Fewer cardiac arrests are registered
Health personnel are instructed to register cardiac arrests in The Norwegian Cardiac Arrest Registry. Still, only one in three patients with cardiac arrest in the intesive care ward is registered.
Background: Reported prevalence and survival after cardio-pulmonary resuscitation (CPR) in intensive care units (ICU) vary, but no Norwegian studies on this topic seem to have been published.
Objective: To report prevalence, survival and registration after CPR.
Method: A cross-sectional study was performed in 14 ICU departments at Oslo University Hospital in 2013. Diagnoses and procedure codes for cardiac arrest (CA), ventricular arrhythmias and CPR were collected from patient administrative systems. Diagnoses and procedure codes confirmed in the medical records were included in the study sample, and incidences further compared with the internal quality registry for cardiac arrest.
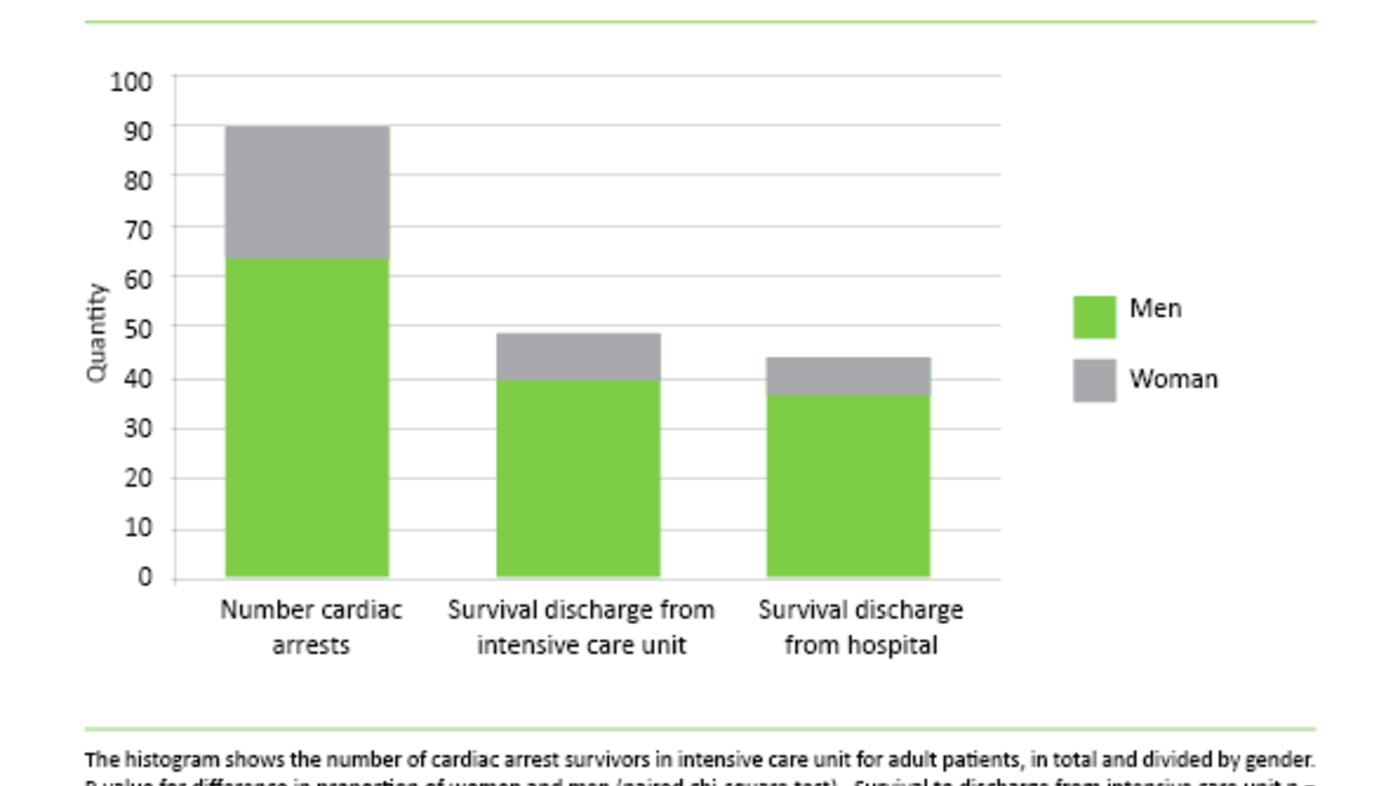
Results: Among 15 101 admissions to the ICU, there were 117 (0.8 %) events of CPR on 99 individual patients. Of 91 adults, 64 (70 %) were men, the mean age was 64 years and 44 (48 %) survived to discharge. The survival was significantly lower for women than for men: 8 (30 %) women survived, and 36 (56 %) men, (p = 0.023). Only 32 (32 %) of the patients were registered in our in-hospital CA registry.
Conclusion: CPR was conducted in about 1 of 100 admissions to the ICU. About half of the patients survived to discharge after CPR. One third of these patients were registered in the in-hospital quality registry for CA. Compared to similar studies from other countries, the prevalence and registration of CPR were low, while the survival rate was high.
Cardiac arrest is defined as cases where ”patients without vital signs … are either treated with defibrillation of a lethal arrhythmia or need cardiopulmonary resuscitation to survive” (1). Cardiac arrest is feared among patients in hospital, also in intensive care units. Due to comorbidity and organ failure (2), patients in intensive care wards are already more prone to cardiac arrest and have poor prognosis in spite of performed cardiopulmonary resuscitation (CPR). Intensive care patients are continually monitored and surrounded by high level medical and nursing expertise. Cardiac arrest can thus be discovered and treated quickly (3). International research shows that the prevalence of CPR among intensive care patients varies between 0.6 – 8 per cent per hospital admission (4-7), while survival following CPR varies between 0-79 per cent (4). There are no studies of prevalence and survival following cardiac arrest in Norwegian intensive care patients.
