Urinary tract infection among older patients in the home care services
Differences in the level of knowledge and unreliable equipment make it difficult for health personnel in the home health care services to discover and diagnose urinary tract infection. We need national guidelines for the collection of urine samples and the use of urine dipsticks in the home care services.
Background: Urinary tract infection (UTI) is the most common infection among older patients in home care services. Quick and reliable diagnosis of UTI depends on assessment methods with as few errors as possible, as well as the knowledge level of UTI among involved health personnel.
Purpose: This article presents a survey of the knowledge level of UTI and the practice of UTI assessment methods among health personnel in the home care services. The purpose of the study was to identify possible points of improvement for practice in home care.
Method: We developed a questionnaire with 16 items, distributed it to 209 employees in the home care services in six Norwegian municipalities. 141 employees responded (response rate: 67.5 per cent).
Results: Several areas for potential improvement were identified. There is a need for better knowledge among all health personnel when it comes to symptoms related to UTI. Areas of potential improvement with regard to the urine dipstick were: interpretation of the urine dipstick, and optimal amount of urine for testing. Areas of potential improvement for handling urine samples were knowledge of sources of contamination, storage of the urine samples, routines for shipment, and sufficient documentation.
Conclusion: We recommend the development of national guidelines for the procedure for handling UTI assessment methods in the home care services. More reliable and effective diagnostic tools for UTI in older patients in home care are needed.
Although many older people remain in good health, increasing age is related to degree of morbidity (1, 2). One of the most frequently occurring bacterial infections among the elderly is urinary tract infection (UTI) (3). In 2014 59.3 percent of recipients of home care services were above retirement age (4), which suggests that among the users of home care services a number will contract UTI.
Diagnosing urinary tract infection
Typical symptoms of UTI are painful urination, frequent urination and fever; in older patients, however, vaguer symptoms such as confusion, dizziness and increased tendency to fall may also indicate UTI (2, 3, 5). When health personnel register symptoms of UTI in elderly home dwelling patients, they will frequently respond by taking a urine dipstick test.
If the urine dipstick shows positive for nitrite and/or leukocytes, health personnel will generally contact a physician (6) by telephone, e-mail or in person, and antibiotics will be prescribed (7). Although UTI is the most common type of bacterial infection, elderly patients are frequently overdiagnosed and overtreated due to vagueness of symptoms and high incidence of asymptomatic bacteriuria (ASB) (5, 8-10), which shall not be treated according to clinical guidelines (11-14).
A frequently used assessment method is using a urine dipstick; there are, however, several sources of error related to the use and interpretation of the urine dipsticks in relation to the various parameters such as leukocytes, nitrite and others (5, 10, 15). Much suggests that urine dipsticks are inappropriate for diagnosing UTI in the elderly, as the method is not very reliable. Urine dipsticks cannot distinguish between UTI and ASB (9, 10, 16).
In addition to using urine dipsticks, a urine sample is often collected for culture. To ensure a reliable test result it is essential that the urine sample is properly handled during collection, transportation, storage, analysis and reporting (5, 15). There are currently no guidelines for urine sample collection in the home care services, whereas a gold standard exists for hospitals (17).
Routines for urine sample collection leave sources of error
Current routines for urine sample collection in the home care services appear to have several sources of error. Collecting a urine sample from urine incontinent patients that use urine absorbent products is especially difficult. The way the home care services are organised often result in the nurses having to drive long distances, alone and with many patients to serve before returning to the home care services offices. This can make following correct procedures for storing urine samples and sending them to microbiological testing difficult (18).
Health personnel are uncertain of whether they have read the urine dipstick correctly due to difficulties in distinguishing the colour nuances on the stick.
The symptoms of UTI are often atypical (2), and the reliability of urine dipsticks and urine samples is uncertain. That is why many emphasise the importance of a holistic nursing approach, in which the mapping of vital signals such as pulse, temperature and blood pressure is essential (9, 10). From this follows that health personnel must have sufficient knowledge to recognise symptoms and act adequately, so that patients receive the help they need. After searching several databases we have not found any research addressing health personnel’s knowledge on UTI or how urine dipsticks and urine samples are applied and collected, treated and read in the home care services in Norway. We want measures that will contribute to quick and secure diagnosis, which would also hinder overtreatment of UTI.
The study’s research question
It is not clear which knowledge health personnel in the home care services have on UTI and how they perform the necessary tests in connection with UTI. We therefore designed a survey to identify points of possible improvement of practice. The survey had the following research questions:
- What knowledge do health personnel have on symptoms of UTI?
