Simulation-based team training in paediatric units
Simulation-based team training improves quality of patient care, but the training should be a planned activity.
Background: Medically justifiable practice of health care requires collaboration between the health professionals involved, who must have excellent professional knowledge and practical training in teamwork. In recent decades, healthcare providers have undergone simulation training in realistic patient situations demanding complex decision-making and teamwork. The training was based on experiences with “Crew Resource Management” (CRM) used in civil aviation.
Objective: To describe the experiences of clinical nurse specialists working in paediatric units related to participation in simulation-based team training and the impact this may have on patient care in emergency situations.
Method: The study has a qualitative, inductive and descriptive design. The sample consisted of ten clinical nurse specialists recruited from the paediatric units of three different hospitals. Data were collected through individual interviews and analysed according to Graneheim and Lundman’s (2004) content analysis.
Results: Clinical nurse specialists in paediatric units described the importance of a scheduled and realistic simulation, how they learn and cope through simulation, and the importance of these simulations for their performance in emergency situations.
Conclusion: Clinical nurse specialists in this study found that participation in simulation-based team training contributes to enhancing the quality of patient care and confidence in their own skills. They emphasise that simulation-based team training should be offered as a scheduled activity. The organisation and implementation of simulation in individual paediatric units is described as random and lacking in clear requirements and parameters. This study may indicate a need for a common Norwegian standard for simulation-based team training to ensure patient safety in emergency situations.
Medically justifiable practice of health care requires collaboration between the health professionals involved. They must have sound professional knowledge and practice in coordination (1, 2). In recent decades, healthcare providers have undergone simulation training in realistic patient situations demanding complex decision making and teamwork. The training was based on experiences with ‘Crew Resource Management’ (CRM) (3-7), as used in civil aviation.
Simulation-based training is described as a measure to improve teamwork, reduce adverse events and improve patient safety (3, 7, 8). Establishing simulation-based team training requires resources for training facilitators (instructors), as well as available room capacity and equipment. The task of facilitators is to facilitate learning (7, 9).
Ziv and collaborators define simulation as ‘any educational activity that utilizes simulation aids to replicate clinical scenarios’ (10), and it is divided into three phases:
- the briefing phase, in which the participants are informed of what will happen, the learning objectives, the patient simulator, the room and available equipment
- the implementation phase, in which the participants implement the scenario and behave as though it were a real patient situation
- the debriefing phase, in which the participants have the opportunity to reflect on their participation in the simulation as compared with the predetermined learning objectives.
Simulation has been shown to enhance knowledge and skills. However, only a small number of studies support its transfer value to clinical practice (11, 12). The educational principles that lead to effective learning are discussed. According to Motola and collaborators, feedback, awareness of practice and integration of theory are key elements (13).
The purpose of the study was to describe how clinical nurse specialists experience their participation in simulation-based team training. We also wished to describe the impact that this training may have on patient care in an emergency situation.
We formulated the following research questions:
- ‘How do you find that simulation-based team training is organised and implemented in your unit?’
- ‘How do you find that participation in simulation-based team training affects your competence in emergency situations?’
- ‘In your opinion, what impact does simulation-based team training have on patient care in an emergency situation?’
Method
The study has a qualitative, inductive and descriptive design based on ten individual, semistructured interviews.
Sample
We invited senior charge nurse at seven hospitals in one selected regional health authority to participate. We included nurse specialists in intensive, paediatric and neonatal care (clinical nurse specialists with between two and ten years of experience from the paediatric units at three hospitals. The participants needed to have undergone simulation-based team training in the previous year, and been involved in a minimum of one emergency situation since then. The sample consisted of nine women and one man, employed in 70–100 per cent positions.
Ethical considerations
We obtained informed consent from the participants, and the study followed guidelines for research ethics (14). The Norwegian Centre for Research Data (NSD) considered that the study was exempted from the obligation to give notification and to obtain a licence. None of the informants withdrew from the study.
