Early identification of children who stutter – a survey of assessments made by public health nurses
In order to identify children who need a referral to a speech therapist, public health nurses must pay attention to repetitions, blocks and prolongations in the child’s speech.
Background: Stuttering can have an adverse effect on the child’s emotional, behavioural and attitudinal development. Early identification and speech therapy is therefore recommended. Public health nurses at child health centres see children at their regular check-ups at two and four years of age. According to national professional guidelines, public health nurses are responsible for monitoring the children’s language so that any speech difficulty or other language-related disorder, such as stuttering, can be identified as early as possible. We have little knowledge of the observations and assessments that form a basis for the public health nurses’ practice when they identify stuttering.
Objective: To enhance our knowledge of public health nurses’ practices when they first encounter parents with children who stutter. We sought to evaluate practices against recommendations that are based on recent international research.
Method: This was a descriptive cross-sectional study with an online questionnaire designed specifically for completion by public health nurses at child health centres in seven Norwegian counties. The data were analysed using descriptive statistics, ordinal regression analysis and chi-square testing.
Results: Ninety-five public health nurses completed the questionnaire. Providing information about stuttering and making another appointment with the parents were the practices identified as the most frequently adopted by the public health nurses in their first encounter with the parents of children who stutter. The most commonly provided advice was associated with interaction and communication, and to contact a specialist. When assessing whether to continue to monitor the situation or to give a referral, the public health nurses considered the child’s age, the child’s perception of or reaction to the stuttering, and parental concern. Very few of them had access to written guidelines with respect to appropriate practice and when to contact a speech therapist.
Conclusion: The public health nurses’ practice and advice during their first encounter with parents whose child stutters, were generally in line with recommendations that are based on recent international research. The public health nurses’ assessments of which children need further follow-up are inconsistent with the recommendations in that they do not assess the actual stutter. The results indicate that the public health nurses need more knowledge about stuttering. They need clearer guidance on when and how to identify stuttering during child health centre check-ups in order to ensure that the right children are identified and benefit from early intervention.
Stuttering is a neurodevelopmental disorder (1) that affects approximately one in ten preschool-age children (2). The disorder may have an adverse effect on the child’s behaviour and emotions as well as their own attitude to their speech (3, 4). In the longer term, stuttering can impact on the child’s mental health and lead to social anxiety (5) and a reduced quality of life (6).
Children who receive treatment are almost eight times more likely to stop stuttering than those who do not receive treatment (7). Early identification of stuttering, and referrals for treatment, are therefore critical to prevent further development of the stuttering, and to prevent potential adverse effects (8).
Stuttering and natural disfluency
A stutter is an audible pause in a person’s speech flow and involves 1) repeating sounds, whole words and/or syllables, 2) prolonging sounds and /or 3) voice and/or respiration blocking (9). Avoidance behaviours (like changing words to avoid stuttering) and escape behaviours (like shaking your head to escape the moment of stuttering) are considered part of the stutter.
The specialist literature normally distinguishes between stammering/stuttering and natural disfluency. Both stuttering and stammering refer to the disrupted flow of speech, but while stammering is the term used in Britain, stuttering is more commonly used in Australia, New Zealand and North America.
Natural disfluency involves fewer and easier repeats of whole words or phrases, and the use of pauses, interjections and/or filler words (10). However, it can sometimes be difficult to distinguish between natural disfluency and stuttering due to insufficiently clear definitions and classifications.
Stuttering is caused by multiple interacting factors, including hereditary, neurological, psychological, motor, linguistic and environmental (1). There is therefore no single indicator that predicts stuttering.
The study’s objective
Public health nurses at child health centres routinely see children in the 0–5 years age group. The purpose of the regular check-ups is to promote health and prevent disease and harm. According to national guidelines for the screening of vision, hearing and language in children, public health nurses are meant to identify language disorders relating to expression and comprehension as well as phonological difficulties.
It is also part of the public health nurses’ remit to identify other language-related difficulties such as pragmatic language disorder, dyspraxia and/or stuttering (11). It is therefore extremely important that public health nurses are familiar with how to distinguish stuttering from natural disfluency, to ensure that the children who need it, are referred to a speech therapist for assessment.
The purpose of this study was therefore to enhance our knowledge about public health nurses’ practices when they encounter preschool-age children with a stutter, or when they suspect a stutter. The research questions were as follows:
- Do the public health nurses distinguish between stuttering and natural disfluency?
