How much guidance on parent-infant interaction is provided in NICUs in Norway?
Parents in NICUs report good follow-up from contact nurses and doctors, as well as a high level of self-efficacy after discharge. However, parental guidance should be strengthened in some areas.
Background: National guidelines recommend that parents of premature infants be offered evidence-based guidance on parent-infant interaction while the infant is in hospital. Research shows that a modified version of the Mother-Infant Transaction Programme (MITP-m) can foster good development outcomes and adaptability in families with premature infants.
Objective: This study examines the extent to which the assumed core components of the MITP have been implemented in Norwegian neonatal units, and whether this impacts on parenting self-efficacy immediately after discharge from hospital.
Method: A total of 150 parents from eight different NICUs in Norway responded to an electronic questionnaire two weeks after discharge from hospital. The questionnaire consisted of questions we formulated in relation to the MITP-m, as well as two validated questionnaires. We performed a descriptive analysis of the data in addition to regression analyses.
Results: The parents reported receiving extensive general guidance and training. Topics relating to interaction, such as guidance on the infant’s state regulation and social nature, were less well covered. Parents who confirmed having extensive knowledge of parent-child interaction after discharge received good follow-up from their primary nurse and their doctor. The parents were often present in the had considerable support from their own social network. Parents’ social networks have a significant impact on perceived parenting self-efficacy after discharge.
Conclusion: The parents report good follow-up in the NICUs and that they were well taken care of by dedicated contact nurses and doctors. The results of the study do not indicate whether this was related to various guidance programmes. Parental guidance with a focus on the infant’s state regulation and capacity and need for social interaction would benefit from being strengthened.
Families with premature infants are more likely to face difficulties in adjusting to everyday life than families with full-term infants. Problems can arise with the infant, the parents’ coping ability and/or the parent-infant relationship (1–4). Persistent increased stress in the parents and more self-regulation problems in the infant are typical examples of this (3, 5, 6).
Premature birth combined with difficulties in parent-infant adaptation can lead to long-term adverse effects on a child’s behavioural and socio-emotional development throughout childhood and adolescence (4, 6).
The Norwegian Directorate of Health’s guidelines for the follow-up of premature infants (2007) recommend that parents be offered guidance on interaction with their infant before being discharged from the neonatal intensive care unit (NICU) (7). It is unclear whether evidence-based guidance on parent-infant interaction has been implemented systematically as of 2020.
Norwegian NICUs aim to provide family-centred, individualised developmental care (8, 9). This care includes minimising the infant’s stress and pain as well as reinforcing parents’ presence, insight and participation in the care of their child.
Little is known about whether differences in the implementation of guidance on parent-infant interaction in Norwegian NICUs impact on the child’s and the parents’ long-term adaptation to each other.
Mother-Infant Transaction Programme (MITP)
Various guidance programmes have been tested in Norwegian NICUs (9–11). The Mother-Infant Transaction Program (MITP) has been tested in two Norwegian studies; initially in the Tromsø Intervention Study on Preterms (TISP) (10) and then in a study at Ullevål Hospital (12).
The TISP showed that the MITP improved outcomes in the development of premature infants and parents’ mastery of the parental role from the neonatal period up until the child is nine years old (4, 10). The MITP-m and the Newborn Individualised Developmental Care and Assessment Programme (NIDCAP), which is a similar programme, have inspired the design of family-centred individualised developmental care at Norwegian NICUs (9).
NIDCAP characterises care practices in some NICUs, but it is not known whether some NICUs have implemented the MITP systematically. Both approaches have resulted in major changes in care practices at NICUs since the turn of the millennium (9).
Nowadays, parents are present and involved in the care of their infant throughout the hospital stay. They are encouraged to have skin-to-skin contact with their newborn (kangaroo care), even when it needs to be monitored and receive intensive care (13). A growing number of NICUs are also providing rooms where the family can stay together for much of the hospital stay (14).
Core components of the programme
This study explores the extent to which the MITP has been implemented in Norwegian NICUs. The MITP is a structured and manualised intervention in which an interaction mentor follows up the infant and parents in twelve one-hour meetings; eight before discharge from the NICU and four during the first three months after discharge (4, 15).
The MITP is clearly described, but the core pedagogical components of the guidance have not been defined (15). However, we assume that these are:
- to help deepen parents’ understanding of the infant’s unique behaviour and way of expressing itself;
- to improve parents’ ability to take the necessary action to meet the infant’s changing needs;
- to enhance parents’ experience of the infant’s social nature and of enjoyment and attachment to the infant.
In line with pedagogical guidance theory, we assume that continuity in relationships between families and healthcare personnel is also an important component (16). During the planning of this study, key elements of the MITP were defined by a multidisciplinary research group with in-depth knowledge of the programme (see Appendix 1 [in Norwegian]).
