Healthcare personnel’s recognition of people with hydrocephalus affects their self-esteem
While the illness is potentially life-threatening, it is invisible and not well known. Consequently, patients may be mistrusted and ignored, and they may feel inferior, vulnerable and insecure.
Background: Hydrocephalus is a chronic illness that often requires lifelong follow-up by healthcare personnel. However, the illness is not well known, and the symptoms are often invisible. This may make it difficult for patients to be taken seriously when interacting with healthcare personnel. The patient perspective in the treatment of hydrocephalus appears to be under-researched.
Objective: The objective of the study was to investigate and describe experiences related to recognition from healthcare personnel for people with hydrocephalus.
Method: This is a descriptive, explorative study that employs a qualitative methodology. We conducted 13 individual interviews and one focus group discussion with adults with hydrocephalus. Hermeneutical principles were used generally in the analysis and interpretation. The analysis was inspired by qualitative content analysis.
Results: The analysis revealed four main categories:
to be believed and acknowledged
to be mistrusted and ignored
to promote mental and emotional balance
to contribute to mental and emotional imbalance
Conclusion: The experience of being recognised when interacting with healthcare personnel can be highly significant for how people with hydrocephalus perceive themselves and their situation. The results indicate that recognition can lead to empowerment, while a lack of recognition can contribute to powerlessness. Empowerment at individual level can be described as having a sense of control over one’s own life and health.
Hydrocephalus is an illness characterised by abnormal circulation of the cerebrospinal fluid. The illness may be congenital or it may develop secondarily as a result of other conditions (1). The most common treatment is surgical implantation of a shunt that diverts the flow of cerebrospinal fluid from the brain to the abdominal cavity (1).
Many patients live their lives without limitations despite having been treated for hydrocephalus. In some patients, it may be difficult to achieve optimal drainage, and for them hydrocephalus means living with an invisible, chronic illness. Headaches, fatigue and cognitive impairments are common (1–3). There is always a risk that the shunt will fail, which can be life-threatening in some cases (1).
For many people, living with hydrocephalus entails lifelong follow-up by the health services (4). Some patients require numerous operations. In addition to surgical treatment, many need follow-up nursing care to help them live with the illness. In spite of this, the patient perspective in the treatment of hydrocephalus appears to be under-researched.
Norway does not have a national registry for hydrocephalus, and it is unknown how many people live with the diagnosis. In Norway, approximately 2200 hydrocephalus-related operations are performed each year across five neurosurgical departments (5). In addition, healthcare personnel in neurosurgical departments and in the primary health services encounter this patient group both pre- and post-operatively. Thus, the number of healthcare workers who deal with this patient group is quite large.
Recognition of people with the diagnosis
In the experience of the first and second authors, the diagnosis of hydrocephalus is not well known outside of the specialised hospital departments. Research indicates that adults with hydrocephalus do not always receive the follow-up they need, probably because the health services have not given the illness sufficient attention (4). Studies show that recognition of patients and their illness may be significant for how they perceive their own situation (6–10).
Recognition was first postulated as a philosophical concept by Hegel. The Norwegian psychologist Schibbye writes about Hegel’s philosophy using practical, clinically oriented language (11). Experiences related to recognition may have profound importance because we as human beings need to be recognised in order to maintain our identity and self-esteem (12). The German philosopher Honneth also uses Hegel as his point of departure when he writes that disrespect is the opposite of recognition (12). Disrespect destroys identity and self-esteem (12).
Recognition is one of the main principles of empowerment, as this term is understood in a health-promoting perspective (13, 14). Empowerment at individual level may be described as a process in which individuals gain greater control over their own lives and health (13–15). Helping patients to gain control is a crucial part of the professional practice of healthcare workers (14).
Objective of the study
The objective of this study is to investigate and describe the significance of experiences related to recognition for people with hydrocephalus.
Although hydrocephalus can be compared to other chronic illnesses, it is different because it can become life-threatening at a moment’s notice. Improper treatment can cause irreparable harm. The patient’s subjective symptoms are important for assessing whether or not the patient requires emergency medical treatment (1). This, along with lack of attention to the illness, is the reason why we chose to study the significance of recognition for people with hydrocephalus.