Important with complete registering
Quality registries are tools for evaluating activity and for planning and implementing quality improvement. The establishment of internal quality registries and collection of data for such registries are authorised by The Health Personnel Act § 26 (8). The Norwegian Cardiac Arrest Registry serves under the Norwegian Cardiovascular Disease Registry, a national quality registry with its own regulations (The Health Registry Act §§ 8, 11) (9). Cardiac arrest is thus a condition for which nominal reporting to a registry is mandatory in line with cancer and births. An internal quality registry is a prerequisite for the reporting of data to the national registry. The internal quality registry for cardiac arrest in hospitals opened January 1 2013 and followed upon earlier local initiatives in the hospitals that now make up Oslo University Hospital (OUS).
For the registries to fulfil their function, the registering of cardiac arrest must be complete. The comprehensiveness of the reporting must be controlled to establish whether the registries fulfil this function. A Swedish study of 103 quality registries points to that recent implementation of a registry may give incomplete reporting (10). Knowledge of the quality of and the level of reporting in registries is important to nurses who want to use the registries for evaluation, development and improvement of practice. The purpose of the study was thus to take a closer look at prevalence and registration practice of cardiac arrest in the intensive care units at OUS in order to validate and improve the registry. We wanted to contribute with knowledge of the usefulness of carrying out this type of audit of a quality registry.
Research questions and method
We formulated three research questions to respond to the purpose of the study:
- What is the prevalence of CPR?
- How many patients survive cardiac arrest in the intensive care wards?
- To what extent is performed CPR registered in the intensive care units’ patient journals, patient administrative coding and the internal cardiac arrest registry?
The study had a cross-sectional design and we examined data for all of 2013 at the 14 intensive care units at OUS that offer ventilator treatment to investigate the prevalence of cardiac arrest. We collected data from wards at all four somatic OUS localisations: Aker Hospital, The Norwegian Radium Hospital, Rikshospitalet and Ullevål Hospital. The intensive care units