Objective of the study
The health authorities recommend using patient-reported outcome measures in health service quality development (17). When patients are premature infants, the parents are the most important informants.
This study is aimed at all parents whose child was born before the 37th week of gestation, because even a low level of prematurity can increase the risk of adaptation problems within the family (18).
Norwegian NICUs have undergone significant changes in the last 20 years, but little is known about whether these changes have brought about a focus on stimulating parents’ interaction skills, as defined and described in the MITP.
The purpose of the study was to investigate the extent to which the MITP’s assumed core components have been implemented in Norwegian neonatal wards and whether this has a bearing on parenting self-efficacy immediately after discharge from hospital. To this end, the following research questions were formulated:
- To what extent do parents report having received guidance and support at the NICU that relates to one or more of the eleven core components of the MITP?
- How much confidence do parents have in their own competence immediately after discharge from hospital in relation to the guidance they received on parent-infant interaction at the NICU and to other factors during their hospital stay?
Method
This study was based on a questionnaire and had a descriptive and quantitative design. We invited a total of 13 NICUs to participate in the study, and eight of them agreed to do so. Three large and one medium-sized NICUs declined due to lack of capacity or interest.
The eight participating NICUs varied in size and patient flow, and all regional health authorities were represented. Information about the study was translated into eight languages and distributed in the NICUs. Mothers and fathers of premature infants were asked to participate in the study before discharge from the NICU. The parents provided their email addresses in the consent form and, where relevant, indicated their need for an interpreter to answer the questionnaire.
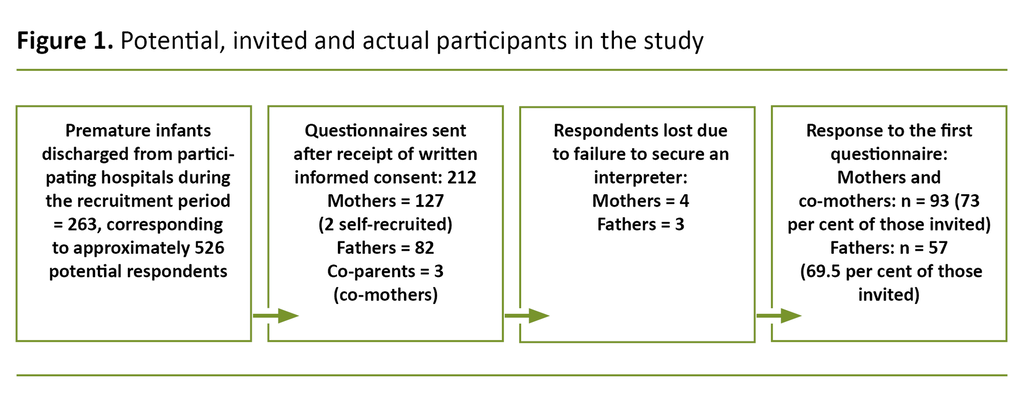
In the recruitment period February–June 2019, a total of 212 informants agreed to take part (Figure 1), and these included mothers, fathers and co-mothers. Families where the mother had been discharged directly from the maternity ward were not included.
In cases of multiple births, the parents were asked to relate their questionnaire responses to the infant with the lowest birth weight. The questionnaire was sent electronically to the parents’ email address two weeks after the planned discharge date.
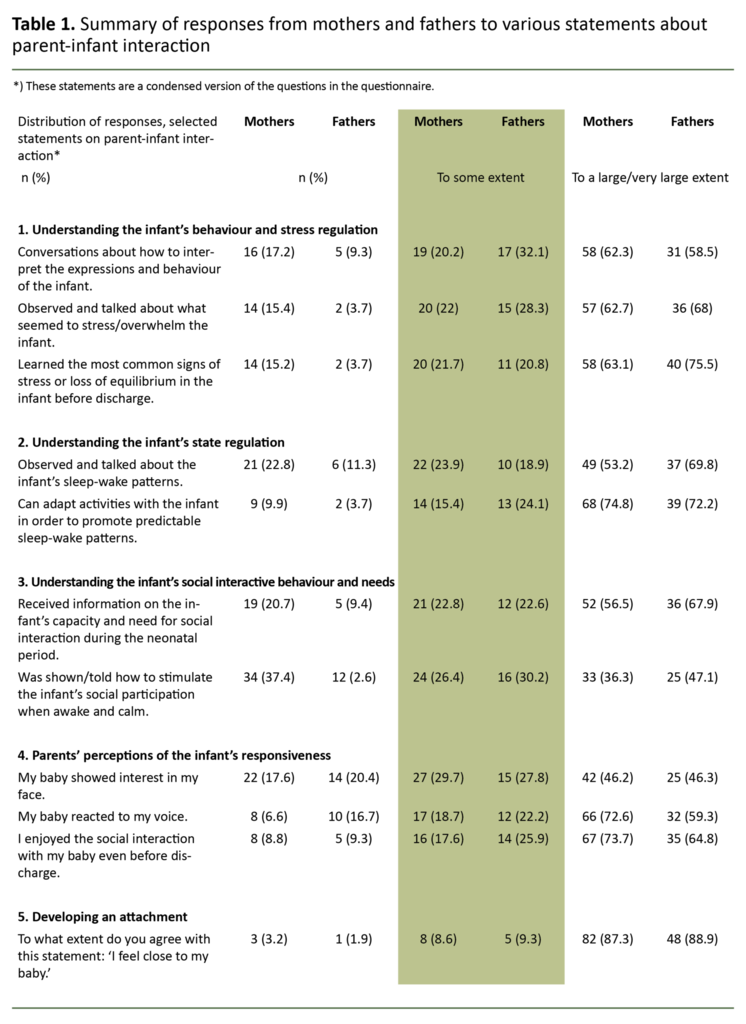
The questionnaire consisted of 101 questions, 51 of which were new questions that related to neonatal and demographic information, parents’ presence in the NICU, parental participation in discharge preparations and the guidance on parent-infant interaction they received (Table 1).
