Experiences with mobile intensive care nurses (MICNs)
Mobile intensive care nurses are called out to hospital wards when a patient’s condition is showing signs of deterioration. When are they called out, and what measures do they initiate?
Background: Mobile intensive care nurses (MICNs) have been established at Oslo University Hospital, Ullevål, but there is little knowledge about how these resources are used or what their work entails.
Objective: To map the number of requests for MICNs during a six-month period, and to assess the reasons for the requests, measures initiated by MICNs and the number of admissions to an intensive care unit.
Method: We recorded the requests for MICNs over the period June–December 2015. The MICNs recorded socio-demographic and clinical variables on a registration form for each call-out. When the data on the registration form were inadequate, we retrieved information from DIPS, the electronic patient record system.
Results: The MICNs received a total of 163 requests during the registration period. Of these, 91 were either for advice to ward nurses or assistance in dealing with various nursing procedures (group 1), while 72 were mainly associated with respiratory (56.9 per cent) and circulatory (18.1 per cent) deterioration in a patient (group 2). The most common measures taken in group 2 were the following: supplying O2, intravenous fluid, medication, correct positioning for bedrest and consulting with an MICN. Of the patients in group 2, 22.1 per cent were transferred to an intensive care unit for treatment.
Conclusion: In most cases, MICNs were called out due to deterioration in a patient as a result of respiratory distress. Future studies should map whether MICNs can prevent admissions to intensive care.
Several countries use dedicated teams that are called out to hospital wards when a patient’s condition shows signs of deterioration. The most common names of such teams are Medical Emergency Team (MET), Rapid Response Team (RRT), Rapid Response System (RRS) and Critical Care Outreach (CCO) (1–4). Internationally, the function and composition of such teams vary somewhat, but normally consist of a doctor and a nurse, known as a mobile intensive care nurse (MICN) or a mobile intensive care group (MICG) (5, 6).
Although some hospitals in Norway and Sweden have introduced such teams either as a project in individual wards or as an additional resource, little is known about the scope of these arrangements. The purpose is to identify high-risk patients in hospitals at an early stage in order to prevent deterioration in their condition and potentially improve their outcome. (7). Two previous meta-analyses concluded that the introduction of such teams is associated with a reduction in cardiac arrest rates, and some studies have found a decrease in mortality (8, 9).
MICNs established at OUH
MICNs were established at the Division of Medicine, Oslo University Hospital (OUH), Ullevål, in the summer of 2015. The hospital also has a resuscitation team that can be called out to any ward in the event of cardiopulmonary arrest.
The Division of Medicine at Ullevål consists of ten wards, with a capacity of 193 beds. The wards cover the following specialities: infectious diseases, geriatrics, heart disease, lung disease, stroke treatment, kidney disease, gastromedicine and general internal medicine. There is also a ward that is used as an observation unit specifically for the treatment and observation of poisoning.
If a nurse observes signs of deterioration in the condition of a patient in one of these wards, or if the nurse needs advice and/or guidance on specific nursing procedures, they can call an MICN. A dedicated mobile number is in use for this purpose. The MICN post is staffed between 15:00 and 08:00 on weekdays, and around the clock at weekends.
Although patients are moved to observation units or intensive care units prior to the manifestation of respiratory or cardiac arrest, ward patients whose condition is showing signs of deterioration have initially been taken care of by ward nurses and the duty doctor.
However, experience has shown that doctors are not always available when they are called out, because they may, for example, be attending to new and critically ill patients in the accident and emergency department. Time conflicts sometimes occur. The purpose of establishing the MICNs was to provide an extra resource that could relieve the doctor, provide professional guidance to ward nurses, participate actively in assessing the health status of patients and initiate adequate measures. MICNs have extensive experience in dealing with complex medical patients.
The aim of the study
Some studies have shown that deterioration in the condition of hospital patients is mainly caused by hypotension or respiratory failure (10, 11). The studies also show that a number of measures are initiated to stabilise such patients, such as intravenous fluids and medicinal treatment (1, 11). In a number of European countries and countries such as the USA and Australia, it is the METs and RRTs that handle such patients. When nurses identify symptoms of deterioration at an early stage, such as sepsis symptoms, earlier studies have shown an increase in the 30-day survival rate (12). A previous study by OUH, Rikshospitalet found that the nurses were satisfied with the MICN service, but did not provide reasons for use or descriptions of measures taken by the MICNs (5).
The aim of this study was therefore to map the number of requests for MICNs within a six-month period. We also wanted to assess the reasons for such requests, the measures initiated by MICNs and the number of admissions to an intensive care unit.
Method
Design, sample and setting
In this observation study, which has a descriptive design, we included all patients aged ≥18 who had been admitted to wards in the Division of Medicine at OUH, Ullevål during the period 1 July to 31 December 2015. For practical reasons, the inclusion period was limited to six months, as the first author wanted to use the data in his master’s thesis.
Two groups: consultations and interventions
Based on different levels of use of MICNs, we classified patients during the inclusion period in two different groups: 1) consultations and 2) interventions. Patients in group 1 represent cases where ward nurses call on an MICN for professional advice or assistance, and professional guidance on specific nursing procedures. Group 2 is made up of patients whose condition deteriorated, as identified using the National Early Warning Score (NEWS).
