Factors affecting functional ability in older patients after hip fracture surgery – implications for tailored nursing interventions
Delirium, an ASA score of 3–4 and not being sent home were associated with reduced functional ability four months after discharge.
Background: Scandinavia has the highest incidence of hip fractures in the world. A significant proportion do not regain their pre-fracture functional ability, and mortality rates are high. Poor functional outcomes and high mortality rates postoperatively can be linked to frailty, comorbidity and complications that can be prevented or reduced by providing the correct nursing care in the hospital setting.
Objective: The objective of the study was to describe the patient group and identify priority areas for quality improvement in nursing care. Research questions: 1) What demographic and clinical factors characterise hip fracture patients at Akershus University Hospital? 2) To what extent do patients regain their previous functional ability four months after surgery? 3) What clinical factors are predictors of change in functional ability in the four months after discharge from hospital?
Method: The study had a quantitative, exploratory and prospective longitudinal design. The sample (N = 131) was made up of hip fracture patients who were admitted to Akershus University Hospital in the period April 2018 to June 2019. We collected clinical data on physical condition (NEWS, ASA), functional ability (Barthel), mobility, cognitive function (IQCODE), pain (NRS) and delirium (4AT, DSM), and performed analyses using descriptive statistics, t-tests and linear regression analyses.
Results: The mean age of participants was 78.2 years (between 51 and 100 years). They mainly lived at home, and 52 per cent were independent before the hip fracture (mean Barthel score of 17.8). About 46 per cent had another serious health condition (ASA 3 or 4). Upon discharge from hospital, the majority were dependent on help (mean Barthel score of 12.1). After four months, their Barthel scores were 1.7 points lower on average than before the fracture. One-third experienced delirium during their hospital stay. The average period of bed rest was two days and nine hours, and the degree of mobilisation was low. Many (seven out of ten) experienced considerable pain the first two days. Delirium, an ASA score of 3–4 and not being sent home were associated with a significant reduction in functional ability four months after discharge.
Conclusion: The study indicates a need for more nursing interventions in the hospital setting in order to better identify and prevent delirium, improve mobility and relieve pain in patients after hip fracture surgery.
Scandinavia has the highest incidence of hip fractures in the world, and hip fractures are a serious public health issue (1–2).
Around 9800 people suffer hip fractures in Norway every year (3), and about 600 of these are operated on at Akershus University Hospital. This patient group mainly consists of older people who have had a ground-level fall and arrive as emergency cases. They often have a reduced general condition, comorbidities and complex physical, mental and social problems (2–6).
International studies show that 40–60 per cent do not regain their pre-fall functioning, and that mortality rates are high. Excess mortality of 20–30 per cent in the first year compared with control populations is reported, especially among the over 80s (5–6).
Poor functional outcomes and high mortality rates after hip fracture surgery are largely related to frailty and comorbidity, but can also be attributed to complications that arise during the disease course (5–7). Some of the main complications among hospital patients are related to the surgery itself, such as delays in surgery of more than 48 hours, and complications during the operation (5–6).
Poor functional outcomes can also be linked to patient-related factors such as delirium, pain, limited mobility and physical rehabilitation as well as prolonged bed rest (7). These complications can be reduced or prevented through proper follow-up during and after the patient’s stay in hospital. Interdisciplinary orthogeriatric follow-up has proven to be very effective (6). Good nursing care, as part of the interdisciplinary follow-up, is crucial (6–12). Low nurse to patient ratios are associated with poorer outcomes (7).
As reflected in the literature review, it is important to know patients’ characteristics in order to be able to tailor the nursing care to the greatest degree possible. This can prevent potentially poor outcomes with both short- and long-term repercussions (5, 8–12). The background for the study was the desire to identify areas where the quality of nursing care for this large and vulnerable group could be improved.
Research questions
We formulated the following research questions:
- What demographic and clinical factors characterise hip fracture patients at Akershus University Hospital?
- To what extent do patients regain their previous functional ability four months after surgery?
- What clinical factors are predictors of change in functional ability in the four months after discharge from hospital?
Method
Design
The study was exploratory and had a prospective longitudinal design.