In addition, 35 of the 40 questions from the Neonatal Satisfaction Survey (NSS-8) (19) were included as well as all 15 questions from the Karitane Parenting Confidence Scale (KPCS) (20).
In order to collect data on the parents’ satisfaction with the hospital stay, we used a five-point Likert scale from ‘Not at all satisfied’ to ‘Extremely satisfied’ in the NSS-8. The NSS-8 has been developed and validated for use in Norway (19). The KPCS is a validated questionnaire aimed at mapping parents’ self-confidence and parenting self-efficacy in the neonatal period (20, 21).
The KPCS questions shed light on three underlying dimensions (parenting, social support and the infant’s development). The KPCS uses a four-point Likert scale from ‘Hardly ever’ to ‘Almost always’, and the total score can vary between 0 and 45 points.
The KPCS has been validated in Australia (20) and was translated into Norwegian for this study by the first author and an English government authorised translator. The final questionnaire (101 questions) was pilot-tested on five parents of premature infants who were recruited via social media.
Ethical considerations
The study was approved by the Northern Regional Committee for Medical and Health Research Ethics (REK), project number 2018/1948, the data protection officer at the University Hospital of Northern Norway (UNN) (ref. 2019/341) and the data protection officers at the relevant hospitals.
We drew up an agreement on data storage and use of the data processing tool REDCap with UNN’s Clinical Research Department (CRD) in January 2019. Healthcare personnel in the various NICUs invited the parents to participate in the study and informed them of their right to decline.
Data collection and analysis
The project manager transferred the email addresses provided by the parents to the REDCap system, and the questionnaire was dispatched two weeks after the estimated discharge date. We analysed the data in SPSS (IBM statistics 26).
In addition to descriptive analyses, we used a generalised linear mixed model (GLMM) to test the effect of independent variables (predictors) on the dependent, ordinary variables (MITP-related questions).
The GLMM corrected for dependence in data related to the mother and father reporting on the same child in some cases. Correlations between the parents’ self-efficacy (total KPCS score) and various predictors were identified using a multi-level linear mixed model (MLMM).
The study has relatively few participants (data volume) and many possible predictors. In order to reduce the complexity of analytical models, each predictor was tested for each dependent variable and only included in the final GLMM analysis or MLMM analysis if the effect on the dependent variables corresponded to a p-value < 0.25, as described by Hosmer and Lemeshow (22).
Information about testing can be obtained from the first author. We tried to include random effects (intercepts) in the analyses, but this had to be excluded in six out of eleven cases due to estimation difficulties.
We omitted some predictors due to a high correlation with other predictors. For example, ‘Length of hospital stay’ was omitted due to correlation with ‘Number of days of CPAP treatment’ (Pearson correlation = 0.77). We chose a significance level of 0.05.
Results
Recruitment and participants
We received between 8 and 63 consent forms from each of the NICUs. Using data from the register of sick and premature infants in Norway (case number S-DFC437E7), we were able to compare participation from each hospital, controlled for the number of potential participants.
The NICUs recruited between 0.4 and 1.4 informants per premature infant who was discharged during the recruitment period. This corresponds to 30 per cent of all potential informants, assuming that all infants had two parents. Three parents signed up on their own initiative after reading about the study on social media (Figure 1).
A total of 150 parents answered the questionnaire and answers from mothers and co-mothers are combined in the analyses. Ninety-six (74 per cent) of the 130 mothers who agreed to take part responded, and 54 of the 82 (66 per cent) fathers.