Method
Design
This is a descriptive, explorative study that employs a qualitative methodology. We used hermeneutical principles to analyse and interpret the data. This perspective was chosen because it accentuates the contextual basis of people’s interpretations and understandings (16). The informants as well as two of the authors had a connection to the topic under study, and it was therefore appropriate to take such a perspective. We recorded our preconceptions in writing before the study commenced so that we would be aware of them during the research process.
The first and second authors conducted the study in cooperation with the third and fourth authors, who served as supervisors.
Data collection
We chose individual interviews and a focus group discussion as our method of data collection. By conducting individual interviews, we could investigate the informants’ thoughts and experiences, and through a focus group discussion we could explore the range of viewpoints. Interaction in focus groups generates different data than individual interviews (17).
The sample was appropriate, meaning that the respondents had the competence to answer. The informants were recruited through the Norwegian Association for Spina Bifida and Hydrocephalus. The inclusion criteria were as follows: a member of the association, has hydrocephalus, over 18 years old, and speaks Norwegian. Those with spina bifida were excluded. The association’s general manager sent out invitations to all relevant members, and the members who wished to participate contacted us.
We conducted 13 individual interviews divided between the first and second authors, and one focus group discussion in which the first and second authors were present. We collected the data in the autumn of 2014. Five of the individual interviews were held at the Oslo and Akershus University College (HiOA), now OsloMet – Oslo Metropolitan University, two at a different public location, one at the home of the informant and five on the telephone.
We held the focus group discussion at HiOA after the individual interviews were completed. Four of the 13 informants were present. The interview guides were semi-structured and contained questions about the informants’ thoughts and experiences related to recognition when interacting with healthcare personnel (Table 1). We made an audio recording which was saved on a password-protected computer. The first and second authors transcribed the interviews. The individual interviews ran from 22 to 80 minutes, and the focus group discussion lasted 74 minutes.
The group of informants consisted of 8 women and 5 men from 23 to 43 years old, with an average age of 35. Seven of them had congenital hydrocephalus and 6 had secondary hydrocephalus. The informants stated that they had been admitted to hospital 3 to 50 times, which is an average of 17 hospital admissions. The patient group is relatively small on a national basis. To ensure the anonymity of the informants, we do not provide any further demographic data.