all serve local, regional and national functions and cover medical and surgical conditions. The study also includes both paediatric and adult intensive care units with no limitation in age or cause of admission. There were too few children to isolate this as a separate subgroup and they differed markedly from the rest of the study sample with regard to survival. They are therefore not included in the analyses of patient characteristics, survival and length of stay. Patients from neonatal intensive care units are not included in the study.
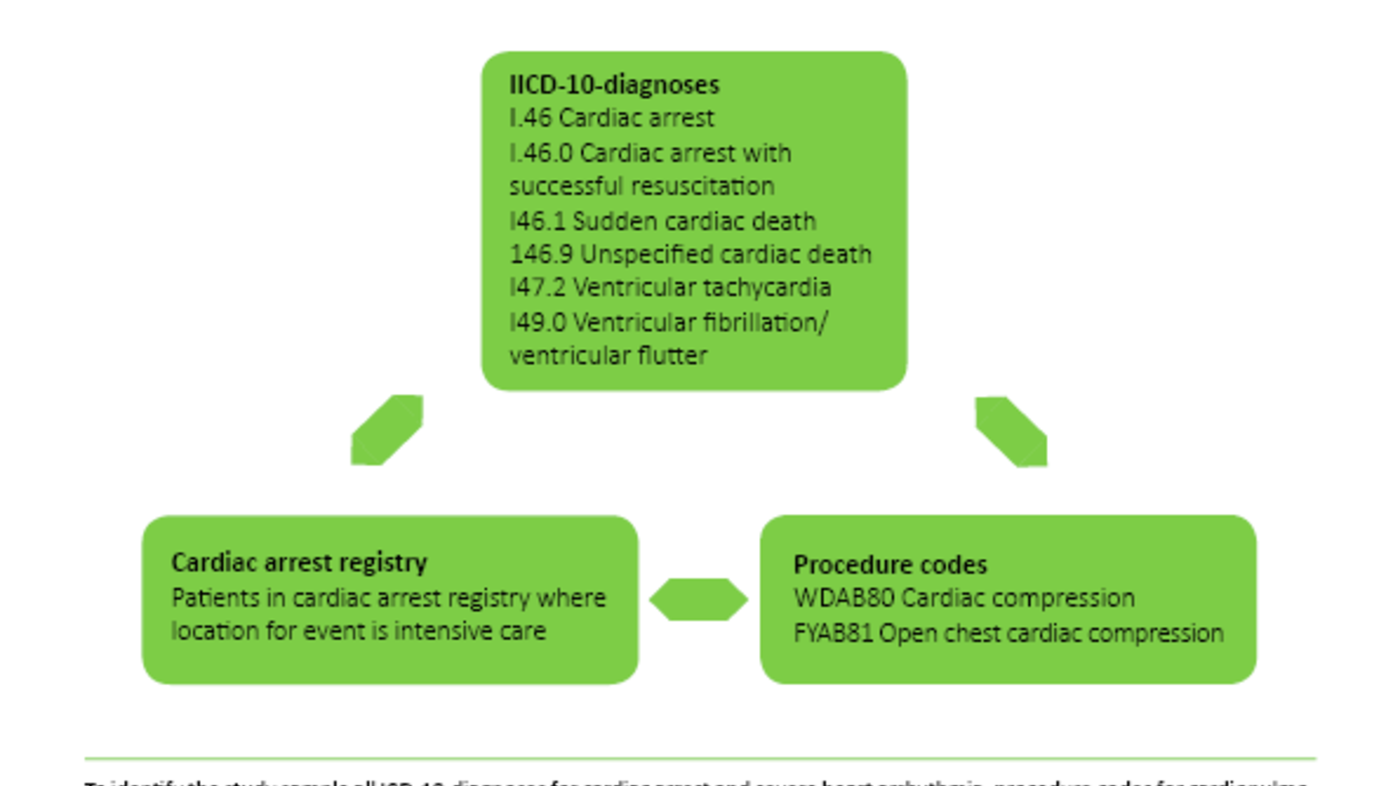
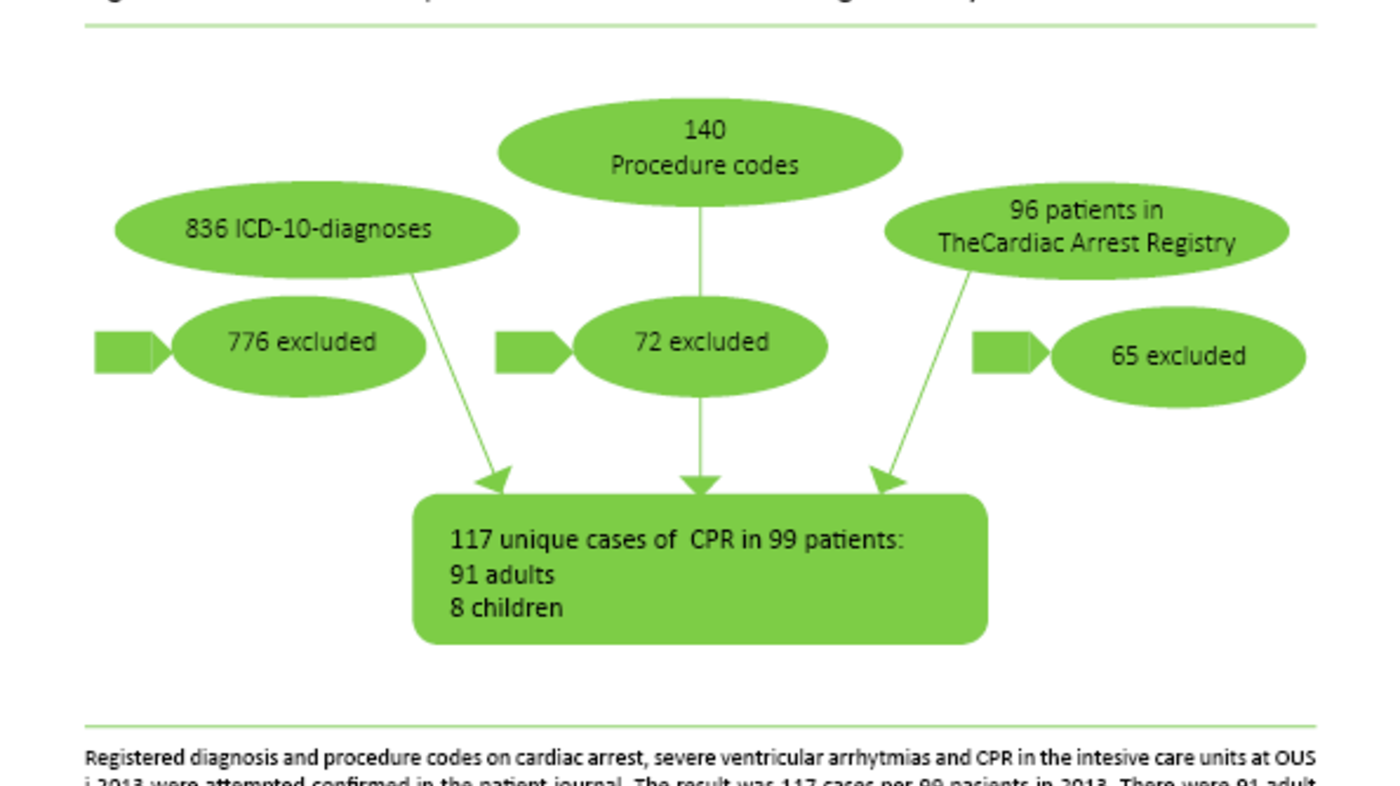
The study sample was made by a triangulation of diagnoses and procedure codes taken from the patient administrative systems PasDoc and SPISS (Figure 1) (11). We then examined identified patients’ journals, both doctors’ and nurses’ notes. Patients with cardiac arrest or CPR not documented in their journal were excluded. We compared the findings with the patients in The Cardiac Arrest Registry. Patients from the registry that were not already identified were added to the study sample (Figure 2).
Inclusion criteria
The Cardiac Arrest Registry’s criteria for inclusion comprise patients that are lifeless and treated with either chest compressions for more than 30 seconds or attempts at defibrillation (12). Repeated cases of cardiac arrest treated with > 1.5 hours intervals qualified for separate registrations. Patients with cardiac arrest at several occasions are included only once in the registry, but the number of CPR is registered. Induced cardiac arrest as part of procedure, such as ventricular fibrillations at the introduction of a heart starter, is not included. We used the same criteria for inclusion in this study.
Data collection
We collected data for the variables age, gender, ward, time of admission, CPR and discharge, location for CPR, survival to discharge from intensive care ward and hospital, as well as to where the patient was discharged. Data were collected from patient journals. We registered whether cardiac arrest or CPR was documented in the doctors’ and nurses’ notes, whether the incident was coded with diagnosis and procedure code in the patient administrative system, and registered in The Cardiac Arrest Registry. Documentation of the patient in all five systems was considered a complete registration. Time for CPR is given in whole days, as there were few exact times given for CPR in the patient journals.