Sample
We included patients who were admitted as emergency cases at Akershus University Hospital and received hip fracture surgery in the period April 2018 to June 2019, and who could communicate in Norwegian or English. We excluded patients who were not resident in Norway or were in intensive care or an observation ward prior to surgery. A project nurse recruited the participants preoperatively.
Data collection
We assessed factors that could conceivably affect functioning after a hip fracture in the first months after discharge. We assumed that the following factors may be impacted by the nursing care that hospital patients receive, and are therefore particularly relevant from a nursing perspective: an acute confusional state (delirium), extent (number of hours) of bed rest from admission to initial mobilisation, highest degree of mobility during the hospital stay and pain during mobilisation (Numerical Rating Scale, NRS) (0–10) the first two days after surgery.
We further assumed that the patient’s general system stability (measured using the National Early Warning Score [NEWS]) and surgical risk (measured using the American Society of Anesthesiologists’ classification [ASA]) as well as follow-up after discharge (short-term in-patient rehabilitation, long-term in-patient rehabilitation, follow-up at home, no follow-up at home) would have an impact on the outcome of the hip fracture and the surgery, and would therefore have to be mapped.
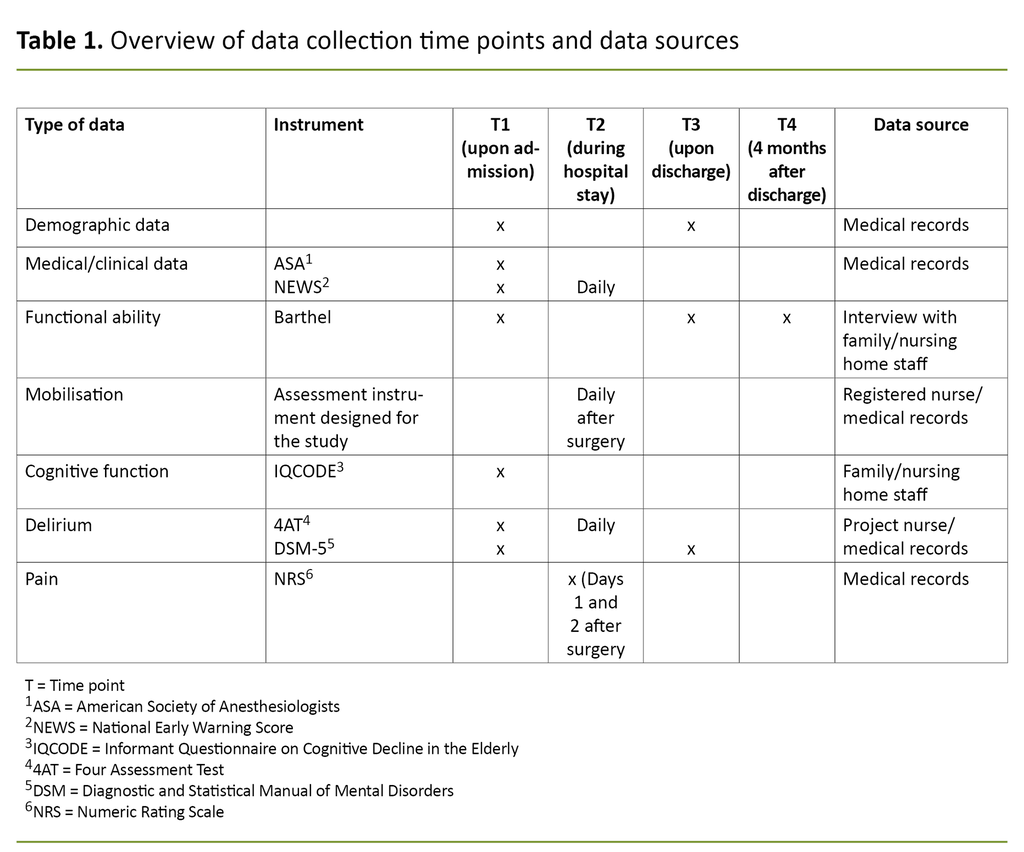
We collected quantitative data at the point of admission and during the hospital stay from medical records and interviews with the patients’ families or others who knew them well. Data were also collected four months after discharge via telephone interviews with family members or nursing home staff. See Table 1 for an overview of data collection times and data sources.
Demographic data
We registered data on age, gender, living conditions, municipal services and whether the patient was discharged to their own home, a rehabilitation unit or a nursing home. The latter was dichotomised for regression analyses as own home versus nursing home or rehabilitation unit.