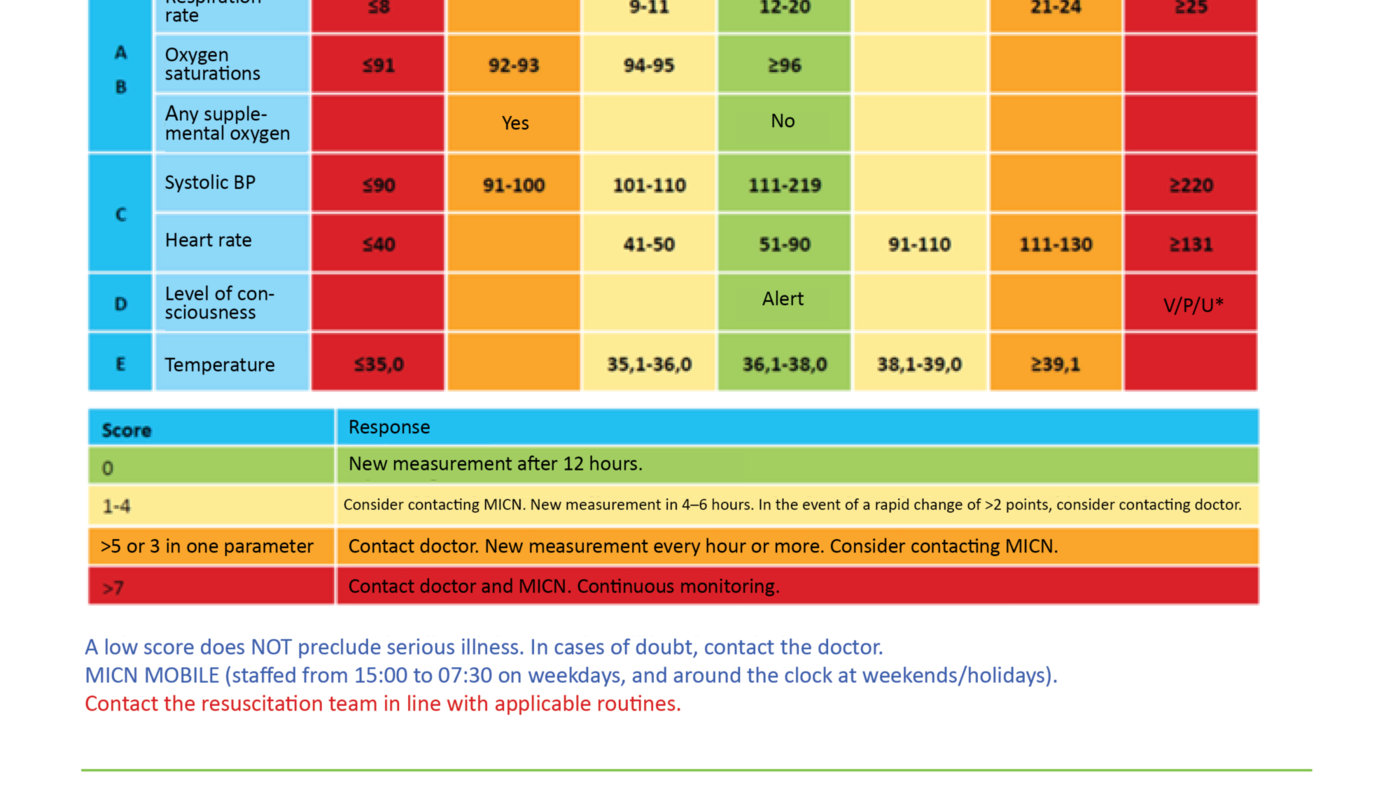
The nurses used NEWS to score the patient based on their vital signs, such as respiratory rate, blood pressure, heart rate and temperature. In addition, a score was given for whether or not the patient received O2 and for the level of oxygen in the blood. Consciousness was also given a score. All values outside the normal window will trigger a score (table 1). In group 2, we recorded which interventions the MICNs performed on patients in this group, and how many patients had to be transferred to an intensive care unit.
Data collection
A registration form developed by the Division of Medicine for use with MICN call-outs was used to retrieve all of the relevant data (Appendix 1). Socio-demographic variables included the patient’s gender and age. Clinical data included the reason for call-out, NEWS score, which nursing procedures and other measures were performed on the patient, and whether the patient was admitted to an intensive care unit. In addition, we collected data on the patient’s status in relation to cardiopulmonary resuscitation and what time of day the MICN was called out.
We also collected information about the call-out time, described as the time from when the MICN was contacted to when they were in the physical presence of the patient. Where the data in the registration form were incomplete, we used the electronic patient record system DIPS to fill the gaps. In cases where the NEWS score was not calculated in the form, the project manager entered this based on other data given in the form.
Analysis
In order to describe the population, we used descriptive analyses, frequency analyses and exploratory analyses. We used normally distributed data curves to control whether collected data were normal or skewed. Abnormally distributed data were examined with non-parametric tests such as the chi-square test, Spearman’s correlation coefficient (rho) and the Mann-Whitney U test. Continuous data that were not normally distributed were expressed as the median and interquartile range (IQR). Statistical significance was set to p values below 0.05. We analysed the data using the Statistical Package for the Social Sciences (SPSS), version 22.0.
Ethics
This study was submitted to and approved by the Data Protection Official at OUH as a quality assurance study. Clinical management at the Division of Medicine, OUH also approved the study and the use of registered data. All collected data was de-identified.
