritional needs, as well as from reduced nutritional intake or uptake, due to illness or treatment. Patients at nutritional risk should receive individual interventions to prevent or treat malnutrition, and these interventions should be documented in the patient’s medical record.
Objective: The objective of this study was to assess whether the nutritional care provided at Haukeland University Hospital complied with the recommendations in the national guidelines on prevention and treatment of malnutrition.
Method: We performed a retrospective survey of nutritional data from medical records.
Results: We reviewed 714 medical records from eight somatic departments. Screening of the patient’s nutritional risk was documented in 107 medical records (15%). Altogether 64 patients were assessed within 24 hours of admission, and 26 patients were identified to be at nutritional risk. A nutrition plan was recorded for 18 of the patients, and energy needs were calculated and energy intake was documented for two of these patients. Twenty-six discharge summaries included malnutrition diagnostic codes, but they did not correspond to the documentation of nutritional risk.
Conclusion: Documentation of nutritional care in the medical records at Haukeland University Hospital was inadequate and did not comply with national guidelines. A national initiative under the Norwegian Patient Safety Programme provides a unique opportunity to improve nutritional practice at the hospital.
Disease-related malnutrition is a major challenge for the health service, and has serious health and economic consequences (1–3). The prevalence of malnutrition varies from 18 to 45 per cent (2, 4–9), depending on the population measured and method used.
At Haukeland University Hospital (HUS), 29 per cent of hospitalised adult patients are at nutritional risk (10). Patients 70 years or older and those with infectious diseases, cancer and lung diseases are particularly at risk (6, 10). The nutritional risk in these groups is 40–43, 51, 44 and 42 per cent, respectively.
Identification of nutritional risk and early initiation of targeted nutritional treatment may increase energy intake (11), improve nutritional status, shorten recovery time following illness, prevent complications and death (12), and reduce the length of hospitalisation (13, 14).
Adequate nutritional practice
According to the national guidelines on prevention and treatment of malnutrition, adequate nutritional practice includes screening for nutritional risk, preparing a targeted nutrition plan for patients at risk and implementing interventions. It also involves documenting nutritional status and interventions in the patient’s medical record and discharge summary, and communicating this to the next phase of care (1).
Establishing routines for adequate nutritional practice is a challenge (15–17). Barriers that prevent nurses from providing adequate nutritional care are a lack of time, insufficient knowledge and skills, a lack of cross-disciplinary goals, and little involvement from management (18). Results from Norwegian qualitative studies show that nurses perceive a lack of involvement on the part of doctors, that risk assessment is given low priority because patients do not appear to need nutritional intervention, and that nurses have too many other duties (19, 20).
In 2006, HUS established a management-based nutrition strategy that included targeted efforts to implement good nutritional practice among nurses and doctors in order to introduce adequate nutritional care. The hospital established a cross-disciplinary, management-based nutrition network, introduced online courses and implemented mandatory registration of nutritional information to improve risk assessment skills and increase knowledge about prevention and treatment of nutritional risk.
Registration of nutritional information was conducted four times a year in which nurses, and later on doctors as well, submitted reports on the results of risk assessment (21). During the first two years, the proportion of patients screened for nutritional risk increased from 54 to 77 per cent, but only half of those found to be at nutritional risk received interventions to improve their nutritional status.
Geiker et al. compared the planned registration with a retrospective survey of medical records. They concluded that pre-planned, self-reported registration does not provide the best basis for assessing nutritional practice (22). Therefore, we wanted to study which information on nutritional status and nutritional practice is documented in medical records.
Objective of the study
The objective of the study was to survey medical record data to assess whether nutritional practice at HUS complied with recommendations in the national guidelines for prevention and treatment of malnutrition.
Research questions
The research questions were as follows:
- Are data on nutrition documented in medical records?
- Are the nutritional data documented in medical records at HUS in compliance with recommendations in the national guidelines for prevention and treatment of malnutrition?
Method
We conducted a retrospective data collection from medical records at HUS. Webport software generated a list of all hospitalised adult patients from eight different departments at 8 am on 4 November 2011.