- How are urine dipsticks used and urine samples collected and treated in the home care services?
- How do health personnel experience the utility and the reading of the urine dipstick parameters?
Method
Design
The survey is designed as a cross sectional study. We developed a questionnaire to map knowledge on UTI, use of urine dipsticks, and urine sample collection. The questionnaire contained 16 questions, of which 11 were multiple-choice questions. Two were open questions, and three were demographic questions (profession, number of years in the work place, and position). To the majority of the questions more than one answer was possible. The authors developed the questionnaire in collaboration with a professional development nurse and a leader for the relevant unit in a Norwegian municipality. The questionnaire was twice tested for content validity with typical respondents, a total of six employees in the home care services. These respondents gave their opinions on whether the questionnaire was acceptable, understandable, relevant for the setting, and free of ambiguities (19).
Data collection
We invited six municipalities in South East Norway, and they were all willing to participate in the study. The questionnaire was administered electronically via Questback survey. The inclusion criterion for participation in the survey was employment in the home care services, either as a permanent employee, a nursing student or a substitute. All employees in the home care services in the six municipalities were invited and encouraged to participate. Those invited received a letter with information on the study with a link or QR code to the questionnaire, or an e-mail with information and link to the questionnaire.
Analysis
We analysed differences between the groups by using chi square test and analysis of variance (ANOVA) where 1000 bootstrap samples were chosen, as a normal distribution could not be ascribed to all variables. The analyses were performed using SPSS version 22. A strict level of statistical significance was set at p£0.01 to avoid the multiple comparisons problem. We did a principal factor analysis of question 13 to reduce the many response alternatives to a manageable size. We extracted factors with value ³1 and used oblique rotation (direct oblimin) as we expected the factors to correlate (20).
Result
The questionnaire was sent to 209 employees in the home care services, including registered nurses, assistant nurses, nursing students and assistants (health personnel without formal nursing education), in six Norwegian municipalities. A total of 141 persons responded (response rate 67.5 percent). Of the respondents 49 percent were registered nurses, 21 percent assistant nurses, 7 percent assistants, 3 percent department leaders and 20 percent nursing students. The registered nurses had worked on average 4.7 years in the home care services and 70 percent of the registered nurses had a permanent position.
