New practice model improved students’ leadership and organisational skills
At the University of Tromsø, first year students in nursing homes are supervised by final year students in order to strengthen their occupational competence in nursing leadership.
Background: Nurses form the largest group of health personnel in the municipal health and care services. Even as newly qualified nurses, they are expected to have nursing leadership skills in order to be able to organise and manage patient care. Nursing education programmes together with the field of practice share joint responsibility for developing theoretical and practical knowledge to enable nurses to acquire occupational competence in nursing leadership.
Objective: The objective of this study was to gain knowledge of how the students perceive their own development of occupational competence in nursing leadership following the introduction of a new practice model in the sixth semester. The students’ experiences provide key knowledge for developing the practice model in accordance with the requirements of the field of practice regarding newly qualified nurses.
Method: We chose a qualitative approach using student focus groups at the conclusion of the clinical practice period in spring 2016, utilising qualitative content analysis.
Results: The study shows that a new practice model can help to boost the students’ leadership and organisational skills, thereby helping to reduce the gap between nursing education and nursing homes’ expectations of newly qualified nurses.
Conclusion: The students faced challenges linked to nursing leadership, student supervision, involvement in quality assurance work as well as interprofessional collaboration. The study shows that the balance between challenges and reflection is central for learning and critical thinking in nursing.
Changes in the health and care sector in recent years have led to requirements for better interaction, coordination and more effective services while also safeguarding patient safety and quality (1–3). These changes affect the education of health personnel, and nursing education must correspond to competence needs – particularly in the municipal health services (4).
Nursing leadership
Earlier research shows that increasing the focus on nursing leadership skills helps to ensure good quality care and patient treatment (5, 6).
Nursing leadership involves tasks intended to secure professional content and flow in work processes related to the patient (7, 8). The main task is to assess the patient’s need for nursing, evaluate nursing measures, and coordinate interaction with other professions. This function also includes responsibility for delegating tasks, following up and collaborating with colleagues as well as interacting with other professions. In addition, nurses are responsible for professional updating and documentation (8).
Nursing leadership is challenging and is characterised by working methods with clear goals, professional problems being solved jointly with others, while communication and interaction skills are paramount (9). Learning outcomes at the end of nursing education programmes include requirements for knowledge and skills in coordination, professional development and communication. It is also expected that the candidate is a change-oriented leader in their field (10).
Earlier research
Earlier studies show, however, that newly qualified nurses lack competence in nursing leadership and that they are not prepared for tasks linked to leadership and the organisation of patient care (11–14). Research also shows that newly qualified nurses do not acquire occupational competence in nursing leadership until three years after the end of their education (11, 13).
Meanwhile employers expect nurses to possess such skills at the time of their appointment. A number of researchers point out that there is a need to strengthen nursing education in order to close the gap between education and the employer’s expectations, particularly in terms of leadership and organisation (5, 9, 12, 15).
Explanation of concepts
The National Framework Curriculum for the Bachelor Degree in Nursing uses the terms ‘occupational tools’ and ‘occupational competence’ (16). Occupational tools include areas in which nursing education helps to ensure that newly qualified nurses have knowledge of the field while lacking experience in acting independently (16).
Occupational competence encompasses areas where nursing education is responsible for enabling newly qualified nurses to function independently (17). Competence is linked to the subject-related context, the individual mental process and the social context in which competence is developed and applied. Occupational competence is developed and realised through action.
Students’ occupational competence
At UiT – The Arctic University of Norway, Narvik campus, we wanted to strengthen nursing students’ occupational competence in nursing leadership. We devised a course plan in the sixth semester for a new practice model at nursing homes (18). The course plan focuses on students acquiring occupational competence in managing and organising nursing, and participating in interprofessional collaboration as well as supervising first year students, colleagues and patients.
The students must complete coursework requirements during the clinical practice period. Coursework requirements focus on health-promoting and preventive nursing, which entails project management and interaction with several actors. Moreover, students must gain knowledge about and contribute to quality improvement measures, internal controls and clinical incident reporting.
