The experiences of registered nurses and specialist ICU nurses before and after implementation of ISBAR – a survey
The registered nurses found that the ISBAR communication tool improves the treatment and safety of patients in ICU and on general hospital wards by ensuring that transfer reports are made more standardised and time-efficient.
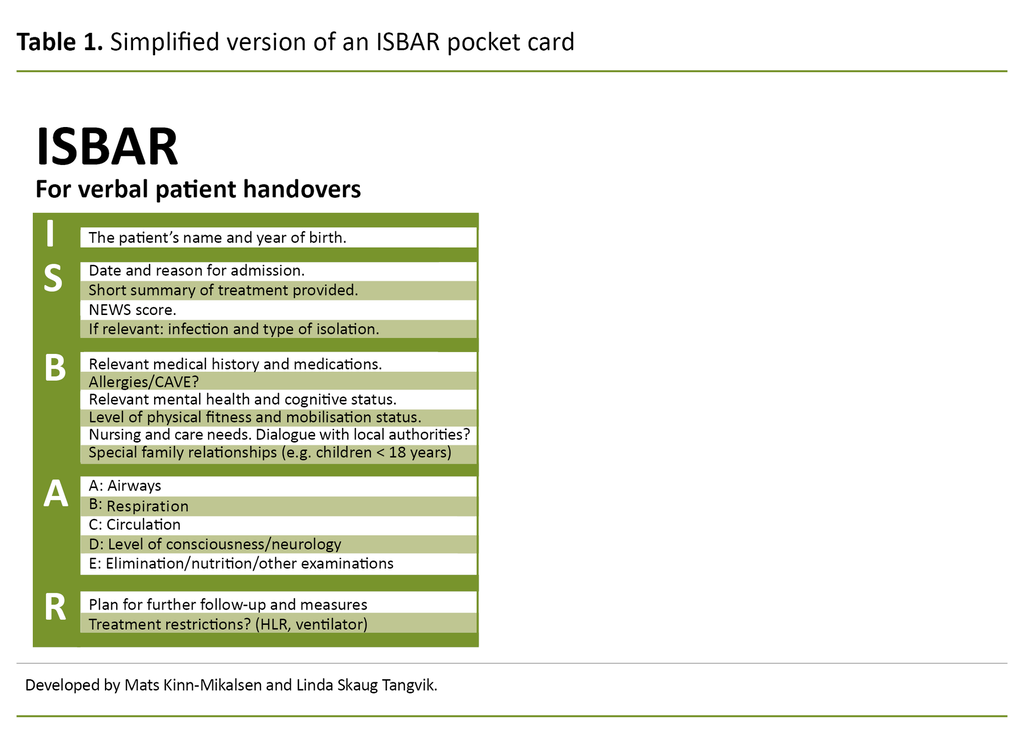
Background: Communication failure is one of the main causes of adverse events in the health service. In particular, the transfer of patient responsibility can represent a risk if important information is not passed on. The World Health Organisation and the Norwegian Health Directorate recommend using the communication tool ISBAR (identification, situation, background, assessment, recommendation) to ensure safe verbal communication during patient handovers.
Objective: To survey the experiences of registered nurses in ICU and on general hospital wards with verbal transfer reporting, before and after implementation of ISBAR.
Method: We conducted a survey in an intensive care unit and on three medical wards in an effort to chart the registered nurses’ experiences of transfer reports, before and after ISBAR was implemented. The data analysis was based on descriptive statistics and non-parametric testing. Answers to open-ended questions in the questionnaire were subjected to content analysis.
Results: A total of 89 registered nurses responded to the survey at the pretest stage (64 per cent) and 87 at the posttest stage (56 per cent). Compared to the pretest, the posttest showed greater standardisation of transfer reports (p = 0.001) and greater time-efficiency (p = 0.001) after the introduction of ISBAR. In the posttest, 83 registered nurses (95 per cent) agreed that ISBAR had improved patient treatment, and they felt more confident when taking over responsibility for patients (p = 0.003).
Conclusion: ISBAR is a time-efficient communication tool that can help to improve the treatment of patients, produce more structured transfer reports and standardise patient handover information. Introducing changes to clinical practice can be challenging, but training and the introduction of a range of different information material proved to be effective measures when introducing ISBAR to the hospital.
Communication failure between healthcare personnel is the cause of more than 60 per cent of adverse events in hospitals (1). Patient handovers are particularly prone to communication failure (1, 2), and the latest annual report issued by the Government’s Incident Reporting System referred to 317 adverse events that had occurred during patient transfers in Norwegian hospitals (3).
Internationally, patient transfers rank among the five most common causes of adverse patient events and unnecessary medical costs (4). Patient safety can be compromised if significant information is not passed on, and this can lead to treatment delays, incorrect diagnoses, and erroneous treatment (5).
