Evidence-based practice in nursing education
The study suggests that if evidence-based practice is taught systematically, it affects the students' learning outcome.
Background: Evidence-based practice (EBP) is expected to underlie decisions in the healthcare environment. This requires that the professional nurses use the EBP process. According to HelseOmsorg21, the Norwegian nursing education only modestly responds to the challenges healthcare faces within this framework.
Objective: To examine and describe research literature about EBP in nursing education.
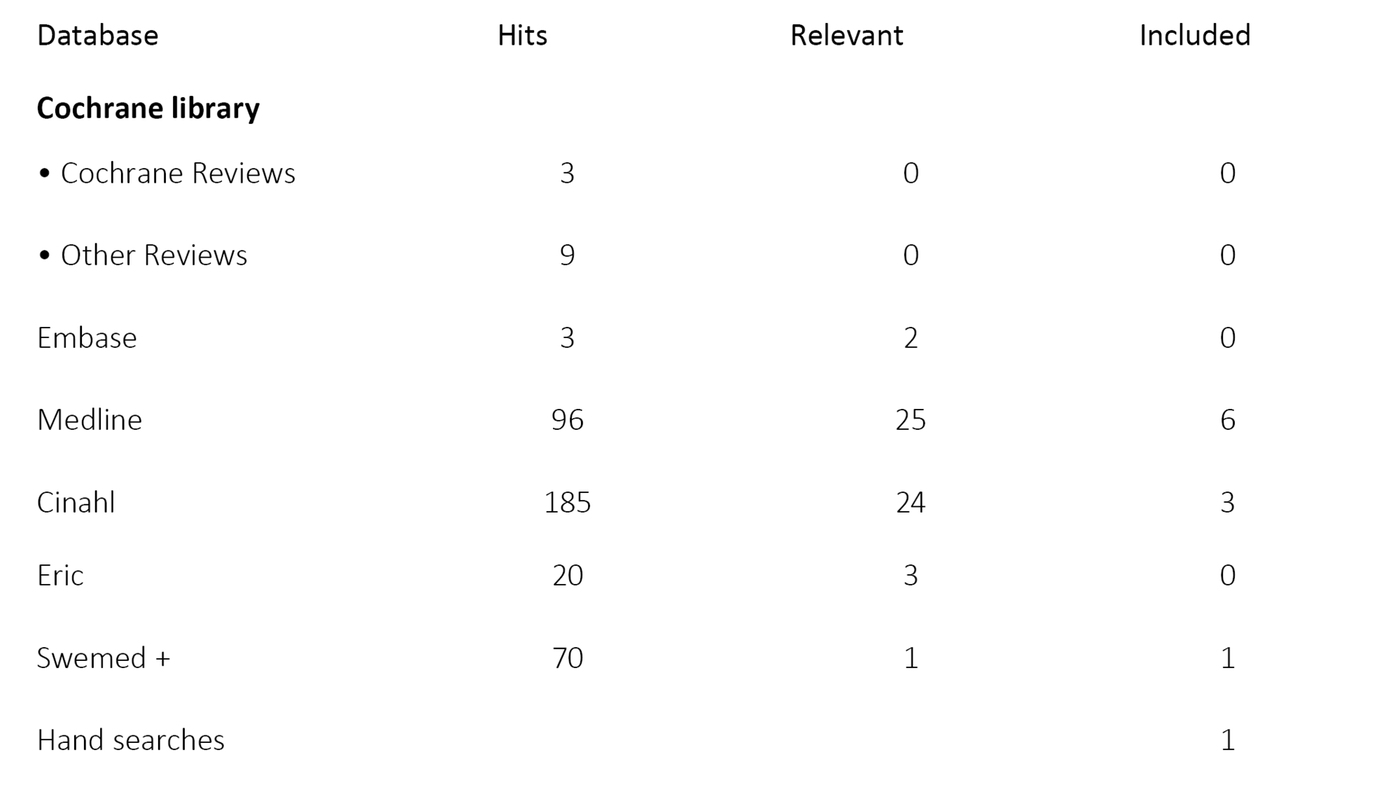
Method: Modified scoping review with systematic searches (Cochrane Library, Medline, Cinahl, Embase, Swemed+, and Eric) and manual searches. The search covered the period 2000–2014. All studies which addressed EBP in nursing education were considered. Two independent reviewers assessed the eligibility of each study.