Ethics
The concerned heads of clinics and the data protection official at OUS have approved the study (2013/18062). The Regional Committee for Medical and Health Research Ethics (REK) assessed the project as not needing need approval from REK as it qualified as quality assurance of the health services, case number 2014/1017. Data were anonymised prior to analyses.
Results
In 2013 the 14 intensive care units reported 15 101 admissions distributed on 25 909 bed days. Fifty eight per cent of the hospitalised patients were men. The prevalence of treated cardiac arrest was 0.8 per cent per admission, or 4.5 per 1000 bed days.
The CPR episodes were found at 12 of the 14 wards. The majority of the patients had only one CPR episode, and ten patients experienced two or more episodes of CPR. The age of the patients with cardiac arrest varied between 0 – 91 years. Of the 99 patients we studied, eight were less than 18 years. These children were given CPR at two intensive care units. The majority of the 91 adult patients were men. There was no difference in age between the genders (Table 1).
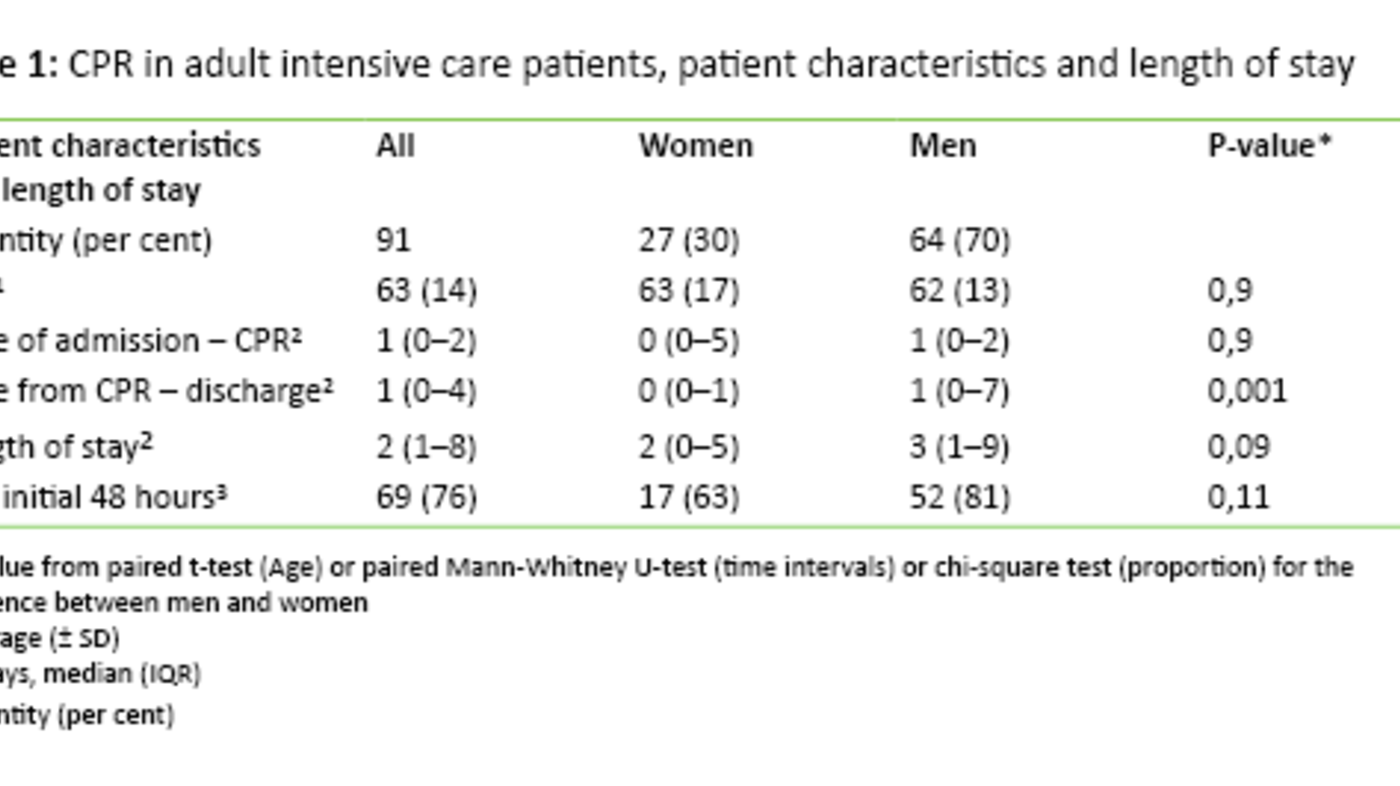
Length of stay and CPR
The majority of patients were given CPR during the two first days in the intensive care unit. A greater number of men than women suffered cardiac arrest within two days, but this difference was not significant (Table 1). For patients who died, time from admittance to CPR was somewhat longer compared to those who survived to discharge from hospital (Table 2).
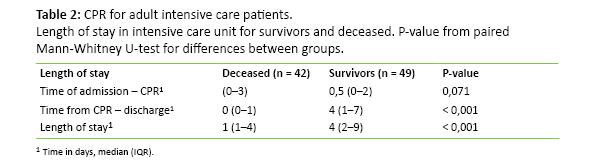
Time from CPR to discharge or death was significantly shorter for women than for men (Table 1). Those who died had significantly shorter time from CPR to discharge than the survivors (Table 2).
The majority of cases of CPR, 93 per cent, were performed in the intensive care ward. The remaining 7 per cent of the cases were performed during transport to radiological examinations or shorter surgical procedures performed outside the ward. These patients were also admitted to the intensive care unit.