The transcribed material was analysed using qualitative content analysis inspired by Kvale and Brinkmann (17). Qualitative content analysis entails an analysis of the content and meaning of texts in the context in which they appear (17). First, we read the transcriptions of the individual interviews to form an overall impression. Then we identified meaningful words and sentences. Meaningful units were condensed into sub-categories, and the sub-categories were abstracted to main categories.
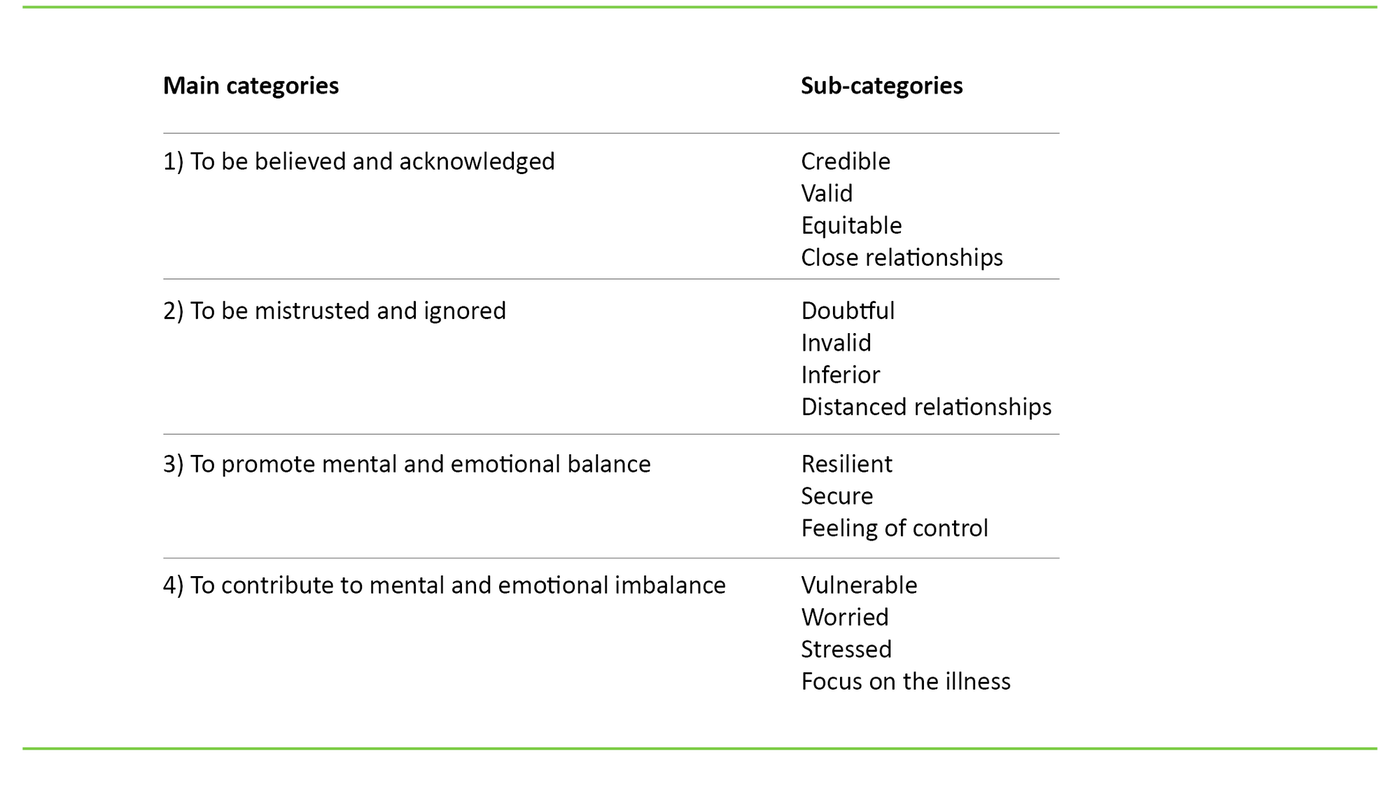
The analysis revealed 15 sub-categories, which we abstracted to four main categories. The analysis of the focus group discussion uncovered no new information that had not already come to light in the individual interviews. The focus group discussion was used to validate the individual interviews. Hermeneutical principles of interpretation emphasise a continual process of shifting back and forth between the parts and the whole and between preconceptions and new understanding (17). As a result, the phases of the analytical process were not linear.
Ethical considerations
We conducted the study in accordance with the ethical guidelines set out for nursing research in the Nordic countries (18). The study was not encompassed by Section 2 of the Norwegian Health Research Act (19), and could be conducted without the approval of the Regional Committees for Medical and Health Research Ethics (REK). The study was approved by the Norwegian Centre for Research Data (reference no. 38995/3/AMS).
The informants received verbal and written information about the study’s content and objective. They were guaranteed anonymity, informed that their participation was voluntary, and that they were free to withdraw whenever they wished. All of them signed informed consent forms in which they were asked to take part in an individual interview and a focus group discussion.
The study’s first and second authors are nurses in a neurosurgical department. Five of the informants had met the authors before. We reflected on ethical dilemmas that could arise as the result of our dual role, which could cause informants to withhold information or provide more information than they wished to (17). This dual role required particular sensitivity, and is discussed in the section on the study’s limitations.
Results
The main categories and sub-categories are presented in Table 2. The first two main categories deal with the informants’ thought and experiences related to recognition. The final two address the significance of their experiences. We present the results in four paragraphs which are summarised with the associated main categories. The sub-categories are presented throughout and are exemplified with quoted material.
