Infection prevention in the community nursing service: experiences of nursing managers and nursing consultants
Local procedures are useful, but not sufficient to comply with the Standard Precautions in the community nursing service. There is therefore a need to develop national guidelines.
Background: Standard Precautions are the infection prevention measures that should be performed in all patient contact in the health sector. Although the requirement for professional standards of practice is based on the Health Personnel Act and regulations on management and quality improvement in the health service, the regulations on infection control in the health service do not include any specific requirements in relation to infection control in home-based nursing care. There are few Norwegian studies on infection control practices in the community nursing service, but international research indicates that there is a need for such procedures in health services provided in private homes. Patients receiving home-based nursing care can also be exposed to infections associated with treatment in institutions. During the COVID-19 pandemic, the prevention of infection in the vulnerable user group receiving home-based nursing care has become extremely important. Infrastructure, management, time pressure, staffing levels, knowledge and risky behaviours among staff are all factors that seem to affect compliance with Standard Precautions.
Objective: We wanted to explore nursing managers’ and nursing consultants’ experiences with infection prevention in the community nursing service.
Method: This is a qualitative study, and the data material is based on in-depth interviews with eight participants from the municipal administration in two Norwegian local authorities. We conducted the interviews in the period October 2019 to March 2020 – before and after the COVID-19 pandemic had hit Norway. We analysed the data using Braun and Clarke’s thematic analysis method.
Results: Standard Precautions were devised locally for the community nursing service in both municipalities, but the degree of implementation in the training of new staff varied. The introduction of work clothes, new premises, risk mapping and targeted training facilitated compliance with these procedures. However, the participants found that lack of knowledge, time pressure, low staffing levels and high staff turnovers were all barriers to compliance. Participants found that procedures and guidelines were not always adapted to the home nursing context.
Conclusion: The study generates new insight into nursing managers’ and nursing consultants’ experiences of infection control efforts in the community nursing service. There is a need for further research in this area. We suggest mapping nurses’ experiences across municipalities and counties in order to identify the need for procedures and national guidelines that are tailored to the community nursing service.
The modern-day community nursing service is a complex service that requires interaction between many different actors. The patient and user groups are growing, and the need for help varies considerably across all ages (1). The number of users under the age of 67 is increasing the most, but older people nevertheless constitute a significant part of the user group (2) that is particularly prone to infections (3, p. 28).
Among recipients of nursing and care services, 90% have four to five diseases (4). Patients in hospitals and institutions can be exposed to healthcare-associated infections (HAIs). However, research shows that HAIs also pose a threat to patient safety in home-based nursing care (5–7).
In Sweden, the Global Trigger Tool method was used in a study to scan medical records for adverse events among patients. The researchers found that HAIs were a frequent cause of adverse events in community nursing services (5). National studies in the United States suggested that infections that occurred while patients were receiving home-based nursing care were a common cause of hospitalisation (6, 7).
A study of community nursing agencies in the United States that was conducted during the COVID-19 pandemic showed that responsibility for infection control was added to the workload. A third of those responsible for infection control had no formal training in this area. Urban areas were more likely to have someone in charge of infection control than rural areas (8).
When the pandemic reached Norway, the Norwegian Institute of Public Health (NIPH) published advice to prevent infection in Norwegian community nursing services (9). Standard Precautions must be followed in all patient contact in the health service in order to prevent known and unknown infections.
The procedures include hand hygiene, cough etiquette, patient placement, personal protective equipment (PPE), handling of equipment used by patients, cleaning and disinfection, waste management, handling of bedding and textiles, safe injection practices, disinfection of skin and protection against sharps injuries (10).
In the publication ‘Situational description of infection control in Norway’, the NIPH states that little is known about infection control practices in Norwegian community nursing services (11). Studies from the Swedish community nursing service revealed that time pressure and low staffing levels were barriers to compliance with Standard Precautions (12, 13).
A systematic literature review showed that factors that could affect compliance were lack of necessary equipment, lack of space, type of patient contact and insufficient training and knowledge (14, 15). However, organisational campaigns had a positive impact on attitudes and behaviours related to infection control and prevention (15).
