Fathers want to play a more active role in pregnancy and maternity care and at the child health centre
The father’s role has changed, and fathers have become more active as regards childcare. Nevertheless, they may feel excluded during pregnancy, childbirth and follow-up at the child health centre.
Background: In recent years, pregnancy and maternity care and the child health centre have changed. Instead of only focusing on mother and child, they now try to include the whole family. Meanwhile the father’s role has changed, and fathers play a more active role in childcare. Despite this, mothers remain the main users of the healthcare services. Little research has been conducted on how fathers feel the healthcare services cater for their interests, and what can be done to increase fathers’ participation.
Objective: The purpose of the study was to describe first-time fathers’ perceptions of the encounter with pregnancy, maternity and post-natal care and the child health centre throughout the pregnancy and birth, and in the child’s first three months of life.
Method: The study has a qualitative design and consists of nine individual interviews with first-time fathers. We carried out a qualitative content analysis of the data material.
Results: We identified two categories that describe the fathers’ encounter with the healthcare services: being on the outside and inclusion. Being on the outside is described through two sub-categories – exclusion and being overridden. Inclusion deals with the fathers’ perceptions of adaptation and participation in the healthcare services.
Conclusion: The study describes healthcare services where fathers experience a varying degree of inclusion. The services focus mainly on mother and child, even though the family perspective should apply. The fathers want to play a more active role and be more included during pregnancy, childbirth and follow-up at the child health centre. In order to attain this degree of inclusion, the healthcare services must acknowledge fathers as independent and equal carers. They must also make better provision for the participation of fathers.
Pregnancy and maternity care and the child health centre have undergone considerable changes in recent years. Instead of solely focusing on providing help to mother and child, the services now try to include the whole family. The gender perspective, men’s needs and service user participation must be key factors in the design of the healthcare services, and guidance must be aimed at both parents (1–3).
The father’s role is being expanded, and the development keeps pace with the changing role of men, both in the family and in society. The pattern of family formation and cohabitation is in a process of change, and today encompasses several different forms of cohabitation. The family concept is broadening, and often includes more people and different combinations than the traditional nuclear family. Modern paternity also comprises a paternal role that is independent of sexual orientation and ethnic background (4, 5).
Changed family pattern
The family pattern has shifted from the nuclear family to the symmetrical family. The family’s function has changed from that of a production unit, via the industrial society and household society to the family of today, characterised by equality, parity and reciprocity between the sexes.
Kindergarten policies, women’s growing participation in working life and the introduction of the paternal quota has meant that gender roles have changed and become more flexible. Men who start a family today must shape their own role as a father, and must achieve a balance between employment, childcare, housework and professional and leisure interests in line with women (4, 6, 7).
Becoming a parent is a major transition in life and entails a number of changes for both sexes (8), including psychological changes, a shift in life focus, new roles and an altered relationship with one’s partner (9–11). The purpose of pregnancy, maternity and post-natal care and the child health centre is to help the parents master and feel secure in the parental role (2).
Despite increasing involvement from fathers in caring for their own child, it is still mainly mothers who accompany their children for consultations at the child health centre (5, 12). Succeeding in making fathers more active and engaged will be best for the children and the family as well as being in line with national and political aims (2, 3).
Objective of the study
The objective of the study is to describe how first-time fathers experience their encounter with the healthcare services throughout pregnancy, childbirth and the child’s first three months of life.
The article focuses on the following research question: How do first-time fathers experience the encounter with the healthcare services (pregnancy and maternity care, the maternity ward and the child health centre) during pregnancy, during the birth and in the child’s first three months of life?
Method
The study has a qualitative design using interviews as a data collection method.
Sample
The informants constitute a strategic sample (13). Public health nurses recruited informants at four child health centres in a medium-sized municipality in Southeast Norway. The public health nurses presented the study to the fathers on home visits or at the six-week check-up. Altogether, 73 fathers with a new-born infant who met the inclusion criteria during the project period were invited in turn to participate in the study.
The inclusion criteria were as follows: they had to be first-time fathers and have a satisfactory command of Norwegian. The child’s age had to be around three months at the time of the interview.
We contacted the informants in turn after they had agreed to participate. We obtained informed consent and set a date for the interviews. We discontinued recruitment when no new factors emerged, i.e. when we reached data saturation (13) after conducting nine interviews.