Recognition – to be believed and acknowledged as a person
For the informants, recognition meant that their experiences were regarded as credible and valid. One patient stated the following: ‘The most important thing is to be believed; it’s more important than water’. They used words such as listening, understanding, acceptance and acknowledgement to describe recognition. Recognition also meant that their relationship with the healthcare personnel was equitable and friendly. Several used the word ‘compassionate’ about healthcare workers who gave them recognition.
Care, time and involvement were significant for whether or not the patients felt recognised. One described recognition when interacting with nurses like this: ‘The ones who take the time to listen to you when you’re feeling down, even if it’s just two minutes, to have a chat and be acknowledged’.
Lack of recognition – to be mistrusted and ignored
A lack of recognition meant that their experiences were regarded as questionable or invalid. Several patients talked about situations in which healthcare personnel doubted their experiences, e.g. by making statements such as: ‘Are you sure you have a headache?’.
Many patients felt that clinical findings were taken more seriously than their subjective experience. Several of them talked about similar experiences: ‘They believed me after an intracranial pressure measurement. Then I had proof for what I had been saying all along.’ Another said the following: ‘I wish I could have said: “You know what? It was no joke! Why didn’t you listen to me?”’.
According to the informants, one reason they were not taken seriously was that their symptoms are invisible. Some emphasised that the competence level of the healthcare personnel was significant for whether they were taken seriously. A lack of recognition also entailed feelings of inferiority in their relationship with healthcare workers and that the healthcare personnel distanced themselves from them. Several had experienced condescending attitudes. One felt that she was treated like a ‘pawn in a game’. Another said the following about her interactions with healthcare workers: ‘I could have been a stone they kicked along the road’.
The sub-categories suggest that recognition at its deepest level meant that the informants felt they were believed and acknowledged as a person, while a lack of recognition implied being mistrusted and ignored.
Recognition promotes mental and emotional balance
Recognition appeared to enhance the informants’ resilience and sense of security. One said the following: ‘It’s been most important for how I think about myself.’ Another said this: ‘Your self-confidence gets a boost when you are believed.’ Recognition had a positive impact on the patients’ disposition and helped to increase optimism and peace of mind. Recognition could establish trust in the health services and create a sense of security about living with the illness.
One informant said the following: ‘The road to the hospital doesn’t feel so long, and this means that I need it less, because I know I will be taken seriously when I contact them’. Another described a sense of security like this: ‘No one can live your life for you, but if you use the health services like crutches to help you hold your balance, it gives you a sense of security.’
Recognition could also contribute to a sense of control because patients were spared the stress of fighting to be believed, while at the same time recognition increased their acceptance and understanding of their own situation. One informant said: ‘To finally be taken seriously has helped me to accept my situation and set realistic goals’.
Lack of recognition contributes to mental and emotional imbalance
In contrast, it appeared that a lack of recognition led to vulnerability and worry. One informant said: ‘Your self-confidence plummets when you are not believed’. Another noted that recognition or a lack of recognition from neurosurgeons had the greatest impact on their feelings about themselves: ‘What is said by those who know something about your challenges has a huge impact. You feel very insignificant.’
Lack of recognition created a sense of powerlessness, dejectedness and frustration, and could erode patients’ confidence in the health services and increase their fear of being ill. Lack of recognition from healthcare personnel could also cause them to keep quiet about their own situation. One informant said: ‘It was difficult to say that I had problems that were not recognised or that did not exist except in my head’. Lack of recognition increased stress and a focus on the illness because the patients had to spend their time and energy on being believed.
Some found it difficult to contact the health services and struggled with their challenges by themselves. Some were more focused on their symptoms and searched for explanations on their own. One tried alternative treatment. One got sterilised in the hope that oral contraceptives were causing her symptoms. Others began to look at their close relationships as a possible cause of their challenges.
The sub-categories suggest that recognition promoted mental and emotional balance in the situations that the informants were in, while a lack of recognition contributed to mental and emotional imbalance.
Discussion
In this section, we discuss the significance of experiences related to recognition for the informants.