We have found a few Norwegian qualitative studies that describe the factors for infection control compliance. In a focus group study, community nurses reported that there were a lack of up-to-date procedures in the community nursing service and that this was not a priority of the managers (16).
In a study based on a survey of healthcare personnel in nursing homes and the community nursing service, staffing levels were regarded as a risk factor for patient safety (17).
A report (18) on staffing and qualifications in the community nursing service and nursing homes showed that registered nurses and nursing associates on sick leave were being replaced by unskilled personnel. Up to 22% of the shifts of absent nursing personnel were covered by unskilled workers. The proportion of unskilled personnel was particularly high on weekends, in the evenings and during holiday periods (18).
The regulations on infection control in the health service do not include any specific requirements in relation to infection control in the community nursing service (19), but the Health Personnel Act and the regulations on management and quality improvement in the health service set a requirement for a professional standard of practice (20, 21).
The NIPH’s infection control guide on the prevention and control of infectious diseases is also clear that Standard Precautions must be followed in all patient contact in the health service (3, 10).
The purpose of this study was to explore the experiences of nursing leaders and nursing consultants in relation to procedures and practices formulated at municipal level, as well as the needs and challenges they identified in connection with Standard Precautions.
Method
The study had a qualitative descriptive design (22) and included in-depth interviews with registered nurses working in the administration of community nursing services, and with the infection control public health nurse from the local authority’s infection control group. As the use of Standard Precautions in the community nursing service is an under-researched area, we wanted to take a broad approach to exploring the experiences of community nursing staff.
Interviews
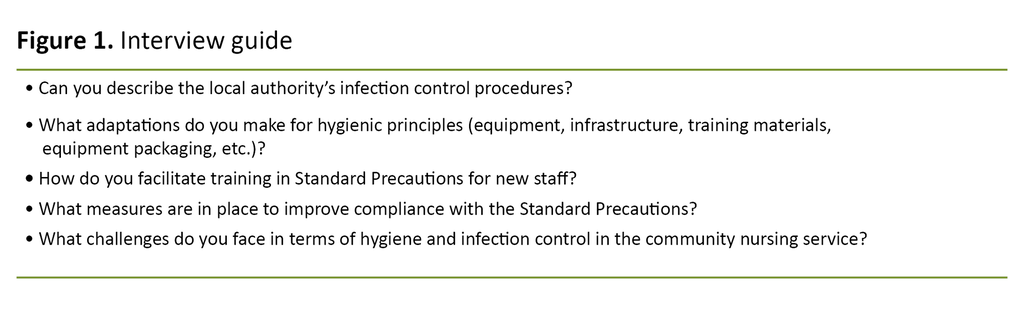
The questions in the semi-structured interview guide related to practices and staff training in Standard Precautions (Figure 1). The guide was based on previous research on compliance with infection control (14, 15, 23, 24).
The survey was based on seven in-depth interviews with eight participants. One of the interviews was conducted with two participants together, in line with their own wishes. The interviews lasted between 40 and 70 minutes.
The first four interviews were conducted at the participants’ workplaces, while the remaining three were telephone interviews due to COVID-19 restrictions during the first lockdown in March 2020. All of the interviews were conducted by the first author, who was a master’s student at the time.
We tested the interview guide on colleagues in the community nursing service and made adjustments to it before starting the study. The interviewer was a woman with a background in home-based nursing care, just like the participants.
Recruitment and sample
The Centre for Development of Institutional and Home Care Services assisted with recruitment for the study. Three host local authorities received an email invitation, two of which agreed to participate. The participating municipalities have relatively large populations, several community nursing districts and a central infection control group.
The local authorities used an electronic quality management system for local infection control procedures. The ‘snowball method’ was used to recruit participants for the study, i.e. someone who had already agreed to take part helped recruit colleagues with relevant experience (22).
