The CPOT – a tool for pain assessment for intensive care patients
Intensive care patients often suffer from undertreated pain. A pain assessment tool in a Norwegian version may increase the quality of patient treatment.
Introduction: Research shows that intensive care patients experience pain both at rest and during procedures. Critically ill patients frequently have impaired ability to communicate pain and discomfort, making pain assessment and pain management challenging. Systematic pain assessment with valid tools is essential for good pain management. The Critical-Care Pain Observation Tool (CPOT) is a pain assessment tool with four domains.
Objective: To translate The Critical-Care Pain Observation Tool (CPOT) and to examine the tool's validity and reliability.
Method: The study has a descriptive quantitative design. The CPOT was first translated into Norwegian using an internationally recommended translation process. Six intensive care nurses were given a one-hour training session in the use of the CPOT, and an instruction video was used to achieve a common understanding of the CPOT scoring system. Independently, two intensive care nurses (in pairs) assessed and scored the patient’s pain expression, using the CPOT, before and during a turning procedure. A total of 182 (91 pairwise) CPOT assessments were performed of 18 intensive care patients on mechanical ventilation. The Norwegian version of the CPOT was examined for discriminant validity by comparing the nurses’ scores before and during the turning procedure. Interrater reliability was evaluated by analysing agreement between the two nurses’ observations.
Result: The Norwegian version of the CPOT demonstrated good discriminant validity and moderate to excellent interrater reliability. The domain "facial expressions" showed the lowest agreement between the nurses.
Conclusion: The Norwegian version of the CPOT appears to be a valid and reliable pain assessment tool for ICU patients on mechanical ventilation.
Research shows that intensive care patients frequently suffer from undertreatment of pain (1–5). Undertreatment of pain can have serious physical and psychological consequences (6–8). The golden standard for pain assessment is the patient’s own description of pain (9, 10). However, the intensive care patient’s impaired ability to communicate entails that the patient may experience pain without being able to express it in a way that health care personnel comprehend (4, 7, 11). Patients’ inability to self-report pain hinders effective pain management.
Systematic pain assessment with valid tools has proven essential to good pain treatment and may be used as a quality indicator of clinical practice (12, 13). There are several tools for assessing pain in adult intensive care patients, but according to international clinical guidelines (14), The Behavior Pain Scale (BPS) (15) and The Critical-Care Pain Observational Tool (CPOT) (16, 17) have the highest validity and reliability. Rijkenberg et al. compared the CPOT and the BPS and concluded with a preference for the CPOT, due to better discriminant validity, meaning the tool measures pain better when the intensive care patient is assumed to have pain (19).
In the international clinical guidelines, Barr et al. refer to the testing of the two tools’ psychometric characteristics (measurement characteristics, user friendliness, the tool’s validity and reliability, etc.). The CPOT appeared to be somewhat better, but both the CPOT and the BPS are equally recommended (14). The guidelines recommend that the CPOT and the BPS be translated and validated into more languages (14). The BPS is translated into Norwegian and tested for reliability by Olsen and Rustøen (18). Translating the CPOT into Norwegian and testing it for validity and reliability will thus be an advantage. The aim of the study was to translate and investigate the validity and reliability of the Norwegian version of the CPOT in a general intensive care unit.
Method
The study had a descriptive quantitative design. The pain assessment tool CPOT was translated into Norwegian and examined for discriminant validity and interrater reliability. Discriminant validity refers to whether the CPOT measures pain when pain is present and does not measure pain when pain is not present. Interrater reliability measures the degree of agreement between two intensive care nurses’ CPOT scores.
Study setting and sample
The study was performed in a general intensive care unit at a Norwegian university hospital from April to September 2014. The majority of the unit’s patients were mechanically ventilated, received continuous analgesia (pain medication) and sedation (tranquilisers/sleep medication), and had impaired ability to communicate. Of a total 100 nurses in the unit, 95 were intensive care nurses.