Small gestures – major consequences
The informants described recognition using words such as listening, understanding, acceptance and acknowledgement. These qualities are embodied in an attitude of recognition (11). The informants emphasised the importance of equity in relationships. Equity is regarded as a precondition for recognition in a relationship (11).
Informants said that a lack of recognition entailed a feeling of inferiority and invalidation of their experiences by healthcare personnel. Such experiences can be degrading and are a form disrespect. Degradation can have a negative impact on people’s self-esteem and identity because they feel that they are stripped of their own worth (12).
The results indicate that recognition strengthened the informants by enhancing their resilience, sense of security and feeling of control. On the other hand, a lack of recognition led to vulnerability, worry, stress and a focus on the illness. Studies confirm that recognition has an enhancing effect because of its positive impact on self-confidence and self-esteem, and because recognition initiates a process of acceptance and self-understanding (6–10). In contrast, a lack of recognition can weaken self-confidence and self-esteem as well as increase isolation and loneliness (6–10).
Perhaps recognition in encounters with healthcare personnel is particularly significant for people with hydrocephalus because the symptoms are invisible and the illness is not well known. This can make it difficult for patients to elicit understanding from most people. Studies suggest that recognition in encounters with healthcare personnel is especially crucial for patients with subjective symptoms (6–10).
Recognition can validate patients’ experiences and spare them from having to fight for their credibility (8, 9). Some people with hydrocephalus live in fear that their illness will become life-threatening without proper treatment. We can assume that this fear increases their need for recognition.
The informants felt that clinical findings were viewed as more valid than their subjective experiences. It can be comforting that healthcare personnel do not diagnose or treat without objective documentation indicating that it is appropriate. By the same token, listening to the patient is essential for proper diagnosis and treatment (20). Perhaps it is especially important in this context because optimal diagnosis and treatment options are still being developed (21). We can assume that current medical equipment does not always provide adequate answers.
There may be a basis for asserting that recognition of health symptoms can lead to greater focus on the illness. However, this and other studies suggest the opposite (6, 7, 22). The results indicate that a lack of recognition resulted in greater focus on the illness. Several patients tried to find reasons for their symptoms when they were not believed. It is common for patients to interpret their symptoms themselves when there is no dialogue with healthcare personnel (23). On one hand, this can be viewed as the patient taking active steps to address his or her own situation. On the other hand, it can result in more health problems if the patient tries out risky treatment.
We wonder if the informants interpreted a lack of recognition more negatively than the healthcare personnel were aware of. Small gestures, such as speaking encouraging words and listening to the patient, were highly significant for whether or not they felt recognised.
In general, people with a chronic illness can be sensitive and interpret comments in a negative way because chronic illness in itself can be detrimental to one’s self-confidence (24). The fact that we raise this question, however, should not be used to fail to hold healthcare personnel accountable, but rather to remind them of how important even the smallest of gestures may be to the patient.
On the path to empowerment
One way to understand the results is that recognition helped to put the informants on the path to empowerment because recognition gave them a sense of control. Studies indicate that recognition in encounters with healthcare personnel can lead to an empowerment process in the patient (8, 10, 25).
In contrast, the results can be interpreted to mean that a lack of recognition led to powerlessness. When the informants were not acknowledged or believed, they felt powerless to take constructive action to address their situation. Powerlessness is regarded as the opposite of empowerment (26). Studies confirm that there is a correlation between a lack of recognition and a sense of powerlessness (6, 7, 10).
The results suggest that recognition helped the informants to think differently about their own situation. Schibbye (11) confirms that recognition promotes self-reflection and heightened awareness. In their study, Aujoulat et al. assert that an expression of control is only a valid indicator of an empowerment process if the person also expresses some type of change in his or her values and priorities around living with a chronic illness (27).
Feeling recognised can bring about change in a person’s values and priorities through self-reflection, and can therefore be linked to a person’s empowerment process (27).
Significance for practice
A hectic workday can make it difficult for healthcare workers to keep recognition in mind. However, the results indicate that even small gestures are meaningful. Even during busy moments it should be possible to have an attitude of recognition when interacting with patients. Perhaps the attitudes and skills of healthcare personnel constitute a greater threat to recognition than a lack of time. Studies confirm that the ability of healthcare personnel to instigate dialogue, show empathy and engage in ethical reflection can be significant for whether they take the patient seriously (28, 29).