A survey of re-admissions to ICU from general wards found that the odds of re-admission were five times higher among patients with an incomplete written transfer report (6). The past year has demonstrated the vulnerability of Norway’s ICU capacity, and measures that prevent unnecessary use of ICU beds should therefore be prioritised.
Research has found a lack of structure as well as varying and incomplete content in verbal intrahospital transfer reports, thus highlighting a need for standardisation (7, 8). Our study surveyed the experiences of registered nurses (RNs) and ICU nurses (both hereafter referred to as ‘nurses’) in an intensive care unit and on general wards with intrahospital transfer reports before and after introduction of the ISBAR communication tool.
It has previously been documented that expectations differ between these two groups of nurses with respect to the content of transfer reports. ICU nurses feel a strong sense of ownership in respect of intensive care patients and have a great need to pass on detailed information about them (9), while nurses on general wards seek less information about the patient’s time in ICU and more information about current status and treatment plans (9, 10). The lack of standard guidelines in respect of transfer report content can give rise to such discrepancies in expectations.
ISBAR
The ISBAR communication tool originated in the US navy in the 1980s and was first introduced in the US health service in 2001 as a measure to reduce communication failures among healthcare personnel (11).
Use of the tool has since spread internationally, and it is now recommended by the World Health Organisation (WHO) as a leading example of standardisation of communication during patient handovers (12). Since 2017, ISBAR has been a part of the Norwegian patient safety programme as per recommendations issued by the Directorate of Health (13) to give healthcare personnel a tool to ensure safe verbal communication (14).
Research into the use of ISBAR in clinical practice has shown a potential 20 per cent drop in the number of adverse events caused by communication failure (15), as well as more effectively structured report content (16) and significantly improved handover quality in transfers between specialist wards (17).
A study that investigated the use of ISBAR among master students in specialist nursing, found that students became more aware of their own communication structure and gained a better overview of the patient’s situation. The use of ISBAR also led to greater agreement among healthcare personnel about the treatment and plan of action for patients (18).
The objective of the study
Despite the fact that there is now more ISBAR research available, few studies survey the communication tool’s impact on intrahospital transfer reports in handovers between nurses on medical wards and in specialist departments. This study’s objective was therefore to gain more knowledge about this area. We asked the following research question:
‘What experiences do nurses in ICUs and on medical wards have of verbal transfer reports, before and after implementation of ISBAR, in terms of content, structure and time spent?’
Method
Study design
The study is an intervention study with a pre–post-design. A questionnaire was used to collect data.
Recruitment and data collection procedure
One intensive care unit and three medical wards at a local hospital were asked to take part in the study. The heads of department approved the enquiry. We only included medical wards with both inward and outward patient transfers. This meant that no emergency departments or outpatient wards were asked to take part in the study. In order to encourage responses from nurses who experience frequent patient transfers the inclusion criterion was a full-time equivalent of > 50 per cent to encourage.
Information about the study was communicated by email and posted in the hospital’s intranet. We handed out a questionnaire designed to survey experiences of patient transfers to the heads of the four departments that were taking part in the study. The heads of department distributed the questionnaire among their staff.
These were hardcopy forms that were returned in an envelope after completion. To enable parametric testing, we asked participants to specify an anonymised code. We conducted the pre-test in February–March 2018 and the post-test in September–November 2018.
Data collection tools
With the developers’ permission, we translated an Australian patient transfer questionnaire (19) into Norwegian in line with the six stages of the recognised translation procedure developed by Beaton et al. (20). The stages include forward translation, synthesis, back-translation, expert committee review, pretesting, and documentation of the translation process.
Each researcher undertook a forward translation, followed by a synthesis of the different versions. We hired two native English-speaking translators to carry out the back-translation, one of whom had a medical background. The content of the draft submitted to the expert committee was validated by eight recently qualified ICU nurses before a final version was produced.