The nurses daily assess the intensive care unit patients’ level of consciousness using the Richmond Agitation and Sedation Scale (RASS) (14, 20). The RASS measures agitation and sedation level, the score ranging from +4 to –5, where a score of 0 indicates an awake and adequate patient. Scores from –1 to –5 indicate an increasingly sedated patient, and scores from +1 to +4 indicate an increasingly irritable and agitated patient.
The inclusion criteria for the patients in the study were a stay in the intensive care unit of >24 hours, ≥18 years, and being mechanically ventilated. Patients given muscle relaxants were excluded from the study. Muscle relaxants effectively stop all grimacing and peripheral muscle movements, and the CPOT cannot be used in pain assessments of patients when such medication is administered. One of the authors and one intensive care nurse not directly involved in patient care included patients as they were admitted to the unit. A total of 18 patients were included in the study: seven men and eleven women aged 31–84 years, with a median age of 51 years. The patients were divided into three diagnosis categories:
- thoracic surgical and cardiovascular patients
- gastrosurgical and gastromedical patients
- neurosurgical and neurological patients
The inclusion criteria for the nurses were being experienced intensive care nurses with a minimum of five years seniority, who had worked some shifts together, and were willing to participate in the study. The six nurses consenting to participation had between five and 23 years of experience as intensive care nurses, with a median of 16 years. The nurses, in pairs, performed 91 CPOT scorings of the 18 included patients.
Translation of the CPOT
The English original version of the CPOT (16) and accompanying instructions were translated into Norwegian in accordance with an internationally recommended translation process, in which both cultural and linguistic adaptations are emphasised (22). The translation process contains ten steps: preparation, forward translation, reconciliation, back translation, review, harmonization, cognitive debriefing, review of cognitive debriefing results and finalisation, proofreading and final report.
Patients unable to self-report pain constitute a challenge to effective pain relief.
In step one, preparation, the CPOT copyright holder, Céline Gélinas, gave written permission for a Norwegian translation on certain conditions. The translation should build on the English original version, and source and references should be included in all CPOT documents. Two intensive care nurses with good knowledge of Norwegian and English, and one of the authors, translated the CPOT independently. After several adaptations they agreed on a translation. A professional translator back translated the Norwegian version into English. This version of the CPOT was reviewed by the three initial translators and sent to Gélinas, who approved the version without comments.
We compared the English translation with the Norwegian version to ensure that the translation harmonized with the original text, i.e. had the same content as the original tool. Five experienced intensive care nurses unfamiliar with the CPOT tested the Norwegian version. The feedback was that it was understandable and practicable in use, and consequently, we did not change anything after the review. The final version of the CPOT was proofread several times by persons with good knowledge of Norwegian. Each step of the process was described in a table that constituted the final report for the translation work.
The Critical-Care Pain Observation Tool (CPOT)
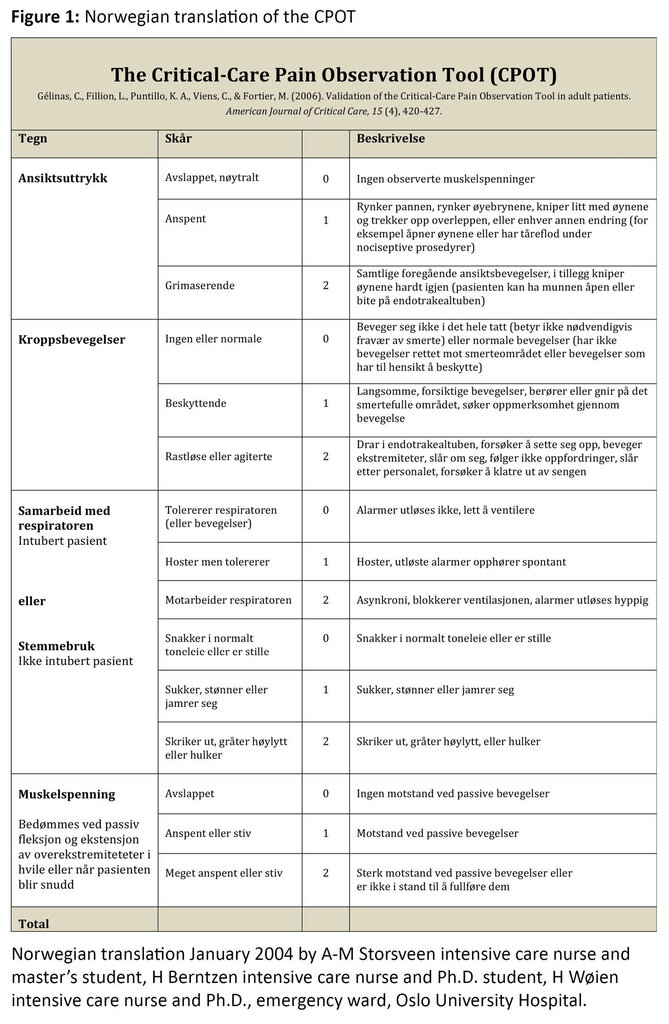