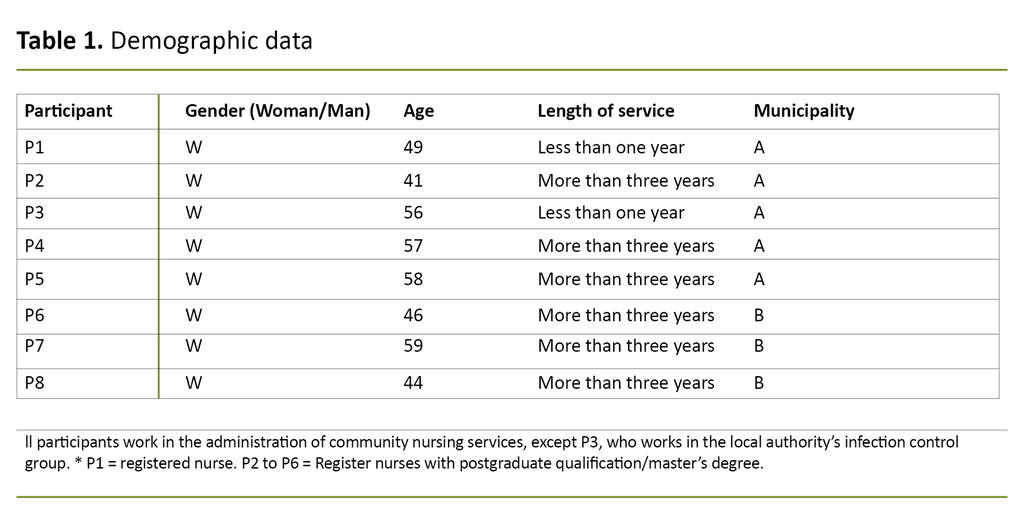
The sample consisted of nursing consultants, a nursing manager and an infection control public health nurse (Table 1). They were informed about the purpose of the study and the interviewer’s background from the community nursing service.
The interviews were relatively long, and the participants provided rich information. The interviews were conducted in the period October 2019 to March 2020. The participants’ experiences were therefore affected by the situation before and after the first lockdown as a result of the COVID-19 pandemic.
Analysis
The first author made audio recordings of the interviews and transcribed these. Both authors participated in the data analysis. We used Braun and Clarke’s thematic analysis to identify codes and themes of meaning units in the transcripts across the entire dataset, and identified patterns that elucidated the research questions.
We repeated the analysis process several times before arriving at the final themes and sub-themes (Table 2) (25).
Ethics
Before starting the study, we performed a risk and vulnerability analysis to plan the management of sensitive personal data in audio files and documents in accordance with Oslo Metropolitan University’s guidelines (26). We reported the study to the Norwegian Centre for Research Data (NSD) and received approval on 19 September 2019 (reference number 262833).
The participants were given details of the study and were informed that they could withdraw without giving a reason. They were also told that the information they provided would be de-identified. All participants provided written consent to participate in the study.
Results
The analysis of the study participants’ experiences with facilitating Standard Precautions in the community nursing service resulted in two main themes and four sub-themes.
Procedures and training of new staff
The participants’ infection and hygiene practices were largely related to the use of existing procedures as well as the need for training of new staff. They also expressed a need for training in disposable PPE.
Procedures are only part of the solution
Infection control procedures in the community nursing service differed between the municipalities. The participants in one municipality helped devise the Standard Precautions during their postgraduate training, under the direction of their employer. In the other municipality, the Standard Precautions were devised by a central infection control group.
The participants considered the development of the procedures to be a step in the right direction, and that ‘hand hygiene day’ – a day when hand hygiene is particularly emphasised – helped increase the focus on infection prevention through hand washing. Several participants also stressed that they were dependent on close cooperation with local managers in order to be able to implement the procedures according to plan.
Some participants expressed frustration over the lack of national guidelines.
Some participants expressed frustration over the lack of national guidelines and the fact that few of the local procedures are adequately adapted to home-based nursing care. One participant described a situation in which she sought advice from the specialist health service:
‘If you call infection control at the hospital and say: “We’re going to give subcutaneous injections”, they respond, “They should be in a yellow bucket at the user’s home”. “What are we supposed to do with the yellow buckets?” “Bring them to the office.” But we don’t have any more deliveries for the office. Missing the mark really. So we put them in transparent plastic bottles at the users’ homes. I mean, it’s their home (P4).’