Clinical data
We registered the diagnosis, type of fracture and comorbidities at the time of admission, as well as ASA and NEWS.
ASA is a system developed by the American Society of Anesthesiologists to classify patients’ physical condition prior to surgery. The system helps assess the risk associated with surgery (13). The patient is assessed by an anaesthesiologist according to this five-category classification system, where 1 indicates a normal healthy patient and 5 is a moribund patient that is not expected to survive 24 hours with or without surgery. In our study, the scores were dichotomised for the regression analysis to 1 + 2 versus 3 + 4. Patients with an ASA score of 5 were not included.
NEWS (National Early Warning Score) is a scoring tool for detecting clinical deterioration in a patient. It measures vital signs such as respiration rate, systolic blood pressure, pulse rate, level of consciousness, temperature and oxygen saturation (14). Each parameter is assessed on a scale from 0 to 3, where 0 indicates a normal value and 1–3 indicates the severity of deviations from the norm – either higher or lower scores than normal. An aggregate score of 1–4 indicates circulatory stability, while a score of 5–6 indicates a need for closer follow-up of the patient’s condition. A score of 7 or more indicates a serious risk of clinical deterioration that requires continuous monitoring of vital signs.
Functional status
The patient’s functional ability was assessed using the Barthel Index for Activities of Daily Living (ADL) (15). This index consists of ten variables that measure the extent to which someone can function independently in relation to ADLs such as bowel and bladder continence, personal hygiene, toilet use, feeding, transferring from bed to chair and back, indoor mobility, dressing, climbing stairs and bathing. The maximum score in the Norwegian version is 20 (completely independent), and the minimum score is 0 (completely dependent on help with basic ADLs).
In cases where the patient was living in a nursing home, we asked their family or a member of staff about the patient's functional ability two weeks before they were admitted to hospital. We also assessed their functional ability upon discharge and four months after surgery via a telephone call with a family member or nursing home staff.
Mobilisation
The date and time of initial postoperative mobilisation was recorded. In addition, we registered the highest degree of mobilisation, measured in the number of metres the patient had walked whilst in hospital. The categories used were ‘not mobilised out of bed’, ‘walked 0-2 metres’, ‘walked 2-10 metres’ and ‘walked over 10 metres’.
Cognitive function
The patient’s cognitive function before the hip fracture was assessed using the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) (16). This screening tool focuses on changes in cognitive function over the past 10 years and is answered by a person who knows the patient well, such as a member of their family or care provider.
The questionnaire consists of 16 variables that describe activities involving cognitive functions, such as memory, learning, reasoning, decision-making and instrumental skills. The maximum score for each variable is 5, which indicates that the patient is much worse than 10 years ago. A score of 3 indicates no change in cognitive function, and a mean score of over 3.5 indicates suspicion of cognitive decline.
Upon admission, we completed the IQCODE via telephone with a family member or someone who knew the patient well. For patients who were long-term nursing home residents, we completed the questionnaire with a member of staff at the nursing home.
Delirium screening
We screened the selected patients daily for delirium using the Four Assessment Test (4AT) and assessed the patient based on the diagnostic criteria for delirium in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) from the American Psychiatric Association. The 4AT is a screening tool for assessing cognitive impairment and delirium in patients, but it is not a diagnostic tool.
The 4AT includes four items: level of alertness, attention, abbreviated mental test, and acute change or fluctuating course. A score of 4 or more indicates possible delirium, and a score of 1–3 indicates possible cognitive impairment. The 4AT has shown a sensitivity of 78 per cent and specificity of 95 per cent in identifying delirium (17).
The DSM system is the most commonly used classification system in psychiatric research. The fifth version, DSM-5, was released in 2013 (18). The diagnostic criteria for delirium in DSM-5 are as follows: A) Disturbance in attention, B) The disturbance develops over a short period of time, C) An additional disturbance in cognition, D) The disturbances are not better explained by a pre-existing, established or evolving neurocognitive disorder, and E) There is evidence that the disturbance is a direct physiological consequence of another medical condition.