The informants had a mean age of 30.7 years. They were all ethnic Norwegians with married or cohabiting civil status. Upper secondary school was the highest level of education for three of the fathers, while six had a university or university college education. On average, they had had a relationship with the child’s mother for five years prior to the birth. The child’s age was 15 weeks on average at the time of the interview.
All the informants had participated in one or more consultations with a midwife or public health nurse. Three of the fathers had participated in all types of consultation, i.e. home visits, six-week and three-month check-ups at the child health centre. All the fathers had been present at the birth.
Data collection and implementation
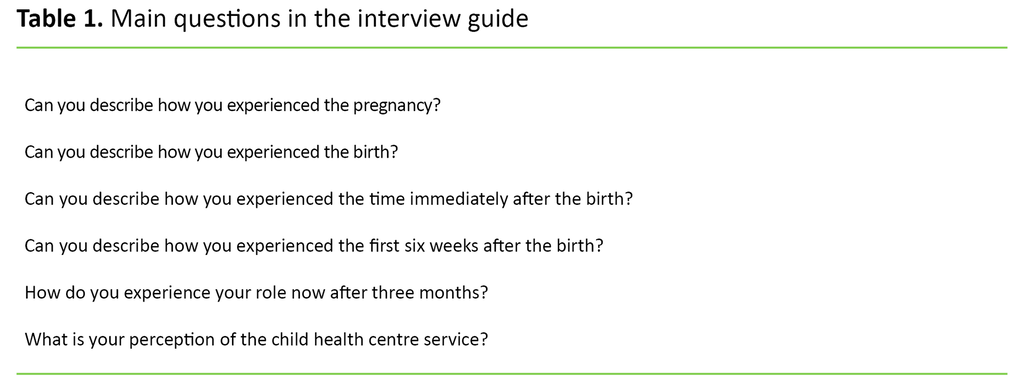
The first author conducted the interviews, which were based on a semi-structured interview guide consisting of altogether six open-ended main questions with more detailed follow-up questions (Table 1). All the main questions were based on the research question (14).
During the interviews, the informants spoke freely about the main questions. Consequently, we used few of the follow-up questions. All interviews included aspects relating to all the main questions.
We carried out a pilot interview to test the interview guide and to gain experience of using the interview method. This did not result in any changes to the guide. The main objective of the pilot interview was to test the interview guide, method and technique. Since the focus was more on process and improvement than on content, the pilot interview was not included in the study itself.
We carried out the interviews in the period from May to December 2016 and they lasted between 45 and 75 minutes. We conducted them in a neutral, private room: eight were carried out on the premises of the child health centre, and one at the informant’s workplace. The interviews were audiotaped.
We transcribed the interviews on an ongoing basis. After transcription, we reviewed the audiotapes and compared them again with the transcribed text to ensure quality.
Privacy protection and ethics
The informants received oral and written information about the study and its objective. All participation was voluntary. The informants gave written consent and had the opportunity to withdraw during the process. We anonymised the data and processed them confidentially. The authors did not take part in the recruitment nor did they know the informants from earlier. The Norwegian Centre for Research (NSD) approved the study (project number 47652), which was conducted in accordance with research ethics guidelines (15).
Analysis
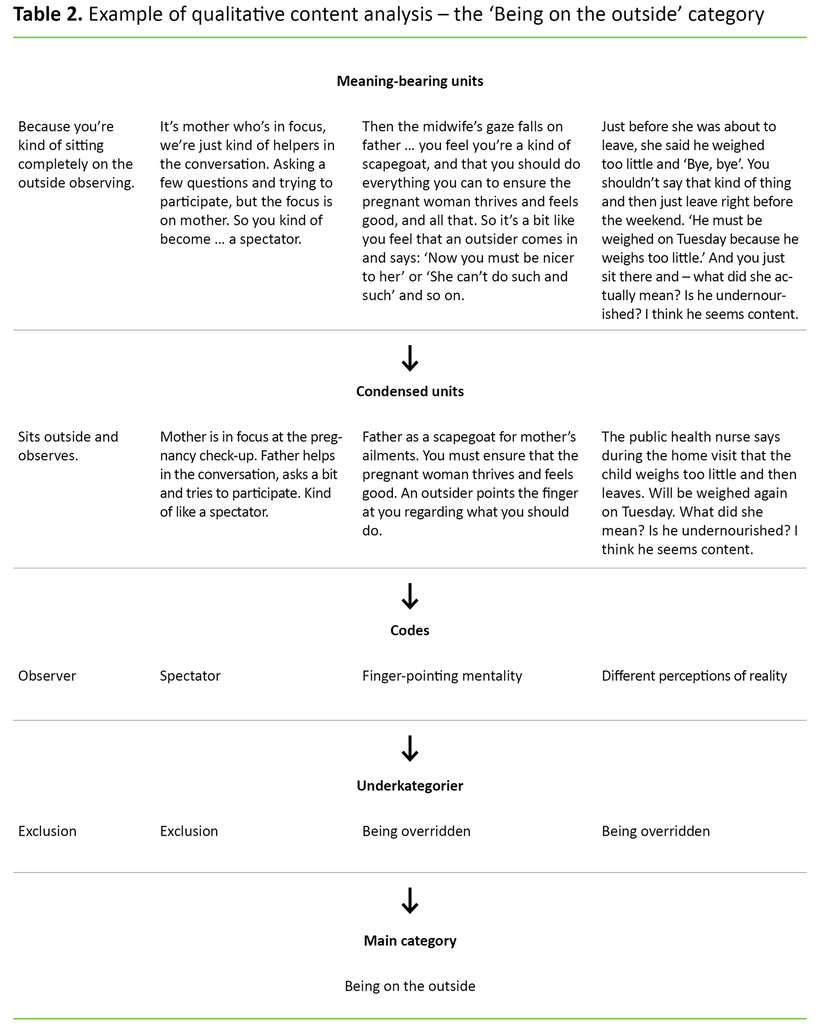
The analysis adheres to Graneheim and Lundman’s qualitative content analysis (16). The method is suited to analysing qualitative data with the purpose of describing informants’ perceptions. The analysis method encompasses the data material’s manifest and latent content, and employs an inductive approach. The manifest content consists of the informants’ direct statements. The latent content is what is said implicitly, allowing room for interpretation. The analysis is a five-step process. We first read all the interviews and identified meaning-bearing units, and then condensed and coded these. We sorted and assembled the codes in sub-categories and then categories (Table 2).