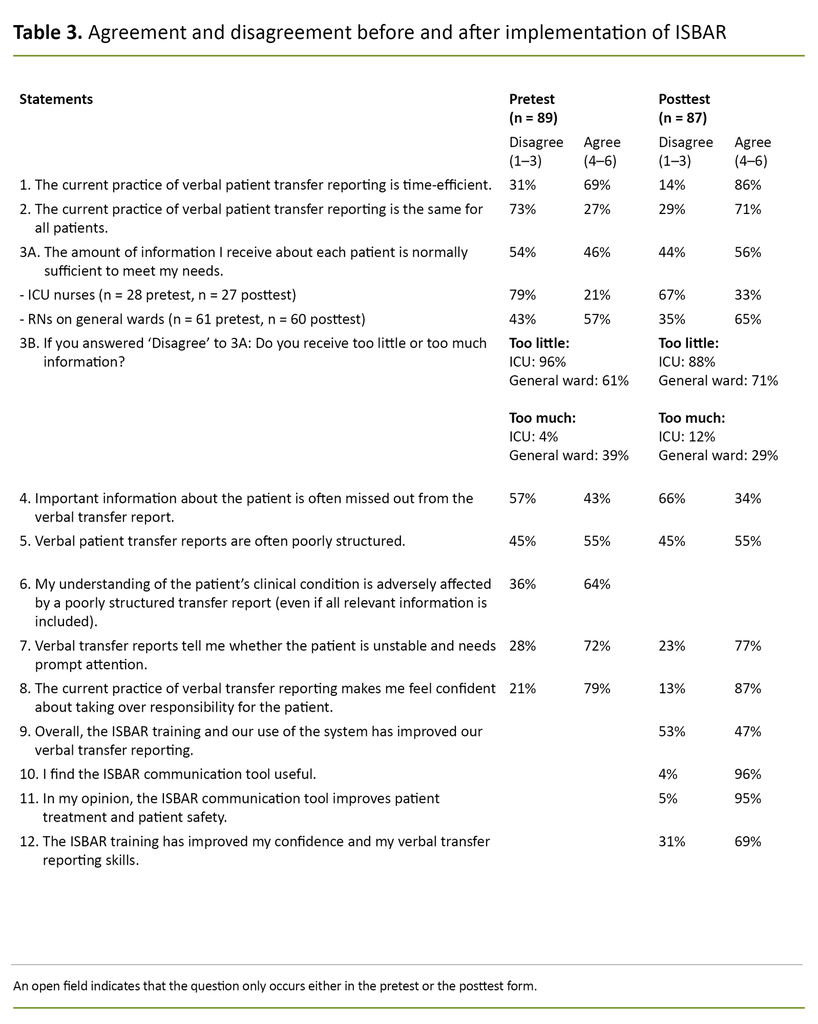
The questions included in the questionnaire asked about time spent on the verbal transfer reports as well as their content and structure before and after implementation of ISBAR. The pretest consisted of one open-ended and eight closed questions, while in the posttest there were two open-ended and twelve closed questions (Table 3).
A six-point Likert scale with responses ranging from ‘strongly disagree’ to ‘strongly agree’ was used for each of the featured statements. Open-ended questions were used to elicit experiences and views that were not captured by the closed questions.
We asked the following open-ended question in both the pretest and the posttest: ‘Based on your experience, are there any other negative or positive aspects of the verbal transfer report that you would like to point out?’
Additionally, the posttest also included the following question: ‘Have you found that the ISBAR communication tool has enhanced or reduced the quality of the verbal transfer report?
Intervention
Based on the recommendations issued by the Norwegian Directorate of Health, the hospital that took part in the study had already decided to introduce ISBAR, and we were put in charge of the implementation process. We identified several potential barriers to implementation: ongoing reorganisation of the hospital, the short period of time allocated to implementing ISBAR, and the potential reluctance of nurses to learn how to use new tools.
We conducted 22 training sessions, each of 30 minutes duration, in the period from April to June 2018, involving a total of 150 nurses. The training took the form of on-the-ward training in addition to drop-in sessions for nurses who were unable to attend the ward sessions.
However, attending the training sessions was not mandatory. The sessions covered research findings that identified communication failures in the health service, the history behind the introduction of ISBAR, and the outcomes of the pretest. The aim was to provide the background information required for the nurses to appreciate why the ISBAR communication tool was considered useful.
We recorded two videos for use in the training session, and these were subsequently posted on YouTube. The first clip shows a telephone conversation with a doctor where ISBAR is not used, while the second clip demonstrates the use of ISBAR in a telephone conversation with a doctor.
We produced pocket cards that included all the relevant points in a transfer report and handed them out on all the wards. In order to encourage the nurses to use the communication tool, we had mouse mats and posters made showing a simplified version of ISBAR, and these were placed in the staff rooms where transfer reports are exchanged.
We also handed out badges for pinning to nursing uniforms, saying ‘Give me an ISBAR’, and stickers saying ‘Calling a doctor? Remember ISBAR’. These were stuck to all telephone handsets.
Analysis
The statistics software we used for our statistical analyses was IBM SPSS, version 24. Because of the non-normal distribution of one dataset, the non-parametric Mann-Whitney U test was used to calculate the significance level and median to describe the mean value. In order to show the range of responses while excluding the most extreme, we present the 5th and 95th percentiles.