- What is the public health nurses’ standard practice when they first encounter a child who stutters?
- What advice is given by public health nurses to the parents of children who stutter?
- What factors are considered important by the public health nurses when assessing whether a child should be referred to a speech therapist?
- Who do the public health nurses liaise with when they suspect stuttering?
Method
The questionnaire
This study forms a part of the Effective Stuttering Treatment (EST) research project, which is funded by the Research Council of Norway. This is an interdisciplinary project that seeks to establish an effective treatment for stuttering in children aged 0-6 (12). The sub-study was approved by the Norwegian Centre for Research Data under registration number 144522.
The sub-study is a descriptive cross-sectional study for which data were collected via an online questionnaire (nettskjema.no). The questionnaire was distributed in the autumn of 2019 to public health nurses working at child health centres in a random group of Norwegian counties.
The researchers on the EST project developed the questionnaire in connection with a larger survey across several professions (speech therapists, public health nurses and preschool teachers). Some of the questions were specifically intended for public health nurses while others were the same for all professions.
The online questionnaire that was sent to the public health nurses took 5–7 minutes to complete and included the following questions, with the response options provided in brackets:
- How many years have you been working as a public health nurse (number of years)?
- Have you encountered children who stutter in the last three years (yes/no)?
- On average, how many children do you see per year who stutter (number of children)?
- Do you distinguish between stuttering and natural disfluency when you see children with speech disfluencies (yes/no/don’t know)?
- Does your employer provide professional guidelines in respect of children who stutter (yes/no and free-form text answer)?
- How often do you use the following practices when you first encounter parents with a child who stutters (8 response options involving a five-point Likert scale plus free-form text answer)?
- What are the three most common pieces of advice that you give to parents when you first encounter a child who stutters (14 response options plus free-form text answer)?
- Which factors are important when you assess whether the child needs a referral/follow-up by a speech therapist (13 response options plus free-form text answer)?
- Who do you liaise with when you encounter a preschool-age child who stutters (11 response options plus free-form text answer)?
The questionnaire was pilot tested by six public health nurses before it was distributed. We revised the questionnaire based on their feedback.
Sample
The sample consisted of public health nurses from six random counties. A unique number was allocated to all Norwegian counties (2019) after which a randomiser was used to pick arbitrary numbers (13). The six counties comprised a total of 155 municipalities, some of which run several child health centres.
The survey invitation was emailed to the chief public health nurse in each municipality if their email address was in the public domain. If not, the invitation was sent to the local authority’s email address with a request to forward it to the chief public health nurse.
The chief public health nurse was asked to forward the email to all public health nurses in the municipality. The email included the information letter and a link to the online questionnaire. The chief public health nurses were also asked to report on how many public health nurses had received the forwarded survey invitation, to allow us to calculate the response rate.
Two reminders were issued to chief public health nurses who failed to report back that the invitation had been forwarded. In addition, we telephoned the child health centres in municipalities where no response had been forthcoming, in order to ascertain that the email had been received.
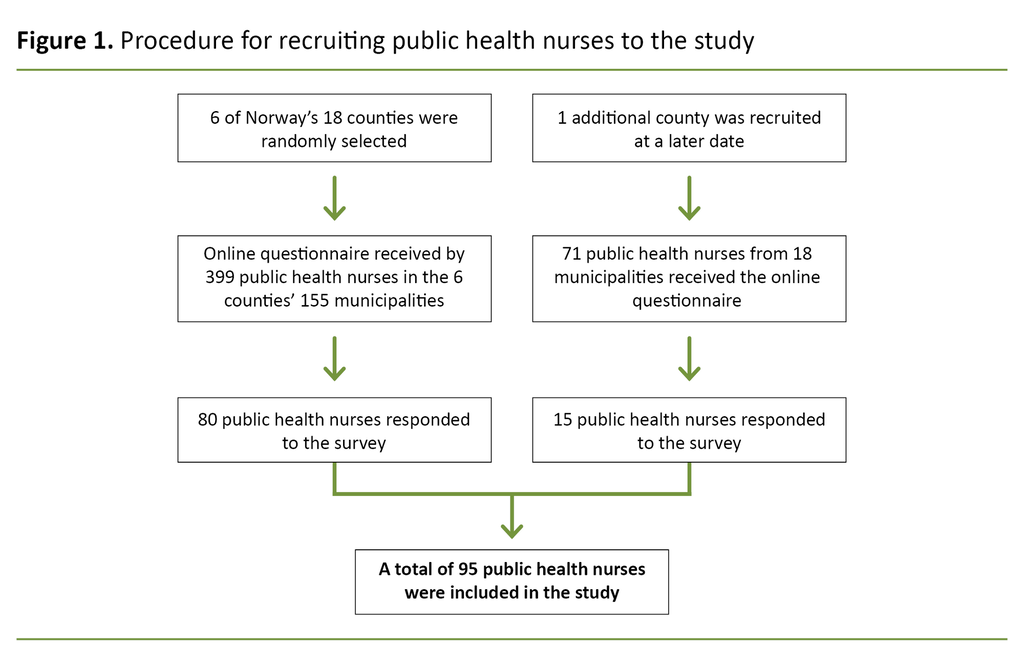
Due to a low response rate, we extended the sample to include an additional county comprising of 18 municipalities. The county was strategically chosen to ensure that both large and small municipalities were represented. In the seven counties, a total of 470 public health nurses were confirmed to have received the email that gave a link to the questionnaire and the information letter (Figure 1).