Results
Analysis of the interview data resulted in two main categories describing the fathers’ encounter with the healthcare services in pregnancy, during the birth and at the child health centre (here referred to as ‘meetings with professionals’): being on the outside and inclusion.
Being on the outside
The main category ‘being on the outside’ encompasses two sub-categories: ‘exclusion’ and ‘being overridden’.
Exclusion
In the encounter with all healthcare services, the fathers felt a sense of being on the outside, both in the mother–child relationship and in the mother–health personnel relationship. They often described themselves as only being physically present. They took part in consultations but did not feel that they were included:
‘It isn’t hostile to Dads, but the greatest focus is on mother and baby.’
‘They ask kind of in passing: “How’s Daddy doing?” They asked little ‘by the way’ questions but 80 to 90 per cent is devoted to the mother. We get a chair that’s placed behind her, and then we sit together.’
Mother and child are the focus of attention. The father felt himself to be the least important person during meetings with professionals. The fathers described their vulnerability in this setting. They wanted to be included but had no expectation of this, however:
‘The times I was there, they didn’t address me. But maybe that’s quite natural?’
The fathers described their role with words like ‘spectator’, ‘conversational helper’, ‘co-pilot’, ‘observer’, ‘helper’ and ‘supporter’. All of them expressed a wish and a need to be seen as having an independent role vis-à-vis the child:
‘It would be good if someone asked: “How are things?”
Nevertheless, the fathers felt that they had the opportunity to ask questions at health check-ups, and they were asked for their opinions. Their involvement in pregnancy care mostly concerned how the mother felt, and the child health centre’s attention was primarily addressed to the child. Few fathers experienced being asked about their own situation and feelings.
The fathers felt unprepared if they were asked direct questions and found it difficult both to answer and to ask questions in return. They also described feeling that they did not really believe that their opinions were important.
‘I was given the opportunity to ask questions but this was so sudden that I was almost unable to think of anything …’
The fathers found that the child health centre was not adapted for them and they felt it was unnatural to take the initiative to visit the centre on their own. They would attend consultations on their own if this was part of the established programme. Attending consultations was just as much about giving the mother support as for their own sake. They described the child health centre as a female-dominated society:
‘I’m there mostly as a support for Mum when she needs it. She asks me if I can come along when there are injections.’
The healthcare services are not a natural place to seek information. The internet was the main source of knowledge, then the mother and finally friends and family. All these came before the health services:
‘I feel that I can check this out later, find out myself.’