Results: Eleven studies, with various research questions and designs and of varying quality, were retrieved. All articles described that learning activities in all stages of EBP had to be included in the curriculum. Eight studies had included EBP in clinical topics. Five studies examined students' learning by systematic introduction of EBP in the curriculum. The findings suggest that a systematic training in EBP with interactive learning strategies in collaboration with practice can have a positive impact on student learning.
Conclusion: Systematic training in EBP in cooperation with the practice field can have a positive impact on student learning. More international and Norwegian research with different study designs is necessary to increase the knowledge base.
Introduction
Patient safety and quality of care are prioritised areas within the health services (1,2), and decisions in clinical practice are expected to be based on up-to-date evidence (1). According to HelseOmsorg21, today’s nursing curricula only modestly respond to the challenges faced by the health services in this area (3).
Evidence-based practice (EBP) entails making professional decisions based on systematically retrieved research-based evidence, experience-based knowledge, and the patients’ wishes and needs in the given situation (4,5). In order to work evidence-based, nurses need competence in professional reflection, formulation of clinical questions, conducting searches, critical appraisal of research literature, as well as application and presentation of research (4).
International studies show that nurses in clinical practice lack basic EBP skills (6,7), and that many nurses in clinical practice have a negative attitude to applying research (8,9). A literature review from 2011 pointed out that measures against identified barriers, competence building, and professional development are important in promoting evidence-based practice (10).
Current health policies state that educational communities shall integrate evidence-based forms of practice in professional education curricula (3,11). Internationally the aim is to integrate EBP in the health professions’ curricula (5,12) and in the medical curricula (13,14). In spite of increased attention to EBP, we know little about its implementation in the nursing education curricula. A Norwegian study addressed the nursing students’ experiences with implementation of EBP in clinical practice studies. The results of this study suggest that cultural challenges may come between the students’ learning goals and the implementation of EBP in practice (9). A Swedish study (15) showed great differences in the way students from different universities in Sweden experienced the emphasis on EBP in the nursing curricula.
3630 new nurses graduated in Norway in 2014 (16). This is a large group and they will all have a central role in working evidence-based. The educational institutions have a great responsibility in this regard. Current health policies suggest mandatory training in handling evidence and evidence-based practice for all health profession curricula (3). To fulfil such health policy goals, the students must acquire sufficient EBP competence during the course of their education. The purpose of this literature review is thus to identify and describe research on EBP in nursing education.
Method
The literature review is a modified scoping review based on the Arksey and O’Malley framework (17). A scoping review is a suitable method for gaining an overview of a research field in which a variety of study designs are used. The scoping review, as opposed to the systematic literature study, opens for inclusion of various study designs (17). We chose scoping review as method due to the limited research field and our wish to include all relevant articles. To ensure good quality in the search process the search was planned and carried out in collaboration with a librarian. We searched the databases Cochrane Library, Medline, Cinahl, Embase, Swemed+ and Eric, for the period from January 1 2000 to December 15 2014. The searches were limited to peer reviewed publications in English or Scandinavian languages.
The following search terms were combined; evidence-based practice/(or evidence based or evidence-based or evidencebased or research based or research-based or researchbased or knowledge based, or knowledge-based or knowledgebased) and nursing/ (or evidence-based nursing/) and schools, health occupations/(or schools, nursing/ or universities/ or education, nursing/ or education, nursing, baccalaureate/ or education, nursing, graduate/ or nursing education research/) and curriculum/ (or faculty, nursing/ or learning). We performed a combination search with the same search terms adapted to the various databases. In Medline we added «facilitat*» and «implement*» to limit the search. Nordic journals are not automatically indexed in Cinhal and Medline, so we searched in Swemed+ with the search terms evidence based and nursing education. For the periods during which the journals were not available online, we did a hand-search; Norsk tidsskrift for sykepleieforskning (2000 - 2010), Sykepleien forskning (2006 - 2008) and Vård i Norden (2000 - 2004).
Inclusion criteria were quantitative and qualitative studies addressing organisation of education curricula and description of learning activities related to EBP in nursing education. Only studies on bachelor level nursing were included. Studies involving post-registration programmes, master’s degree programmes, and commentary articles were not included.