Results
During the six-month study period, the MICNs were contacted a total of 163 times. There were no statistically significant disparities between the two groups (figure 1).
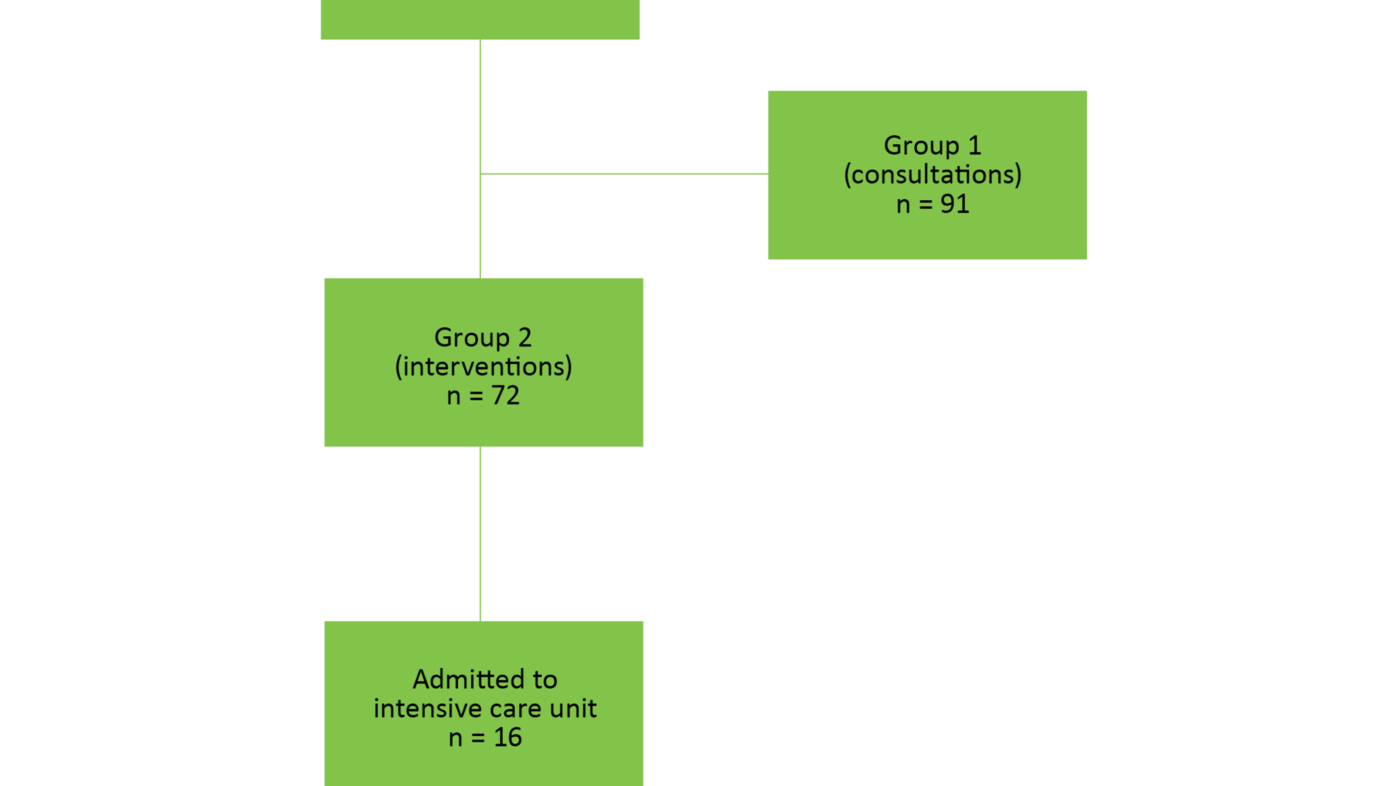
Of the 163 call-outs by MICNs, there were 91 cases (group 1) where an MICN provided guidance to a ward nurse on nursing procedures, or gave other advice. In this group, information about age and gender was available for 59 patients. In the group (group 2) where MICNs physically attended to a patient in a ward due to a clinical change in the patient and a change in the NEWS score, a total of 72 patients were registered.