The feeling of being excluded was also reinforced by the services being poorly adapted to working fathers. Several fathers wanted more convenient opening hours, for example in the evening. The fathers wanted to be invited to participate in consultations and believed it was important that health personnel communicated that the father was welcome to participate.
The fathers were uncertain of their own role during home visits. Several experienced that the public health nurse was unclear about whether the father should participate or not. A couple of fathers chose to carry out other tasks in the house because they were unsure whether they should take part in the conversation or not.
Being overridden
Another factor in relation to being on the outside was the feeling of being overridden by the health personnel. Several fathers described having a bad conscience about not doing enough to help and support the women in the everyday situation. One father felt that he had been designated a ‘scapegoat’ in relation to the woman’s pregnancy problems.
The fathers described a certain degree of monitoring as to whether they did a good enough job. They described their vulnerability to remarks that they perceived as criticism. One father called this the health personnel’s ‘finger pointing mentality’, when someone from outside the family criticised his way of dealing with family members. This criticism created distance to the support system. Trust in the healthcare service was in general more dependent on relationships with individuals than with the system:
‘It doesn’t matter if they are highly skilled if they don’t have the personal qualities to build relationships.’
The fathers felt a sense of security if they had good chemistry with the health personnel and if the health personnel exhibited solid professional competence. They felt secure when they perceived that health personnel took their concerns seriously, and when their own understanding of the situation corresponded with that of the health personnel.
Inclusion
The main category ‘inclusion’ encompasses two sub-categories ‘participation’ and ‘adaptation’.
Participation
The fathers felt that specific, practical tasks, particularly in connection with childbirth, gave them a sense of involvement and security. Having responsibility for things such as cold compresses, food, drink, folding sheets and the like resulted in security in an unknown situation:
‘They saw us both the whole time during the birth. Were attentive and gave me tasks: “Now you can do that.” I felt that now I could do something. Finally!’
The fathers described some midwives as looking after them during the birth. They made provision for the father to play a practical role, and also stood out as clear and distinct.
‘I became midwife number two in a way.’
It was important that the fathers received information underway in the delivery process, particularly when unexpected incidents arose. The fathers described that they felt more included during the delivery itself than in the period before and after. Having the opportunity to be together with mother and child in the maternity ward, preferably in a family room, gave a feeling of inclusion:
‘It’s important that I’m not just a third person sitting there, but that they ask a bit about what we think. Otherwise I feel that there’s no point in being present.’
The degree to which fathers felt involved and were invited to participate in the conversations determined whether they participated in further consultations.
Adaptation
All the fathers described the meetings with professionals as generally positive despite experiencing being on the outside.
The fathers thought it was positive that check-ups had a good structure and a set programme. They wanted specific, clear information and direct answers. They specifically wished to be included more during pregnancy with a focus on their own role, independent of the mother’s role.
The fathers wanted their own role to be a subject of discussion. Several suggested separate consultations for fathers because they felt there was a need for such consultations, both during pregnancy and in the post-natal period. These consultations would deal with the father’s role, mental health and how best to support mother and child. Several fathers felt that some topics, such as mental health and daily challenges were difficult to talk about when their partner was present, and they thought they would get better support through individual conversations.
‘Call it a father-child session if you like, to get some tips and advice, or simply to ‘get it off your chest.’
Few of the fathers had experienced being asked directly about their own mental health. When the mother faced challenges, the fathers found it difficult to talk when the mother was present:
‘It’s challenging and difficult to broach topics related to this … what you feel.’
The fathers also wanted more Dad-friendly information on the internet, preferably under the auspices of the child health centre. Several of them described mothers’ networks on Facebook, for example, and wanted to see similar forums for fathers as well. However, no one would take the initiative to start such a group but described it as a ‘useful place to take a look’.
Several had been invited to take part in fathers’ groups at the child health centre and had considered this, but they were uncertain what it entailed, and therefore they had all declined the offer.
The fathers emphasised that inclusion in relation to healthcare personnel also requires the fathers themselves to take the initiative themselves:
‘We must maybe become better at making room for ourselves.’
An active father’s role means involving oneself as a father in the existing range of healthcare services.
Discussion
Father as a participant
The secondary role fathers described in their encounter with the healthcare services made it difficult for them to find their role in consultations, and led to uncertainty about the relevance of their own participation. In a study of first-time fathers, Premberg found that good, well-adapted information can reduce this kind of uncertainty. Participating in forums where one meets other fathers-to-be and can discuss the father’s role can lead to a sense of inclusion and empowerment. She also found that a lack of inclusion may maintain and strengthen the secondary role to some degree, create greater distance and complicate the transition to the father’s role (6).