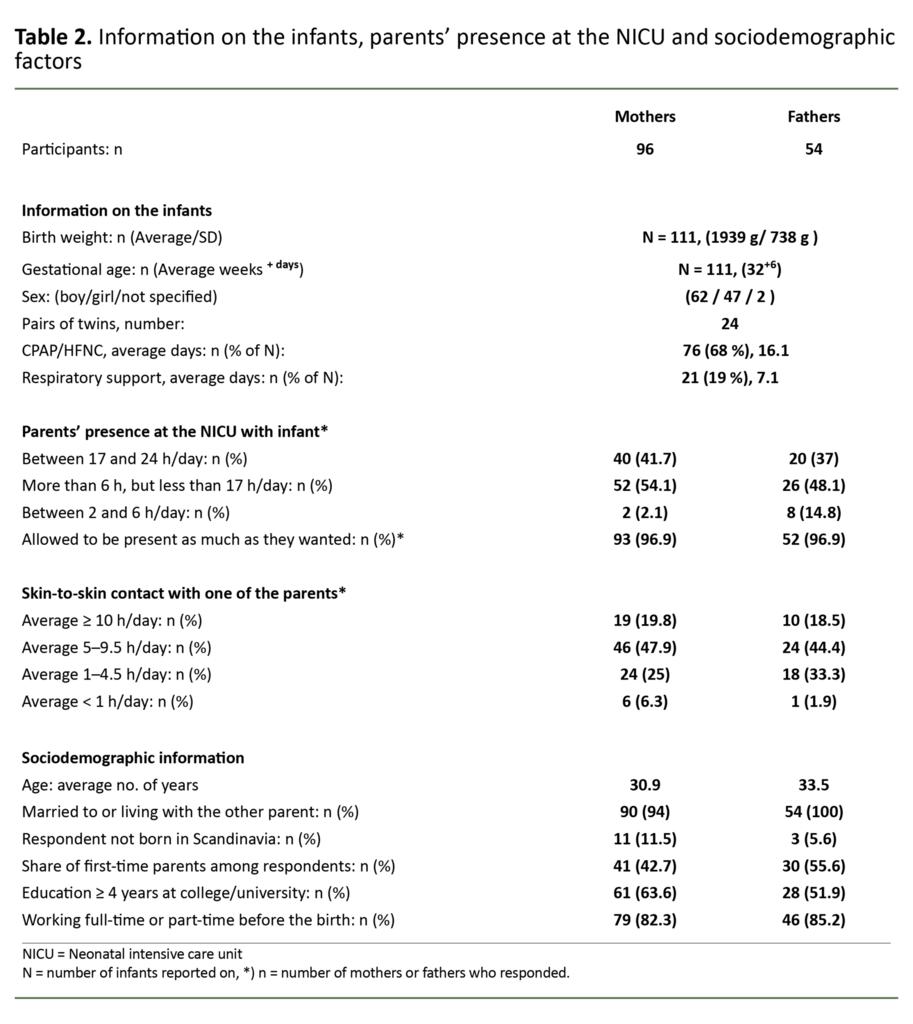
Neonatal and medical information, extent of parental presence at the NICU, extent of kangaroo care and socio-demographic data on the informants are shown in Table 2.
The infants had an average birth weight of 1939 grams (g): 7 were < 1000 g, 27 weighed 1000–1499 g, 24 weighed 1500–2000 g and 53 were > 2000 g. The infant’s gestational age (GA) varied from 24.7 to 36.9 weeks.
Approximately three out of four infants had received respiratory support (CPAP/HFNC), while one in five had received respiratory support whilst in the NICU. The parents’ presence at the NICU and the extent of kangaroo care are shown in Table 2.
Parents’ knowledge of the different components of the MITP
In answer to the NSS-8 question ‘How much guidance/information did you feel you received with regard to meeting your infant’s needs?’, 79 mothers (85 per cent) and 48 fathers (89 per cent) reported that they had received extensive or very extensive guidance.
The response to this general question provides a backdrop to the answers to eleven MITP-related statements summarised in Table 1, which are presented under five main themes below.
This significance was tested with respect to the distribution of responses to MITP-related statements and total KPCS scores, but the variable ‘discharging hospital’ had only a non-significant effect on five of eleven MITP-related statements. Beyond this, we only report significant correlations.
Understanding the infant’s behaviour and stress regulation
Parents who had extensively participated in conversations about understanding the infant’s behaviour cues reported more follow-up from contact nurses (F (3; 391) = 7.03; p < 0.001). This also applied to parents who had observed and talked about what might cause the infant stress (F (3; 109) = 3.55; p = 0.017).
However, extensive support from the parents’ own social network was negatively associated with having learned the infant’s most common signs of stress or loss of equilibrium before discharge (F (3; 96) = 2.86; p = 0.041).