Analysis
We carried out descriptive analyses of the data material using SPSS (version 26). Both average and spread were calculated for years of experience as a public health nurse. With respect to the question about distinguishing between stuttering and natural disfluency, the ‘don’t know’ response option was re-coded to ‘no’, to make the variable dichotomous.
We conducted a t-test for independence to determine if there were statistically significant differences between the public health nurses’ years of work experience and the extent to which they distinguished between stuttering and natural disfluency. Frequencies and percentages were analysed in respect of all categorical data.
A chi-square test was conducted to determine if distinguishing between stuttering and normal disfluency was related to previously having encountered children who stutter. We also investigated whether years of work experience impacted on whether children were referred for treatment and further follow-up by a speech therapist.
We used ordinal regression analysis to determine whether years of work experience impacted on the degree to which referrals were given for further treatment. Statistical significance was set at p < 0.05. Free-form text in comment fields was categorised if more than three different respondents made the same comment.
Results
A total of 95 out of 470 public health nurses completed the questionnaire, which gave a response rate of 20 per cent. All invited counties were represented in the material, and all the respondents had completed all variables. The data sets were therefore complete. The mean for years of working as a public health nurse was 12.5 years, while the spread was 0–32 years.
Of all the public health nurses who took part in the study, 46 per cent reported that they had seen children who stutter in the course of the last three years, and that on average they saw one child with a stutter per year. Eight per cent (n = 8) of respondents answered that they had access to written professional guidelines for children who stutter, and half of these respondents had instructions that told them when to contact a speech therapist.
The local guidelines were considered to require compliance with the Directorate of Health’s national guideline for screening vision, hearing and language in children, or provided a description of natural disfluencies in children and guidance on who needs follow-up.
When we asked if the public health nurses distinguish between stuttering and natural disfluency when they see children with speech disfluencies, 56 per cent (n = 53) confirmed that they do make the distinction while 32 per cent (n = 30) responded ‘don’t know’ and 12 per cent (n = 12) responded ‘no’.
The first time they saw the parents and child, the public health nurses would normally provide information about stuttering and make a new appointment with the parents.
There were no statistically significant differences between years of working as a public health nurse and the degree to which they distinguished between stuttering and natural disfluency (t(93) = –1.089, p = 0.279) (Table 1).
There was no significant correlation between distinguishing between stuttering and natural disfluency and having previously encountered children who stutter (x²(1, N = 95) = 0.305, p = 0.581).
The first time they saw the parents and child, the public health nurses would normally provide information about stuttering and make a new appointment with the parents. Table 1 shows the different practices listed by the public health nurses as their standard procedure when they see children who stutter.