The results suggest that if patients feel more secure, they may seek out health services less frequently. As one informant said, the knowledge that one is taken seriously can provide a sense of security about living with the illness. It is conceivable that healthcare personnel can contribute to making savings in the health sector if their awareness is raised about interacting with this patient group with an attitude of recognition.
Strengths and limitations of the study
The authors’ dual role may have affected the study’s reliability. We attempted to use our background knowledge for the benefit of the informants and the data. We spoke with the informants about our dual role, were sensitive to how the interview impacted them emotionally and made adaptations based on their physical condition.
When we interviewed the patients who had met us before, we emphasised that their comments would be anonymous and would not have an impact on the follow-up they received in the department so that, for example, they would not be afraid to express negative views.
As a result of our dual role, we may have overlooked interesting perspectives in the analysis and interpretation. At the same time, this may have helped us to identify perspectives that others would not have noticed. We have strived for reliability in the study by being as transparent as possible in our account of the research process (17). The results correspond with similar studies, which may indicate that our study has transfer value to other patient groups.
The focus group discussion did not generate new information. The reason may be the composition of the group, the researchers’ ability to lead the group or that people with hydrocephalus can have cognitive impairments that make it difficult for them to concentrate in a group (2, 17). However, the content of the focus group discussion corresponded with the individual interviews. It is unknown whether we would have obtained more information by holding another focus group discussion.
The fact that several researchers analysed the data bolsters the study’s reliability. Reliability could have been strengthened even further if the informants had validated the results and interpretations. The relevance of the study could have been greater if people with hydrocephalus had participated in the research process, as recommended by the Ministry of Health and Care Services (30).
Conclusion
Being recognised can be significant for how people with hydrocephalus perceive themselves and their own situation. The results indicate that recognition can lead to empowerment, while a lack of recognition can contribute to powerlessness.
Recognition from healthcare personnel may be especially crucial because the illness is invisible, not well known and potentially life threatening. To avoid negative ripple effects, healthcare personnel must have an attitude of recognition when interacting with this patient group. More research on the patient perspective in the treatment of people with hydrocephalus is needed.
References
1. Berg-Johnsen J. Introduksjon til nevrokirurgi. Oslo: Legeforlaget; 2012.
2. Paulsen H, Lundar T, Lindegaard KF. Twenty-year outcome in young adults with childhood hydrocephalus: assessment of surgical outcome, work participation, and health-related quality of life. J Neurourg Pediatrics. 2010;6(6):527–35.
3. Rekate HL, Kranz D. Headaches in patients with shunts. Semin Pediatr Neurol. 2009;1(24):1–4.
4. Simon TD, Lamb S, Murphy NA, Hom B, Walker ML, Clark EB. Who will care for me next? Transitioning to adulthood with hydrocephalus. Paediatrics. 2009;124(5):1431–7.
5. Eide PK. Årsrapport 2016 for hydrocephalusseksjonen. Oslo: Oslo universitetssykehus HF, nevrokirurgisk avdeling; 2016.
6. Zangi HA, Hauge MI, Steen E, Finset A, Hagen KB. «I am not only a disease, I am so much more» Patients with rheumatic diseases’ experiences of an emotion-focused group intervention. Patient Educ Couns. 2011;85(3):419–24.
7. Lind AB, Risoer MB, Nielsen K, Delmar C, Christensen MB, Lomborg K. Longing for existential recognition: A qualitative study of everyday concerns for people with somatoform disorders. J Psychosom Res. 2014;76(2):99–104.
8. Werner A, Malterud K. «The pain isn’t as disabling as it used to be»: How can the patient experience empowerment instead of vulnerability in the consultation? Scand J Public Health. 2005;33(66):41–6.
9. Werner A, Steihaug S, Malterud K. Encountering the continuing challenges for women with chronic pain: recovery through recognition. Qual Health Res. 2003;13(4):491–509.