Understanding the infant’s state regulation
Parents who had extensively observed and talked about the infant’s sleep-wake patterns had received more follow-up from contact nurses (F (3; 380) = 8.14; p < 0.001) and more support from their own social network (F (3; 380) = 4.47; p = 0.004). Their infants also had a lower GA (F (1; 380) = 9.62; p = 0.002).
A positive correlation was seen between the parents’ self-reported capacity to facilitate a good sleep rhythm in the infant and the variables ‘extensive follow-up from contact nurses’ (F (3; 378) = 3.04; p = 0.029) and ‘extensive parental presence at the NICU’ (F (3; 378) = 3.12; p = 0.026).
Understanding the infant’s social nature and needs
Parents who had received extensive information on the infant’s capacity and need for social interaction reported more follow-up from contact nurses (F (3; 367) = 2.66; p = 0.048) and more support from their own network (F (3; 367) = 2.78; p = 0.041).
There was also a positive correlation between being shown how to stimulate the infant’s social participation and extensive follow-up from contact nurses (F (3; 385) = 6.08; p <0.001).
Parents’ perceptions of the infant’s responsiveness
Parents who reported that the infant showed interest in their face to a large/very large extent, reported closer follow-up from their doctor (F (4; 99) = 2.47; = 0.050) and that the mother had given birth to only one child (F (1; 99) = 4.11; p = 0.045).
A positive correlation was also seen between the parents’ perceptions of the infant reacting to their voice and a large degree of follow-up from the doctor (F (4; 377) = 3.85; p = 0.004. The mothers’ and fathers’ answers differed here (F (1; 377) = 5.70; p = 0.017).
A total of 73 per cent of the mothers said that they felt very strongly that their infant had reacted to their voice, while the corresponding figure for the fathers was 59 per cent.
The third statement was about whether the parents enjoyed the interaction with the infant before discharge. More positive responses to this were associated with a strong presence at the NICU (F (3; 111) = 3.30; p = 0.023 and closer follow-up from the doctor (F (4; 111) = 2.72; p = 0.033).
Parents’ attachment to the infant immediately after discharge
Parents who confirmed that they felt very close to their child reported a higher level of support from their own social network (F (3; 105) = 3.22; p = 0.026).
A majority of the parents (84 per cent) said that the care and treatment of the infant at the NICU followed a carefully devised plan to a large or very large extent.
Parenting self-efficacy after discharge from the NICU
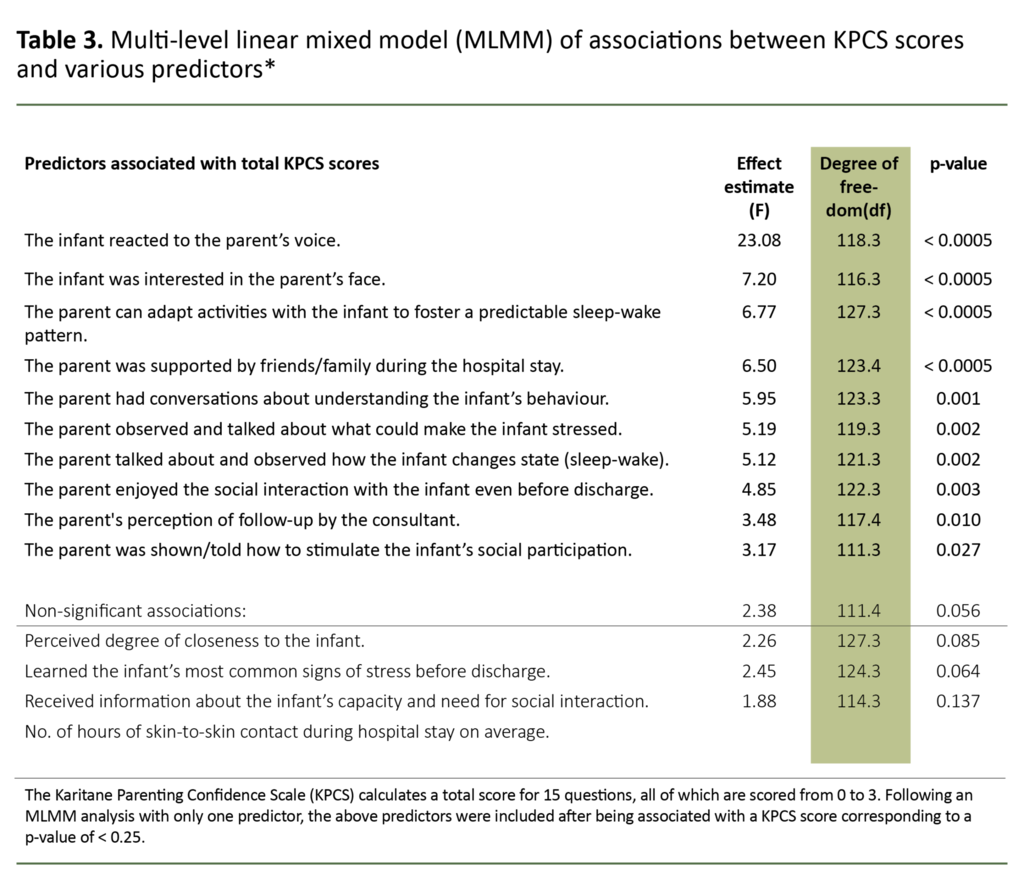
The average KPCS score for all respondents was 40.5 (SD = 3.7, 25th percentile = 39 points). We found a small, significant difference between mothers (41 points) and fathers (39.7 points) (t (df = 142) = 2.06, p = 0.041). Nine of the eleven MITP statements were significantly associated with the total KPCS score (Table 3).