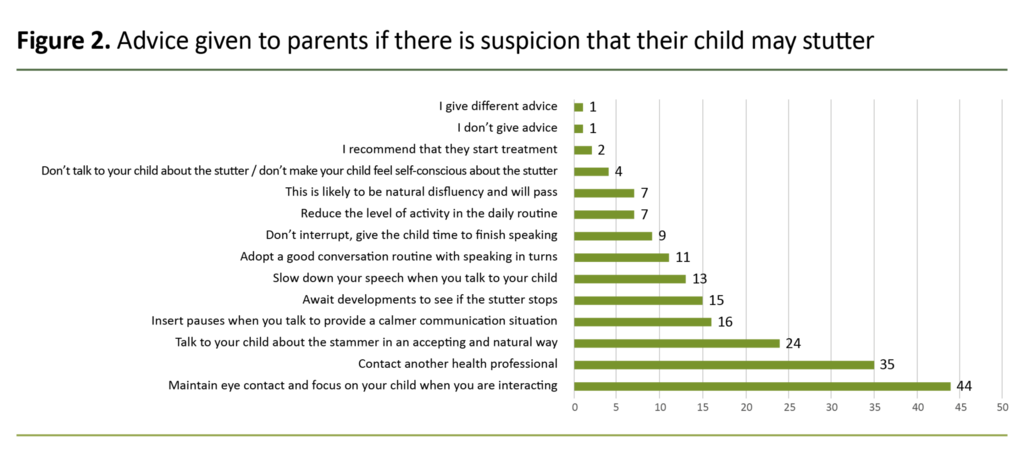
The advice most frequently given by the public health nurses to the parents of children who stutter, was to maintain eye contact with the child during interactions, to talk about the stutter in an accepting and natural way, and to contact a specialist. Figure 2 shows the advice given to parents.
The public health nurses attached importance to different factors when assessing whether a child needs to be followed up by a speech therapist. The child’s age, the child’s perception of or reaction to the stuttering and parental concern were the factors most frequently used to decide whether further follow-up or referral was required (Table 2).
In their free-form text answers, some of the public health nurses pointed out that their internal procedures included instructions from the Educational and Psychological Counselling Service that any stutter should be reported straight away.
Additionally, the Educational and Psychological Counselling Service advised the public health nurses to repeat words used by the child, using the correct phonics. Years of work experience showed no significant impact on the degree to which the public health nurses referred children for further treatment (Wald x²(1) = 0.042, p = 0.837).
The public health nurses in the study reported that they liaised with different partners in connection with children who stutter: 1.1 per cent (n =1) of the public health nurses stated that they liaise with other public health nurses, 36 per cent (n = 34) with preschool staff, 31 per cent (n = 29) with the Educational and Psychological Counselling Service, 28 per cent (n = 27) with speech therapists, 4.2 per cent (n = 4) with special needs teachers and 23 per cent (n = 22) with the parents. Three per cent (n = 3) responded that they liaise with a doctor when they encounter a child who stutters.
Discussion
The study’s objective was to enhance our knowledge of the practices adopted by public health nurses at child health centres when they encounter children who stutter or who they suspect may have a stutter.
Distinguishing between stuttering and natural disfluency
More than half the public health nurses stated that they distinguish between stuttering and natural disfluency. Many reported that repetition of syllables was an identifying factor when classifying a speech disfluency as a stutter.
This interpretation is in keeping with the study conducted by Tumanova et al. (10), which describes a stutter as frequent disfluencies in the form of part-word repetitions. Natural disfluency refers to less frequent speech disfluencies that occur between words, or repetitions of multi-syllable words.
Several public health nurses stated that they do not distinguish between stuttering and natural disfluency in young children.
Several public health nurses stated that they do not distinguish between stuttering and natural disfluency in young children. Over half the public health nurses reported that the child’s age was an important factor with respect to referral to a speech therapist (Table 2).
Tumanova et al. (10) point out that it is normal for stuttering to start at the same age as natural disfluency, and studies show that the age of the child is not a suitable indicator for distinguishing between stuttering and natural disfluency (2, 14). The reason is that stuttering can start at a very young age (two years), or at a later age (four years) (2).
Different practices at the first encounter with children who stutter
More than half the respondents reported that they gave advice about stuttering, and that they made another appointment to see the parents and child if they suspected a stutter. According to several studies, stuttering tends to start between the ages of two and four (2, 14), and early identification and treatment of stuttering is considered key to a positive prognosis (7, 8).
If stuttering is suspected, it is therefore important that the child is referred to a speech therapist as early as at the two-year check-up. Because children are not seen by public health nurses between the ages of two and four, it is important to make another appointment, as was reported to be standard practice by many of the public health nurses.
If stuttering is suspected, it is therefore important that the child is referred to a speech therapist as early as at the two-year check-up.
According to the ‘National guideline for screening vision, hearing and language in children’ issued by the Norwegian Directorate for Health and Social Affairs, the recommended course of action is to invite the child to attend a further consultation between the ages of two and four if there is uncertainty about potential stuttering. This is to ensure that the children who need help, will receive it as early as possible (11).