The pain assessment tool, CPOT is based on four domains: the patient’s facial expressions, body movements, compliance with ventilator (or voice use for non-intubated patients), and muscle tension (16). Each domain has a possible score of 0 to 2. The total score can vary between 0 and 8, where 0 indicates no pain behaviour and 8 indicates clear signs of pain behaviour (Figure 1).
The intensive care nurses were given a one-hour training session in the use of the CPOT. The training included a thorough presentation of the tool, how to score the behavioural components in CPOT, and how to fill in the registration form. The training session also included a practical exercise in which the nurses scored CPOT based on four “patient situations”, presented in an instruction video.
Data collection
The six intensive care nurses assessed, in pairs and simultaneously, the pain expression of a patient during a turning procedure. We chose the procedure of turning the patient as this constitutes a painful procedure for intensive care patients (2). The patient was first observed for one minute at rest in accordance with the written instructions. The nurses next observed the patient being turned. Each nurse filled in the CPOT form independently, giving the patient a score for each of the four behavioural domains both at rest and during turning (16).
We used the nurses’ CPOT score to analyse differences between the score at rest and during turning (discriminant validity), and to analyse agreement between the scores of the nurse pairs (interrater reliability).
The six intensive care nurses performed a total of 182 CPOT scorings (91 paired scores) for the 18 patients included. Each patient was scored with the CPOT between one and 17 times with a median of three, dependent on length of stay in the intensive care unit. The six nurses scored between eight and 55 times with a median of 29. To reduce the possibility of the nurses becoming familiar with the patient’s pain behaviour, a patient was never scored more than four times by the same pair of nurses.
The nurses documented the patients’ RASS level at each CPOT scoring in order to assess the included patients’ level of sedation. The majority of the patients had a RASS score indicating that they were moderately to deeply sedated, with a median RASS score of –3 (+1 to –5).
Analysis
Data were analysed using the statistics programmes IBM Statistical Package for the Social Sciences (SPSS) version 18 and the computer programme Vassar Stats (23). We used similar analysis as in earlier studies in order to compare the results (16, 24, 25). The CPOT can be regarded as having both categorical and continuous data, which is significant for the choice of analysis method (26). We used the median for categorical data at the ordinal level, while estimating mean values for continuous data (27).
Discriminant validity for the CPOT was analysed for differences in CPOT scores at rest and during turning within all domains: facial expressions, body movements, compliance with ventilator, and muscle tension. These categorical data were analysed at the ordinal level with Wilcoxon signed-rank test. To estimate discriminant validity of continuous data at the interval level, we compared the mean total score at rest with mean total score during turning by using paired t-test. For both analyses, the level of significance was set at p >0.05.
Two different methods of analysis were used to measure interrater reliability (IRR) for the CPOT: weighted kappa for categorical data and intraclass correlation coefficient (ICC) for continuous data. Nurses assessing the same patient with equal CPOT scores yielded a perfect IRR. Weighted kappa values at 0.81–1.0 indicate excellent agreement, 0.61–0.80 good agreement, 0.41–0.60 moderate agreement, 0.21–0.40 slight agreement and £0.21 poor agreement (28). ICC greater than 0.75 indicates fair agreement, 0.50–0.75 moderate agreement, and <0.5 poor agreement (29). For both ICC and weighted kappa 1.0 indicates perfect agreement, while 0 indicates no agreement.