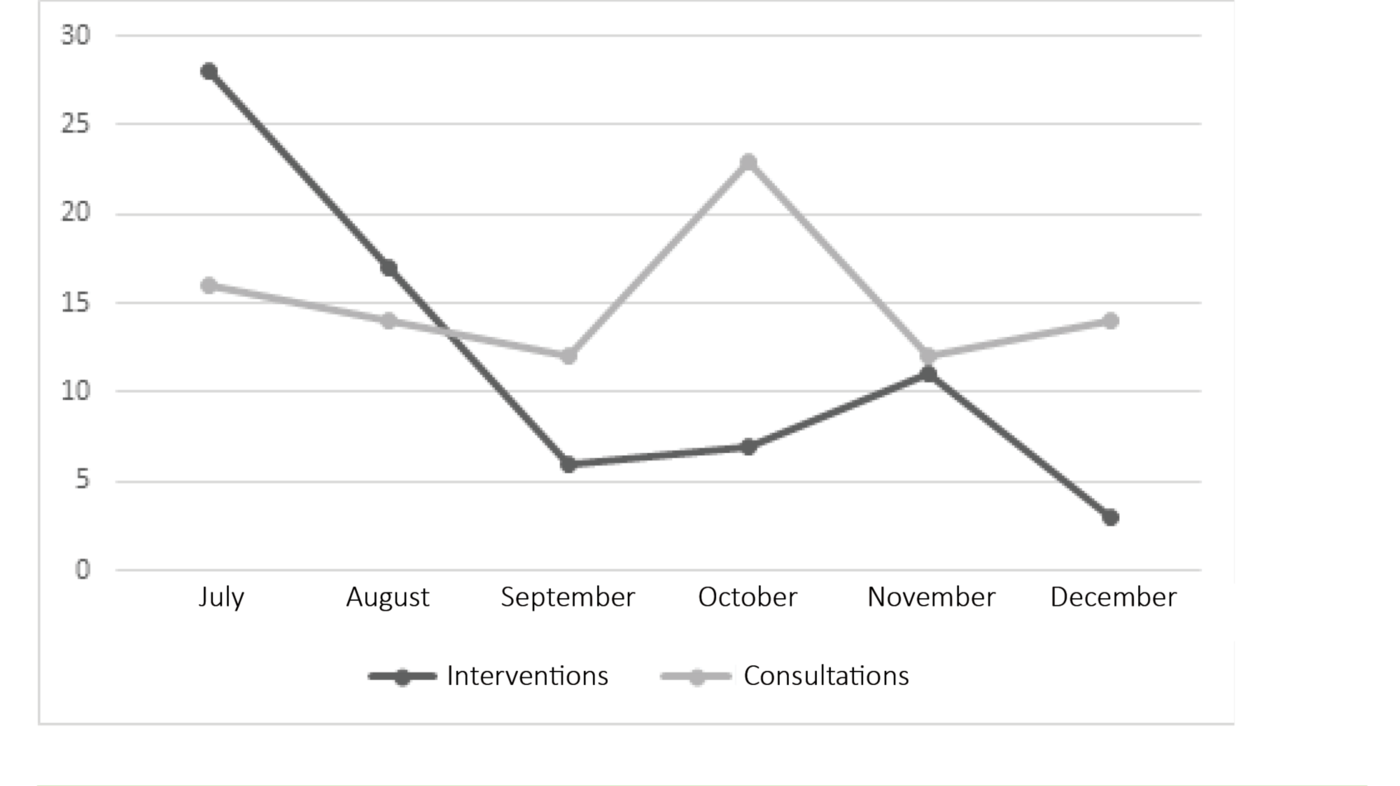
Figure 2 shows the number of call-outs broken down per month during the study period for both group 1 (consultations) and group 2 (interventions). Table 2 shows a complete overview of age and gender within the groups and between the groups.
Reasons for contact
In the registration form, the reason for calling out an MICN was either specified as a diagnosis (such as pneumonia, sepsis or hypotension), or as free text describing the problem. We redefined these reasons according to actual patient problems as well as clinical findings noted on the form, and identified the following reasons for contact:
- respiration (including: dyspnoea, hypoxaemia, rapid respiratory rate, secretion stagnation)
- circulation (including: hypotension and/or fast heart rate. Such conditions are revealed in isolation using NEWS (table 1)).
- infection
- neurology
- other
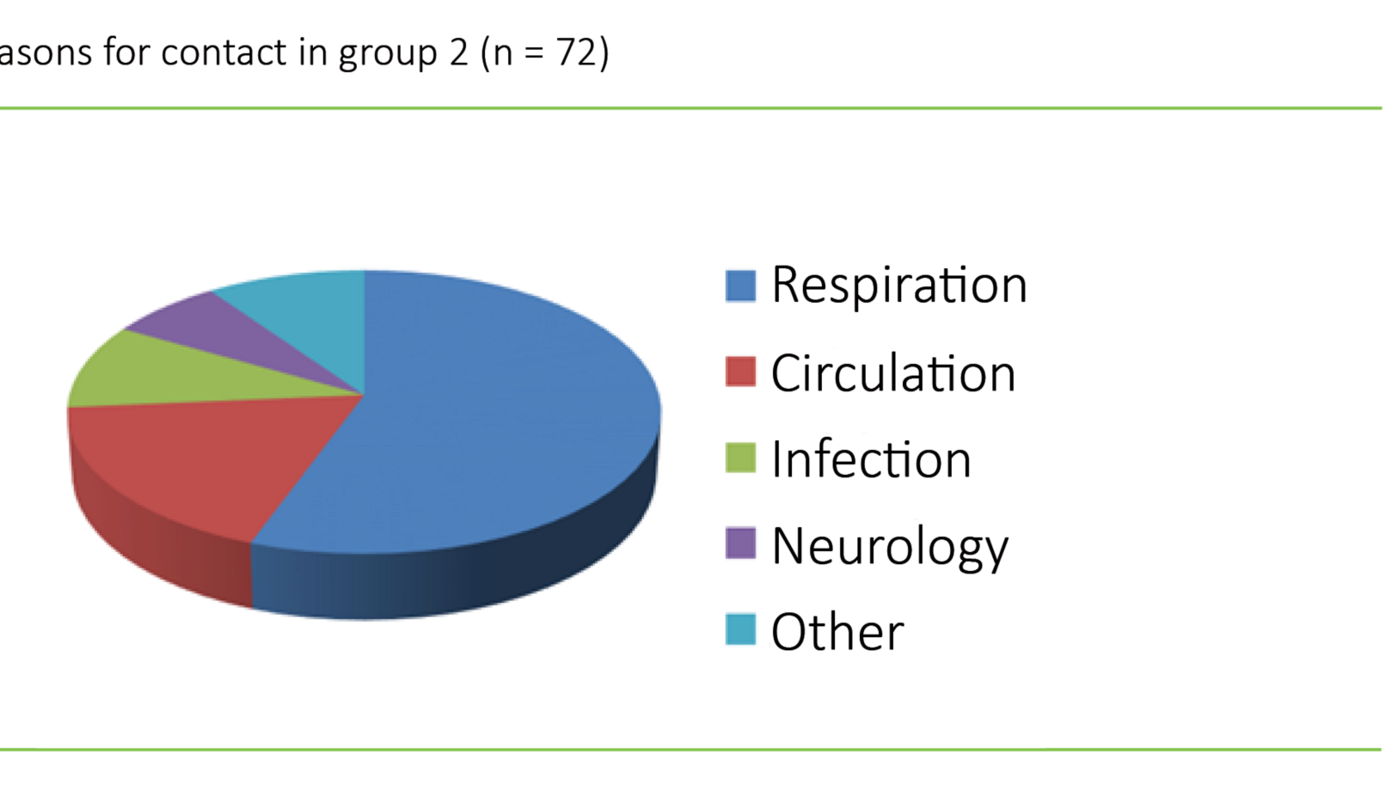
Where an MICN was called out to a patient with hypoxaemia and a rapid respiratory rate, which in turn triggered a high NEWS score, the reason for contact was registered as respiratory. Some patients had few deviations in their NEWS scores. These patients could, however, have isolated scores on ‘consciousness’, where the reason for contact was classified as neurological. Other conditions noted on the form, such as hyperglycaemia, anaphylaxis, hypothermia and urinary retention, only occurred rarely. We collated these conditions into the group ‘other’. More than half of the MICN call-outs were due to respiratory problems (n = 41; 56.9 per cent) followed by circulatory problems (n = 13; 18.1 per cent). Figure 3 shows the distribution for other categories.