Just under a third of the public health nurses responded that they liaise with preschool teachers when they encounter children who stutter. Just as many reported to be liaising with the Educational and Psychological Counselling Service. A collaborative partnership with preschool teachers and the Educational and Psychological Counselling Service is a positive move, and shows that many of the public health nurses comply with the Directorate of Health’s guidelines about working with other agencies (15). Preschool teachers see the children every day over a long period of time, so liaising with them will be useful to the public health nurses. The Educational and Psychological Counselling Service can provide specialist assessment and advice and initiate treatment (16).
Type of advice given to parents
The advice that the public health nurses most frequently gave to parents, was to maintain eye contact with the child and focus on the child throughout their interactions, and to talk about stuttering in a natural and accepting way. This advice is in line with some of the practices advocated in indirect treatment programmes (17–19).
Only a small minority of the public health nurses gave other types of advice found in the treatment literature, such as inserting pauses when talking to promote a calmer style of communication, avoiding interruptions and talking slowly. However, stuttering treatment involves multiple components and is far more complex than merely providing a few recommendations and suggestions, and therapy programmes tend to be adjusted to the individual (20, 21).
Early treatment of stuttering is important to prevent negative social, emotional and behavioural consequences (3, 5, 22). Public health nurses should therefore give referrals to ensure that the children receive the comprehensive treatment they need. They must also give consistent and evidence-based advice to parents.
Different factors that are considered important when assessing the child’s need for referral to a speech therapist
The three factors that the public health nurses most frequently considered to be important to their assessment of whether a child stutters, were the child’s age, the child’s own perception of their stuttering and parental concern (Table 2). The child’s ability to play, and the severity and duration of the stuttering, were not prioritised factors.
The frequency of stuttering was given the lowest priority by the public health nurses in their assessment of whether a speech therapist should be contacted. This is not in keeping with specialist stuttering recommendations, such as those given by Guitar et al. (23), who point out that frequency of stuttering is an important indicator of severity.
However, the public health nurses often attached importance to parental concern when considering referral, which is a positive finding because the study conducted by Einarsdottir and Ingham (24) points out that parents are largely able to differentiate between stuttering and natural disfluency. According to them, considerable importance should therefore be attached to parental concern in any assessment of whether to give a referral to a speech therapist.
The child’s ability to play, and the severity and duration of the stuttering, are not prioritised factors.
According to the national regulations that impose a duty on local authorities to carry out health promotion and preventive work in child health centres and through the school health service (25), screening must be carried out to identify risks of physical and mental issues/problems and developmental anomalies (25, s. 5d).
In order to comply with the regulations and the national guidelines (11, 15) it is important that the public health nurses assess the children’s communication in order to identify stuttering at an early stage. They must therefore have knowledge of the main symptoms of stuttering and give advice that is in line with the most recent research. It has been established that various professions who work with children have insufficient knowledge about stuttering and its cause and treatment (26, 27).
Public health nurses have many different responsibilities and are required to have extensive knowledge about children’s health and development. They are also asked to carry out preventive work as well as health promotion. During the regular check-ups at two and four years of age, significant attention is given to language and language development, while stuttering may well not receive the same level of attention.
For example, the handbook which is available at many child health centres (28) suggests that stuttering tends to start between the ages of six and ten. This may have led to less attention being given to stuttering in the younger age groups.
Strengths and weaknesses of the study
One weakness of the study is the fact that we developed a new questionnaire because there was no relevant international validated questionnaire available for our target group and objective. The advantage of developing a dedicated questionnaire was that it could be customised to a Norwegian setting. Also, because similar questionnaires were developed for speech therapists and preschool teachers, this gave an opportunity for validation across several professional groups.
Another weakness of the study is the low response rate, which limits its external validity and makes it more difficult to draw conclusions in respect of other public health nurses beyond those who took part in the study. The national guidelines for the screening of vision, hearing and language in children only devote a few sentences to stuttering (15), and relevant specialist Norwegian literature states that the onset of stuttering is most often seen between the ages of six and ten (28).
These factors may have meant that many public health nurses who work with children under the age of five, considered the questionnaire to be irrelevant to them (29). Moreover, a response rate of approximately 30 per cent is relatively common for online questionnaires (29, 30).
The strength of this study is that the sample, in general, was randomly chosen from the population it represents, which means that the responses reflect the perceptions of public health nurses within given margins of error. With a response rate of 20, this study’s margin of error is +/–9.0 per cent, with a 95 per cent confidence level.