Results
Table 1 shows an overview of the number of articles identified, databases, and studies included. A two-step process was used for going through the articles and selecting those relevant to our study (18). Two of the authors read title and abstract of all 386 articles. Three hundred and thirty one articles were excluded in accordance with the inclusion and exclusion criteria. The second step in the process consisted of a thorough reading of the 55 remaining articles. Two authors read all 55 articles in full to select articles for inclusion based on the criteria. Disagreements between the authors were resolved by discussion.
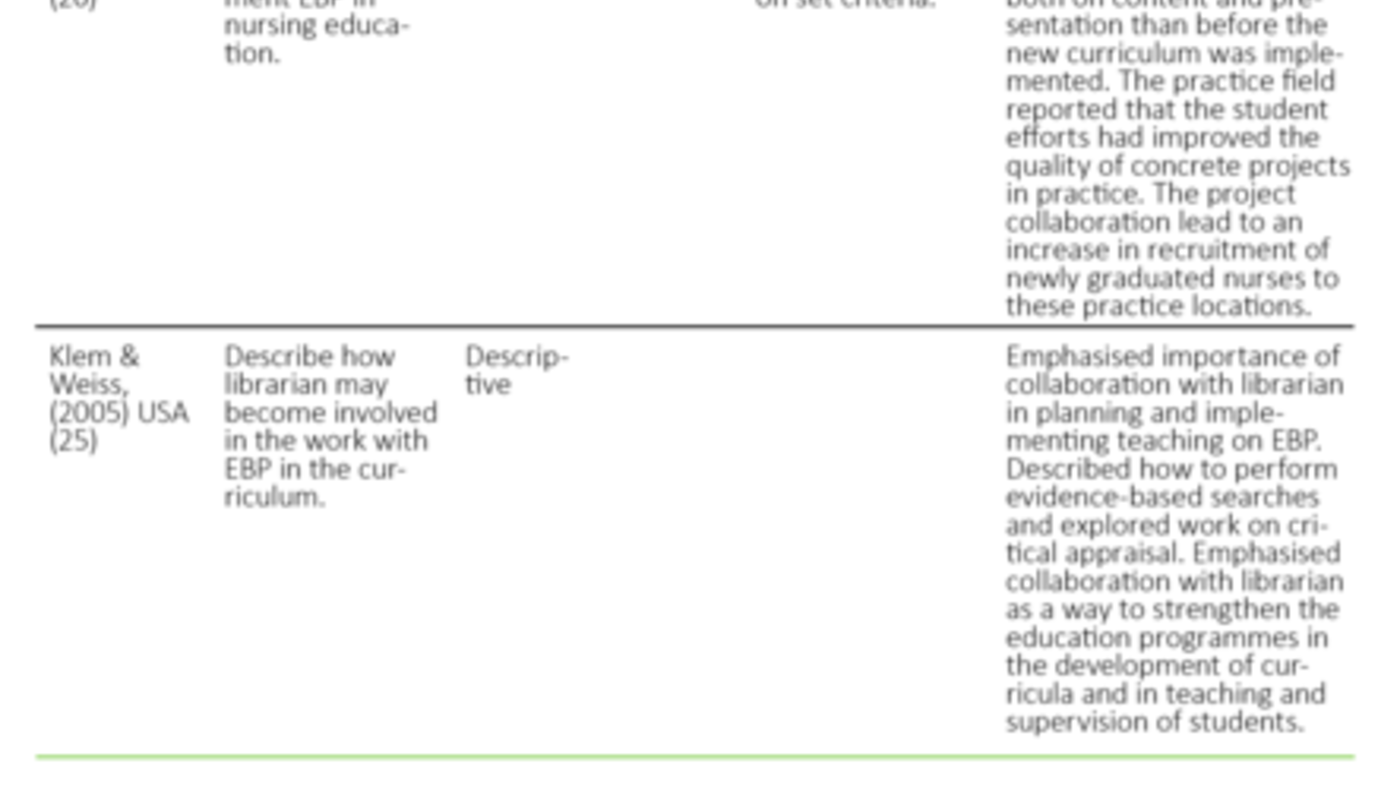
Eleven studies were included: nine from the USA, one from Italy, and one from China. The studies addressed different types of questions and were of varying quality. The research designs varied: one literature review (19), two quasi-experimental studies (20,21), one article with action research design (22), one cohort study (23), two descriptive studies (24,25), and four case studies (26-29). The case studies, the action research study, and one of the descriptive studies (25) dealt with organisation and learning activities related to EBP in education curricula and yielded insight into the positive effect these may have on individual students’ learning outcome. The quasi-experimental studies (20,21), one descriptive study (24), and the cohort study (21) show effect of EBP learning activities on groups of students. Table 2 shows an overview of the studies included.