All criteria must be met for delirium to be diagnosed. In this study, we defined delirium as a score of 4 or higher in one of the 4AT questionnaires that were completed during admission, and/or meeting the DSM-5 criteria. Project nurses screened the patients on weekdays and completed the questionnaires afterwards based on medical records if they were not present on weekends and public holidays.
Pain
The patients’ pain was recorded daily while they were in hospital. This study uses the results of the pain assessments from the first two days after surgery. A registered nurse (RN) assessed pain using the Numerical Rating Scale (NRS), which consists of a scale from 0–10, where 0 indicates no pain and 10 is the worst pain imaginable (19).
Analysis
The demographic and clinical factors describing the patient group were presented as averages and standard deviations (SD) for continuous variables, and as frequencies and percentages for category variables. Outcome variables were calculated as the Barthel score upon admission minus the score registered four months after discharge.
For example, if the patient had a Barthel score of 6 at admission, and a score of 10 four months after discharge, the change in the Barthel score was -4, with negative values on the outcome variable indicating an increase in independence. Conversely, positive values indicate a decline in physical functioning.
We used a t-test to test whether the change in the Barthel score was significantly different from zero. We also used linear regression analysis to test which predefined covariates were associated with a change in the Barthel score, and estimated both bivariate models and a multiple model. The Akaike information criterion (AIC) was used to reduce the number of redundant covariates in the multiple model.
We used correlation analysis between covariates to screen for multicollinearity problems. Standard statistical tests were used for model diagnostics. We estimated regression models for cases that had no missing values for covariates in the model.
All tests were two-tailed, and results with p-values below 0.05 were considered statistically significant. We performed all statistical analyses in SPSS v26.
Ethics
The study was approved by the Regional Committee for Medical Research Ethics South East Norway (REC South East Norway), reference number 2018/315, and the data protection officer at Akershus University Hospital.
Project nurses obtained written informed consent from the patients. For patients with a known cognitive impairment, or who were delirious at the time of inclusion, consent was obtained from a member of the patient’s family.
Results
Sample
A total of 131 people were included in the study. The mean age was 78.2 years (from 51–100 years) and 66.4 per cent of the participants were women. Just over three-quarters of the patients were living at home when admitted to hospital, and more than half were not users of municipal care services.
The most common diagnoses were cardiovascular disease and endocrinological diseases. About 15 per cent had been diagnosed with dementia. The family’s or care provider’s assessment of the patient’s pre-admission cognitive function indicates no change in cognitive function in the last ten years for most patients. For further details on the sample, see Table 2.
Patients’ functional ability at admission, discharge and after four months
The participants were relatively independent before fracturing their hip, with a mean score of 17.8 (SD 3.6) out of a maximum of 20 on the Barthel Index. As expected, their functional ability declined after surgery, and was 12.1 (SD 5.6) upon discharge, which indicates a need for help with basic self-care. Four months after discharge, functional ability had increased to 16.5 (SD 4.5), which indicates that the average decline between admission and four months after discharge was 1.7 points (SD 3.6) (p <0.001).
Before admission, one-third of the patients were receiving home care services, while 52 per cent were managing without. The other 14.5 per cent were living in a nursing home. After four months, 23.7 per cent were receiving home care services, while 45.8 per cent were living in their own home without any help from the health service. The proportion living in a nursing home had increased to 21.4 per cent.
Clinical factors important for regaining functional ability
Approximately one-third of the patients had experienced delirium during their hospital stay. The average length of bed rest from admission to initial mobilisation was approximately two days and nine hours, but this varied considerably.
The most common degree of mobilisation was walking 0–2 metres, which about a third of the patients had managed. A quarter of the patients had walked a maximum of 2–10 metres, while only a sixth had walked more than 10 metres prior to discharge. One-fifth could only be mobilised while sitting on the edge of the bed or not at all.
For the 96 patients we have data on, the average pain score during mobilisation in the first two days was almost 7, on a scale from 0–10. This indicates that many patients experienced some severe pain in the first 24 hours despite the goal of providing sufficient pain relief.
Participants had a mean maximum NEWS score of 4.9 (SD 2.5) during their hospital stay. In other words, they were close to the limit of 5, which indicates that a rapid response is necessary to prevent clinical deterioration and that close follow-up is therefore needed by an RN and a doctor. Almost half had an ASA score of 3 or 4, which indicates that they were seriously ill prior to fracturing their hip.