Several of the participants considered the advice given to the community nurses to be challenging due to the lack of standardised infection control. They were often asked what kind of equipment should be used and stored in the users’ homes. Sometimes new issues arose, such as how to deal with laundry from someone with resistant bacteria in a communal laundry facility.
Inconsistent training
Most participants said that Standard Precautions were part of the training to a greater or lesser degree. Training checklists provided the framework for the content. New staff were also given information about the procedures to read through.
One participant said that infection control had not been covered to any great extent in the training: ‘I actually checked the training checklist before you arrived, and it doesn’t say nothing about hygiene. There is far too little focus on this. We receive training twice a year, but far from everyone participates.’ (P2).
Several of the participants did not consider the training of unskilled personnel to be adequate. One participant had tried to adapt the training for this group:
‘We have drawn up a training checklist for unskilled assistants which only covers training that this particular group needs. The temporary staff also receive a three-hour training session that includes hygiene among other things. I use an Excel spreadsheet to provide an overview of the training given.’ (P8)
Another participant said that the community nursing service prepared for COVID-19 with training in and repetition of infection control procedures in order to reassure the staff. However, several participants pointed out that the training was given orally and in writing, but that there was no practical training in hand hygiene.
Organisational aspects that affect compliance
Insufficient time with service users, low staffing levels and fewer skilled staff on duty in the evenings and on weekends were often barriers to compliance with Standard Precautions. The use of temporary staff reduced the continuity of the service, and infection control procedures had not been practised consistently. Thorough routines were needed to ensure that those without access to medical records were informed about infection.
A complex service with time pressure and low staffing levels
The participants considered the tight constraints on the time they could spend with patients to be a barrier to thorough hand hygiene among the staff. Staff cuts also led to vacant shifts in the evenings and on weekends:
‘Some of the department heads have said repeatedly at management meetings “I can’t vouch for the staff on weekend shifts – I often go home with my heart in my mouth on Fridays”. Few of the staff on evening and weekend shifts are skilled.’ (P6).
One participant said that many of the staff were temporary. This made it difficult to have permanent resource persons with responsibility for professional development and quality assurance and such like. In the past, a specialist consultant had responsibility for an entire district, but it became difficult to follow up all of the community nursing groups sufficiently.
The local community nursing groups also had a department head and an assistant department head. In order to ensure better quality, the assistant department heads now have a professional advisory function in relation to the local community nursing groups which supplements the role of the department heads.
Some consultants found that those with a professional advisory function did not always receive the necessary information. Several also noted that it was difficult to provide partners, such as home helps and ambulance personnel, information about infection, as they did not have access to medical records.
Room for improvement
Several participants reported that they had been given modern premises that were better adapted to the community nursing service. Work clothes had been introduced in both municipalities, and the participants felt that this helped to increase the staff’s focus on Standard Precautions.
The participants found the staff to be diligent about hygiene, but also described what they referred to as risky behaviours and bad habits: ‘When you see nurses with long nails or wearing rings, it seems like an absolute crisis to me’ (P6).
Several participants had received feedback from staff that disposable PPE had been used several times. The misuse and overuse of gloves also came up in several conversations. Feedback from trainees indicated that the differing practices among staff caused confusion.
Hand washing was not possible in all homes as hygienic conditions varied, and soap and paper towels were not always available.
One participant said that they had put the spotlight on the home helps’ knowledge: ‘We’ve had more focus on the home helps, as they tend to visit the same homes as the community nurses. We discovered that they did not have the knowledge we thought they had, particularly in relation to the use of gloves. They have now been given the right type of gloves and been shown films about the correct use of gloves and hand hygiene.’ (P8).
The participants described the cleaning of reusable equipment, especially weekly dosette boxes, as impractical due to the material and design of the boxes and the lack of a suitable place to do this. Hand washing was not possible in all homes as hygienic conditions varied, and soap and paper towels were not always available.
All participants tended to have good access to gloves and other PPE, but it had to be rationed during the COVID-19 pandemic. The participants who were interviewed during the pandemic considered infection control to be better than ever, and saw more commitment to infection control among managers. Standard Precautions were also incorporated into the community nursing service’s risk mapping in one district.