The eight departments were as follows: internal medicine (which also included cardiovascular specialisations), orthopaedics, rehabilitation, oncology, surgery, internal medicine/surgery, neurology/surgery, and other departments that included head/throat, rheumatology, dermatology, ophthalmology and gynaecology. We collected data from the entire duration of the relevant hospital stay. Data collection was carried out by the lead author from 4 November 2011 to 1 May 2012.
Nutritional practice is routinely documented by doctors, nurses or clinical nutritional physiologists in the DIPS Electronic Patient Record using the following two assessment forms: 1) ‘Assessment of nutritional risk’, which is used to identify patients at nutritional risk, and 2) ‘Nutritional intervention/follow-up’, which is the nutrition plan and follow-up of the plan.
‘Assessment of nutritional risk’ consists of four introductory questions and one main survey, which is based on the NRS 2002 (Nutrition Risk Screening 2002) (1). The introductory questions are as follows:
- Is Body Mass Index (BMI) < 20.5?
- Has the patient lost weight in recent weeks?
- Has the patient had reduced nutritional intake in recent weeks?
- Is the patient seriously ill?
A positive response to at least one of the questions triggers more thorough documentation of the patient’s nutritional condition and level of severity of the illness. Age is given special consideration. ‘Nutritional interventions/follow-up’ is used to prepare a targeted nutrition plan for patients at nutritional risk and to document whether the plan is followed up.
We collected data on nutritional practice from the two assessment forms. We prepared a standardised registration form based on qualitative indicators from the national guidelines for prevention and treatment of malnutrition (1) and gathered the following information:
- the patient’s weight
- at nutritional risk or not
- whether the risk assessment had been carried out within 24 hours of admission
- whether the risk assessment had been conducted weekly for patients hospitalised for more than one week
If the patient was at nutritional risk, we gathered information about the nutrition plan and calculated the nutritional needs and nutritional intake.
Variables
In addition, we registered the following background variables from the medical records: length of hospitalisation, age, gender, and department and ward affiliation. From discharge summaries we collected information about the following ICD-10-CM Diagnosis Codes: E46 (at nutritional risk), E44 (moderate malnutrition) and E43 (severe malnutrition).
We used descriptive statistics to describe background variables and variables related to nutritional practice. Categorical variables were reported in absolute numbers and percentages. Numeric variables were reported as an average and standard deviation (SD). Length of hospitalisation was reported as the median with dispersion given as interquartile range (IQR 25–75 per cent).
We used the Mann-Whitney U test to compare age and length of hospitalisation between men and women, and the Kruskal-Wallis test to compare the difference in length of hospitalisation between age groups and departments (23).
We used a chi-squared test to examine the relationship between the proportion of patients found to be at nutritional risk, the proportion found to be at nutritional risk within 24 hours of admission, those for whom weight was recorded, and the background variables of gender, age groups and departments (23). We performed the analyses using SPSS version 24.0 (24).
Two nurses piloted the registration form for 25 medical records. Both nurses recorded the same information for all the items on the form.
Ethics
The study is part of a quality-enhancement project at HUS, and was approved by the data protection official at HUS in August 2011 (reference number 2011/4146).
Results
Of 726 relevant medical records, we included 714 in the study. Twelve medical records were excluded because the patients were pregnant (n = 6), terminally ill (n = 1), did not show up for the planned hospitalisation (n = 2), were registered as a participant in a research project (n = 2) or the medical record was not available (n = 1).