What knowledge on symptoms of UTI do health personnel possess?
Question 2 in the questionnaire asks: “What symptoms do you consider to be the most important signs of UTI?” All health personnel groups agreed that confusion is an important symptom of UTI while apathy and anorexia are not. Table 1 shows what health personnel in the home care services consider to be the most important symptoms of UTI in their patients. The symptoms are here ranked by what the nurses considered to be the most important compared to what the other professions considered the most important signs of UTI. For instance, 90 percent of the registered nurses considered confusion to be an important symptom of UTI, while 70 percent of the nursing students said the same. The analysis shows that there was a statistically significant difference between the groups on “deteriorating general condition”, “burning pain when urinating” and “bad-smelling urine”. This shows that there was disagreement or different levels of knowledge as to how important these symptoms were.
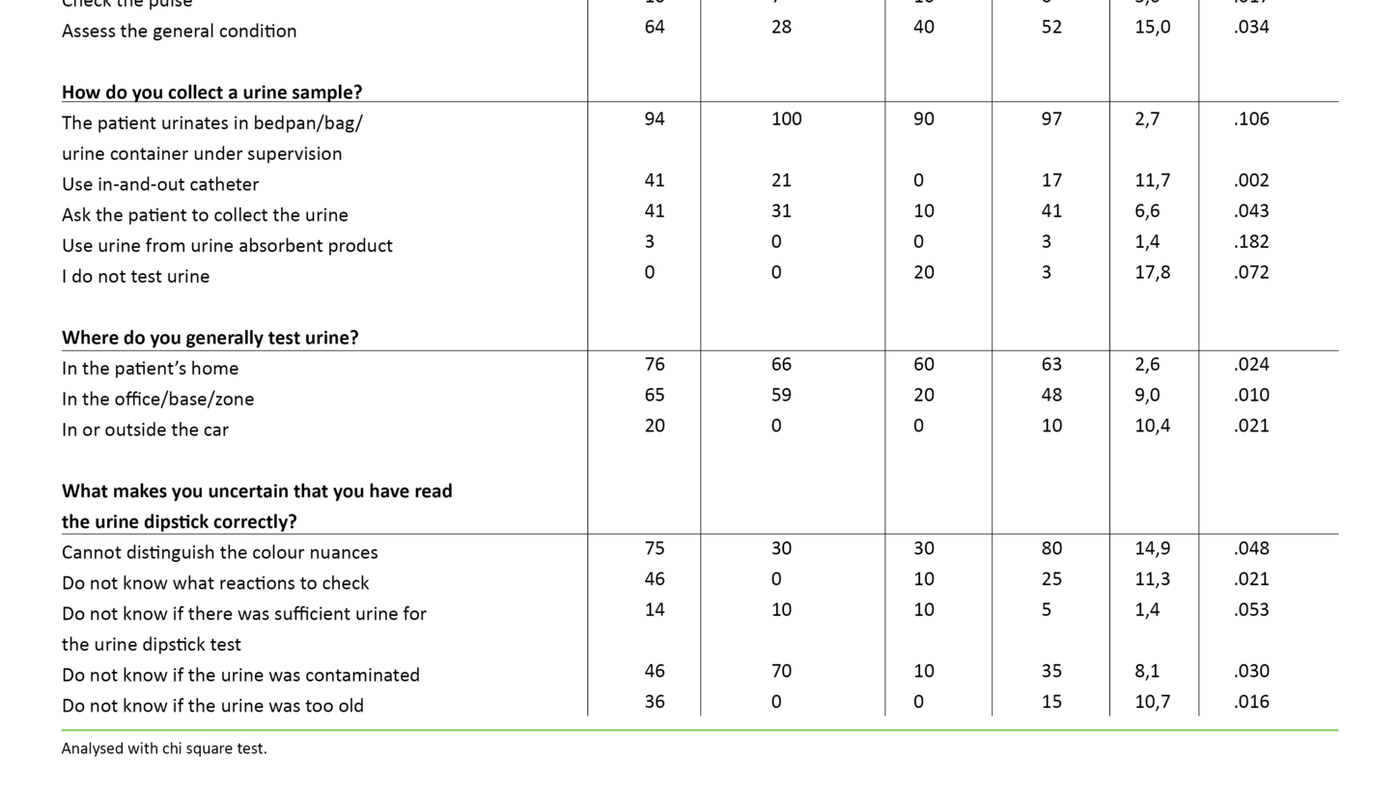
Question 4, “What do you do when you notice that a patient has symptoms of UTI?” is intended to map whether health personnel are able to act adequately on symptoms of UTI. The results from question 4 (see table 1) show that the great majority consider UTI to be their area of responsibility, and assistant nurses (34 percent), students (38 percent) and assistants (90 percent) contact a registered nurse and ask for assistance or advice as to how to proceed. Half of the registered nurses state that they contact a physician, while the great majority (excepting 40 percent of the assistants) use a urine dipstick when they see signs of UTI in a patient.
The number of personnel who collect a urine sample varies among personnel groups, but 67 percent of registered nurses say they collect a urine sample at symptoms of UTI. Relatively few within all groups check temperature and pulse (from 0 – 26 percent), whereas 64 percent of registered nurses assess the patient’s general condition at symptoms of UTI.
How are urine dipsticks and urine samples used and treated?
Question 5 maps practice for urine sample collection in the home care services. The results show that for all groups it is most common to let the patient urinate in a bedpan, plastic urine bag or urine container under supervision (from 94 – 100 percent) (table 1). Some ask the patient to collect the urine; 41 percent of the registered nurses do this. The purpose of question 12 is to map practice for urine dipstick use. The results show that the majority of health personnel use the dipstick in the patient’s home or at the office, base or the zone in which they work (from 76 to 20 percent) (table 1).