The fathers had few expectations regarding the content of the consultations but later described their disappointment that their role had not been acknowledged. This disappointment is also described in other studies (6, 17, 18).
The fathers felt most included in the maternity ward. Here they received practical, specific and clear tasks, and the health personnel indicated that their presence was vital. Other research also describes similar findings (19). A positive experience of childbirth is crucial for a good start in the father’s role (6). There must therefore be some correlation between expectation and experience.
Preparations for childbirth mainly focus on the normal delivery process, and studies show that the fathers are not well prepared for any complications. Such incidents create more uncertainty and distance than if complications had been discussed in advance. This applies to Caesarean section deliveries in particular. The father is then often aware of the anticipated procedure regarding the mother but has little knowledge about his own role after the C-section (18).
The fathers were uncertain how often they were to participate in check-ups at the child health centre. They more often took part more to satisfy the mother’s need for support than to meet their own needs. The purpose of the home visit, for example, appeared unclear. Consequently, they often held back from participating. Public health nurses should therefore be clear about the purpose of the child health centres as early as the first contact with the family. The literature supports this finding, and consultations should involve both parents, who must be invited along as equal status service users (12).
New national professional guidelines also emphasise user participation, whereby service users’ experiences shall be used to improve and plan the activity (2). Fathers as a service user group can therefore constitute a relevant reference group in developing the range of services.
Changing and adapting practice
In the encounter with the healthcare services the fathers wanted there to be a change in focus, with greater emphasis on the father as a carer. National guidelines and political signals support the desire for more focus on the family, even though the amount of attention they call to the father’s role as an independent function varies (1–3). Few child health centres are practically adapted for working fathers. When fathers are involved to a greater degree, it will strengthen the opportunity to develop the father’s role, increase awareness of their independent function as carers and provide security in their role as fathers (7).
Many child health centres have attempted to boost fathers’ participation by means of fathers’ groups, family relations groups and theme days, for example. There is little documentation on participation and there has been no systematic evaluation of this type of measure (2, 7). Clear signals as to how to increase the father’s participation and involvement are also absent in national guidelines (2, 3). Some international studies stress that having dedicated discussion groups for men with male group leaders is positive (6, 20).
The fathers in this study were offered the opportunity to participate in a fathers’ group. They stressed uncertainty about the content as one of the reasons for their failure to participate. In this connection, the fathers themselves suggested that offering individual sessions, in the evening if possible, would be attractive. Groups might be of interest but their purpose would need clarification.
Service user studies from Bergen municipality show, however, that fathers prefer individual consultations (12). The fathers in this study described the healthcare services as a female-dominated society where they often felt like outsiders, and they were uncertain what the child health centres could offer them as a group. Here too, the healthcare services appear to be have been unclear in communicating their goals.
Previously, a political proposal was put forward on inviting fathers in particular to the eight-month check-up at the child health centre (21). The proposal has not been implemented, and inviting fathers to all check-ups should be a natural part of the child health centre’s programme.
It is a stated political goal to maintain the paternity quota. The aim is to pave the way for greater involvement of fathers during infancy and early childhood. Individual studies show that the paternity quota is a factor that increases the father’s involvement generally, not just in early childhood but also as the child grows older (22).
The role of health personnel
The fathers had difficulty distinguishing between the various professions and were often uncertain about the professional groups with which they had been in contact. Personal suitability and the ability to create good relationships with service users were more important for how fathers felt they were looked after than professional affiliation. A lack of clarity related to the role of health personnel and their competence may lead to uncertainty about what is expected of fathers in the various meetings with professionals. Clarification of this would help to create realistic expectations.
Fägerskiöl stresses that satisfaction with the health service is reflected in professionals’ ability to include the service users (20). How satisfied fathers are depends more on the individual health worker’s suitability than on the support system as a whole (24). Studies show that fathers have greater trust in the health personnel who take their concerns seriously. In general they have greater trust in female personnel, preferably with children of their own, than male personnel (20). These descriptions also concur with the descriptions given by the fathers in our study.