Ethical considerations
We have followed the ethical guidelines of the Declaration of Helsinki (30). We deemed the study subject to approval by the Regional Committees for Medical and Health Research Ethics (REC), as we wished to register patient data and assess patients’ pain experiences using a new pain assessment tool. The study was approved by REC (2014/464), and we gained permission from the unit leader at the unit in question to perform the study. The majority of the included intensive care patients lacked competence to consent as a result of their health condition. The patients’ families were thus informed and asked to consent, orally and in writing. In one case the patient consented following oral and written information. The six intensive care nurses were also informed, asked to participate, and gave their written
Results
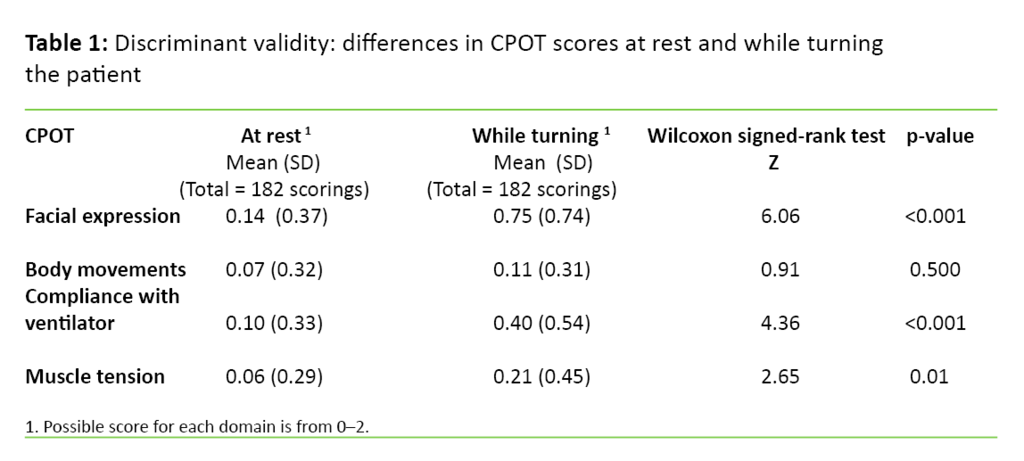
First we present the results of discriminant validity and next, the results of interrater reliability of the CPOT. Discriminant validity was investigated by comparing the nurses’ CPOT scores at rest with the CPOT scores during turning. Table 1 shows mean values, standard deviation and the results of the Wilcoxon signed rank test analysis at the domain level. There were statistically significant differences in the scores between rest and turning within facial expression, compliance with the ventilator, and muscle tension, but not within the domain body movement.
The mean value of the CPOT total score was 0.35 (SD 0.95) at rest and 1.50 (SD 1.20) during turning. There was a statistically significant difference between rest and turning (paired t-test = 7.945, d.f. = 90 and p value <0.001). The difference indicates that the CPOT measures pain when pain is present.