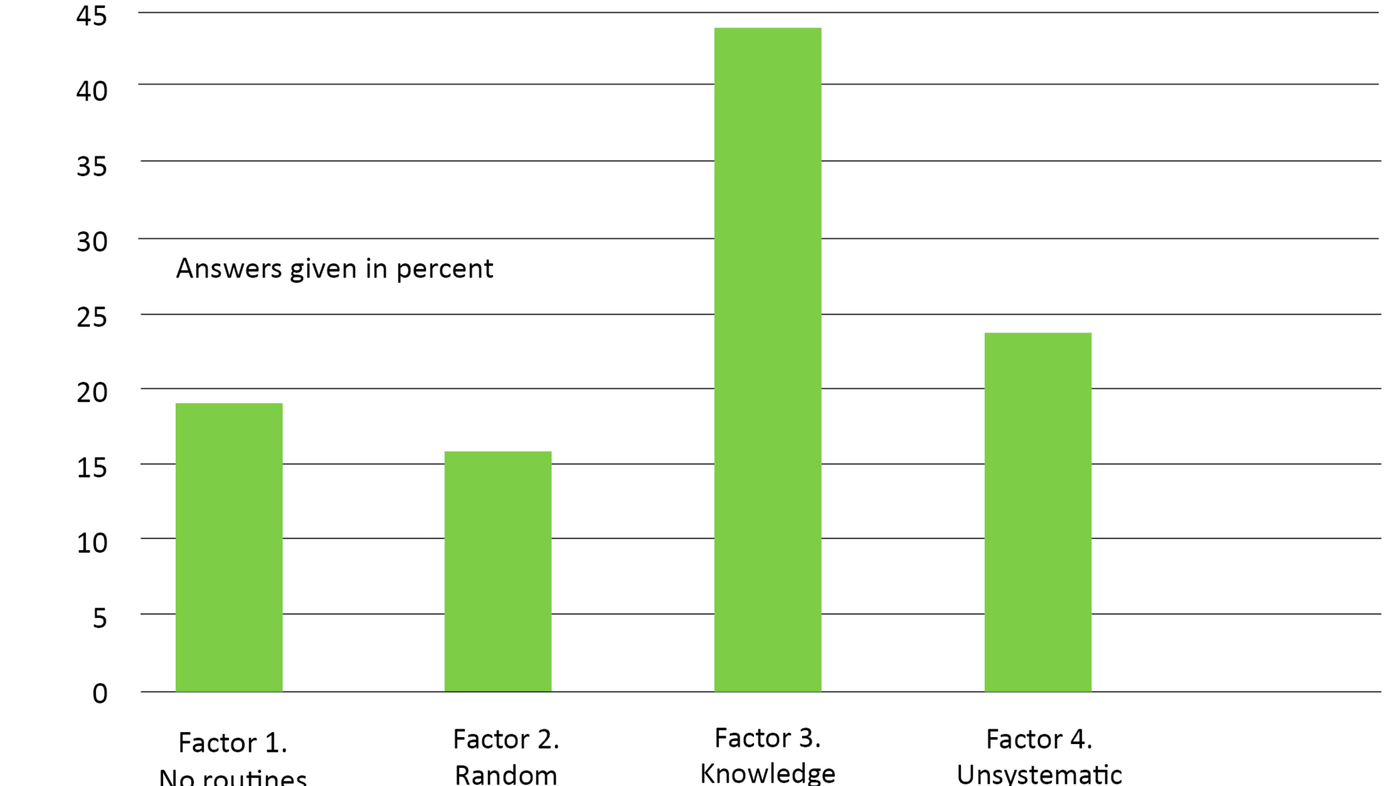
Question 13 asks: “If you collect a urine sample for culture (to send to physician/laboratory), which of the suggested alternatives do you recognise from your work day?” The factor analysis of the answers to this question yielded four factors that we have given the following names: “no routines”, “random storage”, “knowledge-based routines” and “unsystematic practice”. Table 2 shows the results from the factor analysis (20). Analyses of the differences between the personnel groups on the four factors for urine sample handling showed that the registered nurses scored the highest on factor 1 (no routines) and factor 4 (unsystematic practice) (statistically significant).
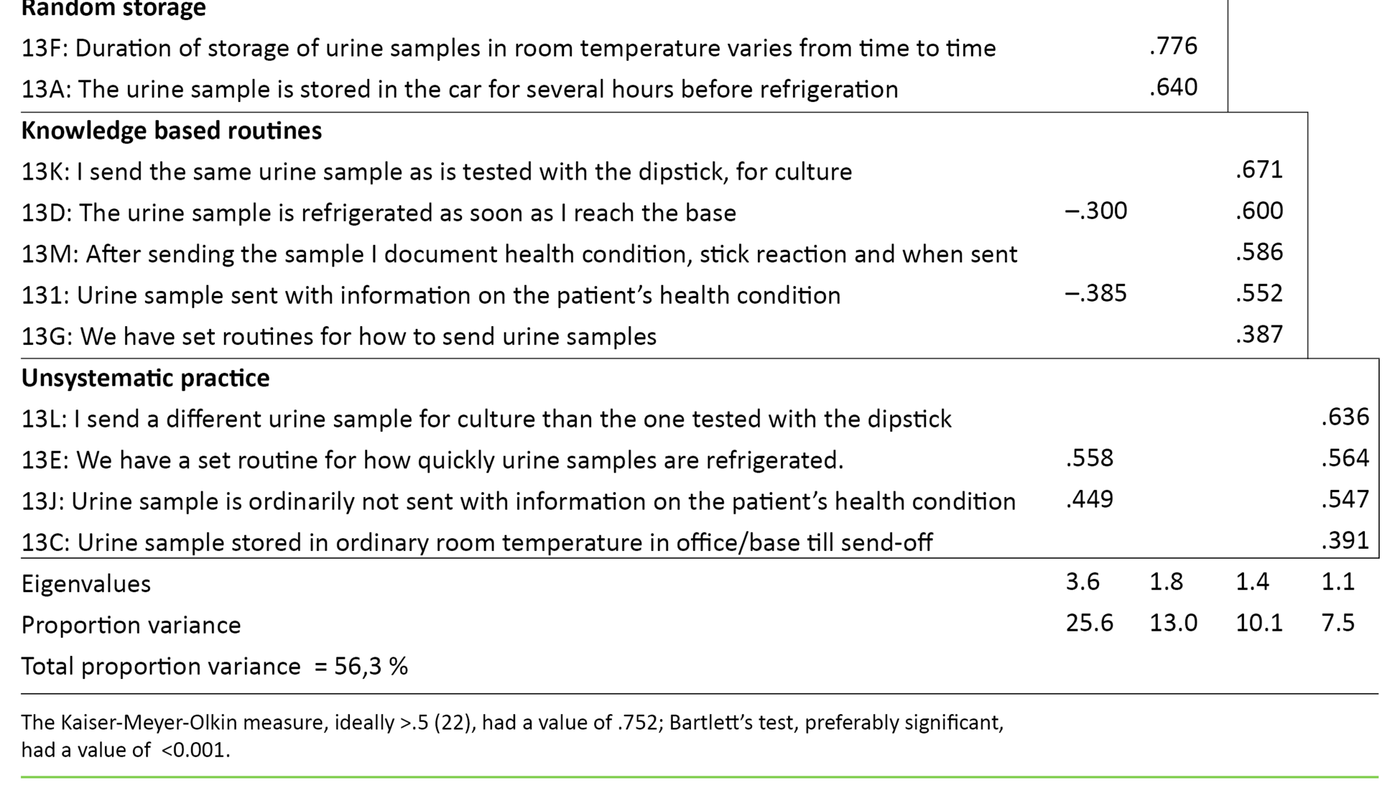
Assistants scored the highest on factor 2 (random storage) (not significant), and assistant nurses scored the highest on factor 3 (knowledge-based routines)(not significant). Figure 1 gives a graphical presentation of the registered nurses’ share of maximum score on the four factor variables – that is, how high the registered nurses score on average on the factors in relation to what was the highest possible score. The figure shows that the registered nurses score the highest on knowledge-based routines.
How do health personnel judge the utility of or problems related to urine dipsticks?
Question 6 asked: “If you use a urine dipstick to check for the presence of UTI, what reactions on the urine dipstick do you look at?” 81 percent of the registered nurses answered that they looked at leukocytes. 97 percent of the registered nurses looked at nitrite, while 48 percent of nurses also looked at blood. The result of question 7 showed that the registered nurses considered glucose (74 percent) and protein (62 percent) to be useful clinical indicators. The result of question 8 supports that the indicators are considered useful and that few registered nurses think that they should be removed (glucose 34 percent, leukocytes 0 percent, nitrite 5 percent, protein 45 percent and blood 5 percent).
To the question “Are you ever in doubt whether you have read the urine dipstick correctly?” 41 percent of the registered nurses, 37 percent of the assistant nurses, 100 percent of the assistants, and 89 percent of the students answered “yes”. The main reason for the uncertainty surrounding the reading of the urine dipstick is difficulties in distinguishing the colour nuances on the test strip (from 30 – 80 percent) (table 1).
Discussion
Knowledge on UTI
With regard to knowledge on important symptoms of UTI, the results from the questionnaire show that health personnel in the home care services have knowledge of the cardinal symptoms of UTI in the elderly. Such cardinal symptoms include confusion, deterioration of general condition, painful urination, bad-smelling urine and frequent urination (3). Our study suggests that the level of knowledge varies among the personnel groups, especially when it comes to assessment of important symptoms such as deterioration of general condition, painful urination and bad-smelling urine.
The results also show that symptoms that may be considered vague, such as delirium, poor appetite, pain localised over the symphysis, apathy and anorexia are not considered important signs of UTI, even though they are considered possible symptoms of UTI in the elderly (3, 21). For older patients signs of disease are typically vague and unclear (2, 3, 5). It is thus important that health personnel know that, for instance, poor appetite and apathy may also signal a somatic disease such as UTI.