Data collection
The interviews were conducted at the informants’ workplace and were undertaken over a period of three months. In the interviews, we needed to strike a balance between seeking answers to the research questions and allowing the informants to speak freely. An interview guide based on the research questions gave structure to the interview, while the follow-up questions encouraged more detailed information. We recorded the interviews on a dictaphone, having obtained the informed consent of the participants.
Analysis
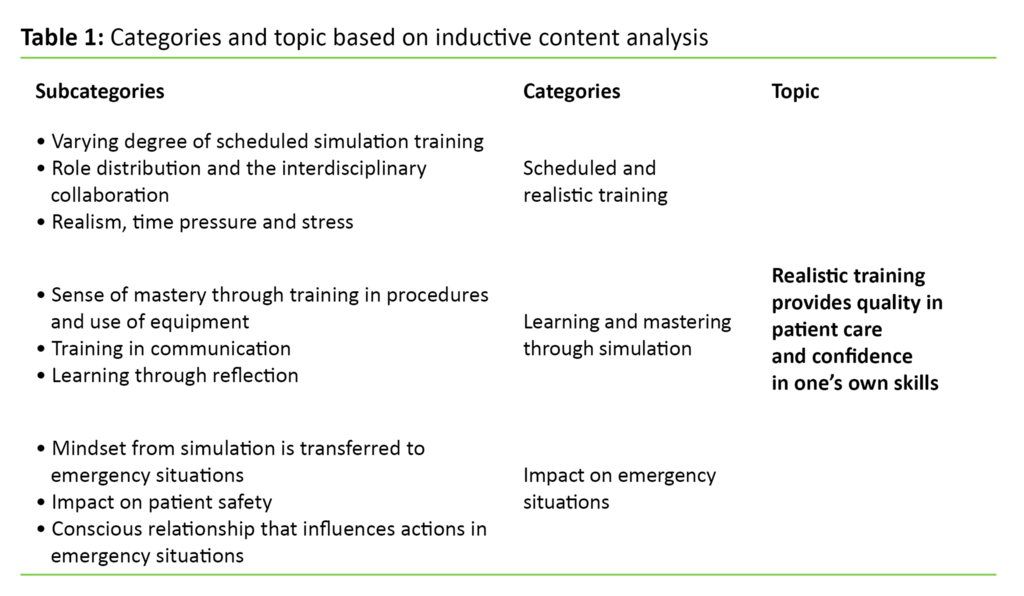
In order to identify meaning units in the text, we analysed the interviews based on Graneheim and Lundman’s qualitative content analysis method (15). We listened continuously and repeatedly to the audio files to ensure verbatim transcription. Meaning units were identified and converted to condensed text, then arranged according to subject matter. A systematic and continuous process of analysis resulted in nine subcategories, three descriptive categories and one latent content.
Methodological considerations
Two of the authors had extensive work experience from paediatric units and had participated in simulation-based team training in their own unit. The third author had experience with simulation used in nurse education. In order to reduce sample-related errors, we excluded our own workplace and took no part in the recruitment of informants.
Results
The results were synthesised into one latent content that expresses the underlying opinion communicated by all the clinical nurse specialists: ‘Realistic training provides quality and confidence in one’s own skills.’ The content includes three descriptive categories (Table 1):
- scheduled, realistic training
- learning and mastery through simulation
- impact on emergency situations
Scheduled, realistic training
The clinical nurse specialists described the various ways in which simulation is planned, organised and implemented. They reflected on role distribution and interdisciplinary collaboration, and described their perception of realism, time pressure and stress during the simulation.
The majority of the clinical nurse specialists had experience of simulation-based team training that was held weekly in the unit. They were uncertain whether they could be freed from their work with patients, as it was only decided on the same morning who would participate. The training was perceived as a non-scheduled activity, and the clinical nurse specialists explained that the simulation training needed to be more systematic.
Three clinical nurse specialists had participated in simulation-based team training at a simulation centre up to three times per year. The unit management’s objective was that all employees should attend, and participation was therefore included in scheduling of rosters. The clinical nurse specialists reported having obtained a good learning outcome from regular training.