We asked the respondents to specify an anonymised code (mother’s name and year of birth), but this was missing in several of the questionnaires. We therefore analysed the dataset as if for two independent groups, before and after ISBAR had been implemented. To shed light on the proportional split between agreement and disagreement for the various statements, the Likert scale was dichotomised: ‘agree’ (1–3) and ‘disagree’ (4–6).
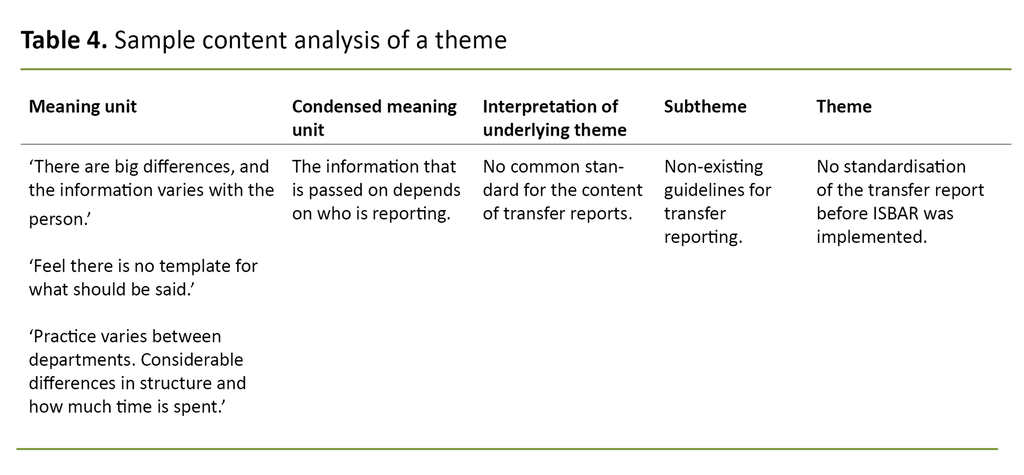
Responses to the open-ended questions made up seven pages of data material, and we analysed the text using Graneheim and Lundman’s (21) content analysis method (Table 4). This condenses the meaning units while preserving the core (manifest content). The condensed material is then subjected to interpretation (latent content) and abstracted into sub-themes and themes.
Ethics
The study has been approved by the Norwegian Centre for Research Data (NSD) (project number 57512). Return of a completed questionnaire was considered to constitute consent to participate in the study.
Results
The survey
Out of 140 nurses, 89 responded to the pretest (64 per cent), and 87 of 155 responded to the posttest (56 per cent). The pretest sample consisted of 28 ICU nurses and 61 nurses from general wards. The posttest sample consisted of 27 ICU nurses and 60 nurses from general wards.
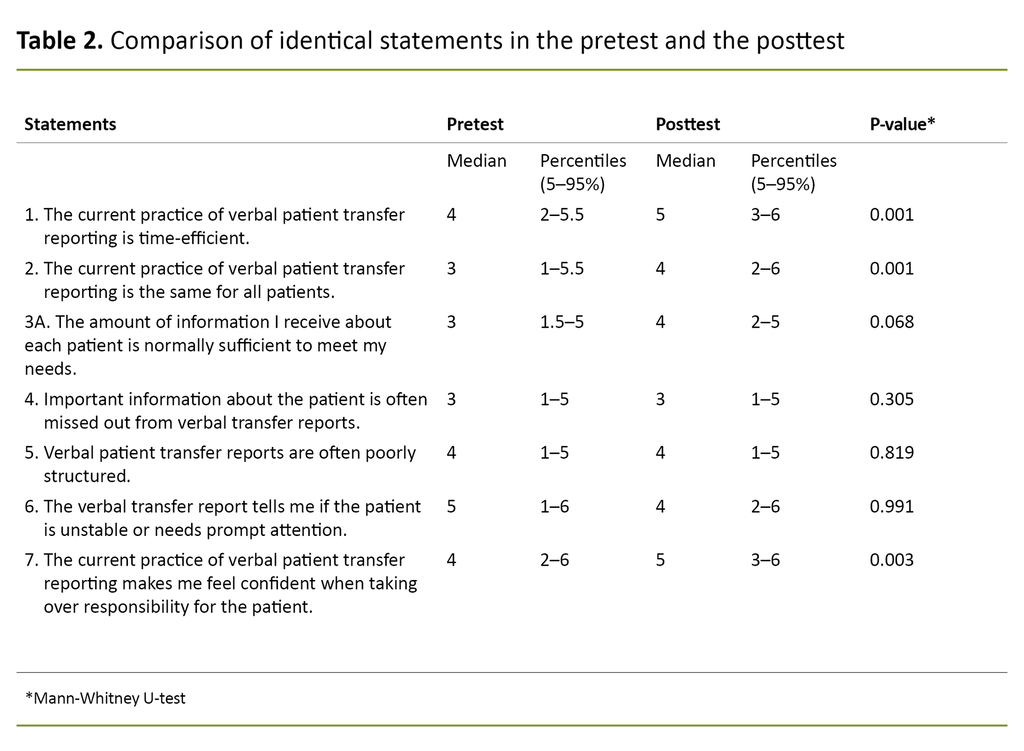
Quantitative analysis
The results show that the nurses found the transfer reports to be more time-efficient and more standardised for all patients after implementation of ISBAR. The nurses felt more confident about taking over responsibility for patients after ISBAR was implemented (Table 2).