Curriculum structure and content
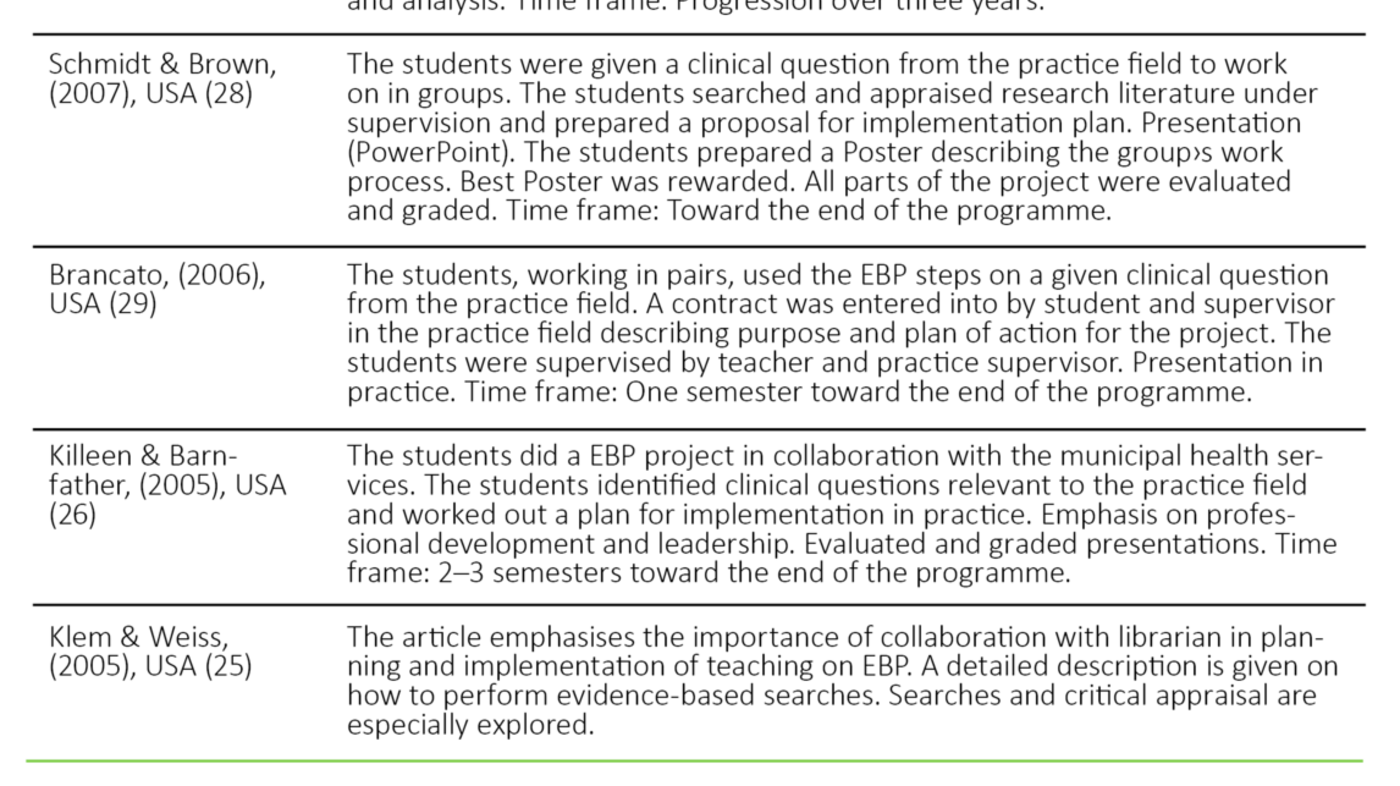
All articles stated that learning activities relating to all steps of EBP must be included in the curriculum. Table 3 shows an overview of the students’ learning activities in the studies included. Three studies (22,24,27) described curricula for all three years, while five studies (20,21,26,28,29) had concentrated on learning activities towards the end of the programme. In most articles EBP was included in clinical topics in the curriculum (20-24,26,27,29); three of these articles were related to the subject of leadership (20,26,27).