Higher KPCS scores were positively related to the following:
- The infant reacted to the parents’ voices.
- The parents received extensive support from their own network.
- The parents had received information on what could cause the infant stress.
- The parents recognised the infant’s most common stress signals.
- The parents found that they were able to facilitate predictable changes in state (sleep-wake patterns).
- The parents had received information on the infant’s capacity and need for social interaction.
In contrast, a higher total KPCS score was negatively associated with:
- the parents having had conversations with healthcare personnel about how to interpret the infant’s behaviour;
- the parents’ perception that the infant showed a lot of interest in their face, and
- the parents’ perception that they received extensive follow-up from the doctor.
Discussion
Almost nine out of ten parents stated that they received extensive guidance on how to meet their infant’s needs, and a similar majority found that the follow-up at the NICU followed a carefully devised plan.
However, up to a quarter of the mothers reported receiving no or little guidance on the infant’s state regulation and capacity for social interaction. The inconsistent response suggests that some of the core components of the MITP are still not being properly implemented in Norwegian NICUs, despite extensive guidance being given.
No significant differences were found across the relevant hospitals, which may be linked to the relatively low number of respondents from each hospital.
Other variables, such as extent of kangaroo care during the hospital stay, a calm atmosphere in the patient’s room, level of prematurity or sociodemographic factors, also had no significant effect on the distribution of responses to the MITP statements or the KPCS scores.
The major improvements in the care of premature infants in recent decades in terms of greater parental presence, kangaroo care and the provision of family rooms, have well-documented benefits for both the infant and parents (23). However, these changes appear to be no guarantee that evidence-based guidance on interaction is provided.
Staff-parent relations are important
Parental participation in conversations about behaviour and stress regulation, state regulation and insight into the infant’s social nature was positively associated with three factors: follow-up from contact nurses, support from the parents’ own social network and extensive parental presence at the NICU.
There was also a positive correlation between extensive follow-up from the infant’s doctor and the parents’ enjoyment of the interaction with the infant as well as recognition of the infant’s interest in the parents’ faces and voices.
These findings confirm that relationships are an important aspect of guidance. Parents who receive good support from their professional and personal helpers are more likely to become more competent and adapt to the role of parent of a premature infant (16, 24).
The parents in this study reported, on average, a high level of self-confidence in terms of their own competence and coping ability two weeks after discharge from the NICU.
Higher KPCS scores are strongly associated with support from the parents’ own social network, which is consistent with the findings in a recently published Norwegian study (25) and reflects a salutogenic understanding of health promotion (26).
Support from personal networks is vital
Social support has been identified as a major factor in fostering the individual’s sense of coherence in life, which is composed of perceptions of predictability, manageability and meaning.
When an infant is admitted to an NICU, support from the parents’ personal networks can be crucial to their self-efficacy and confidence in their own competence.
The developers of the KPCS have defined a total score of 39 as a threshold for possible concern with respect to the parents’ belief in their own competence.
KPCS scores of 31–39 indicated moderate or low levels of concern among parents, while scores below 31 indicated a high level of concern (20, 21). According to this, only one in four parents in our study were within the range of concern two weeks after discharge.
Receiving good follow-up by contact nurses was strongly associated with parents’ perceptions that they received guidance in many of the MITP components.
This is in line with recent parental guidance theory, which describes alliance-building between parents and healthcare personnel as an important prerequisite for parents being able to apply the guidance they receive (16, 24).
In order for perceptions, observations and actions to consciously foster a sense of coping, parents need reflection partners and contexts that enable them to process the experiences (27).
Parents must be told the risk
Parenting self-efficacy (KPCS) reported two weeks after discharge from hospital was negatively associated with reported close follow-up by the infant’s doctor at the NICU.
This may be related to the healthcare personnel’s responsibility to inform parents about treatment risks, possible sequelae from premature birth and precautions the family should take. Receiving such health information is important, but it can also challenge parents’ confidence in their own parenting skills and coping ability.