Survival
Around half of the adult patients survived to discharge from intensive care unit and hospital. Significantly more men survived to discharge from both intensive care unit and hospital (Figure 3).
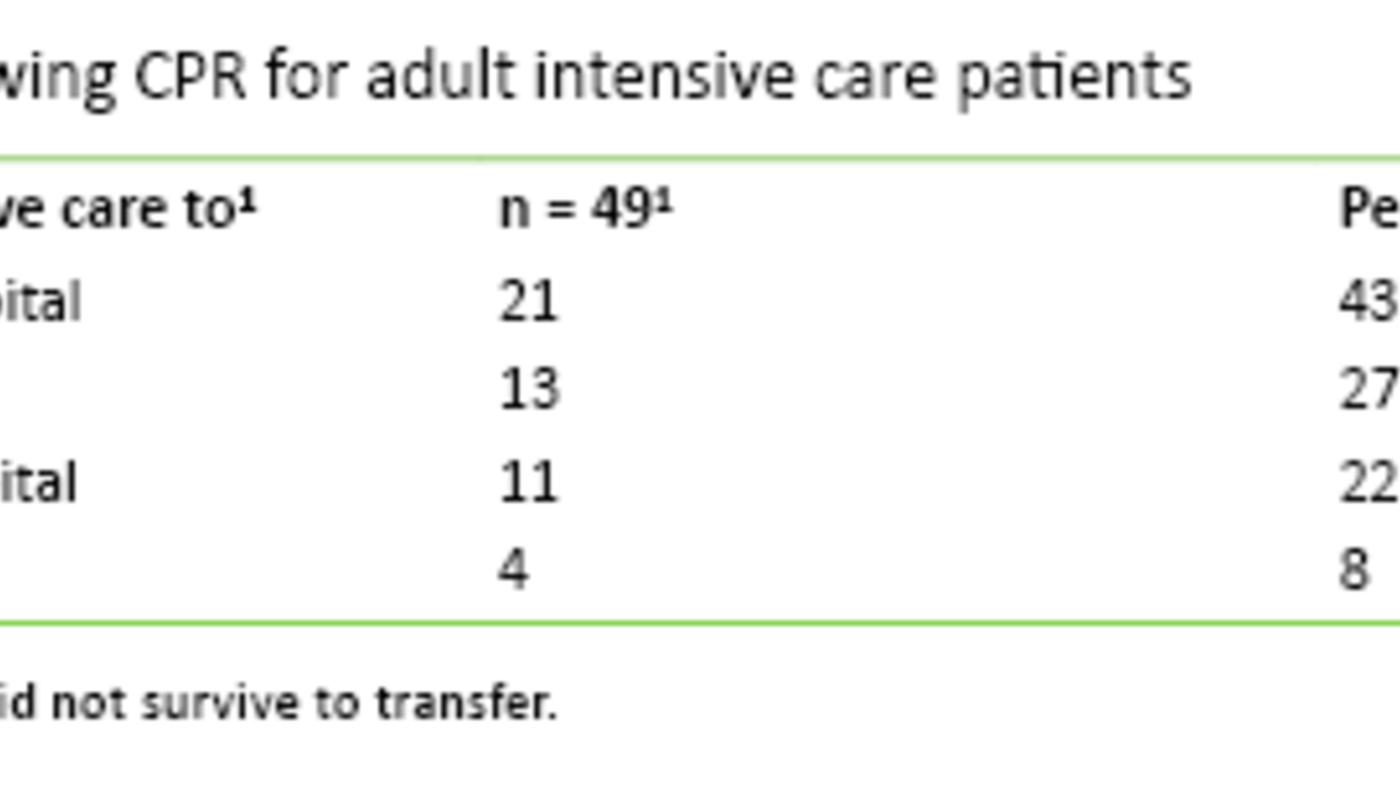
Following discharge from intensive care units where CPR was performed, surviving patients were most often moved to another intensive care unit, either within the hospital or to another hospital. A minority of the patients were moved to a bed ward following cardiac arrest (Table 3).
Registrations
We found 836 diagnosis codes and 140 procedure codes related to cardiac arrest and CPR. A great number were repeated registrations without repeated cases of CPR or cardiac arrest prior to arrival at the intensive care unit. Some cases were excluded as the diagnosis was impossible to confirm in the patient journal. Some of the diagnoses for ventricular arrhythmia were excluded as the patient had had e.g. VF introduced as part of the procedure. The Cardiac Arrest Registry had 96 patients in the study period. Sixty-five of these were not intensive care patients. Of the remaining 31 patients there were nine cases of CPR that had not been identified by diagnosis or procedure codes. These were also included in the study sample (Figure 2).