In collaboration with the practice field, Moch, & Cronje (22) developed a new study model with the EBP curriculum spanning all three years. The clinical practice context was central in both development and implementation of the model. Among the students’ assignments was work on research articles in knowledge groups, across educational levels, with teachers and employees in the practice field. The roles of the students changed from that of observers at the outset to leaders of the knowledge groups toward the end of the programme. Articles on subjects from the practice field were discussed and critically appraised in the knowledge groups. The students searched current research, summed up the evidence, and made plans for implementation.
Finotto and colleagues (24) reported significant improvement in the students’ EBP skills after implementation of EBP in the curriculum, with progression throughout all three years. The students further reported that the curriculum had given them increased insight into, and understanding of, research, through their work on the bachelor thesis in particular. In the first year of study the students worked theoretically with describing the purpose of EBP and how to proceed when working evidence-based. In the subsequent practice period the students worked on formulating clinical questions and using PICO. In the second year of study the students performed searches and critical appraisal, while during the third year emphasis was on search strategies in various databases and different study designs. Student-centred teaching methods with the students working in groups were also emphasised.
The thoroughness of the description of the learning activities varied in the studies included. Most studies combined lectures and/or e-learning with subsequent assignments (20-24,26-29). One study (20) examined the impact of an interactive EBP teaching programme during one semester towards the end of the programme. The intervention, also called E-FIT, consisted of a two-hour introduction to EBP with subsequent group assignments in practice. The group assignments included problem identification, literature synthesis, implementation strategy, and presentation. The results showed a significant effect on the students’ knowledge of EBP for the intervention group, but no difference between the groups with regard to attitudes and future use of EBP (20).
After introducing a two-part intervention, Zhang and colleagues (21) carried out a quasi-experimental study with participants from seven universities. In phase 1 the students worked individually with an e-learning course on EBP and performed a literature search (see table 3). The phase ended with a group study report where the students described how they understood EBP, the significance of EBP for nursing science, and a practical example where they applied the steps of EBP. In phase 2 the groups worked on critically appraising selected research articles. Each group was assigned an article for discussion related to the research question, the literature review, and a theoretical framework. The groups further reflected on and appraised methodical aspects of the article related to research design, selection, data collection method, and analysis. Three group meetings were held in which the students shared their appraisals. Students within the same group worked on the same article. Teacher and clinical practice supervisor supervised the groups and the students reached consensus on the article’s strengths and weaknesses. The study showed significant impact on the students’ knowledge of EBP, attitudes, and behaviour. Significant improvements were reported in analytical skills, problem solving, and ability to work independently and to collaborate with others. Phase 1 with self-study scored lower than phase 2, which was supervised by teacher and practice supervisor.
Group assignments
Eight articles (20-24,26-28) described the students working in groups; six of the eight articles described group sizes of four to six participants (20,23,26,28). One of the articles described groups put together across topics and levels (22).
Study assignments
The study assignments varied in number and size. Some were described extensively and in detail (20,23,24,26-29), and some had clear learning outcome descriptions (24,27). A common characteristic was that the study assignments included both theory and clinical practice topics (19-24,26,27,29), and in three of the studies the students worked on the same assignment over several semesters (20,23,26). Ross et al. had one study assignment for each of the EBP steps (27), while others described a study assignment that encompassed several steps (20,24,26,28).
Supervision
Several students emphasised the importance of supervision (21,23,24,26,27,29). In one study the same teacher supervised the students for two semesters; the study assignment lasted several semesters (26). Others emphasised the role of the teacher as central in both supervision and giving feedback on concrete study assignments (27-29). One study (24) reported that the students to a small degree were encouraged by the practice supervisors to work evidence-based.
Presentations and evaluations
In the majority of the studies the students gave presentations involving Poster or PowerPoint in the practice field (19-21,23,26-29). One study used a blueprint for the presentation to ensure that all steps in the process were followed (26), and in four studies the works were graded (22,23,26,28). Two articles reported rewarding the best wards (22,28). The students assessed such rewards as fun and said this contributed to healthy competition between groups (28).