In the pretest, 21 per cent of the ICU nurses agreed that they received sufficient information about patients during transfers, compared to 57 per cent of nurses on the general wards. In the posttest, this rose to 33 per cent in ICU and 65 per cent on the general wards.
Among the nurses who disagreed with the statement, the majority of the ICU nurses responded that they received insufficient information about patients. Out of the nurses on general wards, several felt they received too little information about the patient, while 39 per cent in the pretest and 29 per cent in the posttest responded that they received too much information.
95 per cent considered that ISBAR might enhance patient safety and treatment.
As many as 96 per cent of all the nurses responded that the communication tool was useful, 95 per cent considered that ISBAR might enhance patient safety and treatment, and 69 per cent stated that the ISBAR training had improved their confidence and their verbal reporting skills. However, only 47 per cent reported that the communication tool had improved verbal transfer reports (Table 3).
Evaluation of the implementation initiatives
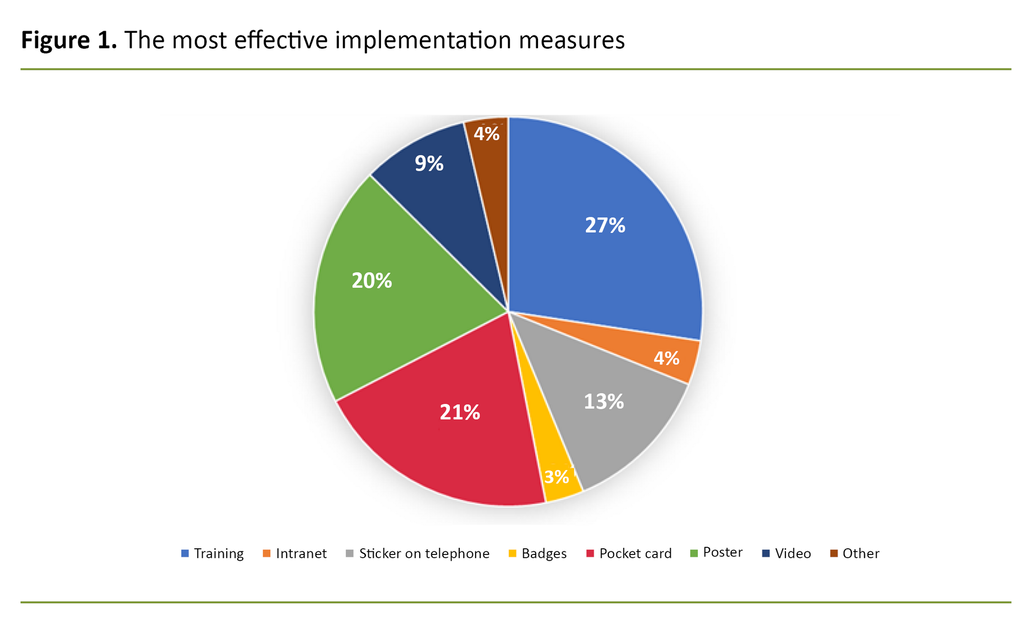
Training sessions, pocket cards and posters were listed as the most effective implementation initiatives (figure 1).
Content analysis
The first open-ended question was answered by 41 nurses (46 per cent) in the baseline study and 29 (33 per cent) in the posttest. In the posttest, 61 nurses (70 per cent) answered the question about whether ISBAR had improved or reduced the quality of transfer reports.
The content analysis of the open-ended questions resulted in three main themes, all of which are described below.
No standardisation of transfer reports before implementation of ISBAR
In the pretest, the nurses explained that that there was no standard practice for structuring transfer reports, and that the patient information that was handed over varied according to whoever did the reporting: ‘Practice varies between departments, and there are considerable differences in structure and how much time is spent’ and ‘There are big differences in the information provided, it varies with the person’.
Different expectations of transfer report content in ICUs and on general wards
Several nurses on general wards explained that they receive too much information when patients are handed over from ICU.
They felt that too much attention was given to what had happened when the patient was in intensive care, and they expressed a need for more information about the patient’s current status and the plan ahead: ‘The reports are often long and include a lot of information’ and ‘Much of the focus is on what has happened rather than the current status […] and what’s the plan ahead.’