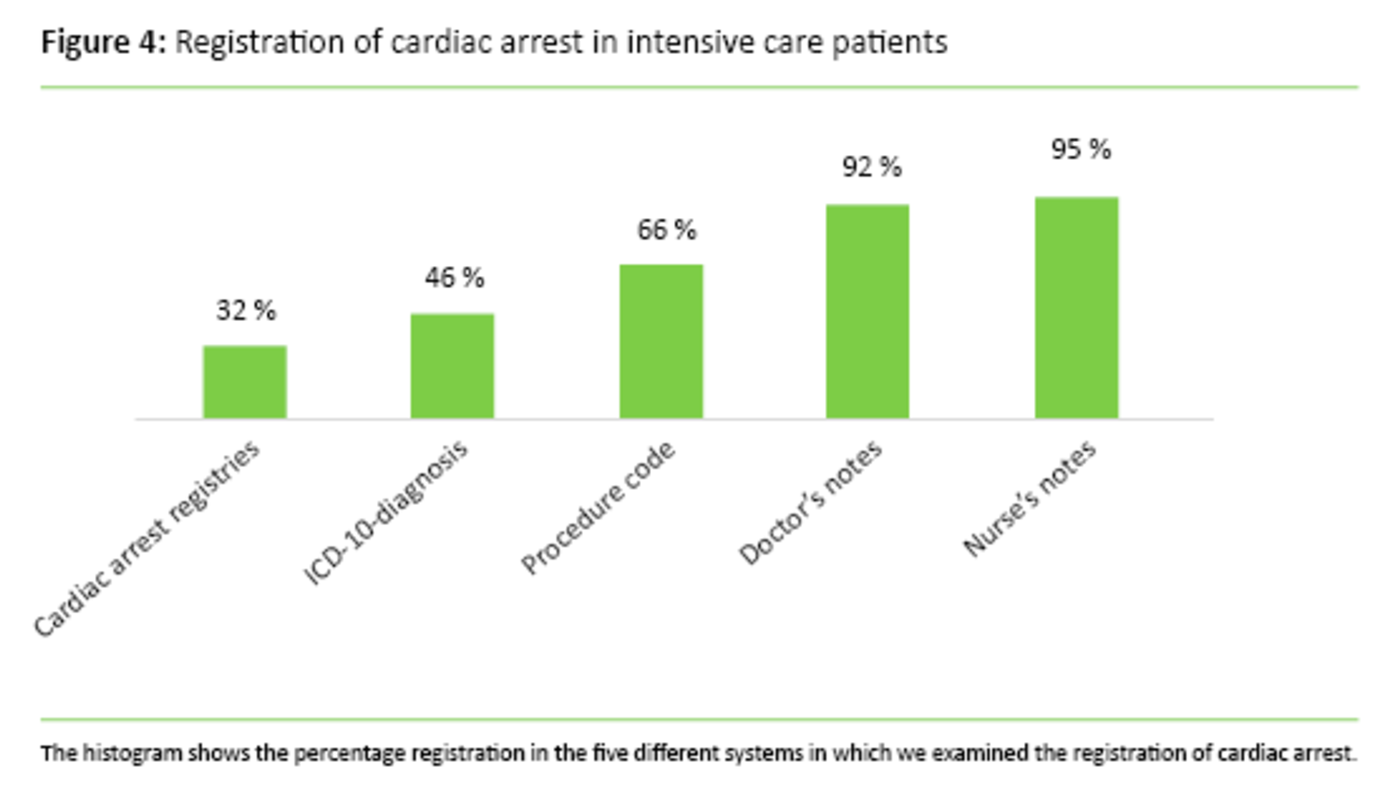
We expected to find registrations in all five systems for all the 99 patients with cardiac arrest, but found only 326 of 495 expected registrations (66 per cent). The greatest omissions were found in The Cardiac Arrest Registry and in the diagnosis and procedure codes. But also the doctors’ and nurses’ notes contained significant omissions with regard to registration. Only eight of the 99 patients had registrations for all the five registration possibilities mentioned above (Figure 4).
Discussion
This study has surveyed the prevalence and registration of CPR, and survival, among intensive care patients in OUS. In 2013 99 children and adults were registered as having received CPR distributed on 117 cases. Forty-eight per cent of the adult patients survived to discharge from hospital.
The population in this study is comparable in age and gender to other similar studies (2, 3, 13 – 19). Prevalence of cardiac arrest varied in other studies between 0.6 – 8 per cent per admission (4 – 7). In our study we found a prevalence of 0.8 per cent. In spite of an extensive mapping process to find CPR at the intensive care units it is uncertain whether all cases of treated cardiac arrest at the intensive care units are in fact included.
Gender differences
Three quarters of the patients in our data had cardiac arrest during the two first days following admission to the intensive care unit. In a study by Rozen et al., two thirds of the patients received CPR during the two first days (1). If most cases of cardiac arrest are caused by cardiovascular disease, this is in keeping with the usual trajectory after acute heart attack and reperfusion. More men than women had cardiac arrest during the first two days. This difference may reflect that women and men have cardiac arrest for different causes, and may also explain some of the gender difference in survival.
A systematic study by Hasan et al., including studies of a half million cases of cardiac arrest independent of location, showed that men have higher prevalence of cardiac arrest when the cause is cardiovascular disease (20). The cause of each individual cardiac arrest was not part of our study. The cause of the cardiac arrest is registered in our internal quality registries, but is coded only as “presumed cardiac” or “other”. The codes are based on best estimates from the treatment team and are rarely reassessed. In a study of cardiac arrest at St. Olav’s Hospital they found that systematic work after-the-fact to clarify cause resulted in a reassessment of the cause of cardiac arrest in one third of the cases (21).
We found that the patients in this study who died following cardiac arrest had significantly shorter time from CPR to discharge. This may be attributed to many patients dying in connection with the CPR procedure or that they later deteriorate to the point where treatment is discontinued.
Higher survival for men
In this study survival to discharge from hospital was 48 per cent. In a systematic literature review by Efendijev, four of 18 studies had similar results with a survival of 47 – 79 per cent. The remaining 14 studies reported a survival rate of 0 – 27 per cent (4). In our study we found that survival to discharge from hospital varied significantly between the genders. This significant difference is also found in Tian et al. who reported a 16.4 per cent survival for men compared to women’s 15.3 per cent (14). Other similar studies do not report survival by gender (2 – 4, 6, 15 – 19, 22 – 26).