Collaboration between education and practice field
In the majority of the included articles collaboration between practice field and education was emphasised (19-24,26-29). In five studies the importance of both parties participating in the planning phase was particularly in focus (21,23,26,28,29). That a teacher supervised concrete improvement projects in the practice field was described as positive (22,23,26,28). Based on a review of the literature, Moch and colleagues (19) suggested that project collaboration on EBP between the practice field and education could contribute to increase competence for both students and employees in the practice field. Such collaboration could, according to several of the articles, become a win-win situation for both education and practice field (19,24,26), and thus contribute to improvement of quality in practice (19).
A common trait was that the students worked on study assignments that were based on clinical questions from the practice field (19-24,26-29). In five articles the clinical practice field had prepared topics for the students to work on during the practice period (21,22,26,28,29). Killeen and Barnfather (26) stressed the importance of supervision of the students in the work of identifying a clinically relevant question for the practice field. This question became the point of departure for improvement projects in which the students applied the EBP steps under supervision. In another study (29) the students worked together in pairs on formulating questions in collaboration with clinical practice supervisors. Formulating the question was described as the most challenging step in working evidence-based (24,26).
Who would supervise the students in EBP varied in the articles included. Some reported that the students were regularly supervised by clinical practice supervisor (22,28,29), while others described the supervision process as collaboration between clinical practice supervisor and teacher (21,23,27). One article reported that the competence requirement for practice supervisors was a master’s degree and completion of a course in EBP (29). In several studies employees in the practice field stated that they had benefited from the students’ work (22,23,26,28,29). Although the practice field viewed the work as useful, employees stated that they did not have sufficient time to go in-depth on the suggested changes (28). Moch and Cronje suggested that the new curriculum in which the students, among other things, taught EBP and lead knowledge groups in practice could help reduce the barriers to EBP (22).
Discussion
Even if EBP has received considerable attention both in the health services and in the professional curricula, this literature review shows that the subject has to a lesser extent been explored in research. Despite significant differences in quality, design, and method, the studies suggest that there are some issues that should be emphasised when introducing EBP into nursing curricula.
The studies suggest that a systematic emphasis on EBP throughout the nursing education has a positive influence on the students’ learning outcome. When all steps of EBP are systematically included in the curriculum, the students’ insight, attitudes, and skills in EBP improve. Progression in learning activities over several topics seems to be of importance. One explanation may be that EBP demands a separate set of skills that the students need time to acquire. If a three year progression is not planned, the literature review suggests that the EBP training should take place toward the end of the programme. This may be related to the students being more socialised in their own learning process and having achieved increased understanding of nursing issues at that point.
The studies characteristically report the use of a combination of several teaching methods. Fairly comprehensive EBP study assignments and a process-oriented approach with work in groups are recommended. Using e-learning in combination with study assignments appear to give the students a fundamental understanding of EBP. The Norwegian Knowledge Centre for the Health Services has a free e-learning course on EBP (30) that may be used in the curriculum. The studies acknowledge that teaching the students the steps of EBP before they start clinical practice may help increase the competence of both students and of employees in the practice field.
The literature review suggests that the students need much practice to achieve sufficient skills in the EBP steps. This is in accordance with findings from studies on the medical curricula (31,32). Reflection and critical assessment skills are important for all professionals and essential to evidence-based professional practice. In the studies included these issues are explored in depth.
Many of the articles stress the importance of practice in formulating clinical questions and this seems to be significant. A common situation is that clinical questions are formulated based on the student’s practice experiences or on request from the practice field. Finotto and colleagues point out that this may be one of the most difficult phases in the EBP process as it involves both critical thinking and the use of PICO (24).
Several of the studies point out that the practice field is a good arena for student learning. The three-way collaboration between teacher, student, and nurses, where EBP is applied to concrete clinical problems, seems to have a positive effect on student learning. Such establishment of good connections between the students’ learning activities in the university college and in the practice field is regarded as an important issue for the professional educations (33,34). Introducing EBP work methods is about associating evidence from research, clinicians’ experience, and user knowledge (4). The findings from this literature review emphasise that a feeling of community between the education and practice fields is essential and must be built over time. Through working with concrete practice projects the students learn the value of critical reflection on practice, and they gain insight into the significance of research for professional practice. The collaboration between practice supervisors and students in the planning of search strategies and critical appraisal of research literature appears to help increase both parties’ competence. The student presentations in the form of posters or presentations in the practice field receive good feedback and are experienced as positive.