Discussion
The main finding of this study is that the participants considered the local procedures in the community nursing service to be a useful tool in the compliance of Standard Precautions, but that the procedures had limitations.
This can be viewed in conjunction with the participants’ statements about unsystematic infection control efforts and inadequate training of new staff. These accounts are consistent with findings from other studies (12–14, 23).
Participants had access to procedures
Several of the participants in our study said that they had access to up-to-date clinical Standard Precautions. Those who had been involved in devising these procedures found them useful, while others felt that the content was more suitable for institutions and not well adapted for home-based nursing care.
The participants also pointed out the need for national guidelines for home-based nursing care. The challenges of infection control in home-based nursing care were also reported in the US study by Shang et al., which shows that responsibility for infection control, particularly during the COVID-19 pandemic, came on top of the many other tasks of community nurses.
Several of the participants in our study said that they had access to up-to-date clinical Standard Precautions.
Infection control also tended to be a more clearly defined area of responsibility in the towns than in less central areas (8). Although the participants in our study said that the participating local authorities had clinical procedures in place, it is important to remember that not all Norwegian local authorities have adapted clinical procedures for infection control, as practices vary (8, 11).
Community nurses can also experience a lack of procedures and guidelines (16). There are therefore strong indications that standardised national guidelines are needed.
Implementing new procedures is a large undertaking
Standardised health care enables the health authorities to reduce undesirable variation in patients’ health care. This is particularly important in view of the risk that clinical procedures are not implemented due to the failure to adapt the content to the needs of the service area or the patient (27).
Stubberud points out that implementing procedures is a large undertaking. In order to create lasting change, the local authorities should have an implementation plan that is approved at management level. Barriers and resistance to change should also be identified (27).
Changes as a result of improvement processes must be coordinated within the organisation, and the infrastructure should be sufficient to support these changes (27). The participants in our study also emphasised the importance of the managers being involved in the introduction of infection control procedures.
The community nursing service management plays a key role in implementing practices and procedures (28), but updating procedures is not a priority task (16). In the work to improve infection control procedures, it is therefore important for managers to be involved in their introduction and to ensure good practices and training of staff.
They must also realise the value of supporting improvement processes. In Sweden and the United States, researchers have mapped infections that occurred during home-based nursing care, and it was found that such infections were a threat to patient safety in home-based nursing care. These infections impaired the health of patients, increased hospital admissions and caused an unnecessary strain on the health service (5–7).
Quality improvements aimed at developing good infection control procedures and protecting patient safety in home-based nursing care can therefore be crucial in the future, particularly with the increasing multimorbidity of patients and scarcity of resources (4).
Difficult to comply with Standard Precautions
In addition to the challenges of adapting clinical procedures and the lack of national guidelines, compliance with the Standard Precautions was a key issue that the participants highlighted in our study. The participants said that use of the procedures was facilitated and focussed on to some extent, but time pressure, low staffing levels and high staff turnovers were often a barrier to compliance.
The participants said that use of the procedures was facilitated and focussed on to some extent, but time pressure, low staffing levels and high staff turnovers were often a barrier to compliance.
They also found that lack of skills and risky behaviours among staff also represented a barrier to compliance. Qualitative studies by Kaya (12) and Karlsson (13) also showed that time pressure prevented compliance with the procedures in the community nursing service due to the already heavy workload (12, 13).
This is consistent with findings in studies from other health service settings (14, 23). According to the Norwegian Institute of Public Health (NIPH), little is known about compliance levels within infection control in the community nursing service (11). Risk factors for low compliance in the community nursing service do, however, exist, as has been documented in several Norwegian studies (16–18).
Evening and weekend personnel mostly unskilled
Evenings and weekends are particularly vulnerable times, as many of the shifts are covered by less skilled personnel. Kaya and Nordin (12) indicated that employing temporary staff was important for preventing work overload on staff over time. The staff were mostly competent, but the skill levels were described as problematic, particularly in the summer when many of the staff were temporary. Participants regarded low skill levels and lack of interest in Standard Precautions as a threat to patient safety (12).
