Obstetric care for breech presentations at Oslo University Hospital, Ullevål in the period 2000–2012
From 2000 to 2006, the number of planned vaginal deliveries fell; numbers started rising again nearer 2012. Practice was probably influenced by the Term Breech Trial.
Background: There is much debate concerning the best way to deliver breech fetuses. October 2000 saw the publication of the results of the Term Breech Trial (TBT), which concluded that a planned caesarean section was the safest mode of delivery for full-term breech babies. The study led to a major change in obstetrics, to the extent that most countries currently deliver breech fetuses by planned caesarean section. In Norway, the recommendation has been for vaginal delivery for selected groups of breech presentations, both before and after the TBT study.
Objective: The objective of this current study has been to describe clinical practice at Ullevål Hospital’s maternity unit in cases of breech presentation, and to study any changes introduced to the unit’s practice after 2000. We have also compared outcomes for newborn infants, measured by their Apgar score, for different modes of delivery.
Method: We carried out a retrospective registry study of women with breech presentation at ≥34 weeks of gestation at Oslo University Hospital, Ullevål over the period 2000–2012.
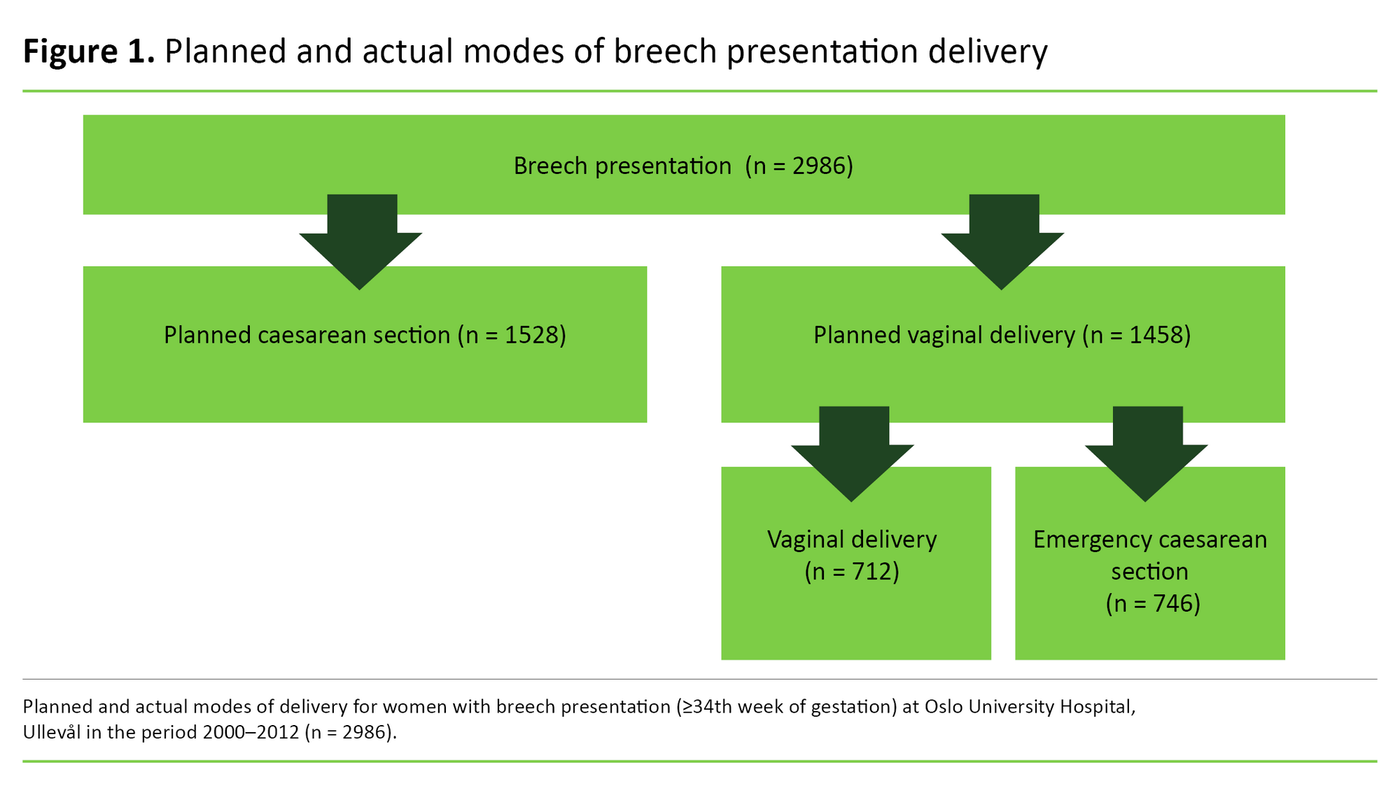
Results: In the course of the study period, Ullevål Hospital treated a total of 2986 women with breech presentation at ≥34 weeks of gestation. This amounted to an average of 3.8 per cent of all births at the hospital. In 2000, the percentage share of planned vaginal deliveries was 62.9. From 2001, the number of women selected for vaginal delivery fell in the period up to 2006, when the share reached its lowest level of 34.2 per cent. Numbers then rose again, and in 2012, a vaginal delivery was planned for 49.8 per cent of women with breech presentation. The odds for a low Apgar score, a measurement of the vitality of the newborn 5 minutes after birth, were higher if the infant was in the group selected for a planned vaginal delivery.
Conclusion: It appears that practice at Ullevål Hospital may have been influenced by the results of the TBT study published in 2000. Following a decline in the number of planned vaginal deliveries in the period up to 2007, numbers rose again near the end of the study period. Infants with a low Apgar score made up a larger proportion of the group selected for a vaginal delivery compared to the group selected for a planned caesarean section.