The literature review suggests that the collaboration resulting from the implementation of EBP as method in practice studies may have a positive effect on quality improvement work in practice. Supervision by teacher in clinical practice projects appears to help stimulate the professional commitment in the practice field. The studies emphasise that the concrete results from the collaborative projects are useful to the employees in the practice field and that the results can be used to improve practice.
The literature review shows that EBP can help increase the students’ understanding of research. Teaching and training bachelor level students to read and critically appraise research during their education is considered positive (35,36). In Norway the research communities are encouraged to plan the curricula so that the students gain experience in applying research during their studies (37). The systematics of the EBP steps may be a good aid. It is further suggested that involving a health profession librarian in both the development of the curriculum and in the teaching may improve the students’ skills in the field.
This literature review documents a need for both Norwegian and international research on the systematic use of EBP as a method in the supervision of nursing students. The evidence base on this subject is limited. We need more knowledge on how curricula implement EBP teaching, what factors enhance and hinder student learning, as well as larger controlled studies to investigate the effect of structured and directed nursing education curricula. Existing research stresses the importance of mandatory collaboration between education and practice field. Teaching methods that start from clinical questions where the students, through student-centred methods in groups, acquire knowledge and skills in all steps of EBP are recommended. Teaching activities that address both practice and theoretical topics are also recommended.
Limitations
The studies included are small with significant differences in quality, design, and method. A possible weakness of this literature review is that we did not use the search terms “Evidence-informed practice”, “evidence-informed decisionmaking” and “evidence-based health care” and that we limited the searches in Medline with “facilitate*” and “implement*”. We may have missed some studies this way.
Conclusion
Norwegian and international research on nursing education curricula that include EBP is limited. Available research literature suggests that systematic training in EBP with interactive teaching strategies in collaboration with clinical practice may have a positive impact on student learning outcome. More research, with a variety of designs, is needed to explore various questions and increase the evidence base.
References
1. Stortingsmelding 10 (2012–2013). God kvalitet – trygge
tjenester. Helse og omsorgsdepartementet. Oslo 2012.
2. Meld. St. 11 (2014–2015). Kvalitet og pasientsikkerhet 2013.
Helse- og omsorgsdepartementet. Oslo 2014.
3. Helse og omsorgsdepartementet. HelseOmsorg21. Et
kunnskapssystem for bedre folkehelse. Regjeringen.no 2014.
4. Nortvedt M, Jamtvedt G, Nordheim LV, Reiner LM. Jobb
kunnskapsbaseret! 2. utgave ed. Oslo: Akribe; 2012.
5. Dawes M, Summerskill W, Glasziou P, Cartabellotta A, Martin
J, Hopayian K, et al. Sicily statement on evidence-based practice.
BMC Med Educ. 2005;5(1):1.
6. Melnyk BM, Fineout-Overholt E. Evidence-based practice in
nursing & healthcare: A guide to best practice: Lippincott
Williams & Wilkins; 2011.
7. Pravikoff DS, Tanner AB, Pierce ST. Readiness of US Nurses
for Evidence-Based Practice: Many don’t understand or value
research and have had little or no training to help them find
evidence on which to base their practice. AJN The American Journal
of Nursing. 2005;105(9):40–51.
8. Ciliska D. Educating for Evidence-Based Practice. Journal of
Professional Nursing. 2005;21(6):345–50.
9. Smith-Strøm H, Oterhals K, Rustad EC, Larsen T. Culture
crash regarding nursing students´ experience of implementation of
EBP in clinical practice. 2012.
10. Sandvik G, Stokke K, Nortvedt M. Hvilke strategier er
effektive ved implementering av kunnskapsbasert praksis i sykehus.
Sykepleien Forskning. 2011;6(2):160-7.
11. Meld. St. 13 (2012–2013). Utdanning for velferd. Samspill i
praksis.: Kunnskapsdepartementet, editor. 2012.
12. Young T, Rohwer A, Volmink J, Clarke M. What are the
effects of teaching evidence-based health care (EBHC)? Overview of
systematic reviews. PloS one. 2014;9(1).
13. Glasziou P, Burls A, Gilbert R. Evidence based medicine and
the medical curriculum. Bmj. 2008;337.