Patient characteristics
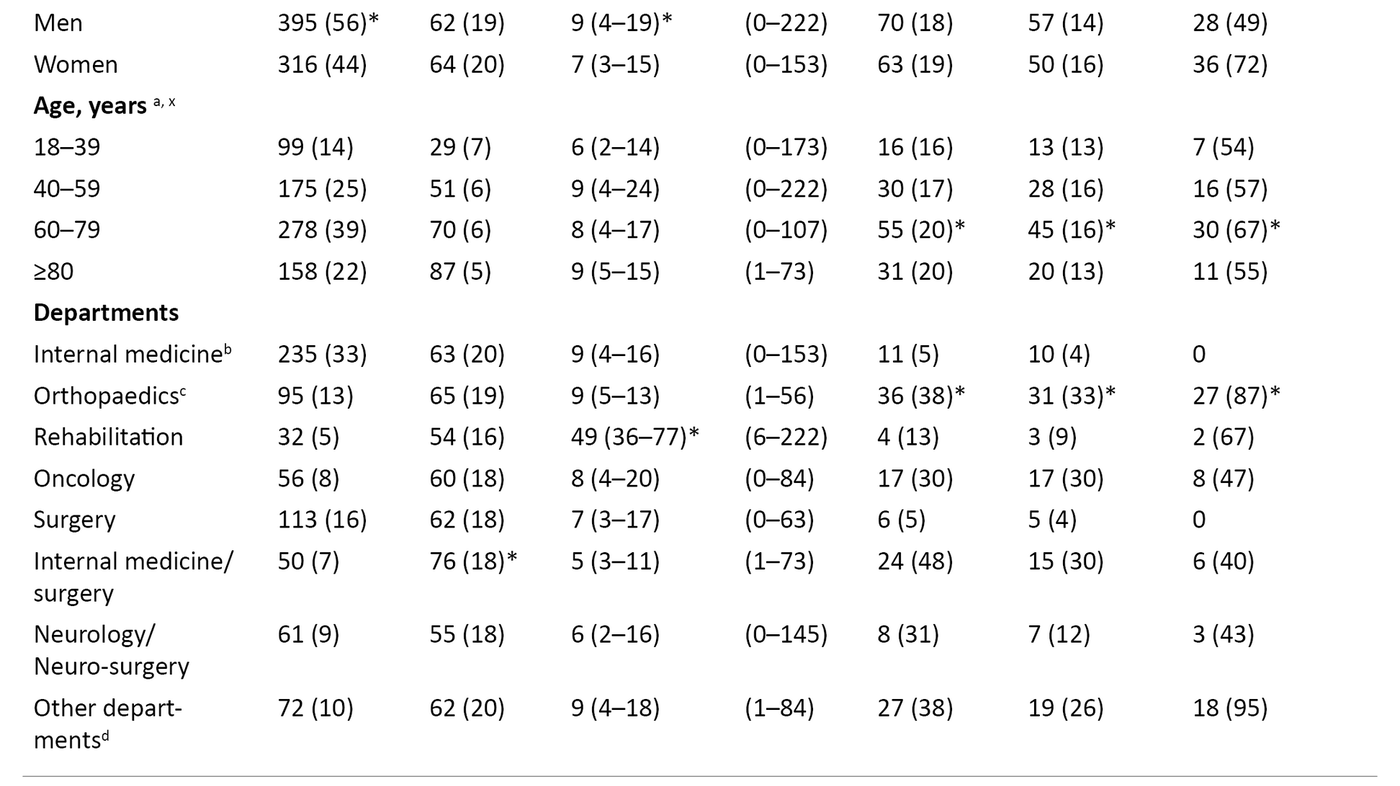
The average age was 63 years (SD 19.4), and there were more men than women (56 vs. 44 per cent, p = 0.04) (Table 1). Median length of hospitalisation was 8 days (IQR 4–17). Men had longer hospital stays than women (9 vs. 7 days, p = 0.01). Length of hospitalisation varied among departments and age groups. The longest hospital stays were recorded for patients admitted to the rehabilitation department (median 49 days, p < 0.05).
Patients in the age groups 40–59 years and older than 80 years had longer hospital stays than the youngest group of 18–39 years (median 9 days, IQR 4–24, median 9 days, IQR 5–15 and median 6 days, IQR 2–14, respectively).
Screening for nutritional risk
We found documentation of nutritional risk in 107 medical records (15%). Of these, 64 medical records (60%) were assessed within 24 hours of admission (Table 1). Two patients were assessed weekly during their hospital stay. This practice varied among the departments.
A larger proportion of patients were screened in the orthopaedic department (33%) than in the departments of internal medicine (4%, p ˂ 0.01), rehabilitation (9%, p = 0.026), oncology (30%, p = 0.191), surgery (4%, p ˂ 0.01) and neurology/neurosurgery (11 %, p < 0.01). Patients in the age group 60–79 years (16%) comprised the largest proportion screened compared to other age groups (p < 0.01). Weight was documented in 133 (19%) of the 714 medical records.