The average stay in hospital was 8.4 days (SD 5.1). Most of the patients were transferred to a nursing home, while just over a third were sent home. See further details in Table 3.
Predictors for change in functional ability between discharge and four months later
The bivariate analyses show that pre-surgery delirium and severe illness, which was indicated by an ASA score of 3 or 4, or being discharged to a nursing home or rehabilitation unit, were associated with a significant functional decline – measured using the Barthel Index – between admission and four months after discharge.
According to the multiple model – after the reduction of redundant covariates – several hours of bed rest from the time of admission to the emergency department to initial mobilisation is the only variable associated with significant functional decline between admission and four months later. Although ASA and place of discharge were retained in the model, they do not predict functional decline. No other predictors were retained in the model as a result of the reduction in the number of redundant covariates using AIC. See Table 4 for details.
Discussion
This study shows that patients who are admitted for emergency hip fracture surgery at Akershus University Hospital are older patients who are living at home, more than half of whom were relatively independent before fracturing their hip. Compared with the study by Taraldsen et al. (4) of a similar patient group in Trondheim, our participants were somewhat younger – 78.2 versus 83.4 years.
As in the study by Taraldsen et al. (4), approximately 66 per cent were women. This is consistent with findings in international studies: women have a significantly higher risk of fracturing their hip (20). It may be due to older age and factors such as sarcopenia and osteoporosis, which are more common in women (21, 22).
The participants’ functional ability was somewhat impaired prior to the hip fracture, with a mean score of 17.8 (SD 3.6) on the Barthel Index, which is about the same as the functional ability in the study by Taraldsen et al. (4). Four months after discharge, the mean Barthel score was 16.5 (SD 4.7), which means that most had regained a significant degree of their pre-fracture functional ability.
In comparison, Karlsson et al. (23) found in an intervention study in Sweden that hip fracture patients who underwent intensive rehabilitation scored on average 15 (home rehabilitation) and 16 (hospital rehabilitation unit) three months after surgery, and 17 in both groups after one year. This may indicate that many of our participants received tailored rehabilitation after discharge.
In our sample, we saw an increase in the need for services four months after discharge. The proportion living in a nursing home had increased from 14.5 per cent to 21.4 per cent, and the proportion who were managing without home care services had fallen from 52 per cent to 45.8 per cent. These figures confirm that a hip fracture is a serious condition that can lead to impaired functional ability and a greater need for help (4-6). The figures also show that it is important to put in place tailored interdisciplinary interventions, both at an early stage (6) and as a follow-up measure at a later stage (4).
It is important to systematically assess delirium and pain
Tailored nursing care can reduce delirium, bed rest and pain, and improve postoperative mobility (24–26). The results show that delirium and a long period of bed rest between admission and initial mobilisation is associated with a reduced functional ability four months after discharge. About a third of the patients had delirium during their hospital stay. The study also showed that many experienced severe pain in the first two days after surgery. It is well-documented that pain can contribute to delirium and, conversely, that delirium can affect the ability to self-report pain (27).
This highlights the importance of systematic assessment, both of delirium and pain, and of effective pain relief and other interventions to prevent delirium. Research has shown that delirium often goes undetected or is detected at a late stage, and that hospitals struggle to prevent and treat this condition (28, 29).
This is despite the existence of various effective nursing interventions that reduce the risk of developing delirium (8–12, 24–30), including measures that help to orient the patient in time and space, reduce noise and other disturbing stimuli in the environment, promote sleep, relieve pain, and help ensure a good fluid balance and that information is provided to the patient in advance (8–12, 30).
Mobility can be promoted during pain assessment
On average, participants had 57.3 hours of bed rest between admission to the emergency department and initial mobilisation, but this figure varied from 33 to 81 hours. The degree of post-surgery mobilisation was moderate. Only about one-sixth of the patients had walked over ten metres, while over one-third had walked between zero and two metres. One-fifth had not left their bed, or had only sat on the edge of their bed.
This may be due to several factors, such as a short hospital stay after surgery, generally impaired health (ASA scores 3–4), dementia and/or other underlying conditions. As prolonged bed rest is associated with complications and functional impairment, mobilisation is critical to preventing complications and initiating rehabilitation. Early mobilisation is associated with a reduced risk of death after hip surgery (24), and mobilisation within 36 hours of surgery is therefore the recommended best practice in a recent study from the UK (24).