In 3–4 per cent of full-term pregnancies, the fetus will present with the buttocks or feet down towards the cervix (1, 2). Breech presentation shows a familial tendency. The risk increases with age and occurs more frequently in primiparous women (1, 2).
If the baby presents in a breech position after week 36, the woman is selected to give birth at a large maternity unit and plans are made for either a vaginal delivery or a caesarean section based on certain selection criteria (2–4). Studies show that approximately 20 per cent of breech presentations are undiagnosed at the onset of labour (5).
Earlier research
Choice of delivery mode has been a contentious issue for many years, particularly since Hannah et al. published the Term Breech Trial in 2000 (6). This was a large, randomised trial in which the objective was to compare outcomes for planned vaginal deliveries with planned caesarean sections for full-term breech presentation pregnancies (≥37 weeks).
The study was conducted at 121 maternity units in 26 countries, and a total of 2088 patients were included (6). The results showed that infant mortality and morbidity were significantly lower in the group randomised for a planned caesarean section than in the group randomised for a planned vaginal breech delivery (6). The medical establishment responded quite promptly to the study’s conclusion, and rarely have the results of a single study changed medical practice as much and as fast as in this instance (7).
A survey published in 2003 showed that out of 80 maternity units in 23 countries, 92.5 per cent had discontinued their policy of planned vaginal deliveries, giving way to planned caesarean sections in cases of breech presentation (7). In Norway, the frequency of caesarean sections also rose after 2000, and planned caesarean deliveries of full-term breech presentations increased from 52.4 per cent in 1999 to 64.3 per cent in 2004 (8).
The TBT study has subsequently been criticised in a number of respects. The inclusion criteria were not followed up in all of the participating centres, most of the women were recruited only once labour had commenced, antenatal ultrasound examinations had not always been carried out at the time of inclusion, and twins were included, as well as fetuses with anomalies that were incompatible with life. Some of the still births included in the study were therefore not associated with the mode of delivery (7, 9).
Recommended mode of delivery
Vaginal breech births and the delivery of breech presentations make up a small part of births in a maternity ward, but they represent an obstetric challenge that requires obstetricians and midwives to master the correct delivery techniques (10).
After publication of the TBT study, a team was set up by the Norwegian Centre for Health Technology Assessment (SMM). The team was tasked with reviewing the relevant literature and asked to come up with a recommended mode of delivery for full-term breech presentations (5). Based on this review, it was decided to continue to recommend a vaginal delivery for breech presentations, provided certain criteria were met (5, 11).
In brief, the criteria are as follows: gestation ≥34 weeks, estimated weight at birth ≥2000–4000 grammes and either complete or incomplete breech presentation (2). Additionally, the Norwegian Directorate of Health recommends that vaginal breech deliveries are routed to the larger centralised maternity units (11).
Disagreement concerning obstetric care for breech presentations
The controversy that surrounds optimal obstetric care for women with breech presentation focuses on two clinical questions in particular:
‘What is the risk of an undesirable outcome for breech babies delivered vaginally?’ And ‘how should this risk be balanced against the short- and long-term risks of a caesarean section?’ (12, 13).
There is some risk of an undesirable outcome whatever the fetal presentation and mode of delivery, but in modern obstetrics the main aim is to reduce the risk of complications to a minimum (10). Within the field of obstetrics it is therefore necessary to balance the advantages against the disadvantages associated with the various modes of delivery for mother and child.
This assessment involves a study of planned vaginal deliveries versus planned caesarean sections, combined with establishing whether the actual mode of delivery is vaginal or involves an emergency or planned caesarean section. Continual follow-up of one’s own practice is important, which is why we wanted to conduct an internal quality assessment of breech deliveries at Oslo University Hospital, Ullevål.
Objective of the study
The objective of the study is to describe clinical practice at the Ullevål maternity unit in respect of breech presentations and to study any changes that may have occurred in the period 2000–2012. Additionally, we wanted to compare infant outcomes, measured by their Apgar score, for different modes of delivery.
Method
Material and method
The study is a retrospective registry study. We obtained data from the Gjessing registry at Ullevål Hospital’s maternity unit. This was the hospital’s register of births throughout the study period. Midwives entered information about each birth into the database, and these data were subsequently submitted to the Medical Birth Registry of Norway. The study ran from 1 January 2000 to 31 December 2012.
The original quality-controlled dataset contained anonymous records of 81 711 births. We excluded all births that involved a cephalic presentation or a transverse lie, as well as twins, triplets, children with abnormalities and stillbirths that had taken place before arrival at the hospital. The breech presentation deliveries that were included took place in the 34th–42nd week of gestation. Prior to the 34th week of gestation, a caesarean section is the recommended mode of delivery (2). These were therefore excluded from the material.
The total study population was 2986 women with breech fetal presentation at ≥34 weeks of gestation. This is a quality study that uses anonymised data and involves no contract with patients. Consequently, we have not sought the approval of the Regional Committees for Medical and Health Research Ethics. The study was reported to and approved by the Personal Data Officer at Oslo University Hospital (case number 2015/1520).
Data
From the Gjessing database we obtained information about mode of delivery (figure 1). Planned modes of delivery were split into planned vaginal delivery (PVD) and planned caesarean section (PCS). Actual modes of delivery are divided into planned caesarean section (PCS), vaginal delivery (VD) and emergency caesarean section (ECS).
The data included the Apgar score, which describes the physical wellbeing of the newborn at 1, 5 and 10 minutes after birth. Five characteristics are subjectively assessed: heart rate, respiration, muscle tone, reflexes and skin colour, each of which are allocated a score of 0–2. The total score is the sum of the five characteristics, with an Apgar score of ≥7 at 5 minutes suggesting that the newborn is well. An Apgar score of <7 at 5 minutes is defined as a low Apgar, and an Apgar score of <4 at 5 minutes as an extremely low Apgar (14, 15).