National Early Warning Score
Of the 72 call-outs in group 2, five patients did not have a NEWS score. In the data that were available for 67 patients, the NEWS scores ranged from 1–18 with a median of 8 (IQR 4). Of the patients with available NEWS data, 15 were admitted to an intensive care unit with a median NEWS score of 10 (IQR 3). Table 1 shows which parameters are included in the assessment of the patient, and the NEWS score threshold that triggers the need to call out an MICN and further follow-up.
Measures initiated by MICNs
In group 1, MICNs assisted with certain nursing procedures, such as the insertion of a peripheral intravenous cannula or dealing with a blocked intrapleural drain. Blocked intrapleural drains were dealt with either by performing the procedure directly or by guiding the ward nurse. Other types of tasks related to advising ward nurses on medication and its administration (e.g. Atrovent/Ventoline, Furix and Seloken), and providing general advice.
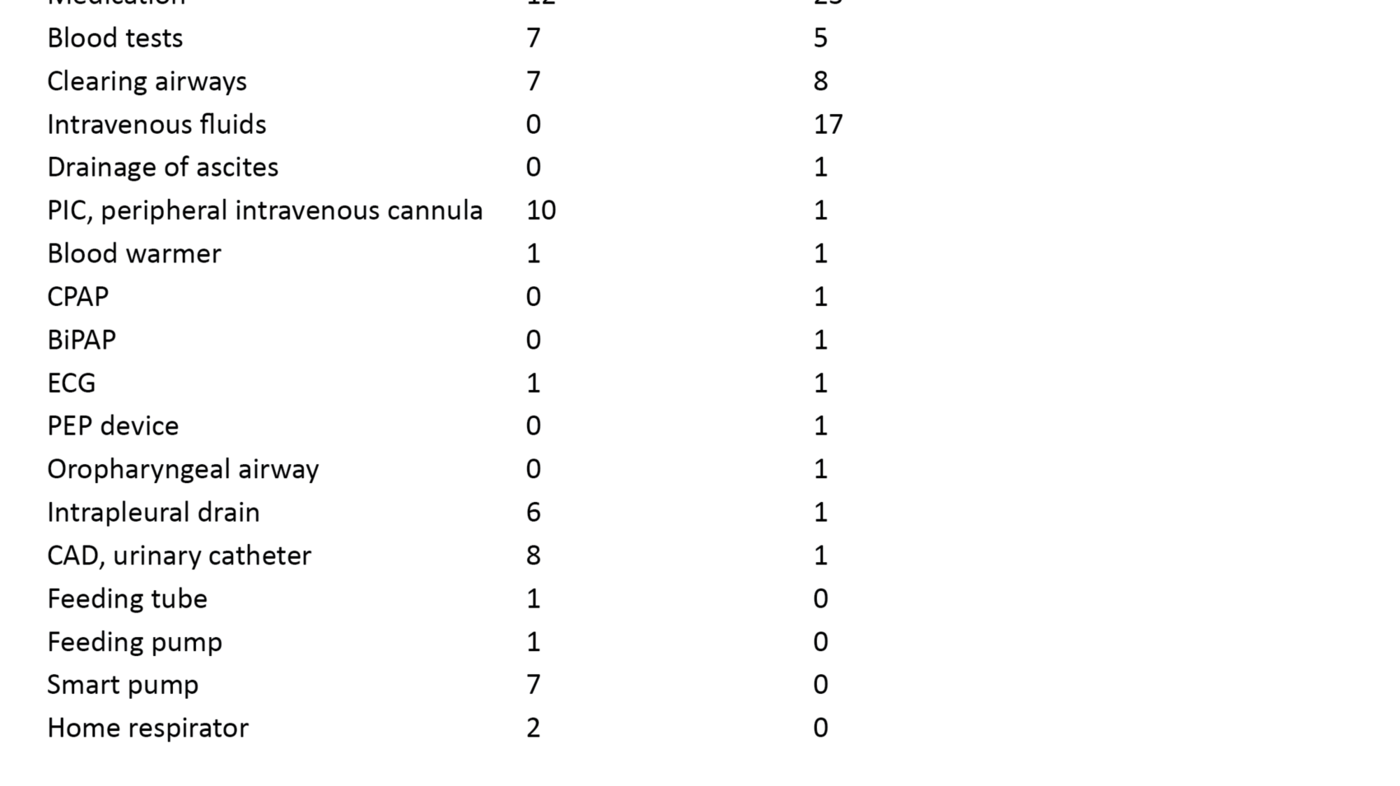
In group 2, MICNs assisted with specific measures related to the stabilisation and treatment of patients. The most common measure was administering O2, but advice was often recorded on the form, for example, when an MICN advised a ward nurse on further follow-up and what observations the nurse should continue. Table 3 shows a complete overview of measures.