Mobilisation and pain are often linked. In our sample, participants reported an average NRS score of 7 (out of a maximum of 10) during mobility. Pain is therefore likely to have been a contributing factor to the relatively low degree of mobilisation. In order to promote mobility, preparing for mobilisation by assessing the patient’s pain and offering pain relief within a sufficient time frame before the planned mobilisation are important elements in the nursing care (30).
Furthermore, studies show that early, intensive physical rehabilitation and interdisciplinary rehabilitation that addresses nutrition as well as physical and psychosocial function are important for subsequent mobility and functional ability in older people with hip fractures (24–26). In our sample, being discharged to a nursing home or rehabilitation unit was not associated with improved functional ability after discharge. This can be partly explained by the fact that this category includes the patients with the poorest health and people who need more follow-up, including rehabilitation.
The information we obtained was not precise enough to be able to distinguish between these two groups. The Barthel Index indicates to some extent that a good proportion of our participants recovered considerably during the first four months after discharge, but that many experienced a significant decline in functional ability.
Methodological limitations
A limitation of the study was the relatively small sample, recruited solely from one hospital and the fact that not all relevant patients were included due to insufficient project resources. The relatively small sample has prevented us from further exploring the relevant covariates in more complicated models, such as possible confounders, mediators and moderators.
It is also open to discussion whether it would have been more appropriate for patients who were cognitively intact to self-assess their degree of independence. We chose to ask their families or nursing home staff to assess the functional ability of all patients in order to ensure consistency and comparability.
Conclusion
Implications for clinical nursing
The objective of the study was to identify priority areas for quality improvement in the nursing care of emergency hip fracture patients. In comparisons with existing literature, the study points to several areas that can be developed with a view to improving the prognosis for hip fracture patients.
The study shows the importance of assessing cognitive function and identifying delirium at an early stage. It also shows that a simple screening tool such as the 4AT can be used to assess cognitive function in order to identify delirium (31). A range of established measures exist that can prevent or reduce delirium (7–12, 24–30).
A quality improvement project at Akershus University Hospital has shown that there is insufficient awareness or systematic assessment of patients at risk of delirium in medical and surgical wards. As part of the project, we developed and tested a suggested treatment plan to increase efforts to screen and implement interventions at an early stage in order to prevent or reduce delirium (32).
The results also show that RNs should have a greater focus on pain relief in connection with mobilisation, on early mobilisation and on increasing the degree of mobilisation. These are resource-intensive nursing tasks, especially in relation to geriatric patients with comorbidities (27), like those in our sample. A good nurse to patient ratio is therefore important for ensuring sufficient intensive follow-up of this patient group during their relatively short stay in hospital, which averages 8.4 days (6, 27).
The literature also shows that early and intensive physiotherapy is crucial to the patient’s outcome. A close collaboration between physiotherapists and RNs will ensure that patients get the most out of rehabilitation (6, 27), which is particularly important if patients do not receive intensive interdisciplinary rehabilitation in the primary health service after discharge.
Future research
A national study with a larger, representative sample would strengthen generalisability and make it possible to investigate more complex relationships between covariates and to include other relevant characteristics such as the importance of staffing levels.
A follow-up study of RNs’ knowledge about delirium, pain relief etc. in orthopaedic wards could uncover knowledge gaps and help to tailor the implementation of improvement measures.
We would like to thank project nurses Sofie Høen, Eline Elshaug Schønneberg and Tine Johnsen Karlsrud who contributed in the start-up phase of the project by devising a project plan. They were also involved in the data collection. We would also like to thank Mia Charlotte Emilsen, who contributed to the data collection.
The authors report no conflicts of interest.