We devised the practice model in collaboration with managers and practice supervisors at nursing homes. Collaboration with the field of practice was necessary in order to gain a joint understanding of the subject-related content of the course and to understand the obligations of nursing education and the field of practice to implement the practice model.
Objective of the study
The objective of this study was to gain knowledge of how the students perceived their own development of occupational competence in nursing leadership following the introduction of the new practice model in the sixth semester. The students’ experiences provide key knowledge for developing the practice model in accordance with the requirements of the field of practice regarding newly qualified nurses.
This study examines the following research question:
What is the students’ personal experience with developing occupational competence in nursing leadership during clinical practice in the nursing home?
Method
In order to answer the research question, we used a qualitative approach with a descriptive, exploratory design. We used the focus group interview as a data collection method. The discussion between the participants led to ideas for potential improvements as well as further elaboration of the issue.
Two important elements characterise focus group interviews. The first is that the group must be headed by a moderator who presents a well-defined topic and helps to keep the participants on track without influencing the group. The second is the aim of eliciting elicit participants’ perceptions of the topic presented, and their attitudes and feelings towards it (19). The method is therefore well suited to collecting data with a view to developing practice (20).
Focus group interviews
We conducted focus group interviews in the study at the end of the clinical practice period in spring 2016. The sample consisted of students who had had clinical practice at four different nursing homes. We undertook three focus group interviews chaired by a moderator. One of the authors carried out two focus group interviews while the other author conducted one. The third author transcribed the data material.
The number of participants in the focus group interviews varied from two to seven, and altogether twelve students participated in the study. We had devised a study guide with six open-ended questions that centred on students’ experiences with managing and administering a ward, supervising first year students, and how the practice contributed to their knowledge of nursing leadership.
The participants were active and the moderator’s role was to ensure that they discussed the stated topic. The moderator had good knowledge of the content of the practice model and could follow up important elements. The focus group interviews were recorded digitally and transcribed verbatim.
Review of method
The moderator was the teaching supervisor for the students when they carried out their practice, which may have affected what students chose to bring up in the focus group interviews. The students had completed their practice, therefore the discussions did not affect the final assessment.
We distributed an information letter and an invitation to participate in the project to a strategic sample of altogether twenty students who had carried out practice at four nursing homes in the sixth semester. The non-participation of eight students may have been related to the fact that the interviews were conducted after the end of the clinical practice period, and that the students were engaged in other tasks. Due to these students withdrawing a short time before the interviews, two of the groups consisted of only two and three participants respectively in addition to the moderator.
The fact that two of the groups had few participants resulted in a sub-optimal interaction among the participants, and the discussions were less nuanced. While having few participants may prevent the formation of groupings in focus group interviews, it can be difficult to elicit the range of opinions that emerge in larger groups (19).
Despite the small number of participants, we chose, nevertheless, to carry out the focus group interviews out of consideration for the participants. Based on the resource situation, we conducted the interviews without an observer, which may have led to less focus on the interaction in the groups.
We have been involved in the entire process, from supervising students in practice to conducting focus group interviews, and interpreting and analysing their content. The person who did not act as a moderator during the focus group interviews had an ‘outsider perspective’ on the material.
Ethical considerations
We obtained written, informed consent, and the participants were informed that they could withdraw from the survey at any time, although no one did so. The study was reported to the Norwegian Centre for Research Data. We anonymised directly identifiable personal data in the transcription and stored the data in accordance with UiT’s current guidelines.