Other variables included:
- Mother’s age, split into four categories: <25 years, 25–29 years, 30–34 years, ≥35 years
- Parity: primipara (P0) or multipara P ≥ 1.
- The baby’s weight and week of gestation at birth: a gestation period of ≥37 weeks is defined as a full-term pregnancy, while infants delivered between week 34+0 and week 36+6 days are defined as premature.
We also looked at indications for caesarean section. The ‘other’ indications included preeclampsia or eclampsia, placenta previa, pathological doppler, haemorrhaging, earlier uterine surgery, and no indication (due to insufficient cases). Breech indications included narrow pelvis and foot presentation.
Analysis
In order to describe trends over time with respect to planned and actual modes of delivery, we express the number of deliveries per mode as annual percentages. We split the study period into two: 2000–2006 and 2007–2012, in order to test whether differences have occurred with respect to the ratios of planned and actual modes of delivery, as well as indications for planned and emergency caesarean section in the course of the study period.
This was done to increase the strength of the test, because the annual variations were only small. There were approximately the same number of breech presentation pregnancies in each period. We used a chi-squared test to analyse differences between the groups.
We examined the correlation between a low Apgar score, prematurity, planned mode of delivery and mother’s age by means of multiple logistic regression analysis. The results are presented as adjusted and unadjusted odds ratios with a 95 per cent confidence interval. We conducted the analyses in SPSS, version 21. We chose a significance level of 5 per cent (p < 0.05) for all tests.
Results