On the other hand, the ICU nurses reported that they receive too little information from the general wards in patient transfers: ‘I sometimes feel that the nurses on the general wards don’t know the patient well enough when they give their report. They hand over the patient and leave before we have received the information we need.’
ISBAR raises awareness of what the handover report should include
ISBAR raised awareness of the type of patient information that should be included in the verbal report, as suggested by the following statements: ‘Greater focus on what is important to report’ and ‘More aware of what you report’.
ISBAR is seen as a useful guide.
Provided all parts of the form are fully addressed, the predictability of using ISBAR makes it unnecessary to interrupt the reporting to ask questions: ‘You get a more structured report from the general ward and there are fewer interruptions, because you know what information is coming.’
ISBAR is seen as a useful guide: ‘A memory aid when you have a lot on the go’ and ‘I find it easier to structure my report when I have a template to follow’. We interpret these comments to mean that ISBAR provides predictability, in terms of the report structure as well as content.
Discussion
Our content analysis of the open-ended questions suggests that transfer reports were poorly structured before ISBAR was adopted. These findings are supported by our quantitative analysis, which indicates that 55 per cent of participants considered the verbal reports to be poorly structured. In the posttest, several nurses reported that the communication tool gave them a template for their reporting, and that the tool worked as a useful memory aid.
We interpret this result to mean that the patient information passed on in the reports has become more standardised in that they follow a set structure. In this way, ISBAR can help to restrict variation in the presentation of patient information. When we compare our findings with those of the original study, which investigated the handover of patient information between junior medical officers, we see that they also found that the reporting became more standardised after the introduction of ISBAR (19).
Other significant findings included the perception that the transfer reports had become more time-efficient, and that the nurses felt more confident about taking over responsibility for patients. Time is a scarce resource in the health service, and ISBAR can help to free up time for other important nursing tasks.
However, several nurses stated that the communication tool had not improved verbal transfer reporting. This may have been due to insufficient practice in using the ISBAR tool due to the short period between introducing ISBAR and conducting the posttest.
Nevertheless, many nurses stated that the training had improved their confidence and verbal reporting skills, and this may impact on the quality of transfer reports. Nearly all of the nurses considered the communication tool to be useful, which is an important premise for the nurses to adopt it.
A greater need for information among ICU nurses
Our findings show that even after the implementation of ISBAR, only 33 per cent of the ICU nurses agreed that they receive sufficient information about the patient at handover. Of those who disagreed with this statement, the majority specified that they were receiving too little information.
On the general wards, 65 per cent of the nurses agreed with the statement, but out of those who disagreed, several stated that they were receiving too little rather than too much information. When we compared those who said that they were receiving too much information, nurses on general wards made up a larger percentage than ICU nurses.
The ICU nurses felt they were receiving too little information and the nurses on general wards felt they were receiving too much information.
This finding is consistent with the results of the content analysis, where the ICU nurses felt they were receiving too little information and the nurses on general wards felt they were receiving too much information about the patient’s medical history. This result suggests a greater need for information among ICU nurses than among nurses on general wards.
The reason may be that ICU nurses need all available information in order to be better equipped to identify problems and complications that may arise as a result of the patient’s medical history and critical condition. Also, the patient may be too ill to provide the necessary information personally.
The nurses on general wards wanted information about how to care for the patient now that he or she had been stabilised.
These findings are consistent with the study conducted by Enger et al. (10), and with a systematic review (22) that describes transfer reports from ICUs as being too rich in information about intensive care history without providing a clear plan for further treatment, to the effect that staff felt overwhelmed by the information provided by the ICU nurses.
The need for information among ICU nurses is different to that of nurses on general wards.
Bunkenborg’s (9) study maintains that ICU nurses feel a sense of ownership vis-a-vis ICU patients, and this may well be because ICU nurses constantly tend to their patients throughout the critical phase of their illness and shoulder the responsibility of taking full charge of the patient’s situation.
Based on these findings, it appears that the need for information among ICU nurses is different to that of nurses on general wards, and this gives rise to different expectations with respect to the content of transfer reports. The extent to which ISBAR, as a communication tool, can solve this disparity in expectations is a matter for discussion.
Barriers that may hamper implementation of new interventions
Intervention studies can encounter barriers that hamper the implementation of new interventions (23). Research shows that it can be challenging to change habits and behaviours, and that successful implementation requires significant effort and motivation from participants (24).
When new guidelines and documentation systems are introduced, additional tasks are often added to the nurses’ busy working day, and they can easily become weary of new types of paperwork. However, ISBAR is a verbal communication tool with no need for documentation.