14. Maggio LA, Tannery NH, Chen HC, ten Cate O, O’Brien B.
Evidence-based medicine training in undergraduate medical
education: a review and critique of the literature published
2006–2011. Academic Medicine. 2013;88(7):1022-8.
15. Florin J, Ehrenberg A, Wallin L, Gustavsson P. Educational
support for research utilization and capability beliefs regarding
evidence-based practice skills: a national survey of senior nursing
students. Journal Of Advanced Nursing. 2012;68(4):888–97.
16. Database for statistikk om høgre utdanning NSD.
Publikasjoner 2015.
17. Arksey H, O›Malley L. Scoping studies: towards a
methodological framework. International journal of social research
methodology. 2005;8(1):19–32.
18. French B. Contextual factors influencing research use in
nursing. Worldviews on Evidence-Based Nursing. 2005;2(4):172–83.
19. Moch SD, Cronje RJ, Branson J. Part 1. Undergraduate
nursing evidence-based practice education: envisioning the role of
students. Journal of Professional Nursing. 2010;26(1):5–13.
20. Kim SC, Brown CE, Fields W, Stichler JF. Evidence-based
practice-focused interactive teaching strategy: a controlled study.
Journal of advanced nursing. 2009;65(6):1218–27.
21. Zhang Q, Zeng T, Chen Y, Li X. Assisting undergraduate
nursing students to learn evidence-based practice through
self-directed learning and workshop strategies during clinical
practicum. Nurse education today. 2012;32(5):570–5.
22. Moch SD, Cronje RJ. Part II. Empowering grassroots
evidence-based practice: a curricular model to foster undergraduate
student-enabled practice change. Journal of Professional Nursing.
2010;26(1):14–22.
23. Kruszewski A, Brough E, Killeen MB. Collaborative
strategies for teaching evidence-based practice in accelerated
second-degree programs. The Journal of nursing education.
2009;48(6):340–2.
24. Finotto S, Carpanoni M, Turroni EC, Camellini R, Mecugni D.
Teaching evidence-based practice: developing a curriculum model to
foster evidence-based practice in undergraduate student nurses.
Nurse education in practice. 2013;13(5):459–65.
25. Klem ML, Weiss PM. Evidence-based resources and the role of
librarians in developing evidence-based practice curricula. Journal
of professional Nursing. 2005;21(6):380–7.
26. Killeen MB, Barnfather JS. A Successful Teaching Strategy
for Applying Evidence-based Practice. Nurse Educator.
2005;30(3):127–32.
27. Ross AM, Noone J, Luce LL, Sideras SA. Spiraling
evidence-based practice and outcomes management concepts in an
undergraduate curriculum: a systematic approach. The Journal of
nursing education. 2009;48(6):319–26.
28. Schmidt NA, Brown JM. Use of the innovation–decision
process teaching strategy to promote evidence-based practice.
Journal of Professional Nursing. 2007;23(3):150–6.
29. Brancato VC. An innovative clinical practicum to teach
evidence-based practice. Nurse Educator. 2006;31(5):195–9.
30. Nasjonalt kunnskapssenter for helsetjenesten. 2015.
31. Johnston JM, Schooling CM, Leung GM. A
randomised-controlled trial of two educational modes for
undergraduate evidence-based medicine learning in Asia. BMC Medical
Education. 2009;9:63.
32. Bradley P, Oterholt C, Herrin J, Nordheim L, Bjørndal A.
Comparison of directed and self-directed learning in evidence-based
medicine: a randomised controlled trial. Medical Education.
2005;39(10):1027–35.
33. Benner P, Heggen K, Thorbjørnsen KM, Kjerland L. Å utdanne
sykepleiere: behov for radikale endringer. [Oslo]: Akribe; 2010.
277 pp.
34. Molander A, Terum LI, editors. Profesjonsstudier. Oslo:
Universitetsforlaget; 2008.
35. Boyer E. The Boyer commission on educating undergraduates
in the research university, reinventing undergraduate education: A
blueprint for America’s research universities. Stony Brook, NY.
1998.
36. Healey M, Jenkins A. Developing undergraduate research and
inquiry: Higher Education Academy York; 2009.
37. Universitets- og høyskolerådet. Utdanning+FoU=Sant.
2010.









Comments