The clinical nurse specialists described the simulation of real patient situations in an interdisciplinary context together with doctors and nurses as very instructive and realistic. They immersed themselves in the scenario, felt the time pressure and could feel their pulses racing. When they were challenged on recognisable elements from practice, such as the role of next of kin, the entire scenario became more realistic. The clinical nurse specialists perceived the scenario and the simulation training as an authentic emergency situation.
Through the training in roles and role distribution, the clinical nurse specialists became more aware of the content of their own role, and also that of other roles in the team. Training in leadership was especially important. One clinical nurse specialist stated the following:
‘I think I got a lot of benefit from it, especially regarding roles. They are very conscious of roles when we are taking part in the simulation.’
Learning and mastery through simulation
The clinical nurse specialists described the feeling of mastery they acquired from training in communication, procedures and use of medical equipment. They also described how they learned through reflection.
The clinical nurse specialists found it to be advantageous that the simulation-based team training was undertaken in the same location where emergency situations arise. In a familiar environment, they were able to concentrate on the scenario and find and hook up emergency medical equipment such as a ventilator. Regular training with medical equipment and relevant procedures resulted in better coping For example, simulation training could focus on advanced cardiopulmonary resuscitation. Theoretical teaching often formed part of the preparations and could be linked to cardiopulmonary resuscitation, like the algorithm for resuscitation. In their opinion, having both a theoretical and practical element enhanced their competence. One clinical nurse specialist described the participation as follows:
‘If you manage to forget that it is a training situation, and try to focus on learning, you learn a great deal.’
They highlighted the importance of good communication in the team. The clinical nurse specialists explained that emergency situations could be chaotic, and might give rise to harsh words and aggressive behaviour. They believed that training in communication is necessary and that simulation-based training gives the whole team a unique opportunity to practise crisp and clear communication. This gives them more confidence in themselves and their role in the team.
The interviews revealed that clinical nurse specialists took a positive view of reflecting on what they had participated in, and what they had done well and less well. They indicated that this was important for learning. A facilitator was present in the simulation centre and led the debriefing. The weekly simulation could be conducted with or without a facilitator. Simulation without a facilitator was perceived as unstructured, and the participants did not feel that they were given a systematic review of what had occurred.
For example, they wanted the following type of feedback:
‘You might think about that next time, remember to give a clearer message, and to have it confirmed.’
Impact on emergency situations
The clinical nurse specialists described how they transferred their thought process from simulation to emergency situations. They also spoke of the impact that simulation had on patient care, and the aspects of simulation that affect their actions in an emergency situation.
In emergency situations, they automatically began to allocate roles and responsibilities in the way that they had been trained. They claimed that the time that had elapsed between the simulation and the occurrence of an emergency situation had an impact on how quickly they accessed their knowledge. One clinical nurse specialist described her experience of performing chest compressions on a baby in an emergency situation:
‘The feeling that with a baby, it was enough to use my fingers; I felt I was doing it correctly, in the way that I had been trained.’
The level of stress was reduced when they mastered the tasks and felt confident in emergency situations. All the clinical nurse specialists stated that simulation-based team training has an impact on patient care in emergency situations, and thereby also on patient safety. One clinical nurse specialist illustrated the impact on patient care as follows:
‘When you practise it, you know what to do, and you act more quickly. And this benefits the patient […] yes, you quite simply become more skilled.’
The clinical nurse specialists underlined the need to maintain and ensure necessary skills. In simulation-based team training, the clinical nurse specialists were drilled in realistic patient situations without entailing risk for the patient. They felt that they were able to test themselves, but also that they obtained confirmation of their own competence. At the same time, they claimed that interdisciplinary participation in simulation gave the team members a better understanding of each other, enabling the entire team to function better.
They had found that their managers and colleagues expected clinical nurse specialists to be competent and up-to-date, and to feel comfortable with mastering their tasks when an emergency arises. They were concerned about the lack of training in practice and found that they have little chance to build up experience-based expertise in pediatric units, where centralized patient management led to shorter hospital stays and less complexity.