Number of admissions to intensive care units
Of the 72 patients in group 2 who received interventions from an MICN, 22.1 per cent (n = 16) were transferred to a higher treatment level in an intensive care unit. Of these, 12 were admitted due to respiratory problems. Two had circulatory problems, and two belonged to the neurology group. Of those who were admitted to an intensive care unit, half (n = 8) had been given a status for cardiopulmonary resuscitation. Five of these patients had the status ‘do not resuscitate’.
Time of day and time spent on call-out
In 153 of a total of 163 call-outs, the time of day that the MICN was contacted was registered. In total, for groups 1 and 2, 92 (60.1 per cent) of the call-outs took place between 15:00 and 22:00, and 61 (39.9 per cent) between 22:00 and 08:00. In group 2, the time spent by the MICN from the first contact up to the point of meeting the patient was registered in 65 cases. This time ranged from 1 to 20 minutes, with a median of 5 (IQR 2).
Discussion
The intention of this study was to map the use of MICNs over a period of six months. Respiratory and circulatory deterioration were the main triggers of MICN call-outs. In order to detect deterioration in a patient’s condition, NEWS scores were used, and a number of measures were initiated with a view to stabilising the patient. Few patients were transferred to a higher level of treatment at an intensive care unit.
MICNs were frequently called out in the start-up period July–August in group 2, but the number of call-outs for this group tended to decline during the period of the study (figure 2). Some previous studies have also observed a decline in the use of such teams after the initial start-up period. Calzavacca et al. (13) concluded that implementation of such teams is a process that takes several years to complete. In this study, we have not mapped the process prior to the implementation of the MICNs, but it is known that MICNs actively contacted all wards during the start-up period. This may have helped to bring the service to the attention of nurses, and served as a reminder of its existence.
In group 1, the use of MICNs was evenly spread throughout the study period, but with a spike in October. One potential explanation for this may be that the patient base was higher than in other months, that patients had more complex issues, or that they were generally more unstable. However, we have not obtained internal reports on the number of patient beds filled, which could provide valuable information in this context.
Reasons for MICN call-outs
Deterioration in cardiopulmonary status was by far the dominant reason for calling out an MICN. A number of studies from other countries have reported that METs or RRTs are called out due to cardiopulmonary issues (10, 11, 14). Silva et al. (1) demonstrated that METs were mainly contacted due to respiratory problems, which corresponds to the findings in our study. In an MET call-out, both a doctor and a nurse attend to the patient (1, 3, 15). The inclusion of a doctor in the team means that more advanced treatment can be given to the patient on the spot. This composition of professionals can therefore strengthen the team (15-17).
Maharaj et al. (9) concluded in a meta-analysis, however, that the presence of a doctor was not significantly associated with a reduction in mortality. In our study, MICNs were called out to unstable patients. Patients with serious and life-threatening conditions would have been dealt with by the resuscitation team. Silva et al. (1) found that staff concerns about a patient (‘staff worried’) was the second most common criterion for activating an MET. This may be due to the fact that the criteria for calling out an MET are stricter (18) than in our study. Bellomo et al. (19) recommended that the ‘staff worried’ criterion be used for patients who did not fit the other criteria for MET call-outs.
Silva et al. (1) identified a need for greater competence among the staff in assessing vital signs and awareness that calling out an MET should be based on actual clinical findings. ‘Staff worried’ is a broad term that does not identify the actual problem. However, this should not be excluded as a criterion for MICN call-outs as studies have shown that the threshold for calling out such teams is sometimes set too high. Where this is the case, the use of MICNs may be reduced or delay call-outs (19-21), which in turn can lead to increased mortality (22).
Jackson et al. (23) asked nurses if they would call out an RRT if they were concerned about a patient even though their vital signs were normal. A total of 29.2 per cent of those asked said they would feel uncertain about what to do. The point is that the MICNs should represent a low-threshold service where only an intensive care nurse is called out, not a whole team. In our study, ‘staff worried’ was not a criterion on the registration form, and we therefore do not know whether this criterion would have been in frequent use at OUH, Ullevål.