Despite this margin of error, the study is nevertheless the first in Norway to examine public health nurses’ practices in relation to children who stutter and can therefore suggest relevant target areas for further efforts and more research.
Conclusion
The study showed that the practices adopted by public health nurses, and the advice they give to parents of children who stutter, normally coincide with recent recommendations given in international research literature. However, the public health nurses in our study do not comply with recommended practice with respect to which children should be referred to a speech therapist, because the public health nurses rarely attach importance to repetitions, prolongations and blocks when assessing children’s speech.
The results suggest that public health nurses need more knowledge about stuttering and clearer guidance on when and how to spot stuttering during child health centre check-ups to ensure that the right children are identified and can benefit from early intervention.
We would like to thank all the chief public health nurses and other managers who distributed the invitation to take part in the study, and to all the public health nurses who completed the questionnaire.
References
1. Smith A, Weber C. How stuttering develops: the multifactorial dynamic pathways theory. 2017 sep.;60(9):2483–505. DOI: 10.1044/2017_JSLHR-S-16-0343
2. Reilly S, Onslow M, Packman A, Cini E, Conway L, Ukoumunne OC et al. Natural history of stuttering to 4 years of age: a prospective community-based study. Pediatrics. 2013 sep.;132(3):460–7. DOI: 10.1542/peds.2012-3067
3. McAllister J. Behavioral, emotional and social development of children who stutter. J Fluency Disord. 2016 des.;50:23–32. DOI: 10.1016/j.jfludis.2016.09.003
4. Guttormsen LS, Stokke L, Kefalianos E, Næss K-AB. Communication attitudes in children who stutter: a meta-analytic review. J Fluency Disord. 2015 des.;46:1–14. DOI: 10.1016/j.jfludis.2015.08.001
5. Iverach L, O'Brian S, Jones M, Block S, Lincoln M, Harrison E et al. Prevalence of anxiety disorders among adults seeking speech therapy for stuttering. J Anxiety Disord. 2009 okt.;23(7):928–34. DOI: 10.1016/j.janxdis.2009.06.003
6. Craig A, Blumgart E, Tran Y. The impact of stuttering on the quality of life in adults who stutter. J Fluency Disord. 2009 jun.;34(2):61–71. DOI: 10.1016/j.jfludis.2009.05.002
7. O’Brian S, Iverach L, Jones M, Onslow M, Packman A, Menzies R. Effectiveness of the Lidcombe Program for early stuttering in Australian community clinics. Int J Speech Lang Pathol. 2013 des.;15(6):593–603. DOI: 10.3109/17549507.2013.783112
8. Onslow M, Lowe R. After the RESTART trial: six guidelines for clinical trials of early stuttering intervention. Int J Lang Commun Disord. 2019 jul.;54(4):517–28. DOI: 10.1111/1460-6984.12463
9. Yairi E, Watkins R, Ambrose N, Paden E. What is stuttering? JSHD. 2001 jun.;44(3):585–92. DOI: 10.1044/1092-4388(2001/046)
10. Tumanova V, Conture EG, Lambert WE, Walden TA. Speech disfluencies of preschool-age children who do and do not stutter. J Commun Disord. 2014 mai–jun.;49:25–41. DOI: 10.1016/j.jcomdis.2014.01.003
11. Sosial- og helsedirektoratet. Retningslinjer for undersøkelse av syn, hørsel og språk hos barn. Oslo: Sosial- og helsedirektoratet; 2006. IS-1235. Available at: https://www.helsedirektoratet.no/retningslinjer/helsestasjons-og-skolehelsetjenesten/helsestasjon-05-ar/horsel-syn-og-sprak/Unders%C3%B8kelse%20av%20syn,%20h%C3%B8rsel%20og%20spr%C3%A5k%20hos%20barn%20%E2%80%93%20Nasjonal%20faglig%20retningslinje.pdf/_/attachment/inline/c2e84a1c-7765-421d-83b6-c31e912c68ed:0610f899cdb717a93e5c6175b1fcb0cb5f1d2c10/Unders%C3%B8kelse%20av%20syn,%20h%C3%B8rsel%20og%20spr%C3%A5k%20hos%20barn%20%E2%80%93%20Nasjonal%20faglig%20retningslinje.pdf. (downloaded 19.10.2020).