The incidence of singletons presenting in a breech position at full term was 3.8 per cent in the study period. Among the premature, born between gestation week 34 and 36, the incidence of breech presentation was 3.9 per cent.
Figure 2 shows the trend over time for planned modes of delivery and actual modes of delivery. The percentage share of women selected for a planned vaginal delivery fell markedly towards the end of the period, giving way to planned caesarean sections.
This trend reached its peak in 2006. From 2007, there was a slight increase in the percentage share of women selected for a planned vaginal delivery; this rise reached its peak in 2012. At that point, the groups allocated to the different planned modes of delivery were almost equal in size, with 49.8 per cent planned vaginal deliveries and 50.2 per cent planned caesarean sections.
Figure 2 also shows the variations in actual modes of delivery over the course of the study period. The percentage share of vaginal births rose later in the period, after 2001, when vaginal deliveries were at their lowest: 13.7 per cent. For a period of four years after 2001, there were fewer emergency caesarean sections.
In 2006, the percentage share of emergency caesarean sections increased, but there were fewer planned caesarean sections. The percentage share of vaginal deliveries was relatively stable throughout these years until vaginal deliveries increased by 14 percentage points from 2011 to 2012.
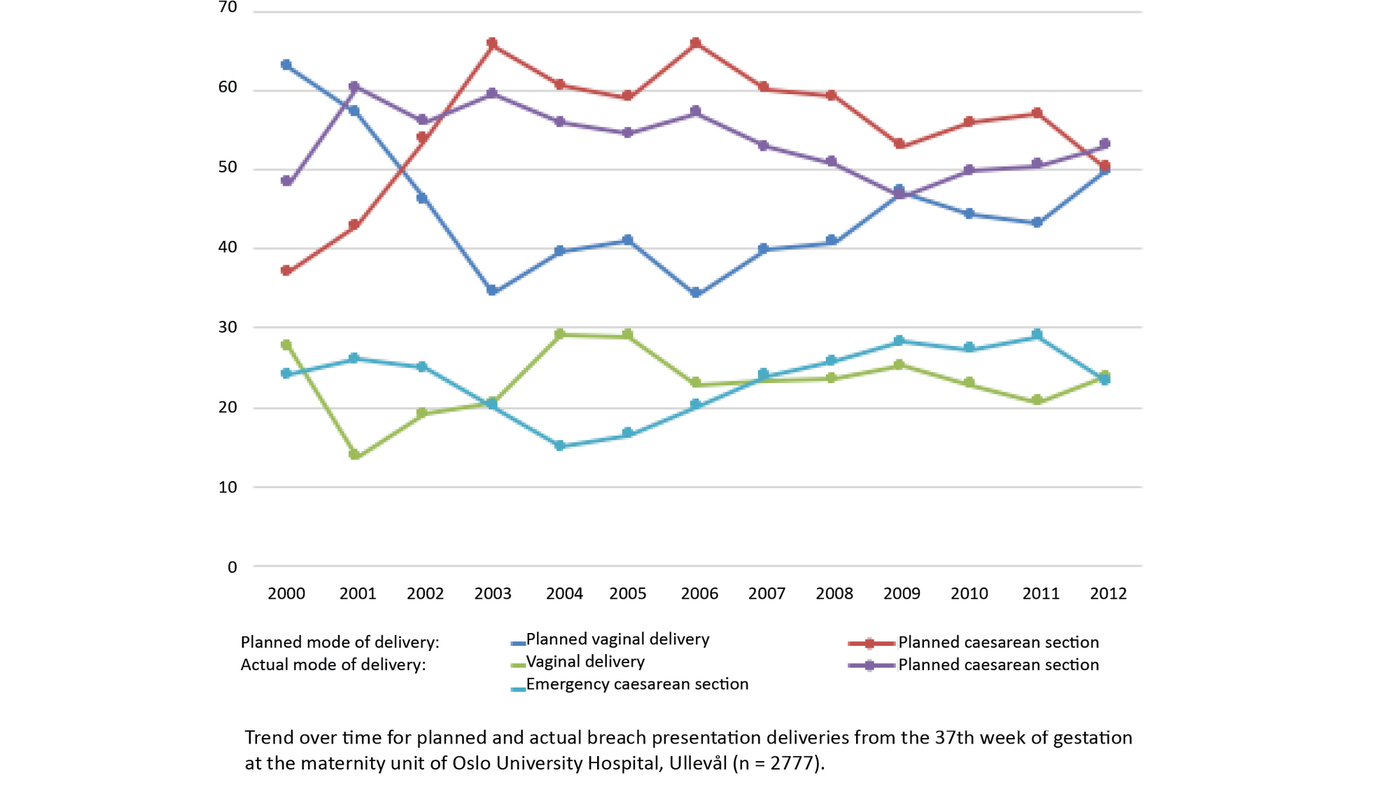
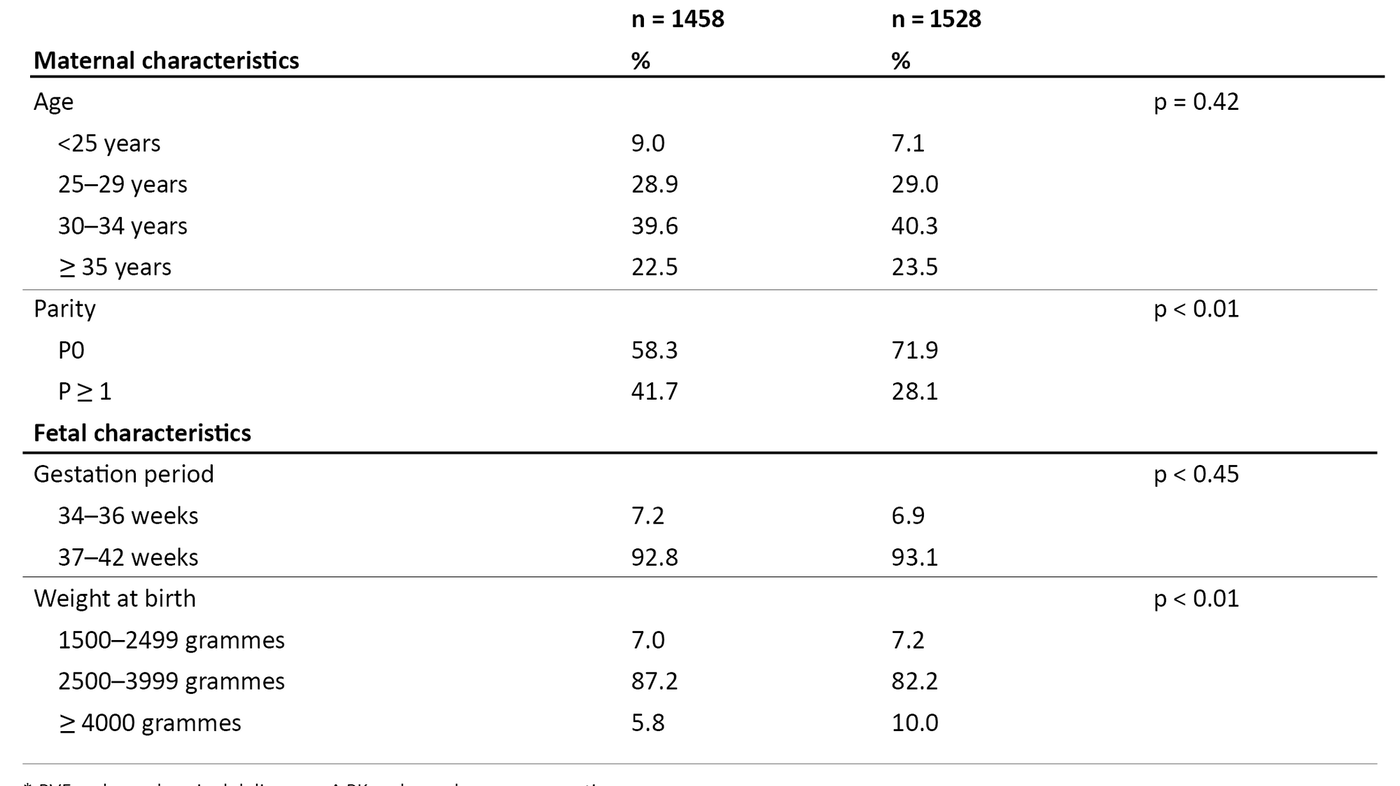
Table 1 shows characteristics of the study population based on the planned mode of delivery. There was no age difference between the two groups. There was a larger percentage share of multiparous women and of infants weighing <4000 grammes in the ‘planned vaginal delivery’ group..
With respect to indications for planned and actual caesarean sections, table 2 shows how this changed over the study period.