Analysis
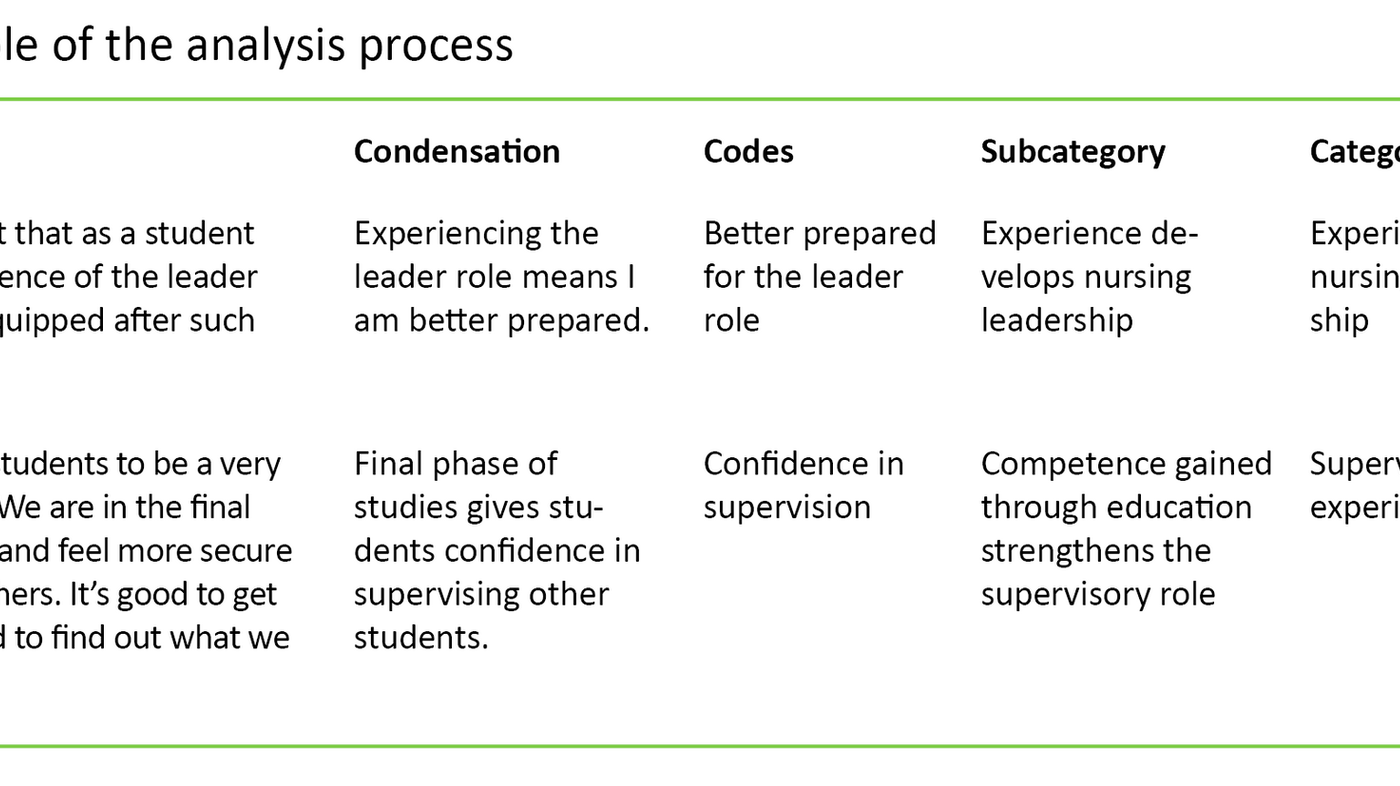
We employed qualitative content analysis inspired by Graneheim, Lindgren and Lundman (21, 22). Qualitative content analysis is characterised by a systematic analysis of the text in order to understand how the text gives meaning and content to a particular phenomenon (22).
In the first part of the analysis, we read through all the text several times in order to gain an overview of the dataset. Then we split the text into meaning units that were condensed and coded. In order to elicit the manifest content of the material, we identified subcategories in our analysis. This resulted in four categories:
- experience of nursing leadership
- supervisory experience
- participation in quality assurance work
- challenges posed by a lack of interprofessional interaction.