We believe that these results may indicate that health personnel in the home care services do not have enough knowledge that diffuse geriatric symptoms may be a sign of disease and functional decline. If this is the case it is cause for worry, especially as we know that health personnel in the home care services are frequently alone with the patients. They may be the only visitor to the patient that day. The patients depend on all personnel having basic competence to act adequately to give sufficient and appropriate help (22-24).
Elderly patients are often overdiagnosed and overtreated due to vague symptoms and high prevalence of asymptomatic bacteriuria.
When it comes to acting adequately on symptoms of UTI, the results show that the majority of health personnel do react and act – either by contacting the nurse for help or by contacting physician, using urine dipsticks and/or collecting a urine sample. At the suspicion of UTI among older patients urine dipsticks are widely used (3), which the results in our study also support.
A Canadian study found that urine dipsticks are used when health personnel suspect UTI based on the typical symptoms of UTI, but also when the patient’s condition changes and at more vague symptoms such as weeping and increased anxiety (6). This seems to be the case for Norway as well, as the results show that the majority of the skilled health personnel use urine dipsticks at any sign of UTI. The same Canadian study showed that registered nurses observe the patient’s symptoms, prescribe urine cultures, use urine dipsticks and influence the initiation of antibiotics when they contact physician (6). They thus have a central role in the diagnosing of UTI in the elderly.
We have reason to believe that registered nurses in the home care services in Norway may also influence whether or not patients are diagnosed with UTI. The registered nurses are responsible for the nursing professional areas of treatment when they are on duty. Our questionnaire also shows that other health personnel act by contacting and consulting with registered nurses at the suspicion of UTI.
We thus see how important it is that all health personnel, and especially the registered nurses, have knowledge on explicit and vague symptoms of UTI in the elderly, in order to make the correct assessments and act accordingly. It is therefore unfortunate that the minority in our sample check vital signs like temperature and pulse. It is also worrisome that a relatively small number evaluate the patient’s general condition as part of a systematic assessment of the health of patients with possible UTI (5, 9, 10).
Practice for use and treatment of urine dipsticks and urine samples
When it comes to practice regarding the collection of urine samples in the home care services, the survey showed that the most common approach is to let patients urinate in bedpans, urine bags or urine containers under supervision, and that a small number ask the patients to collect the urine. It is an advantage to have health personnel present when patients urinate as it makes it possible to check whether the urine collection is done hygienically correct, to avoid contamination of the urine. As far as we know, there are no national guidelines for collecting urine samples in the home care services the way there are for hospitals (17).
We recommend such guidelines due to the varied context of “home care services”. The hygienic conditions and equipment available in hospitals are often lacking in the home care services (25). The hygiene principles in the procedure for collecting urine samples in hospital will necessarily also have to be followed in the home care services to avoid contaminated samples. It is important that health personnel make sure that urine is collected midstream. When collecting urine midstream the foreskin must be pulled back or the labia held apart. The genital area should be cleansed when the patient is urine incontinent (15, 17, 26).
Today there are no guidelines for collecting urine samples in the home care services.
The survey shows that health personnel use a urine dipstick in the patient’s home, in the office, base or zone where they work. By using the urine dipstick in the patient’s home, given that the urine is fresh, the urine is safeguarded against further bacterial growth caused by long storage, such as in the car. With guidance from competent personnel, using the urine dipstick in the office, base or zone would be more hygienic. However, the time of storage in room temperature from the sample has been collected till it has been tested, must not exceed two hours (18).
The factor analysis showed that the answer alternatives for the handling of urine samples (question 13) grouped around four factors, of which three factors measure inappropriate practice and one factor measures knowledge-based practice (17, 18). As figure 1 shows, the registered nurses are closer to maximum score on knowledge-based routines. There is, however, a way to go before all registered nurses attain full score on what is best practice:
- The urine sample must be stored in a cool place immediately upon the nurse’s arrival at the office or base
- The nurse must use urine from the same sample as tested with the urine dipstick in the urine sample sent for culture
- The nurses must have a set routine as to how to send urine samples
- The urine sample must be accompanied by information on the patient’s health condition
- After sending the sample the nurse must document the patient’s health condition, reactions on the dipstick, and when the sample was sent
Being as no national guidelines exist for urine sample collection procedure in the home care services, we recommend that such guidelines be developed. This may secure a more responsible, systematic and knowledge-based care to patients with UTI in the home care services.