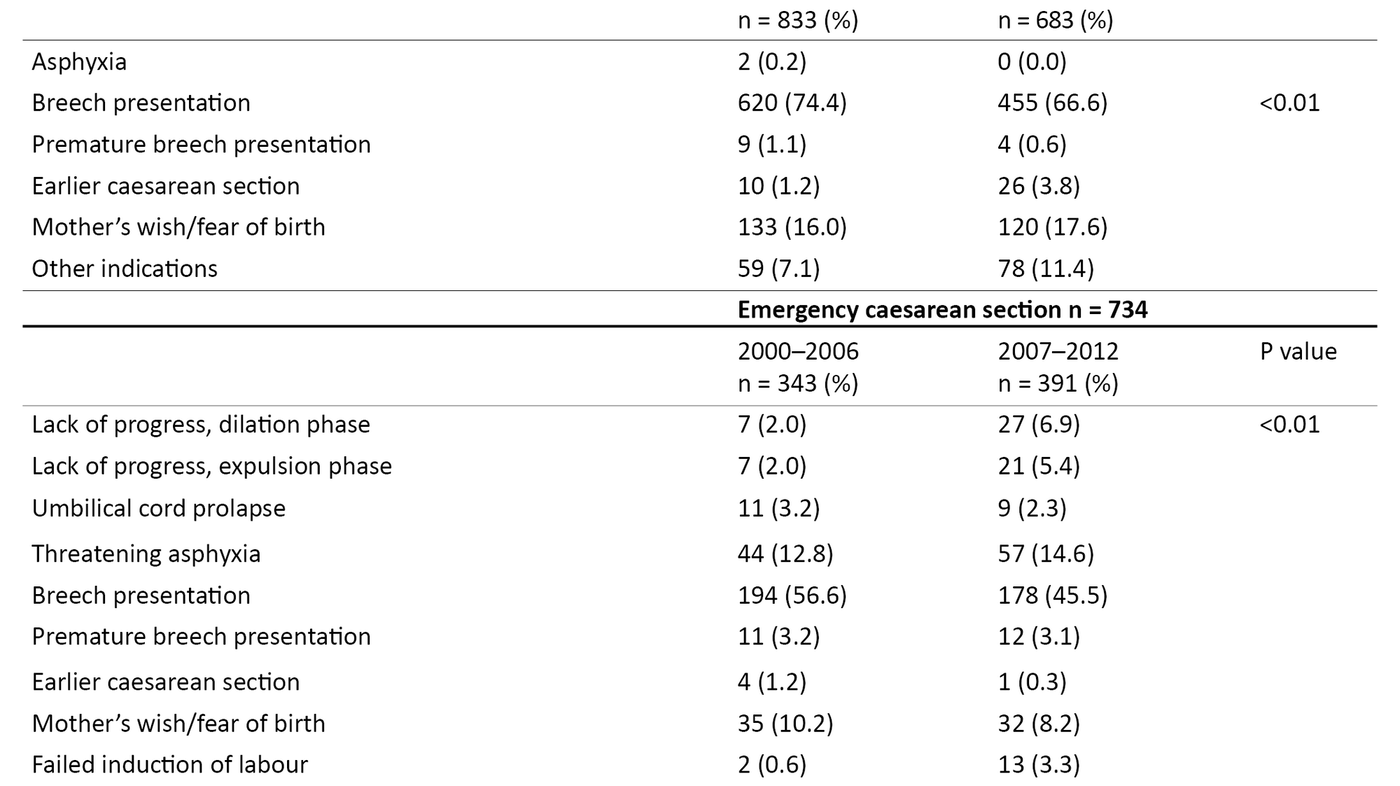
There was a significant difference associated with the distribution of indications for emergency and planned caesarean sections in both time periods. The greatest difference was identified for the indications ‘lack of progress, dilation phase’, ‘lack of progress, expulsion phase’, ‘asphyxia’ and ‘failed induction of labour’ in the ‘emergency caesarean section’ group.
These indications were used more frequently in the second period. The percentage share of earlier caesarean sections was greater in the ‘planned caesarean section’ group in the second period. The percentage share of ‘mother’s wish/fear of birth’ was stable for both groups throughout the two periods.
Table 3 shows how well newborn infants were doing immediately after the birth, as measured by Apgar scores related to the planned mode of delivery, gestation period and mother’s age.
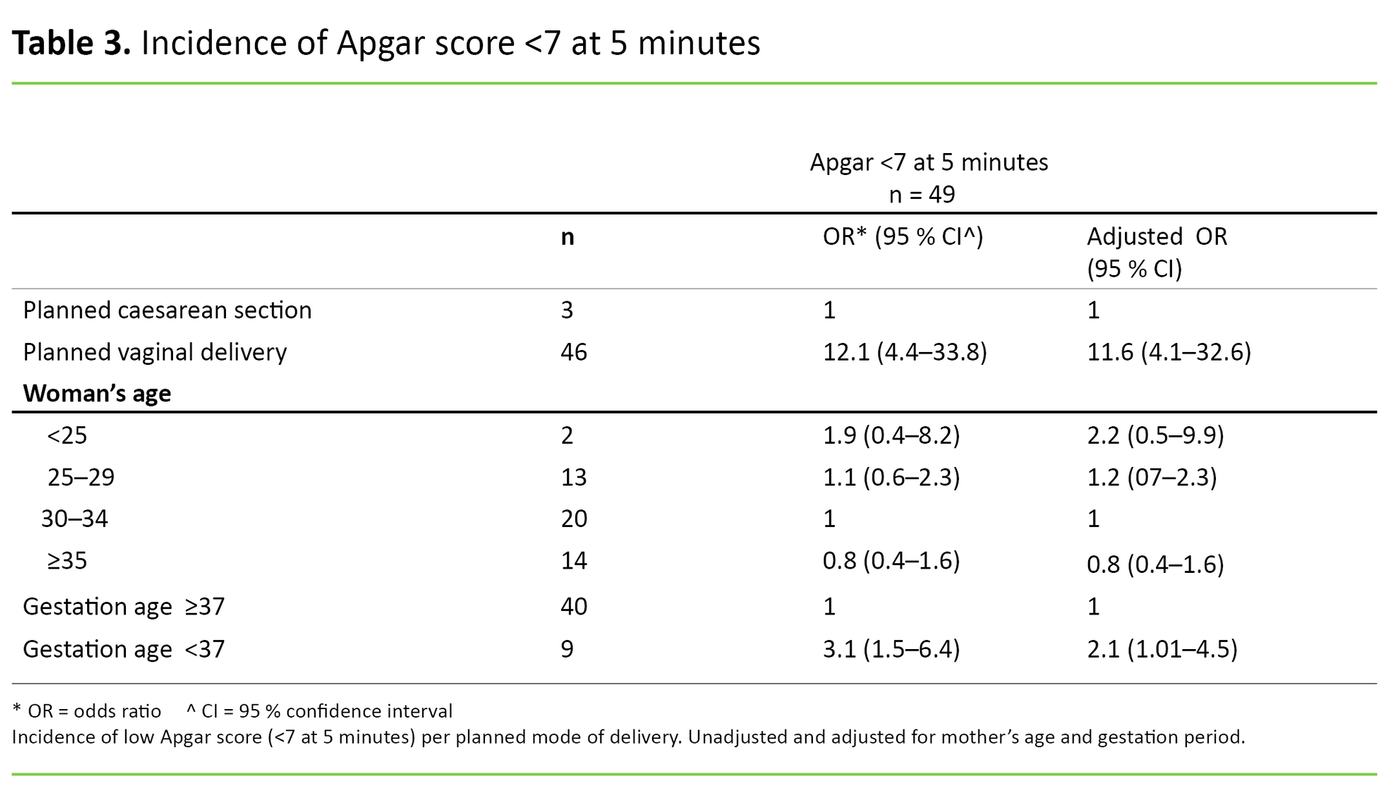
The regression analysis showed that there was a significant difference in the odds ratios for an Apgar score of <7 at 5 minutes between the ‘planned vaginal delivery’ and ‘planned caesarean section’ groups, and for gestational age <37 and ≥37 weeks. The material included only 12 extremely low Apgar scores (<4), 11 of which were in the ‘planned vaginal delivery’ group and one of which was in the ‘planned caesarean section’ group (not shown in the tables).