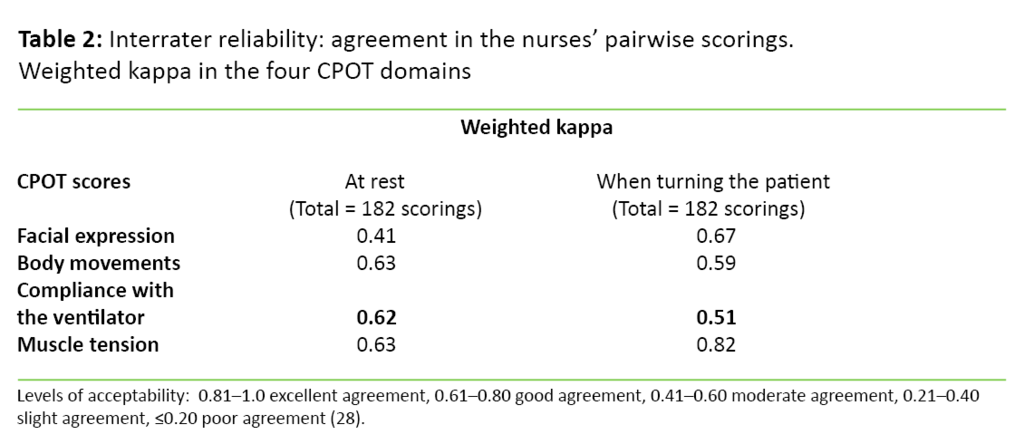
The CPOT interrater reliability was investigated by analysing agreement between scores at rest and during turning for each pair of nurses for each domain. The data were analysed with weighted kappa. The results showed that weighted kappa varied from 0.41 to 0.82, i.e. from moderate to excellent agreement (Table 2).
Agreement for the CPOT total mean score was analysed with intraclass correlation coefficient (ICC). The result showed good agreement at rest with an ICC at 0.80 and confidence interval (CI) of 0.71–0.86, and moderate agreement during turning with an ICC at 0.68 and CI of 0.54–0.77.
Discussion
The result of the study showed a significant difference between total CPOT mean score at rest and during turning. This difference indicates that the CPOT measures pain when pain is present. The result indicates that the Norwegian version of the CPOT has good discriminant validity, which corresponds with results from previous studies (16, 24, 25, 31, 32). Furthermore, the analysis of CPOT scores within each domain at rest and during turning showed significant differences within all domains, with the exception of the domain body movement. This exception may be explained by that patients in this study were relatively deeply sedated; they were given both analgesics and sedatives and were not very mobile.
Facial expression seems to be the most important domain for identifying pain, and also the domain with the lowest reliability.
The analysis of ICC, used to measure interrater reliability, showed excellent agreement between the nurses’ total CPOT mean score at rest and moderate agreement during turning. The results are in accordance with results from similar studies (31, 33). That the agreement between the nurses’ scores was better at rest than during turning, may, in our study, be explained by the patients being sedated. The most frequent CPOT score at rest was 0, while there was more variation in the patient’s pain behaviour during turning, which caused greater variation in the CPOT score.
Another explanation for the moderate agreement may be the variation that arises when as many as six nurses assessed the patients. This may reflect reality better than studies that show somewhat better agreement but have only two nurses performing all the assessments (16, 24). Stilma et al. report a lower agreement than our study (34). She explained the results partly by that many nurses performed the assessments, but she also pointed to the transferability of an intensive care practice that represents reality.
Assessment training useful
Polit and Beck claim that the most efficient way to increase reliability in this kind of study is to train the participants that perform the assessments (21). This is in line with recommendations from similar studies that emphasise that training the nurses is crucial to the tool’s reliability and validity in practice (25, 33). The six nurses in the study had identical training in the use of the tool. In connection with the instruction video the nurses were able to score patient situations and have a discussion in order to arrive at a common understanding of the various domains. More practice in scoring the tool and a better common understanding may have resulted in improved agreement in the scores also during turning.
We have not found any earlier comparable studies that have investigated agreement (interrater reliability) between the nurses’ CPOT score in each domain (16, 24, 25, 31, 32). The analysis of weighted kappa at domain level showed moderate to excellent agreement. Facial expression was the domain with the lowest agreement level between the nurses’ score at rest, with weighted kappa value of 0.41. A possible explanation is that the three response alternatives for facial expressions may be hard to distinguish. In the instructions accompanying the CPOT scale, “tense” (CPOT score 1) and “grimacing” (CPOT score 2) are accompanied by descriptions that may be hard to reach a common understanding on.