Discussion
In this study, we wished to describe clinical nurse specialists’ experiences with participating in simulation-based team training in paediatric units. We also wished to examine the impact of this type of training on patient care in an emergency situation.
The importance of good planning and realism in simulation
The clinical nurse specialists claimed that simulation-based team training must be properly scheduled and organised to provide a learning outcome. In units that arranged weekly simulation training, the clinical nurse specialists found the training not to be well planned, with random opportunity for them to participate. However, if simulation-based team training was part of the ward’s objectives and was planned as part of the roster, they were able to participate regularly – up to twice yearly.
There was common agreement that resources must be allocated, and that managers and network administrators must see the need for a scheduled and organised simulation. This view is supported by the literature, which states that effective results are achieved through a systematic approach to incorporating simulation (5, 16). Investment in simulation should be endorsed by the management and included in the unit’s quality management (13, 17).
Realistic simulation important for learning
In order to provide a learning outcome from simulation-based team training, training in realistic patient situations is highlighted. The clinical nurse specialists stated that to achieve this, it is essential for all those healthcare providers that are present in emergency situations to train together. The literature supports the clinical nurse specialists’ opinion that it is essential for learning that the participants feel that the simulation is realistic (18). Scenarios should be designed that are linked to the learning objectives (7, 13). The participants must be prepared for what they are to react to during the scenario, and they should be familiar with the environment, available equipment and patient history (7, 19). Rules and expectations should be clarified in a briefing session, and the environment should be made safe in order for the participants to feel secure (13).
The literature also supports the clinical nurse specialists’ view that the entire team must train together. Østergaard and collaborators describe simulation that includes a complete, interdisciplinary team as a method which improves the quality of teamwork behaviours (9). In emergency situations, so-called ad hoc teams are formed, which may represent a challenge for team collaboration. They have little time to plan and may find it challenging that team members are unfamiliar with each other and each other’s competence (8, 20).
The importance of a good leader
Experience shows that team members also change continuously. Roberts and collaborators claim that even short simulation-based team-training sessions can improve teamwork and communication in ad hoc teams, as they enhance behavioural skills and critical thinking (20). According to Salas and collaborators (2008), ‘patient care is a team sport’ (21), and the composition of the teams who train together is therefore important.
The clinical nurse specialists also communicate the need for a good team leader to improve the progress and quality of patient care in emergency situations. They believe simulation training in leadership is important. Failures of leadership and team collaboration have been shown to be points of vulnerability for adverse events (8, 9, 20). Leading a team includes coordination and planning of the course of events, for which clear communication is absolutely essential.
Hunt and collaborators point out that a good leader must be capable of giving instructions and ensuring that messages are received, understood and acknowledged (8). Another important quality is to listen to the team members and collect and disseminate the information that emerges (7). Leadership is highly important in emergency situations, which underpins the need for training in this role to improve team collaboration in order to avoid adverse events.
Experience of learning and mastery through simulation
According to the clinical nurse specialists in this study, they both learned and coped by participating in stimulation-based team training. Three of them had participated in a simulation centre, which they found provided them with a considerable learning outcome. The majority of the clinical nurse specialists had experienced that the emergency room in the department was used as a practice area.
They claimed that it was very advantageous that the simulation was conducted in a familiar environment. The clinical nurse specialists described how they introduce elements from the simulation into emergency situations. This may indicate that simulation-based team training is beneficial for clinical practice.
The clinical nurse specialists’ perception that simulation-based training provides them with both learning and mastery may be explained by the fact that simulation as a learning activity builds on key principles of andragogy. The educator Malcolm Knowles claims that safe, familiar surroundings are important to enable adults to learn. He also says that adults learn best when learning provides immediate benefits (22, 23).
In situ training sessions
When healthcare providers train in the established simulation centres, they are given the opportunity to train in everything from simple skills at the individual level to advanced interactions and team-based decision-making (24). Using the emergency room in the department as a practice area, in an environment where emergency situations occur, is referred to in the literature as in situ training (25). The literature supports the need for in situ training in paediatric units, as this can enable healthcare providers to recognise signs of acute illness and therefore provide better treatment (26).