Community nurses in Norway have also previously expressed such a concern (16). The reality is that the staffing level of unskilled workers is often twice as high as planned for in the Norwegian community nursing service (18). Ensuring that all staff in the community nursing service have sufficient knowledge of Standard Precautions and a safe environment is therefore a crucial part of the infection prevention work (14, 15, 23, 24).
Compliance with Standard Precautions in the community nursing service is dependent on factors other than the actual procedures. Management responsibility and a working environment that permits the prioritisation of infection control are crucial.
Strengths and limitations of the study
The interviewer’s background in the community nursing service led to understanding in the interviews with the participants. The co-author has experience from various parts of the primary healthcare service, which has enabled useful interpretations of the data material.
One of the strengths of the study is its practical approach to topical issues that have been under-researched, particularly with regard to the data collection in the middle of the COVID-19 pandemic. The participants represented different districts in the two municipalities in the study and thus helped form a more nuanced picture of the community nursing service.
Both authors reviewed the analysis and transcripts, and they discussed categories and themes, which strengthens the validity of the study (22).
The first interviews were conducted pre-lockdown and the last ones were conducted during the pandemic. The answers would probably be somewhat different if everyone had been interviewed in the same time frame. This assumption is strengthened by the fact that the last informants made a distinction between the time before and the time ‘after’ the pandemic.
Conclusion
This study shows that nursing managers and nursing consultants consider infection control in the community nursing service to have improved, but that they are still inadequate in many areas.
A lack of national guidelines for Standard Precautions in the community nursing service, practices that do not meet the needs of home-based nursing care, inadequate staff training, insufficient time with users, low staffing levels, high staff turnovers are all barriers to compliance with Standard Precautions, and can pose a threat to patient safety.
We propose mapping the community nursing service at the national level in order to identify the need for procedures and guidelines that are suitable for home-based nursing care. One such example is surveys across municipalities and counties.
References
1. Holm SG, Wiik H. Bo lenger hjemme: nye utfordringer for hjemmetjenesten. 1st ed. Bergen: Fagbokforlaget; 2020.
2. Bergsagel I. Stadig flere mottar hjemmesykepleie. Sykepleien; 2020. Available at: https://sykepleien.no/2020/06/stadig-flere-mottar-hjemmesykepleie (downloaded 10.11.2020).
3. Akselsen PE. Smittevern i helsetjenesten. 3rd ed. Oslo: Gyldendal; 2018.
4. Grimsmo A, Løhre A, Røsstad T, Gjerde I, Heiberg I, Steinsbekk A. Disease-specific clinical pathways – are they feasible in primary care? A mixed-methods study. Scand J Prim Health Care. 2018;36(2):152–60. DOI: 10.1080/02813432.2018.1459167
5. Schildmeijer KGI, Unbeck M, Ekstedt M, Lindblad M, Nilsson L. Adverse events in patients in home healthcare: a retrospective record review using trigger tool methodology. BMJ Open. 2018;8(1). DOI: 10.1136/bmjopen-2017-019267
6. Shang J, Larson E, Liu J, Stone P. Infection in home health care: results from national Outcome and Assessment Information Set data. Am J Infect Control. 2015;43(5):454–9. DOI: 10.1016/j.ajic.2014.12.017
7. Shang J, Wang J, Adams V, Ma C. Risk factors for infection in home health care: analysis of national Outcome and Assessment Information Set data. Research in Nursing & Health. 2020;43(4):373–86. DOI: 10.1002/nur.22053
8. Shang J, Chastain AM, Perera UGE, Dick AW, Fu CJ, Madigan EA, et al. The state of infection prevention and control at home health agencies in the United States prior to COVID-19: a cross-sectional study. International Journal of Nursing Studies. 2021;115:1–10. DOI: 10.1016/j.ijnurstu.2020.103841
9. Folkehelseinstituttet (FHI). Råd ved helse- og omsorgstjenester i privat bolig og private hjem i samlokaliserte omsorgsboliger mv. Oslo: FHI; 2021. Available at: https://www.fhi.no/nettpub/coronavirus/helsepersonell/tiltak-i-hjemmetjenesten (downloaded 23.09.2021).