Results
Here we present the findings of the study divided into the four above-mentioned categories, underpinned by the participants’ statements in the focus group interviews.
Experience of nursing leadership
Our findings reveal that the students were satisfied that they had been challenged to function as nurse leaders in the ward. They found that the practice supervisors ‘took a back seat’ and delegated much of the responsibility for the daily organisation of patient care to the students. This meant that the students felt more secure about the challenges they faced.
One participant remarked: ‘We have been challenged and have really experienced the responsibilities we will have when we graduate as nurses.’ Another said: ‘I think it’s important that as a student you get some experience of the leader role. We’re better equipped after such practice.’
Many of the students felt greater confidence in their professional platform in relation to the personnel group. The students discussed the fact that their views and professional input were acknowledged and listened to in a different way from in earlier clinical practice periods. One participant expressed it as follows: ‘During this practice period I felt that I was listened to from day 1. My input regarding patients was taken into consideration. They were more open to listening to us because we would shortly be qualified nurses.’
During the clinical practice, the students were expected to take over the work for two days. The personnel could hold meetings and carry out internal training, while the students were responsible for the patients and the first year students. The participants described this as good experience that also challenged them to organise their own work. One participant said: ‘Managing the ward was very educational, and I was challenged to delegate work tasks … that’s a little difficult.’
Supervisory experience
Nursing students supervise first year students as part of the coursework requirements in the sixth semester. Our findings indicate that all participants benefitted considerably from this task. They said that their own experience of different practice supervisors gave them greater insight into the supervisor role.
One of the participants said: ‘I found supervising students to be a very positive experience. We are in the final phase of our studies and feel more secure about supervising others. It’s good to get some experience and to find out what we can do better.’ Another expressed this in the following way: ‘A lot of people don’t take being a supervisor seriously enough. It actually requires a lot of work, both before and after. What could we have done differently … in order to give feedback.’
The students were to have responsibility for ward management for two days together with the first year students. As supervisors, they had to be aware that personal hygiene care takes time, and the first year students needed supervision in using the patients’ resources.
One participant said: ‘They [first year students] worked too slowly because they lacked experience. I had one [student] who spent one and a half hours on a patient’s shower when the patient could manage most of it on their own. They are too careful at the start.’
Participation in quality assurance work
The students discussed their experiences of incident reporting from the clinical practice period. They gave many specific examples of situations in which incidents were recorded and documented. Our findings indicate that practice varies at the individual institutions, and that the students were unsure what they were supposed to write incident reports about.
One of them said: ‘There was a very high threshold for writing incident reports. Quite a lot had to happen before they were written.’ Several of the students had no clear idea of what routines applied or how the incident reports were dealt with higher up in the system, as shown by the words of this participant: ‘We asked what happens to these incident reports, what’s done with them, and who looks at them. But even so, I was none the wiser.’
As nurse leaders in the wards, the students gained experience of documenting nursing. The participants stated unequivocally that there was a lack of documentation and that the reports were mainly oral reports about the patient’s situation. One participant expressed this as follows: ‘The documentation is a challenge for the ward, there’s no common approach.’
The participants expressed criticism of the fact that only nurses could provide documentation and a very small number of other employees or a few of the agency nurses. One participant said as follows: ‘Very brief notes and a lot of unusable information. When I read the documentation, I wondered what was the point of writing this. I wouldn’t accept it if I worked there.’
Challenge posed by the lack of interprofessional interaction
The study indicates that nursing home employees had little interprofessional interaction. The various services, physiotherapy and ergonomics for example, are requisitioned for the individual patient as required.
The nurses interacted mainly with the doctor, and much of the contact with other professions took place via the telephone. The participants felt that they liaised well with the doctor, and that they were challenged to answer questions and discuss treatment and medication.
However, some students talked about challenges related to dialogue with the doctors. One participant said: ‘At the start I had to kind of go along with what the doctor said. The nurses gave me tips about what I should say, so that improved over time.’ Another participant said: ‘You often have to stand your ground to get things approved regarding the patient. We know the patient best.’