However, a positive correlation was shown for parents who received close follow-up from the doctor and perceived that the infant was interested in their faces and voices and the social interaction with them.
This illustrates how important it is for doctors to strive for a balance in conversations with parents of premature infants. Information about possible future challenges should and can be combined with making the parents’ more aware of how important they are to their infant, and will strengthen their self-efficacy.
A previous study found that a strong sense of self-efficacy among parents was associated with positive development in premature infants, but that this correlation was mediated by the parents’ knowledge in families with premature infants (28). In other words, using knowledge to boost self-confidence is an art.
The study has several limitations, but nevertheless highlights experiences from many different NICUs. Low participation rates from some hospitals and losses to follow-up may have led to either an overly positive or an overly negative picture being painted of parents’ satisfaction.
However, the study provides useful information about key aspects that should be taken into account when implementing more systematic guidance on parent-infant interaction, as is also strongly recommended in the research literature (29).
Conclusion
The majority of the mothers and fathers were very satisfied with the follow-up they received at the NICU, and they reported a high level of parenting self-efficacy immediately after discharge from hospital.
Parents who received a lot of guidance on parent-infant interaction received good follow-up from contact nurses, doctors and their own social network. The variations in responses seem to be largely related to the parents’ relationships with individuals and less about the NICUs’ guidance practices for parent-infant interaction.
Future implementation of guidance on parent-infant interaction should focus on making the guidance less person-dependent and place more emphasis on the parents’ understanding of the infant’s state regulation and social capacity and needs.
The authors would like to thank the parents who responded to the questionnaire and the nurses who provided them with information and obtained their consent to participate before discharge from the NICU. A big thank you also goes to Ingrid Helen Ravn, who helped to design the study, and to the Board of Prematurforeningen, which provided valuable user participation.
References
1. Feldman R. The development of regulatory functions from birth to 5 years: insights from premature infants. Child Dev. 2009;80(2):544–61. DOI: 10.1111/j.1467-8624.2009.01278.x
2. Forcada-Guex M, Pierrehumbert B, Borghini A, Moessinger A, Muller-Nix C. Early dyadic patterns of mother-infant interactions and outcomes of prematurity at 18 months. Pediatrics. 2006;118(1):e107–14. DOI: 10.1542/peds.2005-1145
3. Landsem IP, Handegard BH, Tunby J, Ulvund SE, Rønning JA. Early intervention program reduces stress in parents of preterms during childhood, a randomized controlled trial. Trials. 2014;15:387. DOI: 10.1186/1745-6215-15-387
4. Landsem IP, Handegard BH, Ulvund SE, Tunby J, Kaaresen PI, Rønning JA. Does an early intervention influence behavioral development until age 9 in children born prematurely? Child Dev. 2015;86(4):1063–79. DOI: 10.1111/cdev.12368
5. Neel MLM, Stark AR, Maitre NL. Parenting style impacts cognitive and behavioural outcomes of former preterm infants: a systematic review. Child Care Health Dev. 2018;44(4):507–15. -DOI: 10.1111/cch.12561
6. Ritchie K, Bora S, Woodward LJ. Social development of children born very preterm: a systematic review. Dev Med Child Neurol. 2015;57(10):899–918. DOI: 10.1111/dmcn.12783
7. Sosial- og helsedirektoratet. Faglige retningslinjer for oppfølging av for tidlig fødte barn. Oslo: Sosial- og helsedirektoratet; 2007. Available at: https://helsedirektoratet.no/retningslinjer/for-tidlig-fodte-barn/ (downloaded 13.02.2018).
8. Helsedirektoratet. Nyfødtintensivavdelinger – kompetanse og kvalitet. Oslo: Helsedirektoratet; 2019. Available at: https://www.helsedirektoratet.no/retningslinjer/nyfodtintensivavdelinger-kompetanse-og-kvalitet. (downloaded 16.10.2020).
9. Ludvigsen ES, Tomren U, Lundby HK. Familiesentrert utviklingstilpasset omsorgsmodell – NIDCAP, rev. 20152011. Available at: https://www.helsebiblioteket.no/fagprosedyrer/ferdige/familiesentrert-utviklingstilpasset-omsorgsmodell-nidcap#updates (downloaded 16.10.2020).
10. Landsem IP. Kunsten å forstå de aller minste. In: Severinsen JE, ed. Forskning og innovasjon til pasientens beste. Nasjonal rapport fra spesialisthelsetjenesten, 2019. Foretakene Helse Midt-Norge, Helse Nord, Helse Sør-Øst, Helse Vest; 2020. Available at: https://helse-nord.no/forskning-og-innovasjon/kunsten-a-forsta-de-aller-minste (downloaded 28.04.2021).