Facial expression most important for assessment of pain
Another study investigated interrater reliability at the domain level of the Behavioral Pain Scale (BPS) (18). Also in this study, facial expression showed the lowest agreement at rest as well as during turning. All known pain scales based on behaviour include facial expression as one of the domains, and the patient’s facial expression is considered the most important component (35). Rahu and colleagues claim that facial expression may be a valid alternative to self-report of pain in intensive care patients (36).
Facial expression seems to be the most important domain for identifying pain, at the same time as it is the domain with the lowest reliability. Gélinas, Arbor and Keane have all questioned whether the domain facial expression in the CPOT should be developed to be more sensitive to minimize the risk for underestimating the patient’s pain (25, 35). The need for further development of the domain facial expression is supported by the results from this study. The domain muscle tension showed excellent agreement with a weighted kappa of 0.82. An explanation for this may be that the domain muscle tension in the CPOT has a brief description, and that the patient’s muscular resistance in passive movements is relatively easy to notice when turning a patient.
The intensive care nurse should always have in mind that pain is frequently present in intensive care patients.
In most of the CPOT assessments the patients were estimated with low scores with a total CPOT mean score of 0.35 at rest and 1.5 during turning. The low CPOT scores may be explained by the patients generally being sedated to a sedation level that entails movement in response to being addressed, but without establishing eye contact (RASS = –3). Gélinas and Arbor suggested that sedated patients have a significantly lower CPOT score both at rest and during procedures compared to conscious patients (35). In earlier studies with more awake patients, the CPOT has proved to be more in line with the patient’s self-reported pain with a total CPOT mean score between 2 to 3 (31, 32, 33).
Study limitations
One limitation of the study is that the criterion validity, i.e. a comparison of the nurse’s CPOT score and the patient’s own assessment of pain, was not investigated. However, very few patients were able to use Numeric Rating Scale (NRS), and as a result we decided not to investigate the criterion validity in this study. The decision was also justified by referring to the studies by Keane and Nürnberg Damström et al., in which only a few patients were able to communicate their pain, and consequently the criteria validity could not be evaluated properly due to insufficient data collection (24, 25). In other studies with more awake patients the CPOT has turned out to have high criterion validity in relation to the patients’ self-report of pain (16, 37).
Another limitation of the study was the repeated assessment of the patients due to the limited number of patients included. However, the patient’s sedation level may have varied at the various incidences of assessment and thereby have created a natural variation in pain and pain behaviour in the same patient. The choice to assess patients several times may also be defended with that the nurses’ scores are the basis for the analysis. A further limitation of the study is that it is performed in only one intensive care unit, and that all assessments were performed by intensive care nurses. The generalizability of the study may be limited as many intensive care units have other patient categories and fewer intensive care nurses.
Conclusion
The Norwegian version of the CPOT seems to be a valid and reliable pain assessment tool for mechanically ventilated intensive care patients. The CPOT can be implemented in intensive care units to systematically assess, document and evaluate intensive care patients’ pain. Through several studies the CPOT proves to be a well validated and reliability tested tool. Nevertheless there is a need for further research on the Norwegian version of CPOT on other groups of intensive care patients. Further research should also be directed towards investigating whether the four domains in CPOT may be made more sensitive to pain particularly concerning the domain facial expression.
The intensive care nurse should be aware of the frequent presence of pain in the intensive care patient, especially in connection with procedures. A low score on pain behaviour in a deeply sedated patient does not necessarily indicate that the patient is not in pain (38, 39). If CPOT could give an indication of whether an intensive care patient has pain or not, the tool contributes to increasing the quality of the patient treatment, despite its limitations.
Thanks to the management and colleagues at General intensive care unit 1, Rikshospitalet, Oslo University Hospital (RH OUS), who made it possible to carry out this study.
We also want to thank Helene Berntzen, intensive care nurse and PhD student at the Postoperative and intensive care unit, OUS, and Hilde Wøien, intensive care nurse PhD at the General intensive care unit 1, for reading the manuscript and contributing with good suggestions.
References
1. Puntillo K. Pain experiences of intensive care unit patients. Heart & Lung: the journal of critical care 1990;19(5):526–33.