The utility of and problems with urine dipsticks
A recently published literature review showed that for the elderly nitrite or leukocytes alone, or in combination, are useful urine dipstick indicators of bacteria in the urine (16). It is thus reassuring that the registered nurses in this survey mainly look at leukocytes and nitrite as indicators of UTI on urine dipsticks. The other indicators, glucose, protein and blood were considered useful indicators of other conditions, which is in line with urine dipsticks not being used as a diagnostic tool for UTI alone.
With regard to potential problems with urine dipsticks, all the assistants expressed uncertainty as to how to read the urine dipstick. Several of the assistant nurses and the registered nurses were similarly uncertain about such reading. In the main, health personnel are uncertain as to whether they have read the urine dipstick correctly as they cannot distinguish the colour nuances on the dipsticks.
Being as no national guidelines exist for urine sample collection procedure in the home care services, we recommend that such guidelines be developed.
The literature review mentioned above shows that there are great weaknesses related to using urine dipsticks as diagnostic tools for UTI in the elderly (16). Urine dipsticks give many false positives, and do not distinguish between actual bacteriuria and ASB, which shall not be treated (11). The literature review shows that in spite of these weaknesses we have no better diagnostic tool available.
In addition to the diagnostic weaknesses of urine dipsticks, this survey shows that there is great uncertainty associated with whether health personnel read the urine dipstick correctly. So it seems that a urine dipstick is not a reliable tool in the home care services. Supported by other research (27), this emphasises the need for a more reliable tool for diagnosing UTI. A new tool must compensate for the diagnostic weaknesses of urine dipsticks, but also for the uncertainty associated with subjective variations in reading and interpretation.
Conclusion
The purpose of this study was to map knowledge on UTI in health personnel in the home care services. We also wanted to find out how urine dipsticks and urine samples are used and collected, treated or read in the home care services. The purpose of the study was to identify points for possible improvement of practice. The survey suggests that practice may be improved on several issues: Health personnel in the home care services need more knowledge on the range of symptoms in older patients that may be related to UTI, so that more cases can be discovered and diagnosed earlier. At the same time it is important to think holistically as signs of disease in elderly patients may be both vague and diffuse, and signal other diseases than just UTI. Systematic, clinical observations are necessary for following the development of the patient’s health condition.
The collection of urine samples may be improved with regard to possible contamination of urine, routines for secure transportation, and documentation of necessary and sufficient information on the patient’s health condition. Problem areas for urine dipsticks seem to be the reading, but also a lack of knowledge regarding what reactions to look at, how much is enough urine, what are sources of contamination, and how long and how the urine may be stored. On the basis of these findings we recommend the development of national guidelines for the procedure for urine sample collection and use of urine dipsticks in the home care services in Norway. We also recommend research on and development of more reliable and patient friendly diagnostic tools for UTI adapted to the older patient groups, especially for patients who use urine absorbent products where collecting urine samples is difficult.
References
1. Daatland SO, Veenstra M. Komparative perspektiver på omsorgstjenestene – Norge i en internasjonal sammenheng. I: Daatland SO, Veenstra M (red.). Bærekraftig omsorg? Familien, velferdsstaten og aldringen av befolkningen NOVA-rapport nr. 2/2012. Oslo: Norsk institutt for forskning om oppvekst, velferd og aldring (NOVA); 2012. p. 175–86.
2. Beckett CL, Harbarth S, Huttner B. Special considerations of antibiotic prescription in the geriatric population. Clinical Microbiology and Infection 2015;21(1):3–9.
3. Wyller TB. Geriatri : en medisinsk lærebok. Oslo: Gyldendal Akademisk. 2015.
4. Statistisk Sentralbyrå. Kommunale helse- og omsorgstjenester 2014 Statistikk om tjenester og tjenestemottakere Rapporter 2015/42. Available at: http://ssb.no/helse/artikler-og-publikasjoner/kommunale-helse-og-omsorgstjenester-2014. (Downloaded 15.10.2015).
5. Nazarko L. Treating the patient or the labstick? Urinary infections in older people. British Journal of Healthcare Assistants 2008;2(7):323–26.
6. Walker S, McGeer A, Simor A, Armstrong- Evans M, Loeb M. Why are antibiotics prescribed for asymtomatic bactiuria in institutionalized elderly people? A qualitative study of physicians' and nurses' perceptions. Canadian Medical Association Journal 2000;163(3):273–7.
7. Pettersson E, Vernby A, Molstad S, Lundborg CS. Infections and antibiotic prescribing in Swedish nursing homes: a cross-sectional study. Scand J Infect Dis. 2008;40(5):393–8.
8. Bevridge LA, Davey PG, Phillips G, McMurdo ME. Optimal management of urinary tract infections in older people. Clinical Interventions in Aging 2001;6:173–80.