References
1. Forsén L, Søgaard AJ, Holvik K, Meyer HE, Omsland TK, Stigum H, et al. Geographic variations in hip fracture incidence in a high-risk country stretching into the Arctic: a NOREPOS study. Osteoporos Int. 2020;31(7):1323–31. DOI: 10.1007/s00198-020-05346-8
2. Hagen G, Magnussen J, Tell G, Omsland T. Estimating the future burden of hip fractures in Norway. A NOREPOS study. Bone. 2020;131:115156. DOI: 10.1016/j.bone.2019.115156
3. Nasjonal kompetansetjeneste for leddproteser og hoftebrudd [Internet]. Bergen: Helse Bergen, Haukeland universitetssjukehus [updated 10.05.2022, cited 11.05.2022]. Available at: https://helse-bergen.no/nasjonal-kompetansetjeneste-for-leddproteser-og-hoftebrudd
4. Taraldsen K, Thingstad P, Døhl Ø, Follestad T, Helbostad JL, Lamb SE, et al. Short and long-term clinical effectiveness and cost-effectiveness of a late-phase community-based balance and gait exercise program following hip fracture. The EVA-Hip Randomised Controlled Trial. PLoS One. 2019;14(11):e0224971. DOI: 10.1371/journal.pone.0224971
5. Rapp K, Büchele G, Dreinhöfer K, Bücking B, Becker C, Benzinger P. Epidemiology of hip fractures: systematic literature review of German data and an overview of the international literature. Z Gerontol Geriatr. 2019;52(1):10–6. DOI: 10.1007/s00391-018-1382-z
6. Rapp K, Becker C, Todd C, Rothenbacher D, Schulz C, König HH, et al. The association between orthogeriatric co-management and mortality following hip fracture. Deutsches Arzteblatt International. 2020;117(4):53–9. DOI: 10.3238/arztebl.2020.0053
7. Xu BY, Yan S, Low LL, Vasanwala FF, Low SG. Predictors of poor functional outcomes and mortality in patients with hip fracture: a systematic review. BMC Musculoskelet Disord. 2019;20(1):568. DOI: 10.1186/s12891-019-2950-0
8. Allsop S, Morphet J, Lee S, Cook O. Exploring the roles of advanced practice nurses in the care of patients following fragility hip fracture: a systematic review. Journal of Advanced Nursing. 2021;77(5):2166–84. DOI: 10.1111/jan.14692
9. Flaherty JH, Yue J, Rudolph JL. Dissecting delirium: phenotypes, consequences, screening, diagnosis, prevention, treatment, and program implementation. Clinics in Geriatric Medicine. 2017;33(3):393–413. DOI: 10.1016/j.cger.2017.03.004
10. Inouye SK. Delirium – a framework to improve acute care for older persons. Journal of the American Geriatrics Society. 2018;66(3):446–51. DOI: 10.1111/jgs.15296
11. Sinha SK, Bennett J, Ramsden R, Bon J, Chalk T. Delivering improved patient and system outcomes for hospitalized older adults through an Acute Care for Elders Strategy. Healthcare Management Forum. 2018;31(4):126–32. DOI: 10.1177/0840470418773108
12. Hshieh TT, Yang T, Gartaganis SL, Yue J, Inouye SK. Hospital elder life program: systematic review and meta-analysis of effectiveness. The American Journal of Geriatric Psychiatry. 2018;26(10):1015–33. DOI: 10.1016/j.jagp.2018.06.007
13. Doyle DJ, Goyal A, Bansal P, Garmon EH. American Society of Anesthesiologists Classification. Treasure Island, Florida: StatPearls Publishing; 2022.
14. Lee YS, Choi JW, Park YH, Dong CC, Park I, Lee JE, et al. Evaluation of the efficacy of the National Early Warning Score in predicting in-hospital mortality via the risk stratification. Journal of Critical Care. 2018;47:222–6. DOI: 10.1016/j.jcrc.2018.07.011
15. Mahoney, FI, Barthel DW. Functional evaluation: The Barthel Index: a simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Maryland State Medical Journal. 1965;14:61–5.
16. Harrison JK, Fearon P, Noel‐Storr AH, McShane R, Stott DJ, Quinn TJ. Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) for the diagnosis of dementia within a secondary care setting. The Cochrane Collaboration; 2015. Available at: https://www.journalslibrary.nihr.ac.uk/downloads/other-nihr-research/cochrane-programme-grants/Informant-Questionnaire-on-Cognitive-Decline-in-the-Elderly-for-the-diagnosis-of-dementia-within-a-secondary.pdf (downloaded 16.07.2021).