2. Puntillo KA, White C, Morris AB, Perdue ST, Stanik-Hutt J, Thompson CL et al. Patients’ perceptions and responses to procedural pain: results from Thunder Project II. American Journal of Critical Care 2001;10(4):238–51.
3. Sessler CN, Varney K. Patient-focused sedation and analgesia in the ICU. CHEST (Journal) 2008;133(2):552–65.
4. Payen J-F, Bosson J-L, Chanques G, Mantz J, Labarere J. Pain assessment is associated with decreased duration of mechanical ventilation in the intensive care unit: a post Hoc analysis of the DOLOREA study. Anesthesiology 2009;111(6):1308–16.
5. Puntillo KA, Max A, Timsit J-F, Vignoud L, Chanques G, Robleda G et al. Determinants of procedural pain intensity in the intensive care unit. The Europain® Study. American Journal of Respiratory and Critical Care Medicine 2014;189(1):39–47.
6. Hamill-Ruth RJ, Marohn ML. Evaluation of pain in the critically ill patient. Critical Care Clinics 1999;15(1):35–54.
7. Chanques G, Jaber S, Barbotte E, Violet S, Sebbane M, Perrigault P-F et al. Impact of systematic evaluation of pain and agitation in an intensive care unit. Critical Care Medicine 2006;34(6):1691–99.
8. Barr J, Pandharipande PP. The pain, agitation, and delirium care bundle: synergistic benefits of implementing the 2013 pain, agitation, and delirium guidelines in an integrated and interdisciplinary fashion. Critical Care Medicine 2013;41(9 Suppl 1):99–115.
9. Merskey H, Bogduk N. Classification of chronic pain: descriptions of chronic pain syndroms and definitions of pain terms. Seattle: IASP Press. 1994. XV:222
10. Breivik H, Borchgrevink P, Allen S, Rosseland L, Romundstad L, Hals EB et al. Assessment of pain. British Journal of Anaesthesia 2008;101(1):17–24.
11. Alderson S, McKechnie S. Unrecognised, undertreated, pain in ICU: Causes, effects, and how to do better. Open Journal of Nursing 2013;3(1).
12. Skrobik Y, Ahern S, Leblanc M, Marquis F, Awissi DK, Kavanagh BP. Protocolized intensive care unit management of analgesia, sedation, and delirium improves analgesia and subsyndromal delirium rates. Anesthesia & Analgesia 2010;111(2):451–63.
13. Wøien H, Bjørk IT. Intensive care pain treatment and sedation: Nurses’ experiences of the conflict between clinical judgement and standardised care: An explorative study. Intensive and Critical Care Nursing 2013;29(3):128–136.
14. Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Critical Care Medicine, 2013;41(1):263–306.
15. Payen J-F, Bru O, Bosson J-L, Lagrasta A, Novel E, Deschaux I et al. Assessing pain in critically ill sedated patients by using a behavioral pain scale. Critical Care Medicine 2001;29(12):2258–63.
16. Gélinas C, Fillion L, Puntillo KA, Viens C, Fortier M. Validation of the critical-care pain observation tool in adult patients. American Journal of Critical Care 2006;15(4):420–27.
17. Gélinas C, Tousignant-Laflamme Y, Tanguay A, Bourgault P. Exploring the validity of the bispectral index, the Critical-Care Pain Observation Tool and vital signs for the detection of pain in sedated and mechanically ventilated critically ill adults: a pilot study. Intensive and Critical Care Nursing 2011;27(1):46–52.
18. Olsen BF, Rusten T. Er den norske versjonen av «Behavioral Pain Scale» pålitelig og brukervennlig? Oslo: Sykepleien Forskning. 2011;(3). Available at: https://sykepleien.no/forskning/2011/10/er-den-norske-versjonen-av-behavioral-pain-scale-palitelig-og-brukervennlig. (Downloaded 10.11.2016).
19. Rijkenberg S, Stilma W, Endeman H, Bosman R, Oudemans-van Straaten H. Pain measurement in mechanically ventilated critically ill patients: Behavioral Pain Scale versus Critical-Care Pain Observation Tool. Journal of Critical Care 2015;30(1):167–72.
20. Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O'Neal PV, Keane KA et al. The Richmond Agitation–Sedation Scale: validity and reliability in adult intensive care unit patients. American journal of Respiratory and Critical Care Medicine 2002;166(10):1338–44.
21. Polit DF, Beck CT. Nursing research: generating and assessing evidence for nursing practice. Philadelphia, Pa.: Wolters Kluwer Health. 2012. XIV.
22. Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value In Health 2005;8(2):94–104.
23. VassarStats. Kappa as a Measure of Concordance in Categorical Sorting. Available at: http://vassarstats.net/kappa.html. (Downloaded 01.10.2014).
24. Nürnberg Damström D, Saboonchi F, Sackey P, Björling G. A preliminary validation of the Swedish version of the critical‐care pain observation tool in adults. Acta Anaesthesiologica Scandinavica 2011;55(4):379–86.
25. Keane KM. Validity and reliability of the Critical Care Pain Observation Tool: A replication study. Pain Management Nursing 2013;14(4):216–25.
26. Røislien J, Frøslie KF. Tall forteller: hvordan bruke tall til å finne ut om verden er slik du tror den er. Oslo: Gyldendal Akademisk. 2013.
27. Bjørndal A, Hofoss D. Statistikk for helse- og sosialfagene. Oslo: Gyldendal Akademisk. 2010.
28. Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med 2005;37(5):360–3.
29. Fleiss JL, Cohen J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educational and Psychological Measurement. 1973
30. WMA Declaration of Helsinki. Available at: http://www.wma.net/en/30publications/10policies/b3/index.html. (Downloaded 09.11.2015).
31. Echegaray-Benites C, Kapoustina O, Gélinas C. Validation of the use of the Critical-Care Pain Observation Tool (CPOT) with brain surgery patients in the neurosurgical intensive care unit. Intensive and Critical Care Nursing 2014;30(5):25765.
32. Li Q, Wan X, Gu C, Yu Y, Huang W, Li S et al. Pain assessment using the Critical-Care Pain Observation Tool in Chinese critically ill ventilated adults. Journal of Pain and Symptom Management 2014;48(5):975–82.
33. Gélinas C, Johnston C. Pain assessment in the critically ill ventilated adult: validation of the Critical-Care Pain Observation Tool and physiologic indicators. The Clinical Journal of Pain 2007;23(6):497–505.
34. Stilma W, Rijkenberg S, Feijen M H, Maaskant M J, Endeman H. Validation of the Dutch version of the Critical-Care Pain Observation Tool. Nursing in Critical Care. 2015. Available at: https://www.altmetric.com/details/4920826. (Downloaded 01.02.2015).
35. Gélinas C, Arbour C. Behavioral and physiologic indicators during a nociceptive procedure in conscious and unconscious mechanically ventilated adults: similar or different? Journal of Critical Care 2009;24(4):628-e7.
36. Rahu MA, Grap MJ, Cohn JF, Munro CL, Lyon DE, Sessler CN. Facial expression as an indicator of pain in critically ill intubated adults during endotracheal suctioning. American Journal of Critical Care 2013;22(5):412–22.
37. Gélinas C, Harel F, Fillion L, Puntillo KA, Johnston CC. Sensitivity and specificity of the critical-care pain observation tool for the detection of pain in intubated adults after cardiac surgery. Journal of Pain and Symptom Management 2009;37(1):58–67.
38. Gélinas C, Puntillo KA, Joffe AM, Barr J (red.). A Validated approach to evaluating psychometric properties of pain assessment tools for use in nonverbal critically ill adults. Seminars in Respiratory and Critical Care Medicine 2013;34(2):153–68.
39. Tietize K. Pain control in the critically ill adult patient. Uptodate 2013. Available at: https://www.uptodate.com/contents/pain-control-in-the-critically-ill-adult-patient. (Downloaded 10.10.2014).










Comments