12. Universitetet i Oslo. The Effective Stuttering Treatment Project (EST) [publisert 13.08.2018, oppdatert 16.01.2020, sitert 12.02.2021]. Oslo: Universitetet i Oslo, Institutt for spesialpedagogikk. Available at: https://www.uv.uio.no/isp/forskning/prosjekter/effective-stuttering-treatment-project-/
13. Number Generator. Available at: https://numbergenerator.org/%20randomnumbergenerator/1-18 (downloaded 20.09.2020).
14. Månsson H. Childhood stuttering: incidence and development. J Fluency Disord. 2000;25:47–57. DOI: 10.1016/S0094-730X(99)00023-6
15. Helsedirektoratet. Nasjonal faglig retningslinje for helsestasjon og skolehelsetjeneste. Oslo: Helsedirektoratet; 2017. Available at: https://www.helsedirektoratet.no/retningslinjer/helsestasjons-og-skolehelsetjenesten/helsestasjon-05-ar/horsel (downloaded 20.09.2020).
16. Lov 17. juni 2005 nr. 64 om barnehager (barnehageloven). Available at: https://lovdata.no/dokument/NL/lov/2005-06-17-64 (downloaded 20.09.2020).
17. Millard SK, Zebrowski P, Kelman E. Palin. Parent–child interaction therapy: the bigger picture. Am J Speech Lang Pathol. 2018 okt.19;27(3S):1211–23. DOI: 10.1044/2018_AJSLP-ODC11-17-0199
18. Yaruss JS, Coleman C, Hammer D. Treating preschool children who stutter: description and preliminary evaluation of a family-focused treatment approach. Lang Speech Hear Serv Sch. 2006 apr.;37(2):118–36. DOI: 10.1044/0161-1461(2006/014)
19. de Sonneville-Koedoot C, Stolk E, Rietveld T, Franken M-C. Direct versus indirect treatment for preschool children who stutter: The RESTART Randomized Trial. PLoS One. 2015 jul 28;10(7):e0133758. DOI: 10.1371/journal.pone.0133758
20. Millard SK, Davis S. The Palin Parent Rating Scales: parents' perspectives of childhood stuttering and its impact. J Speech Lang Hear Res. 2016 okt.;59(5):950–63. DOI: 10.1044/2016_JSLHR-S-14-0137
21. Yaruss JS, Reardon-Reeves N. Early childhood stuttering therapy: a practical guide. McKinney, Texas: Stuttering Therapy Resources; 2017.
22. Davis S, Howell P, Cooke F. Sociodynamic relationships between children who stutter and their non-stuttering classmates. J Child Psychol Psychiatry. 2002 okt.;43(7):939–47. DOI: 10.1111/1469-7610.00093
23. Guitar B. Stuttering: an integrated approach to its nature and treatment. Baltimore: Lippincott Williams & Wilkins; 2014.
24. Einarsdóttir J, Ingham R. Accuracy of parent identification of stuttering occurrence. Int J Lang Commun Disord. 2009 nov.–des.;44(6):847–63. DOI: 10.1080/13682820802389865
25. Forskrift 19. oktober 2018 nr. 1584 om kommunens helsefremmende og forebyggende arbeid i helsestasjons- og skolehelsetjenesten. Available at: https://lovdata.no/dokument/SF/forskrift/2018-10-19-1584 (downloaded 20.09.2020).
26. Abdalla FA, St. Luis KO. Arab school teachers' knowledge, beliefs and reactions regarding stuttering. J Fluency Disord. 2012 mar.;37(1):54–69. DOI: 10.1016/j.jfludis.2011.11.007
27. Winters KL, Byrd CT. Pediatrician referral practices for children who stutter. Am J Speech Lang Pathol. 2020 aug.;4:1404–22. DOI: 10.1044/2020_AJSLP-19-00058
28. Brigtsen AK, Lagerløv P. Barnemedisin. In: Misvær N, Lagrløv P, eds. Håndbok for helsestasjoner 0–5 år. 4th ed. Oslo: Kommuneforlaget; 2018. p. 434.
29. Nulty CD. The adequacy of response rates to online and paper surveys: what can be done? Assess Eval High Educ. 2008 apr.;33(3):301–14. DOI: 10.1080/02602930701293231
30. Safdar N, Abbo LM, Knobloch MJ, Seo SK. Research methods in healthcare epidemiology: survey and qualitative research. Infect Control Hosp Epidemiol. 2016 nov.;37(11):1272–7. DOI: 10.1017/ice.2016.171












Comments