We have therefore assembled all infants with an Apgar score of <7 in one group for the purpose of regression analysis. The unadjusted figures reveal that in the ‘planned vaginal delivery’ group the odds that the infant would have an Apgar score of <7 were 12 times higher than in the ‘planned caesarean section’ group. The latter remained virtually unchanged when adjusted for gestation period and mother’s age.
At prematurity, the odds of an Apgar score of <7 at 5 minutes were three times higher than if the delivery was at full term (table 3). When we compared the number of infants with a low Apgar score in the two time periods, we found no significant differences (not shown in the tables).
Discussion
The main findings of this study show that more women with breech presentation were selected for a planned caesarean section at Ullevål as from 2001. After 2007, this percentage share fell, giving way to a rising percentage share of women who were selected for a planned vaginal delivery. In 2012 the percentage shares allocated to the two groups were virtually identical. The indications for planned and emergency caesarean section varied when the study period was split into two.
The difference was greatest for the indications ‘lack of birthing progress’ and ‘failed induction of labour’ for emergency caesarean sections. The incidence of the indication ‘mother’s wish/fear of birth’ was equal in both periods. There were more infants with a low Apgar score at 5 minutes in the ‘planned vaginal delivery’ group.
More caesarean sections after the TBT study
Throughout the study period, Ullevål Hospital practised selection of breech presentation pregnancies for vaginal delivery at a gestational age of ≥34 weeks. In 2000, the percentage share of breech presentation pregnancies selected for a planned caesarean section was 37.1, a few percentage points below the national average (16). The practice resulted in 62.9 per cent being selected for planned vaginal delivery.
After the publication of the TBT study in October 2000 (6), the percentage share of women selected for a planned caesarean section rose in Norway, like in other countries (7, 17). In 2003, the percentage share of women selected for a planned caesarean section at Ullevål was 65.6, and the situation had reversed compared to the period prior to the publication of the TBT study. In the years prior to TBT, practice at Ullevål was based on the Norwegian Obstetrics Guidelines 1998 (18).
The report issued by the Norwegian Centre for Health Technology Assessment (SMM) in 2003 concluded that the current recommendations, dating from 1998, involving the selection of certain breech pregnancies for vaginal delivery, should remain in place (5). The conclusion supports the practice at Ullevål Hospital prior to the year 2000.
Nevertheless, the figures in our study show that the practice at Ullevål is likely to have been influenced by the TBT study, considering the fall in planned vaginal deliveries. This finding is supported by an historic review article by Bergsjø, in which an increase in the use of caesarean section was observed immediately following the publication of the TBT study (8).
Breech delivery skills training
In the years following the publication of the TBT study, other obstetric practices have published results from studies based on populations that better match the clinical practice at Ullevål before 2001. These studies provide more nuanced conclusions (12, 19–21).
It may seem as if the discipline of obstetrics has gradually taken on board the complications that caesarean sections may involve for mother and child in connection with the intervention and in connection with any subsequent pregnancies and births (13, 22). Additionally, the practice of conducting a planned caesarean section for all breech presentation pregnancies may well result in a loss of skills among clinicians. This loss of skills may in turn have an impact on patient safety.
There will always be birthing women arriving at maternity units with an undiscovered breech presentation. Of the breech presentations included in our study, 368 (12.3 per cent) were undiscovered at ≥34 weeks gestation, and 52 per cent of these were delivered vaginally (not shown in the tables). In these instances, the skills of the obstetric team may have been pivotal to the outcome of the birth for mother and child.
Ullevål Hospital has been organising systematic cross-disciplinary skills training sessions in emergency obstetrics since January 2008. Breech delivery has featured on the rolling programme of topics approximately every two years. Auxiliary children’s nurses, doctors and midwives take part in skills training every 16 to 18 months, according to interviews with the Skills Training Officer at Ullevål.
Breech presentation deliveries at Ullevål maternity unit have traditionally followed the recommendations of the Obstetrics Guidelines, which remained the same throughout the study period (18). The guidelines describe the procedure for breech deliveries as follows: ‘Normal delivery is the main method. The infant is delivered spontaneously until the umbilicus is seen, after which the obstetrician actively extracts the shoulders and head’ (18, p. 130).
Anxious about vaginal delivery
We found that indications for both planned and emergency caesarean sections changed over the course of the study period. The indications ‘lack of progress, dilation phase’ and ‘lack of progress, expulsion phase’ in the ‘emergency caesarean section’ group tripled from period one to period two. This change may perhaps be explained by the fact that we have more knowledge about how an extended period of labour may negatively affect the infant (23).