Discussion
The study shows that the students gained greater insight into the nurse’s leader role at the nursing home following the introduction of the new practice model. Nursing leadership must be strengthened because nursing homes are characterised by a lack of nursing positions, understaffing and increased pressure on the nurses (23, 24). This puts a great personal responsibility on the individual nurse and requires a high level of proficiency in their work (7).
The nursing leadership role was demonstrated by the students’ participation in both patient-related and organisational duties. Practice in which the main emphasis is on nursing leadership can help to challenge both the education and the field of practice in knowledge-based practice. The students are updated regarding new theory, and become more aware of the core values necessary for developing occupational competence (25).
The practice supervisor’s approach strengthened the students’ commitment and allowed them to ask critical questions. Critical reflection and dialogue can increase the professional quality of nursing homes as a learning arena (9).
Enhanced occupational competence
The dataset shows that when the students took over the ward for a given period, this allowed them to ‘lift their gaze’ and recognise both the clinical and organisational challenges entailed in being a nurse leader. The students had to organise work with several patients and allocate work tasks to colleagues, which challenged their abilities to organise teamwork. Attention to individual care and the nurses’ core values were safeguarded (25).
The students’ occupational competence increased when the nursing home management, the practice supervisor and the teaching supervisor showed trust in them and gave them responsibilities that they could master. The practice supervisors were accessible and ensured that the students safeguarded professional accountability. According to Blekken et al. (12), taking over the ward gives the students more realistic experience as nurse leaders.
Student supervisors experienced mastery
The course description includes the topic of communication and supervision, which constitutes one of the prerequisites for creating trust and good interaction with patients and their families, colleagues and students. Orvik (9) refers to the supervision of colleagues as an important part of nursing leadership. The students faced the challenge of supervising first year students in basic nursing.
The findings show that the students found that they mastered the supervision of first year students, and this is supported by other studies (12). The participants’ occupational competence developed through their having enough time, and having to use their theoretical knowledge and practical experience in supervision.
Developed awareness of quality assurance work
The findings also show that provision was made for complying with quality development requirements in nursing homes to a varying degree. This may be associated with the nurses’ limited time, resources and knowledge of following up requirements imposed on nursing homes (23). Arntzen (26) maintains that the main instruments in quality assurance work are the personnel’s knowledge and competence as well as their satisfaction in being successful at their jobs.
The findings show that the students developed their occupational competence by participating actively in reporting deviations. However, they expressed uncertainty regarding how these were dealt with higher up in the organisation. Incident reporting is possibly not regarded as important knowledge for nurses in the municipal health services (12).
The study shows that the students gradually developed awareness of quality assurance work and were critical to the lack of follow-up. This particularly applied to reporting and dealing with incidents, and documentation of nursing. The students also saw the necessity of basing changes in routines on a professional assessment. The nurses who supervised the students during the clinical practice period found that the students became important discussion partners and put forward specific suggestions for improvements (27). The practice model can thereby help to improve the quality of the practice.
Interprofessional collaboration
The findings show that the students had little experience of interprofessional approaches to patients in nursing homes. A prerequisite for providing a holistic range of services to patients is close interaction between nurses and other professional groups based on the patients’ individual needs (1). The lack of a variety of care professions in the municipal health services leads to a reduced range of services in nursing homes.
The students’ limited experience of interprofessional collaboration may mean that they are not aware of the nurse’s role in respect of this. Nursing leadership is about ensuring collaboration and flow in patient work (9). Awareness of your own role and responsibility as a professional manager requires more focus on interprofessional approaches in order to address the complexity of patient treatment in nursing homes (28).
The nurse leader role entails building relationships and developing the group as a team (9). When other professions are absent from the nursing home, this poses an even greater challenge to the nurses’ competence.