9. McNulty C. Managing asymptomatic bacteriuria in the elderly. Practice Nursing 2014;25(1):11–5.
10. Nazarko L. Recurrent urinary tract infection in older women. Nurse Prescribing 2014;12(12):608–13.
11. Helsedirektoratet. Nasjonale faglige retningslinjer for antibiotikabruk i primærhelsetjenesten. Available at: https://helsedirektoratet.no/retningslinjer/nasjonal-faglig-retningslinje-for-antibiotikabruk-i-primerhelsetjenesten. (Downloaded 08.11.2016).
12. High K, Schmader KE, Sokol HN. Evaluation of infection in the older adult. Available at: http://www.uptodate.com/contents/evaluation-of-infection-in-the-older-adult?source=search_result&search=infection+elderly&selectedTitle=1%7E13#H1498008. (Downloaded 14.04.2016).
13. Fekete T, Hooton TM, Calderwood SB, Bloom A. Approach to the adult with asymptomatic bacteriuria. Available at: http://www.uptodate.com/contents/approach-to-the-adult-with-asymptomatic-bacteriuria. (Downloaded 01.05.2015).
14. Scottish Intercollegiate Guidelines Network. Management of suspected bacterial urinary tract infection in adults SIGN guideline 88. Available at: http://www.sign.ac.uk/guidelines/fulltext/88/recommendations.html. (Downloaded 20.04.2016).
15. Dolan VJ, Cornish NE. Urine specimen collection: How a multidisciplinary team improved patient outcomes using best practices. Urologic Nursing. 2013;33(5):249–56.
16. Eriksen SV, Bing-Jonsson PC. Kan vi stole på urinstiks? Available at: https://sykepleien.no/forskning/2016/09/kan-ikke-stole-blindt-pa-urinstiks. (Downloaded 04.11.2016).
17. Kunnskapssenteret. Fagprosedyre: Urinprøve til bakteriologisk undersøkelse. Available at: http://www.helsebiblioteket.no/fagprosedyrer/ferdige/urinprove-til-bakteriologisk-undersokelse. (Downloaded 08.11.2016).
18. Noklus. Urinprøve til mikrobiologisk undersøkelse. Available at: http://www.noklus.no/Portals/2/Forskning%20og%20utvikling/Bruk%20av%20urinprover%20hos%20eldre%20-%20for%20allmennlege_%20Noklus%202016.pdf. (Downloaded 08.11.2016).
19. John OP, Benet-Martinez V. Measurement: Reliability, Construct Validation, and Scale Construction. In: Reis HT, Judd CM (ed.). Handbook of Research Methods in Social and Personality Psychology. 1. Cambridge: Cambridge University Press. 2000. p. 33–69.
20. Field A. Discovering statistics using IBM SPSS statistics. Los Angeles: SAGE. 2013. 915 p.
21. Rowe TA, Juthani-Mehta M. Diagnosis and management of urinary tract infection in older adults. Infect Dis Clin North Am. 2014;28(1):75–89.
22. Tønnesen S. Faglige forutsetninger for forsvarlighetsbegrepet. Oslo: Sykepleien Forskning. 2013;2(8):148–55. Available at: https://sykepleien.no/forskning/2013/04/faglige-forutsetninger-forsvarlighetsbegrepet. (Downloaded 04.11.2016).
23. Bing-Jonsson PC, Bjørk IT, Foss C. The competence gap in community elderly care: Imbalance between expected and actual nursing staff competence. Nordic Journal of Nursing Research 2015.
24. Bing-Jonsson PC, Hofoss D, Kirkevold M, Bjørk IT, Foss C. Sufficient competence in community elderly care? Results from a competence measurement of nursing staff. BMC Nursing 2016;15(5).
25. Fjørtoft A-K. Hjemmesykepleie : ansvar, utfordringer og muligheter. 2. ed. Bergen: Fagbokforlaget. 2012.
26. Wisnes C. Urinprøvetaking – kunnskapsbasert eller tilfeldig? Oslo: Sykepleien. 2002;90(6):58–61. Available at: https://sykepleien.no/forskning/2009/03/urinprovetaking-kunnskapsbasert-eller-tilfeldig. (Downloaded 12.11.2016).
27. Hartley S, Valley S, Kuhn L, Washer LL, Gandhi T, Meddings J et al. Inappropriate testing for urinary tract infection in hospitalized patients: An opportunity for improvement. Infect Control Hosp Epidemiol. 2013;34(11):1204–7.










Comments