Nutritional interventions when nutritional risk is present
Of 107 patients screened for nutritional risk, 26 patients (24%) were found to be at nutritional risk – 16 men and 10 women. Eighteen of these patients (69%) received a nutrition plan – 13 men and 5 women. Nutritional needs and nutritional intake were calculated in two of the nutrition plans. In our data we found three nutrition plans for patients who were not assessed to be at nutritional risk.
Diagnosis
The diagnosis codes for malnutrition (the ICD-10-CM diagnosis codes E46, E44 and E43) were used in 26 discharge summaries. We found discrepancies between documentation of nutritional risk and the use of diagnosis codes for malnutrition. For example, 19 patients in the age group 60–79 years were given a diagnosis code for malnutrition in the discharge summary, but no information about nutritional risk was recorded in 7 of the medical records.
Discussion
We collected medical record data to obtain information about nutritional care at HUS. The survey of 714 medical records showed that information about nutritional practice in the medical records was inadequate and not in compliance with national guidelines.
We found no information about screening for nutritional risk in 85 per cent of the medical records. Almost 70 per cent of the patients at nutritional risk were given a nutrition plan, but the plans were not adequately followed up.
Previous documentation of nutritional practice
Our results differ significantly from the hospital’s quarterly registration which indicated that 70 per cent of the patients were screened and over half received a nutrition plan (21). Nutritional registration provides critical information about the prevalence of nutritional risk in the various patient populations, but does not adequately reflect the daily routines.
Similar differences between findings from medical records and planned registration of nutritional information were seen in a previous study at Rigshospitalet in Denmark (22). Geiker et al. found that 2393 medical records were examined in the period 2009–2010, and screening for nutritional risk was documented for only 8 per cent of the patients (22). In contrast, the planned registration showed that 70–80 per cent of the patients had been screened as required.
Our findings are consistent with previous studies that have looked at documentation of nutritional practice in medical records (7, 22, 25). A total of 590 medical records were examined at another Danish hospital (7). Screening for nutritional risk was documented in less than 8 per cent of the records, and few patients were followed up with a nutrition plan and interventions.
Results from a survey of medical record data at a Belgian hospital showed that important nutritional parameters for nutritional risk screening, such as body weight and height, were documented in only 22 per cent of 506 nursing records in the first three days following admission (25).
If the inadequate documentation we found actually reflects the hospital’s nutritional practice, this is a serious concern for patient safety. A previous survey at the hospital shows that one of three patients is at nutritional risk, which is associated with an almost five-fold higher mortality rate and 70 per cent more days in hospital than the subsequent year (3).
Such practice may have consequences for the hospital’s financial situation since preventive interventions for patients at nutritional risk are shown to reduce illness and length of hospitalisation (2). Documentation of nutritional status and nutritional practice is crucial information that should be communicated to the next phase of care upon discharge. When this documentation is missing, the next phase of care must conduct another screening and examination in order to prepare a nutrition plan.
Barriers to nutritional care
Previous studies have documented barriers to nutritional care (18–20, 26, 27). A main barrier to adequate nutritional treatment is a busy clinical day with many competing tasks (18, 20, 26, 27). Porter et al. reported that tasks such as clinical observations, attending to patient hygiene, administration of medication and documentation were prioritised over screening, prevention and treatment of nutritional risk (28).
Nurses state that they conduct their own clinical observations rather than use survey instruments (18, 20). Sufficient time and resources must be set aside to overcome common barriers that lead to inadequate nutritional practice (27, 29).
National guidelines emphasise that nutrition-related work is a joint responsibility shared by nurses, doctors and clinical nutritional physiologists (1, 30). However, nurses feel that they are alone in these efforts. They report that doctors show little involvement and interest and that clinical nutritional physiologists are not present (19, 20, 27). A clearer cross-disciplinary distribution of responsibility is necessary.
In addition, barriers to adequate nutritional practice arise during encounters with patients. Many patients are unable to provide information about their food intake or weight gain/loss (18). Poor appetite, nausea, constipation, and problems with chewing and swallowing are daily challenges in the health service.
Nurses feel that they must protect patient autonomy by accepting the patient’s reluctance to eat (27), and expressed concern that standardisation of nutritional treatment does not meet individual needs and wishes. More knowledge about nutrition is essential for addressing such challenges. It is also important to have ongoing training related to screening, prevention and treatment of nutritional risk in order to advance knowledge and skills (18). It is the responsibility of management to ensure sufficient expertise on nutrition within the organisation.