11. Rønning JA, Ulvund SE, Kaaresen PI, Dahl LB. Prosjekt tidlig intervensjon 2000 [protocol]. 1998. Available at: http://uit.no/prematur (downloaded 16.10.2020).
12. Ravn IH, Smith L, Smeby NA, Kynoe NM, Sandvik L, Bunch EH, et al. Effects of early mother-infant intervention on outcomes in mothers and moderately and late preterm infants at age 1 year: a randomized controlled trial. Infant Behav Dev. 2012;35(1):36–47. DOI: 10.1016/j.infbeh.2011.09.006
13. Raiskila S, Axelin A, Toome L, Caballero S, Tandberg BS, Montirosso R, et al. Parents' presence and parent-infant closeness in 11 neonatal intensive care units in six European countries vary between and within the countries. Acta Paediatr. 2017;106(6):878–88. DOI: 10.1111/apa.13798
14. Tandberg BS, Flacking R, Markestad T, Grundt H, Moen A. Parent psychological wellbeing in a single-family room versus an open bay neonatal intensive care unit. PLoS One. 2019;14(11):e0224488-e. DOI: 10.1371/journal.pone.0224488
15. Rauh VA, Nurcombe B, Achenbach T, Howell C. The Mother-Infant Transaction program. The content and implications of an intervention for the mother of low-birthweight infants. Clin Perinatol. 1990;17(1):31–45. DOI: 10.1016/s0095-5108(18)30586-4
16. Nugent KJ, Keefer CH, Minear S, Johnson LC, Blanchard Y. Nyfødtes atferd og tidlige relasjoner. Manual for NBO (Newborn Behavioral Observations). Oslo: Gyldendal; 2018.
17. Enden T, Bernklev T, Jelsness-Jørgensen L-P, Amdal CD. Pasientene kjenner best egen helse. Kronikk. Tidsskr Nor Legeforen. 2018. DOI: 10.4045/tidsskr.17.1054
18. Hadfield K, O'Brien F, Gerow A. Is level of prematurity a risk/plasticity factor at three years of age? Infant Behav Dev. 2017;47:27–39. DOI: 10.1016/j.infbeh.2017.03.003
19. Hagen IH, Svindseth MF, Nesset E, Orner R, Iversen VC. Validation of the Neonatal Satisfaction Survey (NSS-8) in six Norwegian neonatal intensive care units: a quantitative crosssectional study. BMC Health Serv Res. 2018;18. DOI: 10.1186/s12913-018-3031-z
20. Črnčec R, Barnett B, Matthey S. Development of an instrument to assess perceived self-efficacy in the parents of infants. Res Nurs Health. 2008;31(5):442–53. DOI: 10.1002/nur.20271
21. Črnčec R, Barnett B, Matthey S. Karitane Parenting Confidence Scale: manual 2008. Available at: https://plct.files.wordpress.com/2019/01/karitane-parenting-confidence-scale-manual-copy.pdf (downloaded 10.10.2018).
22. Hosmer jr. DW, Lemeshow S. Applied logistic regression. Hoboken, New Jersey and Canada: John Wiley & Sons; 2000.
23. Griffiths N, Spence K, Loughran-Fowlds A, Westrup B. Individualised developmental care for babies and parents in the NICU: evidence-based best practice guideline recommendations. Early Hum Dev. 2019 Dec;139:104840. DOI: 10.1016/j.earlhumdev.2019.104840
24. Nugent JK, Bartlett JD, von Ende A, Valim C. The effects of the Newborn Behavioral Observations (NBO) System on sensitivity in mother-infant interactions. Infants Young Child. 2017;30(4):257–68. DOI: 10.1097/iyc.0000000000000103
25. Hagen IH, Iversen VC, Nesset E, Orner R, Svindseth MF. Parental satisfaction with neonatal intensive care units: a quantitative cross-sectional study. BMC Health Serv Res. 2019;1. DOI: 10.1186/s12913-018-3854-7
26. Langeland E. Betydningen av den salutogene modell for sykepleie. Klin Sygepleje. 2012;26(2):38–47. DOI: 10.4220/sykepleienf.2009.0143
27. Drageset I. Fag og utdanning – hvor går veien til kompetente sykepleiere? Tromsø: Eureka forlag; 2005.
28. Hess CR, Teti DM, Hussey-Gardner B. Self-efficacy and parenting of high-risk infants: the moderating role of parent knowledge og infant development. Appl Dev Psychol. 2004;25:423–37. DOI: 10.1016/j.appdev.2004.06.002
29. Puthussery S, Chutiyami M, Tseng P-C, Kilby L, Kapadia J. Effectiveness of early intervention programs for parents of preterm infants: a meta-review of systematic reviews. BMC Pediatrics. 2018;18. DOI: 10.1186/s12887-018-1205-9










Comments