The study by Sørensen and collaborators showed that the participants perceived the situation as more realistic when the training was conducted in situ. It made no difference whether the simulation was conducted in a simulation centre or in situ, in terms of attitude to patient safety, coping with stress or teamwork (27).
The clinical nurse specialists had found that it could be challenging to achieve good communication and dialogue in emergency situations. Communication was set as a learning objective for the simulation training, underlining the importance for the entire team to train in communication. They described it as especially challenging to persuade team members to communicate (9). Good dialogue and communication within the team gives team members the courage to provide valuable input with regard to patient care (8). Based on the principles of CRM, the precise purpose of simulation is for the team members to communicate and cooperate (9). Training in communication skills should therefore be formulated as learning objectives in the simulation.
New knowledge acquired
Other learning objectives and attention with regard to the simulation-based team training were connected to advanced cardiopulmonary resuscitation and medical equipment. The clinical nurse specialists were supplied with new knowledge by participating in the simulation, while also obtaining confirmation of their own competence. They prepared themselves for the simulation by reading up on theory and described this as being useful to bring with them into emergency situations. The practical skills they acquired were also useful.
The concept of the learning circle is used in connection with simulation training. It means that theoretical knowledge is put into practice through training in patient situations before this knowledge is translated into clinical practice and experience is augmented for new learning (28, 29). This may indicate that simulation is a suitable learning activity for experienced clinical nurse specialists, and that it provides learning that can be transferred to emergency situations.
Importance of regularity and feedback
There was variation in the frequency with which clinical nurse specialists had the opportunity to participate in simulation, but those who were able to participate regularly reported having obtained a significant learning outcome from it. This tallies with recommendations from the Norwegian Society of Paediatricians that training in basic and advanced cardiopulmonary resuscitation should be undertaken at least every six months (17). This is also in line with Motola and collaborators, who claim that simulation is most successful when it is an established, regular activity (13). In considering how frequently simulation should be conducted, it is important that it is seen as a learning process, and not as a one-time event (30).
The clinical nurse specialists had positive experiences of debriefing and considered feedback from the facilitator and the participants to be important for learning. If simulation is to be used as an educational tool, reflection on one’s own efforts is essential (31). According to Eppich and Cheng, facilitated debriefing is necessary, as learning from simulation-based training begins after completion of the scenario (3, 32).
Hunt and collaborators furthermore claim that simulation training without reflection and feedback does not lead to effective learning (8). The facilitator directs the debriefing in order to elicit systematic reflection in the participants. The learning effect of reflection is therefore dependent on the supervisory expertise of the facilitator (9, 32). This underlines the importance of facilitator’s role, which is described in the literature as a key component of simulation training (9).
The importance for patient care in an emergency situation
The clinical nurse specialists claimed that they acted more quickly and effectively in emergency situations after having participated in simulation training. They brought with them elements from the training situation, such as distribution of roles and tasks and thinking about dialogue and communication in the team.
They argued that participation in simulation training provides an opportunity to enhance the clinical nurse specialists’ competence to act in emergency situations. All of them agreed that regular simulation-based team training in paediatric units is crucial for improving patient care in these situations. The literature supports the notion that training in communication, leadership and teamwork has an impact on patient safety (9). It also helps to enhance the technical skills of the individual participant as well as the team (33).
Truijens and collaborators claim that the patient-reported quality of health assistance improves when the personnel are trained in the principles of CRM (34). According to Draycott and collaborators, this is the first time that a pedagogical intervention has yielded a clinically important and permanent improvement in perinatal outcomes (35). The clinical nurse specialists take responsibility in this regard when they communicate a need to participate in simulation-based team training, because they wish to maintain their competence and improve patient care in emergency situations.