Inadequate documentation of nutritional practice may also be due to the current documentation system, which is not well suited for documenting nutritional status and the patient’s food intake in a systematic, effective and user-friendly manner.
Our findings are confirmed by O’Connell, who concludes that standardised documentation on separate assessment forms in the medical record (27), as is the case at HUS, makes information less accessible than an updated electronic graph in the record. Therefore, we believe that developing appropriate documentation systems that can structure, simplify and improve documentation of nutrition is a pre-condition of adequate nutritional practice and important for integrating nutrition into clinical practice.
National initiative on nutrition
Our findings show that nutrition has a legitimate place in the Norwegian Patient Safety Programme: In Safe Hands. Such a large-scale, national initiative with implementation of the national guidelines for prevention and treatment of malnutrition is crucial for patient treatment and hospital budgets.
Intervention packages have been prepared, tested and found to be feasible for use in clinical practice, and they are ready to be introduced nationwide in 2018. Local barriers should be identified to ensure successful implementation of the intervention packages (29).
Strengths and weaknesses of the study
A strength of the study is that data were collected from a large number of medical records from a university hospital where the management has been concerned about nutrition for many years.
A weakness of the study is that we cannot rule out that different documentation practices were used, e.g. that information about weight, nutritional status and nutritional intervention may have been documented in places other than in the dedicated assessment forms in the medical records that we surveyed. To our knowledge, our study is the first of its kind in Norway that documents nutritional care by using medical record data.
Conclusion
A survey of medical record data showed that documentation of the nutritional care provided at Haukeland University Hospital was inadequate and not in compliance with the guidelines. The large-scale initiative on nutrition under the Norwegian Patient Safety Programme is a unique opportunity to incorporate adequate, systematic nutritional practice. Sufficient knowledge, skills, clear distribution of responsibility, routines and systems are a precondition for success.
References
1. Helsedirektoratet. Nasjonale faglige retningslinjer for forebygging og behandling av underernæring. IS-1580. Oslo: Helsedirektoratet; 2013.
2. Sørensen J, Kondrup J, Prokopowicz J, Schiesser M, Krahenbuhl L, Meier R, et al. EuroOOPS: an international, multicentre study to implement nutritional risk screening and evaluate clinical outcome. Clin Nutr. 2008;27(3):340–9.
3. Tangvik RJ, Tell GS, Eisman JA, Guttormsen AB, Henriksen A, Nilsen RM, et al. The nutritional strategy: four questions predict morbidity, mortality and health care costs. Clin Nutr. 2014;33(4):634–41.
4. Imoberdorf R, Meier R, Krebs P, Hangartner PJ, Hess B, Staubli M, et al. Prevalence of undernutrition on admission to Swiss hospitals. Clin Nutr. 2010;29(1):38–41.
5. Lamb CA, Parr J, Lamb EI, Warren MD. Adult malnutrition screening, prevalence and management in a United Kingdom hospital: cross-sectional study. Br J Nutr. 2009;102(4):571–5.
6. Pirlich M, Schutz T, Norman K, Gastell S, Lubke HJ, Bischoff SC, et al. The German hospital malnutrition study. Clin Nutr. 2006;25(4):563–72.
7. Rasmussen HH, Kondrup J, Staun M, Ladefoged K, Kristensen H, Wengler A. Prevalence of patients at nutritional risk in Danish hospitals. Clin Nutr. 2004;23(5):1009–15.
8. Allard JP, Keller H, Jeejeebhoy KN, Laporte M, Duerksen DR, Gramlich L, et al. Malnutrition at hospital admission-contributors and effect on length of stay: A prospective cohort study from the Canadian Malnutrition Task Force. JPEN J Parenter Enteral Nutr. 2016;40(4):487–97.
9. Banks M, Ash S, Bauer J, Gaskill D. Prevalence of malnutrition in adults in Queensland public hospitals and residential aged care facilities. Nutrition & Dietetics. 2007;64(3):172–8.
10. Tangvik RJ, Tell GS, Guttormsen AB, Eisman JA, Henriksen A, Nilsen RM, et al. Nutritional risk profile in a university hospital population. Clin Nutr. 2015;34(4):705–11.