More frequent use of MICNs in the summer
After the MICN service was started, an overarching NEWS procedure was established at OUH, which was to be implemented in all medical divisions. The Division of Medicine implemented the procedure upon start-up of the MICNs, while all nurses received training in the assessment and treatment of patients. Improving nursing knowledge about patients and practical skills in assessing and treating patients during the training period was likely to have contributed to a reduced need for active use of MICNs in the months that followed.
It is also possible that many of the nursing staff were replaced in the summer by temporary personnel and new employees with less experience, and that this employee group needed more assistance and guidance from the MICNs. This may explain the increased use of MICNs in July (figure 2). At the same time, our analyses show that the patients that the MICNs were called out to had a median NEWS score of 8. According to both internal recommendations (table 1) and international recommendations, this score triggers the need for a doctor to be called out and measures started to stabilise the patient (13). MICNs were also called out to patients with a low score, which may be an indication that MICNs were also considered to represent a low-threshold service.
In group 1, we observed that MICNs were contacted to give advice to ward nurses, which was also noted in group 2. The high number of cases where ward nurses requested advice from MICNs may be an indication that it was easy and safe to contact MICNs for this reason. Providing support and training in different procedures was also covered in the definition of advice. This is in line with the purpose of establishing MICNs, and corresponds with the recommendations in other studies (15).
In group 2, supplying 02 in cases of hypoxaemia, intravenous fluid for hypotension and medication were the most widely used measures. These measures are easy to carry out, as described in other studies (19, 24). The ‘bedrest’ measure was also used frequently, but we have not found descriptions of this measure in international studies. This measure may be considered to be of little importance in an emergency situation, despite being described as a basic nursing measure in nursing literature (25).
Reduced mortality?
It is known that patients who suffer a severe deterioration in their condition, including patients in cardiac arrest, show signs of deterioration several hours earlier. In order to prevent catastrophic outcomes, these warning signs must be treated at an early stage (26–28). In a meta-analysis from 2010, it was not possible to conclude that RRTs reduced mortality (29). However, in the latest meta-analyses, Solomon et al. (8) and Maharaj et al. (9) concluded that RRTs/METs reduced mortality and the occurrence of cardiac arrest.
Our study was not designed to capture these peripheral points. On the other hand, the findings show that only 16 of the patients who MICNS were called out to were transferred to an intensive care unit. Since this study has only used the registration form that was used by MICNs and has not mapped long-term data, we cannot rule out the transfer of patients to an intensive care unit at a later date. Hillman et al. (16) found that METs did not contribute to any significant reduction in the number of admissions in intensive care units, while a Dutch study found a downward trend in the number of intensive care admissions (3).
We also found that most (75 per cent) of the patients admitted to an intensive care unit had respiratory problems. We assume that the majority of these needed respiratory support using, for example, Continuous Positive Airway Pressure (CPAP) or Bilevel Positive Airway Pressure (BiPAP). Future studies aimed at mapping efficacy are needed in order to examine the clinical effect of MICNs, including early transfer to an intensive care unit, or reduced transfers due to early intervention.
Where call-out times and the time taken to initiate measures exceed 15 minutes, a poorer prognosis may be expected (22). Our survey showed that MICNs had a median call-out time of 5 minutes. Silva et al. (1) reported a call-out time of less than 2 minutes for METs. The fact that the MICNs’ call-out time in our study was more than twice that of the other study may be because our hospital covers a large area and some departments are located a considerable distance from the MICNs’ base. Other studies reported call-out times of 4.5 and 12.3 minutes respectively (17, 19).
Weaknesses of the study
In addition to the obvious weaknesses of a cross-sectional study, this study also has a short period of inclusion. It also only covers a small number of call-outs and patients. The finding that patients mainly had respiratory problems may also be due to seasonal variations. Despite these weaknesses, we believe that the study provides valuable clinical information that can be used in the further development of these types of services.
Conclusion
Mobile intensive care nurses are usually called out to medical patients whose condition has deteriorated due to respiratory problems. Future studies should assess whether it is possible to identify symptoms of deterioration at an earlier stage, so that targeted treatment can be initiated sooner and transfer to a higher level of treatment can potentially be avoided.
The measures initiated for the patients are, in principle, simple measures that nurses with broad knowledge and good clinical knowledge can deal with. Future studies should therefore examine whether such a role can also be filled by advanced clinical nurses and not exclusively intensive care nurses. Mobile specialist nurse models can also potentially be tested in the primary health service.
References
1. Silva M, Saraiva M, Cardoso T, Aragao, IC. Medical Emergency Team: How do we play when we stay? Characterization of MET actions at the scene. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2016 Mar 22;24:33.
2. Jones D, Rubulotta F, Welch J. Rapid response teams improve outcomes: yes. Intensive Care Med 2016 42:593–595.
3. Ludikhuize J, Brunsveld-Reinders AH, Dijkgraaf M, Smorenburg S, de Rooij S et al. Outcomes associated with the nationwide introduction of Rapid Response Systems in the Nederlands. Critical care Medicine Dec 2015;2544–51.
4. Priestley G, Watson W, Rashidian A, Mozley C, Russell D, Wilson J et al. Introducing Critical Care Outreach: a ward-randomised trial of phased introduction in a general Hospital. Intensive Care Med 2004;30:1398–1404.