The most challenging barrier at the time of implementation was organisational changes at the hospital. It would have been useful if ISBAR had been introduced at a time of less upheaval, with mandatory training sessions.
When an implementation process has come to an end, it is important to carry on with measures that will ensure continued practical implementation of the changes (24). Since this study, the hospital has introduced simulation training, with ISBAR communication being one of the focus areas. It would therefore be interesting to conduct a further study to establish whether a simulation intervention would have altered the results of our study.
Methodology
This study was a pretest–posttest implementation study with no control group. However, had the study design included a control group, this would have strengthened the study’s conclusions. The average response rate was > 50 per cent for both study periods and is therefore considered satisfactory (25).
However, it is possible that the questionnaire may have been completed by those with the most positive attitudes towards ISBAR. A higher response rate would therefore have increased the reliability of the result (26).
The questionnaire translation process was conducted according to recognised back-translation procedures. One of the back-translators has a medical background, which we believe strengthened the cultural adaptation.
The content of the questionnaire was validated by eight recently qualified ICU nurses with recent experience of different hospital wards and different ICUs. Their backgrounds were from similar wards to those in the study, which meant they were well placed to validate the content. The study was conducted in only one hospital, which may reduce its transfer value.
The questionnaire included several closed questions with set response options. When this format is used in several questions in a row, it can lead to respondents selecting the same response for each question (25).
To prevent this from happening, the questionnaire varied between positively and negatively charged questions. The questionnaire’s open-ended questions allowed the nurses to describe their experiences in their own words, which can be an important supplement to closed questions.
We have described differences between nurses on general wards and in ICUs only for questions 3A and 3B (Table 3). For the remaining questions, the sample has been analysed as a single group. In hindsight, it would have been useful to differentiate between the two groups for all questions in order to establish whether there are differences in areas other than information volume.
Paired tests were desirable for the analysis, but because there were several mismatches between the pretest and posttest codes, we conducted the analysis as if for two independent groups. It would have strengthened the result if we had been able to follow the same person from pretest to posttest.
Conclusion
This survey study shows that transfer reports became more standardised in terms of structure and content after ISBAR was implemented. The content analysis also showed that the nurses found the communication tool to be a useful template that helped to raise awareness of what type of patient information should be passed on.
Nevertheless, we found that in terms of volume of information, expectations differed between the ICU and general wards, and ISBAR had no impact in this respect. However, the nurses felt more confident about taking over responsibility for patients after the implementation of ISBAR, and 95 per cent stated that the communication tool had improved patient treatment and patient safety.
These factors may serve as a good motivator for nurses to use ISBAR when handing over patient information.
We wish to thank all the nurses who took part in the study and contributed to new knowledge, and we are grateful to our employer, who facilitated the study.
References
1. Müller M, Jürgens J, Redaèlli M, Klingberg K, Hautz WE, Stock S. Impact of the communication and patient hand-off tool SBAR on patient safety: a systematic review. BMJ Open. 2018;8(8):e022202. DOI: 10.1136/bmjopen-2018-022202
2. Arora V, Farnan J. Patient handoffs [Internet]. Waltham, Massachusetts: UpToDate; 2016 [updated 19.04.2021, cited 15.01.2021]. Available at: https://www.uptodate.com/contents/patient-handoffs.
3. Helsedirektoratet. Årsrapport 2017. Meldeordningen for uønskede hendelser i spesialisthelsetjenesten. Oslo: Helsedirektoratet; 2018. Report IS-2729. Available at: https://www.helsedirektoratet.no/rapporter/meldeordningene-arsrapporter/%C3%85rsrapport%202017%20Meldeordningene.pdf (downloaded 15.01.2021).