Low occurrence of registering
Only 32 per cent of the study sample was registered in The Cardiac Arrest Registry. Quality registries will frequently have a certain degree of underreporting, and analyses of the extent of reporting must be performed to ensure the validity of the data. We used registered diagnoses and procedures in our survey, but there were significant omissions in the documentation in these sources as well. The written journal turned out to be the most reliable registration, but journal searches were limited for technical reasons. It was thus not possible to use patient journals as a primary source for identifying patients. The Swedish National Registry for Cardiac Arrest outside of hospital did a manual search of a sample of ambulance journals and found that 75 per cent of the cases of cardiac arrest were registered. The registry had then been up and running and well known for more than 18 years (27).
We performed our study in The Cardiac Arrest Registry’s first year of operation, but it is nevertheless surprising that only one in three patients were registered. Maybe information on such mandatory registration is easily overlooked in acute care settings with constant changes in treatment methods, equipment and routines. Another reason may be that such registration is simply forgotten in the aftermath of treating patients.
Codes were overreported
This study found a significant overreporting of codes, mostly as a result of repeated registration of the same case of CPR. There were examples of patients with 10 – 15 repeated diagnoses for the same cardiac arrest. This overreporting gives a false image of the hospitals’ activities and weakens the foundation for administrative decisions and resource use based on the coding. The great discrepancies in a review of one single, but nevertheless dramatic and resource intensive event, suggest a need for a review of the coding practice at the hospital.
In addition to overreporting there was also a significant underreporting of cardiac arrest in the patient journal, procedures and diagnosis coding. In most cases we found documentation in the patient journal from doctors and nurses. But when 13 of 99 patient journals are missing documentation from either doctors or nurses on CPR performed during the intensive care stay, this shows that documentation of CPR is incomplete even in the patient journal. According to the Health Personnel Act § 40, documentation of necessary and relevant information in the patient journal is a requirement (8). A potentially life-threatening situation and treatment, such as cardiac arrest and CPR, clearly fall within this category. Any omission of relevant information undermines the patient journal as a source of information and may constitute a threat to patient safety. Just like overreporting, underreporting of codes gives an incorrect picture of reality. Using codes as documentation of activity, e.g. as a basis for this study, becomes difficult.
Underreporting may have financial consequences
Diagnosis and procedure code were given in 46 per cent and 66 per cent of the patients respectively. This underreporting of activity may also have financial consequences for the unit in the estimation of diagnosis related groups (DRG) and activity based financing. We found nothing indicating systematic differences in who was registered and who was not registered in the various systems (based on age, gender and ward).
The findings of both over- and underreporting of diagnosis and procedure codes show that there is a potential for improving documentation of conditions and treatment. Missing documentation in The Cardiac Arrest Registry, patient journal and diagnosis and procedure codes signalises a need to review and improve documentation practice for CPR. Having good quality figures on the incidence of cases of cardiac arrest is crucial for allocating sufficient resources to treat these patients. Cardiac arrest is a serious complication for intensive care patients. The prevalence of cardiac arrest in intensive care units is low. Nevertheless, the potential for a good result is so high that it is important to practice advanced cardiopulmonary resuscitation regularly to maintain knowledge and skills on the subject.
Limitations of this study
This study has several limitations. The study’s framework gave us no possibility to follow up final survival among the patients. Due to the great number of omissions in all registration systems it is still possible that the study sample is not complete, in spite of triangulation. The study’s retrospective design and moderate sample also constitute limitations. We were dependent on reported diagnoses and procedure codes, which turned out to correspond poorly, to identify the sample. The results of this study show the importance of validating quality registries so that they may fulfil their purpose. This study has shown that the internal cardiac arrest registry, after one year of operation, has a preliminary weakness in registrations to map prevalence of cardiac arrest. Organising a good system for registration is a learning experience.
Health registries and data from patient administrative systems are used for evaluation and dimensioning of the health services, as well as for research. Great discrepancies between reported and real cases may lead to erroneous interpretations and wrong decisions. Health registries should be reliable sources of updated information on the health services, causes for illness and health conditions (28). Nurses participate in the cardiac arrest team and have a documentation responsibility, but they must also contribute to the information that ends up in the registries, and ensure that the documentation is correct.
Good registries will be an important source for evaluating and developing nursing practice in the future. They will also make up the basis for nursing research. In the absence of good electronic solutions, the quality of many registries today depends on the personnel treating the patient, and who also register data. In this job the nurse frequently has an active role. Improved knowledge of existing registries and an added effort in the registration work will yield new knowledge to benefit the patient.
Conclusion
The study shows that barely one in one hundred admissions to intensive care was complicated by cardiac arrest and treated with chest compression and /or attempts at defibrillation. Of the patients receiving CPR, one half survived to discharge. Only one third of the patients receiving CPR were registered in The Cardiac Arrest Registry. The reporting is incomplete. According to the doctor's or nurse’s notes, about every tenth patient has not been documented as receiving CPR during their stay in intensive care, which is quite alarming. Discrepancies and omissions in the remaining documentation and registration practice signal a need for improvement of the registration practice. The findings of a difference in survival between the genders suggest a need for further research to identify the causes of this difference.
Referanser
1. Skogvoll E, Lexow K. Hjertestans – definisjon og forekomst. Tidsskrift for Den norske legeforening. 2009;1351–2.
2. Chang SH, Huang CH, Shih CL, Lee CC, Chang WT, Chen YT et al. Who survives cardiac arrest in the intensive care units? Journal of critical care. 2009;408–14.
3. Enohumah KO, Moerer O, Kirmse C, Bahr J, Neumann P, Quintel M. Outcome of cardiopulmonary resuscitation in intensive care units in a university hospital. Resuscitation. 2006;161–70.