10. Folkehelseinstituttet (FHI). Basale smittevernrutiner i helsetjenesten – veileder for helsepersonell. Oslo: FHI; 2019. Available at: https://www.fhi.no/nettpub/smittevernveilederen/temakapitler/09.-basale-smittevernrutiner-i-hels/ (downloaded 02.05.2019).
11. Folkehelseinstituttet (FHI). Situasjonsbeskrivelse av smittevern i Norge. Oslo: FHI; 2018. Available at: https://www.fhi.no/publ/2018/situasjonsbeskrivelse-av-smittevern-i-norge/ (downloaded 10.05.2019).
12. Kaya A, Nordin A. Patientsäkerhet i den kommunala hemsjukvården – utifrån distriktssköterskors erfarenheter [masteroppgave]. Borås: Högskolan i Borås; 2018.
13. Karlsson E, Vilner H. «Inte byta bakterieflora mellan stugorna på bygden» – Distriktssköterskors erfarenheter om den hygieniska aspekten i samband med sårvård i hemmen [Master's Thesis]. Borås: Högskolan i Borås; 2014.
14. Porto JS, Marziale MHP. Reasons and consequences of low adherence to standard precautions by the nursing team. Revista gaucha de enfermagem. 2016;37(2):e57395.
15. Sax H, Uçkay I, Richet H, Allegranzi B, Pittet D. Determinants of good adherence to hand hygiene among healthcare workers who have extensive exposure to hand hygiene campaigns. Infection Control & Hospital Epidemiology. 2015;28(11):1267–74. DOI: 10.1086/521663
16. Berland A, Holm AL, Gundersen D, Bentsen SB. Patient safety culture in home care: experiences of home-care nurses. Journal of Nursing Management. 2012;20(6):794–801. DOI: 10.1111/j.1365-2834.2012.01461.x
17. Ree E, Wiig S. Employees’ perceptions of patient safety culture in Norwegian nursing homes and home care services. BMC Health Serv Res. 2019;19:607. DOI: 10.1186/s12913-019-4456-8
18. Gautun H. En utvikling som må snus. Bemanning og kompetanse i sykehjem og hjemmesykepleien. Oslo: Oslomet; 2020. Available at: https://hdl.handle.net/20.500.12199/6417 (downloaded 08.11.2020).
19. Forskrift 17. juni 2005 nr. 610 om smittevern i helse- og omsorgstjenesten. Available at: https://lovdata.no/dokument/SF/forskrift/2005-06-17-610 (downloaded 24.08.2020).
20. Forskrift 28. oktober 2016 nr. 119 om ledelse og kvalitetsforbedring i helsetjenesten. Available at: https://lovdata.no/dokument/SF/forskrift/2016-10-28-1250 (downloaded 23.06.2021).
21. Lov 2. juli 1999 nr. 64 om helsepersonell mv. Available at: https://lovdata.no/dokument/NL/lov/1999-07-02-64?q=helsepersonelloven (downloaded 20.06.2021).
22. Kvale S, Brinkmann S, Anderssen TM, Rygge J. Det kvalitative forskningsintervju. 3rd ed. Oslo: Gyldendal Akademisk; 2015.
23. Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Quality & Safety in Health Care. 2005;14(1):26–33. DOI: 10.1136/qshc.2004.011155
24. Kermode M, Jolley D, Langkham B, Thomas MS, Holmes W, Gifford SM. Compliance with universal/standard precautions among health care workers in rural north India. American Journal of Infection Control. 2005;33(1):27–33. DOI: 10.1016/j.ajic.2004.07.014
25. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77–101. DOI: 10.1191/1478088706qp063oa
26. Oslomet – storbyuniversitetet. Personvern, ROS-analyse, dataplaner og databehandling. Oslo: Oslomet; 2020.
27. Stubberud D-G. Kvalitet og pasientsikkerhet: sykepleierens funksjon og ansvar for kvalitetsarbeid. Oslo: Gyldendal; 2018.
28. Lindén E, Lekman J. Riskförebyggande arbete i kommunal hemsjukvård: en intervjustudie om sjuksköterskors erfarenheter [masteroppgave]. Växjö: Linnéuniversitetet; 2018.










Comments