4. Reine E, Ræder J, Manser T, Småstuen MC, Rustoen T. Quality in postoperative patient handover: different perceptions of quality between transferring and receiving nurses. J Nurs Care Qual. 2019;34(1):E1–7. DOI: 10.1097/NCQ.0000000000000318
5. Foronda C, MacWilliams B, McArthur E. Interprofessional communication in healthcare: an integrative review. Nurse Educ Pract. 2016;19:36–40. DOI: 10.1016/j.nepr.2016.04.005
6. Naustdal KI, Drageset J. Pasientreinnleggelse på intensivavdelingen – en kasuskontrollstudie. Sykepleien Forskning. 2020;15(80647):(e-80647). DOI: 10.4220/Sykepleienf.2020.80647
7. Robertson ER, Morgan L, Bird S, Catchpole K, McCulloch P. Interventions employed to improve intrahospital handover: a systematic review. BMJ Qual Saf. 2014;23(7):600–7. DOI: 10.1136/bmjqs-2013-002309
8. Graan SM, Botti M, Wood B, Redley B. Nursing handover from ICU to cardiac ward: standardised tools to reduce safety risks. Aust Crit Care. 2016;29(3):165–71. DOI: 10.1016/j.aucc.2015.09.002
9. Bunkenborg G, Hansen TB, Hølge‐Hazelton B. Handing over patients from the ICU to the general ward: a focused ethnographical study of nurses' communication practice. J Adv Nurs. 2017;73(12):3090–3101. DOI: 10.1111/jan.13377
10. Enger R, Andershed B. Nurses’ experience of the transfer of ICU patients to general wards: a great responsibility and a huge challenge. J Clin Nurs. 2018;27(1–2):e186–94. DOI: 10.1111/jocn.13911
11. Finnigan MA, Marshall SD, Flanagan BT. ISBAR for clear communication: one hospital’s experience spreading the message. Aust Health Rev. 2010;34(4):400–4. DOI: 10.1071/AH09823
12. Verdens helseorganisasjon (WHO). Communication during patient hand-overs. Genève: WHO; 2007. Available at: https://www.who.int/patientsafety/solutions/patientsafety/PS-Solution3.pdf (downloaded 15.01.2021).
13. Helsedirektoratet. Tidlig oppdagelse og rask respons ved forverret somatisk tilstand – nasjonale faglige råd. Oslo: Helsedirektoratet; 2020. Available at: https://www.helsedirektoratet.no/faglige-rad/tidlig-oppdagelse-og-rask-respons-ved-forverret-somatisk-tilstand (downloaded 11.11.2021).
14. Helsedirektoratet. Pasientsikkerhetsprogrammet «I trygge hender 24-7»: ISBAR-sjekkliste. Oslo: Akershus universitetssykehus; u.å. Available at: https://pasientsikkerhetsprogrammet.no/om-oss/innsatsomrader/tidlig-oppdagelse-av-forverret-tilstand/_/attachment/inline/7c89f2ae-ae0b-4ba5-9d3e-b72796924c70:ab5504c818796e771beaadce0027771c2bc11682/isbar.pdf (downloaded 15.01.2021).
15. Randmaa M, Mårtensson G, Swenne CL, Engström M. SBAR improves communication and safety climate and decreases incident reports due to communication errors in an anaesthetic clinic: a prospective intervention study. BMJ Open. 2014;4(1). DOI: 10.1136/bmjopen-2013-004268
16. Blom L, Petersson P, Hagell P, Westergren A. The situation, background, assessment and recommendation (SBAR) model for communication between health care professionals: a clinical intervention pilot study. International Journal of Caring Sciences. 2015;8(3):530.
17. Leonardsen A-C, Moen EK, Karlsøen G, Hovland T. A quantitative study on personnel’s experiences with patient handovers between the operating room and the postoperative anesthesia care unit before and after the implementation of a structured communication tool. Nursing Reports. 2019;9(1):1–5. DOI: 10.4081/nursrep.2019.8041
18. Moi EB, Söderhamn U, Marthinsen GN, Flateland SM. Verktøyet ISBAR fører til bevisst og strukturert kommunikasjon for helsepersonell. Sykepleien Forskning. 2019;14(74699):(e-74699). DOI: 10.4220/Sykepleienf.2019.74699
19. Thompson JE, Collett LW, Langbart MJ, Purcell NJ, Boyd SM, Yuminaga Y, et al. Using the ISBAR handover tool in junior medical officer handover: a study in an Australian tertiary hospital. Postgrad Med J. 2011;87(1027):340–4. DOI: 10.1136/pgmj.2010.105569
20. Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25(24):3186–91. DOI: 10.1097/00007632-200012150-00014
21. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12. DOI: 10.1016/j.nedt.2003.10.001
22. Ong M-S, BiomedE M, Coiera E. A systematic review of failures in handoff communication during intrahospital transfers. The Joint Commission Journal on Quality and Patient Safety. 2011;37(6):274–84. DOI: 10.1016/s1553-7250(11)37035-3
23. Rustøen T, Lerdal A. Klinisk forskning innen helsefag. Hvordan utvikle god forskning – sentrale elementer. Bergen: Fagbokforlaget; 2021.
24. Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. Making psychological theory useful for implementing evidence based practice: a consensus approach. BMJ Quality & Safety. 2005;14(1):26–33. DOI: 10.1136/qshc.2004.011155
25. Jacobsen DI. Hvordan gjennomføre undersøkelser? Innføring i samfunnsvitenskapelig metode. 3rd ed. Oslo: Cappelen Damm Akademisk; 2015.
26. De Vet HC, Terwee CB, Mokkink LB, Knol DL. Measurement in medicine: a practical guide. Cambridge: Cambridge University Press; 2011.










Comments