As qualified nurses, the students must be relatively well prepared to meet the challenges faced by the health and care services in the future. The new course plan is intended to enhance the students’ nursing leadership by putting the spotlight not only on occupational tools but also on occupational competence. Nursing leadership competence will also be of key importance for nurses in the health and care services going forward (29, 30).
Conclusion
The objective of our study was to gain knowledge about students’ experiences of how the new practice model introduced in the sixth semester can help to strengthen nursing leadership. The study shows that a new practice model can help to enhance students’ leadership and organisational skills, thereby reducing the gap between nursing education and nursing homes’ expectations of newly qualified nurses.
The students participated actively in nursing tasks and functions at the nursing home together with practice supervisors and other personnel. The study shows that a critical examination of, among other things, quality at the nursing home and the lack of interprofessional collaboration promotes discussion and boosts nurses’ awareness of their professional responsibility.
The practice model will be further developed in cooperation with students, practice supervisors and teaching supervisors. We are conducting further studies of practice supervisors’ and unit heads’ experiences following the implementation of the new practice model. A follow-up study of students educated in line with the new practice model will also be of interest.
References
1. St.meld. nr. 47 (2008–2009). Samhandlingsreformen – Rett behandling – på rett sted – til rett tid. Oslo: Helse og omsorgsdepartementet; 2009.
2. Lov 24. juni 2011 nr. 30 om kommunale helse- og omsorgstjenester m.m. (helse- og omsorgstjenesteloven). Available at: https://lovdata.no/dokument/NL/lov/2011-06-24-30 (downloaded 03.06.2018).
3. Meld. St. nr. 11 (2014–2015). Kvalitet og pasientsikkerhet. Oslo: Helse- og omsorgsdepartementet; 2014.
4. Meld. St. nr. 13 (2011–2012). Utdanning for velferd. Oslo: Kunnskapsdepartementet; 2012.
5. Curtis EA, de Vries J, Sheerin FK. Developing leadership in nursing: exploring core factors. British Journal of Nursing. 2011;20(5):306–9.
6. Dyess S, Sherman R. Developing the leadership skills of new graduates to influence practice environments: a novice nurse leadership program. Nursing Administration Quarterly. 2011;35(4):313–22.
7. Kristoffersen NJ. Sykepleierens ansvar og arbeidsområder i helsetjenesten. In: Kristoffersen NJ, Nortvedt F, Skaug E-A, Grimsbø GH, eds. Grunnleggende sykepleie. Sykepleie – fag og funksjon, bind 1. Oslo: Gyldendal Akademisk; 2016.
8. Pfeiffer R. Sykepleier og leder : den administrative og den faglige sykepleielederens funksjon. Bergen: Fagbokforlaget; 2002.
9. Orvik A. Organisatorisk kompetanse : innføring i profesjonskunnskap og klinisk ledelse. Oslo: Cappelen Damm Akademisk; 2015.
10. Universitetet i Tromsø, Norges arktiske universitet. Fagplan Bachelor i sykepleie 2016. Available at: https://uit.no/Content/479258/cache=20171003123257/Fagplan-bachelor-i-sykepleie-h%C3%B8st2016.pdf(downloaded 01.03.2018).
11. Solli H. Nyutdannede sykepleieres utvikling fra handlingsberedskap til handlingskompetanse. Sykepleien Forskning. 2009;4(1):52–60. Available at: https://sykepleien.no/forskning/2009/04/nyutdannede-sykepleieres-utvikling-fra-handlingsberedskap-til-handlingskompetanse(downloaded 01.11.2018).
12. Blekken LE, Medby AO, Forbord T. Læringsutbytte i sykepleiefaglig ledelse etter praksis der sykepleierstudenter overtok ansvaret for en avdeling. Sykepleien Forskning. 2013;8(4):344–52. Available at: https://sykepleien.no/forskning/2013/11/laeringsutbytte-i-sykepleiefaglig-ledelse-etter-praksis-der-sykepleierstudenter(downloaded 18.10.2018).