17. MacLullich AM, Shenkin SD, Goodacre S, Godfrey M, Hanley J, Stíobhairt A, et al. The 4 'A's test for detecting delirium in acute medical patients: a diagnostic accuracy study. Health technology assessment. 2019;23(40):1–194. DOI: 10.3310/hta23400
18. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM–5). Washington DC: American Psychiatric Publishing; 2013. Available at: https://www.psychiatry.org/psychiatrists/practice/dsm (downloaded 17.07.2021).
19. Wood BM, Nicholas MK, Blyth F, Asghari A, Gibson S. Assessing pain in older people with persistent pain: The NRS is valid but only provides part of the picture. The Journal of Pain. 2010;11(12):1259–66. DOI: 10.1016/j.jpain.2010.02.025
20. Lobo L, Marcos G, Santabárbara J, Salvador-Rosés H, Lobo-Escolar L, De la Cámara C, et al. Gender differences in the incidence of and risk factors for hip fracture: a 16-year longitudinal study in a southern European population. Maturitas. 2017;97:38–43. DOI: 10.1016/j.maturitas.2016.12.009
21. Di Monaco M, Vallero F, Di Monaco R, Tappero R. Prevalence of sarcopenia and its association with osteoporosis in 313 older women following a hip fracture. Archives of Gerontology and Geriatrics. 2011;52(1):71–4. DOI: 10.1016/j.archger.2010.02.002
22. Salech F, Marquez C, Lera L, Angel B, Saguez R, Albala C. Osteosarcopenia predicts falls, fractures, and mortality in Chilean community-dwelling older adults. Journal of the American Medical Directors Association. 2021;22(4):853–8. DOI: 10.1016/j.jamda.2020.07.032
23. Karlsson Å, Lindelöf N, Olofsson B, Berggren M, Gustafson Y, Nordström P, et al. Effects of geriatric interdisciplinary home rehabilitation on independence in activities of daily living in older people with hip fracture: a randomized controlled trial. Arch Phys Med Rehabil. 2020;101(4):571–8. DOI: 10.1016/j.apmr.2019.12.007
24. Sheehan KJ, Goubar A, Almilaji O, Martin FC, Potter C, Jones GD, et al. Discharge after hip fracture surgery by mobilisation timing: secondary analysis of the UK National Hip Fracture Database. Age and Ageing. 2021;50(2):415–22. DOI: 10.1093/ageing/afaa204
25. Handoll HHG, Sherrington C, Mak JCS. Interventions for improving mobility after hip fracture surgery in adults. Cochrane Database of Systematic Reviews. 2011;16(3):CD001704. DOI: 10.1002/14651858.CD001704.pub4
26. Stott DJ, Handoll HH. Rehabilitation of older people after hip (proximal femoral) fracture. Cochrane Database of Systematic Reviews. 2011;(3):1465–1858. DOI: 10.1002/14651858.ED000023
27. Sampson EL, West E, Fischer T. Pain and delirium: mechanisms, assessment, and management. Eur Geriatr Med. 2020;11:45–52. DOI: 10.1007/s41999-019-00281-2
28. Evensen S, Saltvedt I, Ranhoff AH, Myrstad M, Myrstad C, Mellingsæther M, et al. Delirium og kognitiv svikt blant eldre i norske akuttmottak. Tidsskrift for Den norske legeforening. 13.03.2019. DOI: 10.4045/tidsskr.18.0578
29. Kolanowski A. Delirium in people living with dementia: a call for global solutions. Aging & Mental Health. 2018;22(4):444–6. DOI: 10.1080/13607863.2016.1244805
30. Brent L, Hommel A, Maher AB, Hertz K, Meehan AJ, Santy-Tomlinson J. Nursing care of fragility fracture patients. Injury. 2018;49(8):1409–12. DOI: 10.1016/j.injury.2018.06.036
31. Berg GV, Watne LO, Gjevjon ER. Ny screening gir sikrere diagnose. Sykepleien. 2016;104(3):52–3. DOI: 10.4220/Sykepleiens.2016.56686
32. Weldingh N, Mellingsæter M, Hegna B, Benth JS, Einvik G, Juliebø V, et al. Impact of a dementia-friendly program on detection and management of patients with cognitive impairment and delirium in acute-care hospital units: a controlled clinical trial design. BMC Geriatr. 2022;22:artikkelnr. 266. DOI: 10.1186/s12877-022-02949-0













Comments