4. Efendijev I, Nurmi J, Castren M, Skrifvars MB. Incidence and outcome from adult cardiac arrest occurring in the intensive care unit: a systematic review of the literature. Resuscitation. 2014;472–9.
5. Parra DA, Totapally BR, Zahn E, Jacobs J, Aldousany A, Burke RP et al. Outcome of cardiopulmonary resuscitation in a pediatric cardiac intensive care unit. Critical care medicine. 2000;3296–300.
6. Rozen TH, Mullane S, Kaufman M, Hsiao YF, Warrillow S, Bellomo R et al. Antecedents to cardiac arrests in a teaching hospital intensive care unit. Resuscitation. 2014;411–7.
7. Slonim AD, Patel KM, Ruttimann UE, Pollack MM. Cardiopulmonary resuscitation in pediatric intensive care units. Critical care medicine. 1997;1951–5.
8. Lovdata. Lov om helsepersonell m.v. (helsepersonelloven) 2. juli 1999. Available from: https://lovdata.no/lov/1999-07-02-64. (Downloaded 22.03.2015).
9. Lovdata. Lov om helseregistre og behandling av helseopplysninger (helseregisterloven) 20. juni 2014. Available from: https://lovdata.no/lov/2014-06-20-43. (Downloaded 22.03.2015).
10. Emilsson L, Lindahl B, Köster M, Lambe M, Ludvigsson JF. Review of 103 Swedish Healthcare Quality Registries. Journal of Internal Medicine. 2015;94–136.
11. FinnKode 2014 Versjon 5.0.3. Available from: www.https://finnkode.ehelse.no.
12. Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries. A statement for healthcare professionals from a task force of the international liaison committee on resuscitation. Resuscitation. 2004;233–49.
13. Lee HK, Lee H, No JM, Jeon YT, Hwang JW, Lim YJ et al. Factors influencing outcome in patients with cardiac arrest in the ICU. Acta Anaesthesiologica Scandinavica. 2013;784–92.
14. Tian J, Kaufman DA, Zarich S, Chan PS, Ong P, Amoateng-Adjepong Y et al. Outcomes of critically ill patients who received cardiopulmonary resuscitation. American Journal of Respiratory and Critical Care Medicine. 2010;501–6.
15. Grigoriyan A, Vazquez R, Palvinskaya T, Bindelglass G, Rishi A, Amoateng-Adjepong Y et al. Outcomes of cardiopulmonary resuscitation for patients on vasopressors or inotropes: A pilot study. Journal of Critical Care. 2009;415–8.
16. Wallace S, Ewer MS, Price KJ, Feeley TW. Outcome and cost implications of cardiopulmonary resuscitation in the medical intensive care unit of a comprehensive cancer center. Supportive Care in Cancer. 2002;425–9.
17. Landry FJ, Parker JM, Phillips YY. Outcome of cardiopulmonary resuscitation in the intensive care setting. Archives of Internal Medicine. 1992;2305–8.
18. Myrianthefs P, Kalafati M, Lemonidou C, Minasidou E, Evagelopoulou P, Karatzas S et al. Efficacy of CPR in a general, adult ICU. Resuscitation. 2003;43–8.
19. Yi HJ, Kim YS, Ko Y, Oh SJ, Kim KM, Oh SH. Factors associated with survival and neurological outcome after cardiopulmonary resuscitation of neurosurgical intensive care unit patients. Neurosurgery. 2006;838–45; discussion 45–6.
20. Hasan AF, Al Suwaidi J, Omer AA, Ghadban W, Alkilani H, Gehani A et al. The Influence of female gender on cardiac arrest outcomes: a systematic review of the literature. Current medical research and opinion. 2014;1–30.
21. Bergum D, Nordseth T, Mjølstad OC, Skogvoll E, Haugen BO. Causes of in-hospital cardiac arrest – Incidences and rate of recognition. Resuscitation. 2015;63–8.
22. Bialecki L, Woodward RS. Predicting death after CPR. Experience at a nonteaching community hospital with a full-time critical care staff. Chest. 1995;1009–17.
23. Karetzky M, Zubair M, Parikh J. Cardiopulmonary resuscitation in intensive care unit and non-intensive care unit patients. Immediate and long-term survival. Archives of Internal Medicine. 1995;1277–80.
24. Rabinstein AA, McClelland RL, Wijdicks EF, Manno EM, Atkinson JL. Cardiopulmonary resuscitation in critically ill neurologic-neurosurgical patients. Mayo Clinic proceedings. 2004;1391–5.
25. Peterson MW, Geist LJ, Schwartz DA, Konicek S, Moseley PL. Outcome after cardiopulmonary resuscitation in a medical intensive care unit. Chest.1991;168–74.
26. Skrifvars MB, Varghese B, Parr MJ. Survival and outcome prediction using the Apache III and the out-of-hospital cardiac arrest (OHCA) score in patients treated in the intensive care unit (ICU) following out-of-hospital, in-hospital or ICU cardiac arrest. Resuscitation. 2012;728–33.
27. Stromsoe A, Svensson L, Axelsson AB, Goransson K, Todorova L, Herlitz J. Validity of reported data in the Swedish Cardiac Arrest Register in selected parts in Sweden. Resuscitation. 2013;952–6.
28. Folkehelseinstituttet. Dahl C, Camilla Stoltenberg C, Magnus T. Gode helseregistre – bedre helse : strategi for modernisering og samordning av sentrale helseregistre og medisinske kvalitetsregistre 2010–2020. Oslo, 2009.









Comments