11. Jie B, Jiang ZM, Nolan MT, Efron DT, Zhu SN, Yu K, et al. Impact of nutritional support on clinical outcome in patients at nutritional risk: a multicenter, prospective cohort study in Baltimore and Beijing teaching hospitals. Nutrition. 2010;26(11–12):1088–93.
12. Stratton RJ, Elia M. Who benefits from nutritional support: what is the evidence? Eur J Gastroenterol Hepatol. 2007;19(5):353–8.
13. Johansen N, Kondrup J, Plum LM, Bak L, Norregaard P, Bunch E, et al. Effect of nutritional support on clinical outcome in patients at nutritional risk. Clin Nutr. 2004;23(4):539–50.
14. Kruizenga HM, Van Tulder MW, Seidell JC, Thijs A, Ader HJ, Van Bokhorst-de van der Schueren MA. Effectiveness and cost-effectiveness of early screening and treatment of malnourished patients. Am J Clin Nutr. 2005;82(5):1082–9.
15. Johansson U, Rasmussen HH, Mowe M, Staun M, Scandinavian Nutrition Group. Clinical nutrition in medical gastroenterology: room for improvement. Clin Nutr. 2009;28(2):129–33.
16. Mowe M, Bosaeus I, Rasmussen HH, Kondrup J, Unosson M, Irtun O. Nutritional routines and attitudes among doctors and nurses in Scandinavia: a questionnaire based survey. Clin Nutr. 2006;25(3):524–32.
17. Meijers JM, Halfens RJ, van Bokhorst-de van der Schueren MA, Dassen T, Schols JM. Malnutrition in Dutch health care: prevalence, prevention, treatment, and quality indicators. Nutrition. 2009;25(5):512–9.
18. Green SM, James EP. Barriers and facilitators to undertaking nutritional screening of patients: a systematic review. J Hum Nutr Diet. 2013;26(3):211–21.
19. Juul HJF, Jan C. Kartlegging av underernæring i sykehus. Nordisk Sygeplejeforskning. 2013;3(2):77–89.
20. Eide HD, Halvorsen K, Almendingen K. Barriers to nutritional care for the undernourished hospitalised elderly: perspectives of nurses. J Clin Nurs. 2015;24(5-6):696–706.
21. Tangvik RJ, Guttormsen AB, Tell GS, Ranhoff AH. Implementation of nutritional guidelines in a university hospital monitored by repeated point prevalence surveys. Clin Nutr. 2012;66(3):388–93.
22. Geiker NR, Horup Larsen SM, Stender S, Astrup A. Poor performance of mandatory nutritional screening of in-hospital patients. Clin Nutr. 2012;31(6):862–7.
23. Field A. Discovering statistics using IBM SPSS Statistics. 4. utg. London: SAGE Publications; 2013.
24. IBM Corp. Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp; 2016.
25. Geurden B, Wouters C, Franck E, Weyler J, Ysebaert D. Does documentation in nursing records of nutritional screening on admission to hospital reflect the use of evidence-based practice guidelines for malnutrition? Int J Nurs Knowl. 2014;25(1):43–8.
26. Ross LJ, Mudge AM, Young AM, Banks M. Everyone's problem but nobody's job: Staff perceptions and explanations for poor nutritional intake in older medical patients. Nutrition & Dietetics. 2011(68):41–6.
27. O’Connell MB, Jensen PS, Andersen SL, Fernbrant C, Norholm V, Petersen HV. Stuck in tradition. A qualitative study on barriers for implementation of evidence-based nutritional care perceived by nursing staff. J Clin Nurs. 2017;27(3–4):705–14.
28. Porter J, Raja R, Cant R, Aroni R. Exploring issues influencing the use of the Malnutrition Universal Screening Tool by nurses in two Australian hospitals. J Hum Nutr Diet. 2009;22(3):203–9.
29. Fischer F, Lange K, Klose K, Greiner W, Kraemer A. Barriers and strategies in guideline implementation. A scoping review. Healthcare (Basel). 2016;4(3):36.
30. Kondrup J, Allison SP, Elia M, Vellas B, Plauth M. ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22(4):415–21.









Comments