13. Dyess S, Sherman RO. Developing a leadership mindset in new graduates. Nurse Leader. 2010;8(1):29–33.
14. Ekström L, Idvall E. Being a team leader: newly registered nurses relate their experiences. Journal of nursing management. 2015;23(1):75–86.
15. Nilsen SR, Gjellebæk C, Brynhildsen S, Tjøstolvsen I, Johansen SG. Studenter trenger å lære organisering. Sykepleien 2015;103(11):60–3. Available at: https://sykepleien.no/forskning/2015/10/organisasjonskompetanse(downloaded 18.10.2018).
16. Kunnskapsdepartementet. Rammeplan for sykepleierutdanningen 2008. Available at: https://www.regjeringen.no/globalassets/upload/kd/vedlegg/uh/rammeplaner/helse/rammeplan_sykepleierutdanning_08.pdf(downloaded 03.06.2018).
17. Nygren P. Handlingskompetanse : om profesjonelle personer. Oslo: Gyldendal Akademisk; 2004.
18. Universitetet i Tromsø, Norges arktiske universitet. Læreplan for praksisstudier kommunehelsetjenesten 6. semester. Narvik; 2017. (Upublisert).
19. Halkier B. Fokusgrupper. Oslo: Gyldendal Akademisk; 2010.
20. Karlsson B, Lerdal A. Bruk av fokusgruppeintervju. Sykepleien Forskning. 2008;3(3):172–5. Available at: https://sykepleien.no/forskning/2009/02/bruk-av-fokusgruppeintervju(downloaded 01.11.2018).
21. Graneheim UH, Lindgren BM, Lundman B. Methodological challenges in qualitative content analysis: A discussion paper. Nurse Education Today. 2017;56:29–34.
22. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004;24(2):105–12.
23. Gautun H, Øien H, Bratt C. Underbemanning er selvforsterkende. Konsekvenser av mangel på sykepleiere i hjemmesykepleien og sykehjem. Rapport 6/16: Oslo: NOVA, Velferdsforskningsinstituttet; 2016.
24. Pedersen KR, Tingvoll W-A. Kompetanseutfordringer i sykehjem – en studie basert på sykepleieres erfaring fra hverdagssituasjoner. In: Kassah BL, Tingvoll W-A, Kassah AK, eds. Samhandlingsreformen under lupen : kvalitet, organisering og makt i helse- og omsorgstjenestene. Bergen: Fagbokforlaget; 2014.
25. Karoliussen M. Tilbake til kjerneverdiene. Sykepleien. 2015;103(2):62–4. Available at: https://sykepleien.no/forskning/2015/02/tilbake-til-kjerneverdiene(downloaded 18.10.2018).
26. Arntzen E. Ledelse og kvalitet i helsetjenesten : arbeidsglede og orden i eget hus. Oslo: Gyldendal Akademisk; 2014.
27. Pedersen K, Nymo R, Tingvoll W-A. De kommer som sykepleiere, ikke som studenter. Geriatrisk sykepleie. 2018;(1):28–35. Available at: https://sykepleien.no/meninger/innspill/2018/02/de-kommer-som-sykepleiere-ikke-som-studenter(downloaded 18.10.218).
28. Tingvoll W-A, Sæterstrand TM. Sykehjemmets rolle i fremtidens helsevesen. Tidsskrift for Den norske legeforening. 2007;127(17):2274–5.
29. Meld. St. nr. 26 (2014–2015). Fremtidens primærhelsetjeneste – nærhet og helhet. Oslo: Helse – og omsorgsdepartementet; 2015.
30. Tyrholm BV, Kvangarsnes M, Bergem R. Mellomlederes vurdering av kompetansebehov i sykepleie etter samhandlingsreformen. In: Kvangarsnes M, Håvold JI, Helgesen H, eds. Innovasjon og entreprenørskap. Oslo: Universitetsforlaget; 2016.










Comments