In order to substantiate the fact that simulation is a learning activity that actually improves patient safety, Schmidt and collaborators claim that there is also a need to identify clear patient safety objectives (33). Ziv and collaborators maintain that if simulation is not used as a learning activity, this constitutes not only a training issue, but also an ethical issue (10). Standardised training and certification through simulation-based team training makes it possible to reduce errors and adverse events, and thus improve patient safety. The establishment of this scheme will, in our opinion, enable the health services to appear more reliable and ethically sound.
Conclusion
The clinical nurse specialists in this study found that participation in simulation-based team training contributes to quality of patient care and confidence in one’s own skills. They highlight the need to offer simulation-based team training as a well-planned learning activity in paediatric units, with realistic scenarios and including the entire team. The clinical nurse specialists feel that by participating in simulation training they obtain confirmation of their own competence and a basis for further learning, mastery and sense of security. In the interviews, they point to examples from practice, showing that simulation training has had a positive influence on their competence to act in emergency situations.
This study revealed that the organisation and implementation of simulation in individual paediatric units is random and lacking in clear requirements and parameters. There may therefore be a need for a Norwegian standard for simulation-based team training for doctors and nurses in paediatric units to ensure patient safety in emergency situations.
References
1. Lovdata. Lov om helsepersonell. 2 juli 1999; nr. 4. [Helsepersonelloven]. Available at: https://lovdata.no/dokument/NL/lov/1999-07-02-64. (Downloaded 31.01.2017).
2. Lovdata. Lov om spesialisthelsetjenesten m.m. 2. juli 1999; nr. 61 [Spesialisthelsetjenesteloven]. Available at: https://www.lovdata.no/dokument/NL/lov/1999-07-02-61. (Downloaded 10.09.2016).
3. Gaba DM. The future vision of simulation in health care. Quality and Safety in Health Care 2004;13(suppl 1):i2–i10.
4. Jeffries PR. A frame work for designing, implementing, and evaluating simulations used as teaching strategies in nursing. Nursing Education Perspectives 2005;26(2):96–103.
5. Issenberg SB, Mcgaghie WC, Petrusa ER, Lee Gordon D, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Medical Teacher 2005;27(1):10–28.
6. Kohn LT, Corrigan J, Donaldson MS. To err is human: building a safer health system. Institute of Medicine (US) Committee on Quality of Health Care in America. Washington (DC): National Academies Press (US), 2000.
7. Ballangrud R, Husebø SE. Strategier og verktøy for teamtrening. I: Aase K (ed.). Pasientsikkerhet : teori og praksis 2. ed. Oslo: Universitetsforlaget, 2015.
8. Hunt EA, Shilkofski NA, Stavroudis TA, Nelson KL. Simulation: Translation to improved team performance. Anesthesiology Clinics 2007;25(2):301–19.
9. Østergaard D, Dieckmann P, Lippert A. Simulation and CRM. Best Practice & Research Clinical Anaesthesiology 2011;25(2):239–49.
10. Ziv A, Ben-David S, Ziv M. Simulation based medical education: an opportunity to learn from errors. Medical Teacher 2005;27(3):193–9.
11. Nestel D, Groom J, Eikeland-Husebø S, O'Donnell JM. Simulation for learning and teaching procedural skills: the state of the science. Simulation in Healthcare 2011;6(7):S10–S3.
12. Laschinger S, Medves J, Pulling C, McGraw D, Waytuck B, Harrison MB et al. Effectiveness of simulation on health profession students’ knowledge, skills, confidence and satisfaction. International Journal of Evidence‐Based Healthcare 2008;6(3):278–302.
13. Motola I, Devine LA, Chung HS, Sullivan JE, Issenberg SB. Simulation in healthcare education: a best evidence practical guide. AMEE Guide No. 82. Medical Teacher 2013;35(10):e1511–e30.
14. Sykepleiernes samarbeid i Norden. Etiske retningslinjer for sykepleieforskning i Norden 2003;23(4):1–20.
15. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today 2004;24(2):105–12.
16. McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. A critical review of simulation‐based medical education research: 2003–2009. Medical Education 2010;44(1):50–63.