10. Skuladottir H, Halldorsdottir S. Women in chronic pain: Sense of control and encounters with health professionals. Qual Health Res. 2008;18(7):891–901.
11. Schibbye ALL. Relasjoner. Et dialektisk perspektiv på eksistensiell og psykodynamisk psykoterapi. Oslo: Universitetsforlaget; 2012.
12. Honneth A. Kamp om anerkjennelse. Oslo: Pax forlag; 2008.
13. Verdens helseorganisasjon. The Ottawa charter for health promotion. Genève: Verdens helseorganisasjon; 1986.
14. Tveiten S. Den vet best hvor skoen trykker … Om veiledning i empowermentprosessen. Bergen: Fagbokforlaget; 2007.
15. Gibson CH. A concept analysis of empowerment. J Adv Nurs. 1991;16(3):354–61.
16. Ellingsen S, Drageset S. Kvalitativ tilnærming i sykepleieforskning: en introduksjon og oversikt. Norsk tidsskrift for sykepleieforskning. 2008;10(3):23–38.
17. Kvale S, Brinkmann S. Det kvalitative forskningsintervju. Oslo: Gyldendal Akademisk; 2012.
18. Sykepleiernes Samarbeid i Norden. Etiske retningslinjer for sykepleieforskning i Norden. Available at: http://ssn-norden.dk/wp-content/uploads/2016/01/SSNs-etiske-retningslinjer.pdf(downloaded 27.08.2018).
19. Lov 20 juni 2008 nr. 44 om medisinsk og helsefaglig forskning (helseforskningsloven). Available at: https://lovdata.no/dokument/NL/lov/2008-06-20-44(downloaded 15.09.2014).
20. Jagosh J, Boudreau JD, Steinert Y, MacDonald ME, Ingram L. The importance of physician listening from the patients’ perspective: Enhancing diagnosis, healing, and the doctor-patient relationship. Patient Educ Couns. 2011:85(3):369–74.
21. Williams MA, McAllister JP, Walker ML, Kranz DA, Bergsneider M, Del Bigio MR et al. Priorities for hydrocephalus research: report from a National Institutes of Health-sponsored workshop. J Neurosurg. 2007;107(5):345–57.
22. Paterson BL. The Shifting perspectives model of chronic illness. J Nurs Scholarsh. 2001;33(1):21–6.
23. Nygårdh A, Malm D, Wikby K, Ahlström G. The experience of empowerment in the patient-staff encounter: the patient's perspective. J Clin Nurs. 2011;21(5-6):897–904.
24. Charmaz K. Loss of self: a fundamental form of suffering in the chronically ill. Sociol Health Illn. 1983;5(2):168–95.
25. Tveiten S, Knutsen IR. Empowering dialogues – the patients’ perspective. Scand J Caring Sci. 2011;25(2):333–40.
26. Rappaport J. Studies in empowerment: introduction to the issue. Prevention in human services. 1984;3(1):1–7.
27. Aujoulat I, Marcolongo R, Bonadiman L, Deccache A. Reconsidering patient empowerment in chronic illness: A critique of models of self-efficacy and bodily control. Soc Sci Med. 2008;66(5):1228–39.
28. Rundquist E, Lindström UÅ. Empowerment and authorization – who provides and who receives? A qualitative meta-study of empowerment in nursing research: a caring science perspective. International Journal for Human Caring. 2005;9(4):24–32.
29. Pedersen R, Hofmann B, Mangset M. Pasientautonomi og informert samtykke i klinisk arbeid. Tidsskr Nor Lægeforen. 2007;127(12):1644–7.
30. Helse- og omsorgsdepartementet. HelseOmsorg21. Et kunnskapssystem for bedre folkehelse. Nasjonal forsknings- og innovasjonsstrategi for helse og omsorg. 2014. Available at: https://www.regjeringen.no/contentassets/8ab2fd5c4c7746dfb51e3f64cd4d71aa/helseomsorg21_strategi_web.pdf?id=2266705(downloaded 02.05.2015).









Comments