5. Stafseth SK, Grønbeck S, Lien T, Randen I, Lerdal A. The experiences of nurses implementing the Modified Early Warning Score and a 24-hour on-call Mobile Intensive Care Nurse: An exploratory study. Intensive Critical Care Nursing 2016 Jun;34:25–33.
6. Nordlund K, Joelsson-Alm E. Mobil intensivvårdsgrupp ger bättre patientövervakning och trygg personal. Läkartidningen 2009;42:2690–3.
7. Marquet K, Claes N, De Troy E, Kox G, Droogmans M, Schrooten W et al. One fourth of unplanned transfers to a higher level of care are associated with a highly preventable adverse event: A patient record review in six Belgian hospitals. Critical Care Medicine 2015 May;43(5):1053–61.
8. Solomon RS, Corwin GS, Barclay DC, Quddusi SF, Dannenberg MD. Effectiveness of rapid response teams on rates of in-hospital cardiopulmonary arrest and mortality: A systematic review and meta-analysis. Journal of Hospital Medicine 2016 Jun;11(6):438–45.
9. Maharaj R, Raffaele I, Wendon J. Rapid response systems: a systematic review and meta-analysis. Critical Care 2015 Jun 12;19:254.
10. Choi S, Lee J, Shin Y, Jung J, Han M, Son J et al. Effects of a medical emergency team follow-up programme on patients discharged from the medical intensive care unit to the general ward: a single-centre experience. Journal of Eval Clinical Practice 2016 Jun;22(3):356–62.
11. Topple M, Ryan B, Baldwin I, McKay R, Blythe D, Rogan J et al. Tasks completed by nursing members of a teaching hospital Medical Emergency Team. Intensive Critical Care Nurse 2016 Feb;32:12–9.
12. Torsvik M, Gustad LT, Mehl A, Bangstad IL, Vinje LJ et al. Early identification of sepsis in hospital inpatients by ward nurses increases 30-day survival. Crit Care 2016;20:244.
13. Calzavacca P, Licari E, Tee A, Egi M, Downey A et al. The impact of Rapid Response System on delayed emergency team activation patient characteristics and outcomes—A follow-up study. Resuscitation 2010 Jan;81(1):31–5.
14. Mullins CF, Psirides A. Activities of a Medical Emergency Team: a prospective observational study of 795 calls. Anaesth Intensive Care 2016 Jan;44(1):34–43.
15. Jung B, Daurat A, De Jong A, Chanques G, Mahul M, Monnin M, Molinari N, Jaber S. Rapid response team and hospital mortality in hospitalized patients. Intensive Care Medicine 2016 Apr;42(4):494–504.
16. Hillman K, Chen J, Cretikos M, Bellomo R, Brown D, Doig G et al. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet 2005;365:2091–7.
17. Konrad D, Jaderling G, Bell M, Granath F, EkbomA, Martling CR. Reducing in-hospital cardiac arrests and hospital mortality by introducing a medical emergency team. Intensive Care Med 2010;36:100–6.
18. Aneman A, Frost SA, Parr MJ, Hillman KM. Charasteristics and outcomes of patients admitted to ICU following activation of the Medical Emergency Team: Impact of introducing a Two-Tier Response System. Critical Care Medicine 2015 Apr;43(4):765–73.
19. Bellomo R, Goldsmith D, Uchino S, Buckmaster J, Hart GP, Opdam H et al. A prospective before-and-after trial of a medical emergency team. Med J Aust 2004 Mar 15;180(6):308.
20. Chen J, Bellomo R, Flabouris A, Hillman K, Finfer S. The relationship between early emergency team calls and serious adverse events. Crit Care Med 2009 Jan;37(1):148–53.
21. Cretikos M, Chen J, Hillman K, Bellomo R, Finfer S, Falbouris A et al. The objective medical emergency team activation criteria: a case-control study. Resuscitation 2007 Apr;73(1):62–72.
22. Chen J, Bellomo R, Flabouris A, Hillman K, Assareh H. Delayed emergency team calls and associated hospital mortality: A multicenter study. Critical Care Medicine 2015 Oct;43(10):2059–65.
23. Jackson S, Penprase B. Factors influencing registered nurses' decision to activate an Adult Rapid Response Team in a community hospital. Dimens Crit Care Nurs 2016;35(2):99–107.
24. Lobo R, Lynch K, Casserly LF. Cross-sectional audit on the prevalence of Elevated National Early Warning Score in medical patients at a Model 2 hospital in Ireland. Ir J Med Sci 2015 Dec;184(4):893–8.
25. Eikeland A, Gimnes M, Holm HM. Sirkulasjonssvikt. I: Gulbrandsen T, Stubberud DG (red). Intensivsykepleie. Akribe AS, Oslo. 2010.
26. Goldhill DR, White SA, Sumner A Physiological values and procedures in the 24 h before ICU admission from the ward. Anaesth 1999;54:529–34.
27. Smith AF, Wood J. Can some inhospital cardio-respiratory arrests be prevented? A prospective survey. Resuscitation 1998;37:133–7.
28. McQuillan P, Pilkington S, Allan A, Taylor B, Short A, Morgan G, Nielsen M, Barrett D, Smith G. Confidential inquiry into quality of care before admission to intensive care. Br Med J 1998;316:1853–8.
29. Chan P, Jain R, Nallmonthu BK, Berg RA, Sasson C. Rapid Response Team: A systematic review and meta-analysis. Arch Intern Med 2010 Jan 11;170(1):18–26.









Comments