17. Norsk barnelegeforening. Ferdighetstrening i norsk pediatri; en statusrapport 2010. Available at: http://legeforeningen.no/PageFiles/2988/Last%20ned%20rapporten.pdf. (Downloaded 10.09.2016).
18. Rystedt H, Sjöblom B. Realism, authenticity, and learning in healthcare simulations: rules of relevance and irrelevance as interactive achievements. Instr Sci 2012;40(5):785–98.
19. Brinchmann-Hansen A, Wisborg T, Brattebo G. Simulering – en god metode i legers videre- og etterutdanning. Tidsskrift for Den norske legeforening 2004;124:2113–5.
20. Roberts NK, Williams RG, Schwind CJ, Sutyak JA, McDowell C, Griffen D et al. The impact of brief team communication, leadership and team behavior training on ad hoc team performance in trauma care settings. The American Journal of Surgery 2014;207(2):170–8.
21. Salas E, DiazGranados D, Weaver SJ, King H. Does team training work? Principles for health care. Academic Emergency Medicine 2008;15(11):1002–9.
22. Clapper TC. Beyond Knowles: What those conducting simulation need to know about adult learning theory. Clinical Simulation in Nursing 2010;6(1):e7–e14.
23. Knowles MS, Holton III EF, Swanson RA. The adult learner: The definitive classic in adult education and human resource development. 8. utg. Hoboken, New Jersey: Taylor and Francis. 2014.
24. SAFER. Available at: https://www.safer.net/om-safer/. (Downloaded 30.05.2012).
25. Kobayashi L, Patterson MD, Overly FL, Shapiro MJ, Williams KA, Jay GD. Educational and research implications of portable human patient simulation in acute care medicine. Academic emergency medicine 2008;15(11):1166–74.
26. Theilen U, Leonard P, Jones P, Ardill R, Weitz J, Agrawal D et al. Regular in situ simulation training of paediatric medical emergency team improves hospital response to deteriorating patients. Resuscitation 2013;84(2):218–22.
27. Sørensen JL, van der Vleuten C, Rosthøj S, Østergaard D, LeBlanc V, Johansen M et al. Simulation-based multiprofessional obstetric anaesthesia training conducted in situ versus off-site leads to similar individual and team outcomes: a randomised educational trial. BMJ open 2015;5(10):e008344.
28. Lindamood KE, Weinstock P. Application of high-fidelity simulation training to the neonatal resuscitation and pediatric advanced life support programs. Newborn and Infant Nursing Reviews 2011;11(1):23–7.
29. Kolb AY. The Kolb learning style inventory–version 3.1 2005 technical specifications. Boston, MA: Hay Resource Direct; 2005.
30. Beaubien J, Baker D. The use of simulation for training teamwork skills in health care: how low can you go? Quality and Safety in Health Care 2004;13(suppl 1):i51–i6.
31. Cates LA, Wilson D. Acquisition and maintenance of competencies through simulation for neonatal nurse practitioners: Beyond the basics. Advances in Neonatal Care 2011;11(5):321–7.
32. Eppich W, Cheng A. Promoting Excellence and Reflective Learning in Simulation (PEARLS): development and rationale for a blended approach to health care simulation debriefing. Simulation in Healthcare 2015;10(2):106–15.
33. Schmidt E, Goldhaber-Fiebert SN, Ho LA, McDonald KM. Simulation exercises as a patient safety strategy: a systematic review. Annals of Internal Medicine. 2013;158(5_Part_2):426–32.
34. Truijens SE, Banga FR, Fransen AF, Pop VJ, van Runnard Heimel PJ, Oei SG. The effect of multiprofessional simulation-based obstetric team training on patient-reported quality of care: A pilot study. Simulation in Healthcare 2015;10(4):210–6
35. Draycott T, Sibanda T, Owen L, Akande V, Winter C, Reading S et al. Does training in obstetric emergencies improve neonatal outcome? BJOG: An International Journal of Obstetrics & Gynaecology 2006;113(2):177–82.










Comments