Breech births represent a risk and may involve an extended period in labour (1). Emergency caesarean sections based on this causal chain may seem reasonable, as the desirable outcome will always be a healthy mother and a healthy child. The percentage share of planned caesarean sections based on the indication ‘mother’s wish/fear of birth’ was virtually the same in both mode of delivery groups for both periods.
‘Mother’s wish/fear of birth’ was the second most frequent indication in the ‘planned caesarean section’ group during both periods. These women meet the selection criteria for vaginal delivery, but do not wish or are afraid to give birth vaginally if the fetus presents in a breech position (20).
Pregnant women may be anxious about vaginal breech deliveries due to information received through the media or from healthcare personnel. It is therefore important that all information provided about outcomes is correct, and that details are accurate in respect of the facilities available at the maternity unit concerned (24).
The percentage share of caesarean sections based on ‘mother’s wish/fear of birth’ is relatively similar in the two periods. This may suggest that the pregnant women have received no new evidence-based information. Alternatively, they dare not trust the new results.
What influences a low Apgar score?
Our analyses show that there were higher odds of giving birth to an infant with a low Apgar score in the ‘planned vaginal delivery’ group compared to the ‘planned caesarean section’ group. There were few newborn infants with a low Apgar score, which may explain the wide confidence interval. Our analysis adjusted for gestation period and mother’s age.
Our material did not include enough details or sufficiently good data to examine other factors that may influence the Apgar, such as a high body mass index (25) or mother’s smoking habits (26). The results must therefore be interpreted in this light.
A low Apgar score may suggest that the well-being of the newborn is below optimal immediately after delivery, which is therefore an undesirable outcome (27). A low Apgar score may be associated with underlying factors, maternal or fetal illness, or pregnancy complications, or it may be associated with the delivery, or the fact that the fetus presented in a breech position.
For newborn infants with an Apgar score of <7 at 5 minutes after birth, there may often be a brief period before the infant recovers (19). A poorer prognosis is expected for those with an Apgar score of <4 at 5 minutes, and they will probably need a period of observation and/or treatment after birth (15).
The risk of a low Apgar score in connection with breech delivery has been described in several studies (19, 20, 27), but this risk has been approached in different ways. In Norwegian (20, 26) and Finnish studies (19) the risk is recognised, but selecting certain pregnancies for planned vaginal delivery is still the recommended practice.
An important point in this context is that the researchers found no differences after two years, despite the increased risk of mortality and morbidity among those who had a planned vaginal delivery in the TBT study (29). Although we saw a change in clinical practice with respect to the planned mode of delivery during the study period, there was no difference in the percentage share of infants with a low Apgar score when the period was split into two.
Strengths and weaknesses of the study
The maternity unit at Ullevål Hospital is the largest in Norway, thus providing a sizeable volume of material for our study. It is a strength that the data were obtained from the unit’s registry of births, which has been subjected to multiple quality control procedures in order to ensure that the records are correct. Apgar scores are important and useful assessments of outcomes for newborn infants immediately after birth (30).
However, the weakness of the Apgar score as a method is the fact that it is based on a subjective assessment. A supplementary blood gas analysis of the umbilical cord pH would have given a more objective answer to whether, and to what extent, the fetus has been exposed to stress during birth (31). The data from Ullevål included recorded blood gas analyses for 40 per cent of deliveries in the ‘planned vaginal delivery’ group, so umbilical cord pH could not be used to measure outcomes.
Another weakness associated with the registry data is the absence of follow-up data about the well-being of infants with a low Apgar score. The methods used in our analyses require independent data. We have not allowed for a potentially increased dependency between observations made in 2000 and 2001, for example, compared to observations made in 2000 and 2006.
Conclusion
Our analysis of the clinical practice at Ullevål with respect to modes of delivery for women with breech presentation shows that practice may have been influenced by the results of the Term Breech Trial (TBR), which were published in 2000. In 2007 we saw a beginning return to pre-TBT practice, although the percentage share of planned vaginal deliveries never reached the same heights as before the study.
We found a larger percentage share of infants with a low Apgar score at 5 minutes if the mother was in the group selected for a planned vaginal delivery, and if the infant was born before full term. Despite changes in clinical practice during the study period, there was no difference with respect to the number of infants with a low Apgar score when the study period was split into two.
References
1. Bergsjø P, Molne K, Nesheim B-I, eds. Obstetrikk og gynekologi. 3. ed. Oslo: Gyldendal Akademisk; 2015.
2. Veileder i fødselshjelp 2014. Oslo: Den norske legeforening; 2014. Available at: http://legeforeningen.no/Fagmed/Norsk-gynekologisk-forening/Veiledere/Veileder-i-fodselshjelp-2014/(downloaded 25.09.2018).
3. Moster D, Hånes H. Fakta om keisersnitt [Internet]. Oslo: Folkehelseinstituttet; 28.11.2013 [updated 18.11.2015, cited 25.09.2018]. Available at: http://www.fhi.no/artikler/?id=52705.
4. Albrechtsen S, Rasmussen S, Dalaker K, Irgens LM. The occurrence of breech presentation in Norway 1967–1994. Acta Obstetricia et Gynecologica Scandinavica. 1998;77(4):410–5.
5. Øian P, Albrehtsen S, Berge L, Børdahl PE, Egeland T, Henriksen T, et al. Fødsel av barn i seteleie til termin – assistert vaginal fødsel eller keisersnitt? Oslo: Sintef; 2003. SMM-rapport 3/2003. Available at: https://www.fhi.no/globalassets/dokumenterfiler/rapporter/2009-og-eldre/smm-rapporter/smm-rapport_03-03_foedsel_av_barn_-i_seteleie_til_termin.pdf(downloaded 21.06.2019).
6. Hannah ME, Hannah WJ, Hewson SA, Hodnett ED, Saigal S, Willan AR. Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Term Breech Trial Collaborative Group. Lancet. 2000;356(9239):1375–83.
7. Glezerman M. Five years to the term breech trial: the rise and fall of a randomized controlled trial. American Journal of Obstetrics and Gynecology. 2006;194(1):20–5.
8. Bergsjø P. Keisersnitt gjennom 40 år. Norsk Epidemiologi – Norwegian Journal of Epidermiology. 2007;17(2):185–90.
9. Belfrage P, Gjessing L. The term breech presentation. A retrospective study with regard to the planned mode of delivery. Acta Obstetricia et Gynecologica Scandinavica. 2002;81(6):544–50.
10. Albrechtsen S. Vaginal forløsning ved seteleie. Tidsskrift for Den norske legeforening 2010;130(6):589.
11. Helsedirektoratet. Et trygt fødetilbud: Kvalitetskrav til fødselsomsorgen (IS-1877). Oslo: Helsedirektoratet; 2010. Available at: https://www.helsebiblioteket.no/samfunnsmedisin-og-folkehelse/helsefremmende-og-forebyggende-tiltak/retningslinjer-og-veiledere/et-trygt-fodetilbud.kvalitetskrav-til-fodselsomsorgen (downloaded 25.09.2018).
12. Toivonen E, Palomäki O, Huhtala H, Uotila J. Selective vaginal breech delivery at term – still an option. Acta Obstet Gynecol Scand. 2012;91(10):1177.
13. Villar J, Valladares E, Wojdyla D, Zavaleta N, Carroli G, Velazco A, et al. Caesarean delivery rates and pregnancy outcomes: the 2005 WHO global survey on maternal and perinatal health in Latin America. Lancet. 2006;367(9525):1819–29.
14. Cunningham FG, Leveno K, Bloom S, Hauth J, Rouse D. Williams obstetrics. 23. ed. New York: McGraw-Hill Medical; 2010.
15. Casey BM, McIntire DD, Leveno KJ. The continuing value of the Apgar score for the assessment of newborn infants. The New England Journal of Medicine. 2001;344(7):467–71.
16. Folkehelseinstituttet. Årstabeller for Medisinsk fødselsregister 2011. Fødsler i Norge. Oslo: Folkehelseinstituttet; 2013. Available at: https://www.fhi.no/globalassets/dokumenterfiler/moba/pdf/fodsler-i-norge-2011-pdf.pdf(downloaded 14.07.2017).
17. Vistad I, Hustad B, Cvancarova M. Vaginal breech delivery during the last ten years. A prospective registration study. Acta Obstet Gynecol Scand. 2012;91:142-3.
18. Dalaker K. Veileder i fødselshjelp 1998. Oslo: Den norske legeforening; 1998. Available at: https://legeforeningen.no/Fagmed/Norsk-gynekologisk-forening/Veileder-arkiv--utgatte-versjoner/veileder-i-fodselshjelp-1998/(downloaded 25.9.2018).
19. Mattila M, Rautkorpi J, Heikkinen T. Pregnancy outcomes in breech presentation analyzed according to intended mode of delivery. Acta Obstetricia et Gynecologica Scandinavica: 2015;94(10):1103–6.
20. Andreasen S, Nielsen EW, Oian P. Fødselsmetode ved seteleie. Tidsskrift for Den norske legeforening: 2010;130(6):605–8.
21. Goffinet F, Carayol M, Foidart JM, Alexander S, Uzan S, Subtil D, et al. Is planned vaginal delivery for breech presentation at term still an option? Results of an observational prospective survey in France and Belgium. American Journal of Obstetrics and Gynecology. 2006;194(4):1002–11.
22. Taylor LK, Simpson JM, Roberts CL, Olive EC, Henderson-Smart DJ. Risk of complications in a second pregnancy following caesarean section in the first pregnancy: a population-based study. The Medical Journal of Australia. 2005;183(10):515–9.
23. Altman M, Sandstrom A, Petersson G, Frisell T, Cnattingius S, Stephansson O. Prolonged second stage of labor is associated with low Apgar score. European Journal of Epidemiology. 2015;30(11):1209–15.
24. Kok M, Gravendeel L, Opmeer BC, van der Post JA, Mol BW. Expectant parents' preferences for mode of delivery and trade-offs of outcomes for breech presentation. Patient Education and Counseling. 2008;72(2):305–10.
25. Zhu T, Tang J, Zhao F, Qu Y, Mu D. Association between maternal obesity and offspring Apgar score or cord pH: a systematic review and meta-analysis. Scientific Reports. 2015;5:18386.
26. Kharkova OA, Grjibovski AM, Krettek A, Nieboer E, Odland JO. Effect of smoking behavior before and during pregnancy on selected birth outcomes among singleton full-term pregnancy: A Murmansk county birth registry study. International Journal of Environmental Research and Public Health. 2017;14(8):867. DOI: 10.3390/ijerph14080867.
27. Thorngren-Jerneck K, Herbst A. Low 5-minute Apgar score: a population-based register study of 1 million term births. Obstetrics and Gynecology. 2001;98(1):65–70.
28 Vistad I, Klungsoyr K, Albrechtsen S, Skjeldestad FE. Neonatal outcome of singleton term breech deliveries in Norway from 1991 to 2011. Acta Obstetricia et Gynecologica Scandinavica. 2015:94(9):997–1004.
29. Whyte H, Hannah ME, Saigal S, et al. Outcomes of children at 2 years after planned cesarean birth versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004;191(3):864–71.
30. Papile LA. The Apgar score in the 21st century. The New England Journal of Medicine. 2001;344(7):519–20.
31. Locatelli A, Incerti M, Ghidini A, Greco M, Villa E, Paterlini G. Factors associated with umbilical artery acidemia in term infants with low Apgar score at 5 min. European Journal of Obstetrics, Gynecology, and Reproductive Biology. 2008;139(2):146–50.









Comments