Despite the fathers’ descriptions of being on the outside, they were satisfied with the healthcare services for the most part. They felt that mother and child were well cared for, which meant that they were also satisfied. Here we can observe a certain degree of ambivalence between what they would like to see offered and how satisfied they were with the actual range of services. The fathers also said that they had to make more room for themselves, and be more proactive in order to ensure greater inclusion by the services.
Strengths and limitations of the study
The study has its limitations. The findings are based on a small number of informants, all with relatively similar backgrounds. The results are valid for this group and thus cannot be generalised. Nonetheless, the results will give a picture of the perceptions of a service user group and knowledge that may be transferrable to the healthcare services generally.
First-time fathers were specifically chosen as informants because they have no knowledge of the service beforehand and are therefore not influenced by earlier experiences. This gives them a more similar point of departure.
The use of an interview guide ensures an identical approach. Open-ended questions put emphasis on the informants’ own stories, and the findings are strengthened by the participants having first-hand knowledge of the subject. The interviewer was a public health nurse, which entails a degree of preconception (13) that may affect the interviews even though neutrality was sought.
The study is limited to first-time fathers and their perceptions of the encounter with the healthcare services in connection with pregnancy, childbirth and the child’s first months of life. We know that fathers’ attendance at the child health centre increases when paternity leave starts, and it may be a weakness that the study does not also cover this period.
Conclusion
The study describes a healthcare service related to pregnancy, childbirth and infancy that still focuses on mother and child, even though the objective is to have a family perspective. The fathers found that their inclusion in the healthcare services varied. They wanted to play a more active role and to be included during pregnancy, childbirth and follow-up at the child health centre. This requires a change of focus in the healthcare services, where greater emphasis is placed on fathers as independent and equal carers. Moreover, provision should be made for fathers to participate to a greater degree.
There is a need for further research on fathers’ participation in the encounter with the healthcare services. Different approaches to boost fathers’ participation should be assessed and evaluated, and national guidelines can include fathers to a greater degree. Research in this area should include fathers in different types of families, with a variety of orientations and cultural backgrounds in order to acquire an overall picture of the father’s role today in the encounter with the healthcare services.
References
1. St.meld. nr. 12 (2008–2009). En gledelig begivenhet. Om en sammenhengende svangerskaps-, fødsels- og barselomsorg. Oslo: Helse- og omsorgsdepartementet.
2. Helsedirektoratet. Nasjonal faglig retningslinje for det helsefremmende og forebyggende arbeidet i helsestasjon, skolehelsetjeneste og helsestasjon for ungdom. IS-2582. Oslo; 2017.
3. Helsedirektoratet. Nasjonal faglig retningslinje for barselomsorgen. Nytt liv og trygg barseltid for familien. Oslo; 2014.
4. St.meld. nr. 29 (2002–2003). Om familien – forpliktende samliv og foreldreskap. Oslo: Barne-, likestillings- og inkluderingsdepartementet.
5. Reform – ressurssenter for menn. Far gjør – perspektiver på menn og omsorg i Norge. Oslo: Reform; 2008. Available at: https://reform.no/wp-content/uploads/2017/04/2008-Far-gjoer.pdf(downloaded 20.08.2018).
6. Premberg Å. Förstagångsfäders upplevelser av föräldrautbildning, förlossning och första året som far. Gothenburg: Sahlgrenska akademin, institutionen för vårdvetenskap och hälsa, Universitetet i Göteborg; 2011.
7. Skjøthaug T. Fedres rolle i barnets tidlige utvikling. In: Holme H, Olavesen ES, Valla L, Hansen MB, eds. Helsestasjonstjenesten. Oslo: Gyldendal Akademisk; 2016. s. 35–97.
8. Brudal LF. Psykiske reaksjoner ved svangerskap, fødsel og barseltid. Bergen: Fagbokforlaget; 2000.
9. Condon JT, Boyce P, Corkindale CJ. The first-time fathers study: a prospective study of the mental health and wellbeing of men during the transition to parenthood. Australian and New Zealand Journal of Psychiatry. 2004;(38):56–64.
10. Moe V, Slinning K, Hansen MB. Håndbok i sped- og småbarns psykiske helse. Oslo: Gyldendal Akademisk; 2010.
11. Misvær N, Lagerløv P, ed. Håndbok for helsestasjoner 0–5 år. Oslo: Kommuneforlaget; 2013.
12. Bergen kommune. Rapport fra prosjektet: «Helsestasjon for hele familien». Bergen; 2009.
13. Malterud K. Kvalitative metoder i medisinsk forskning. 3.ed. Oslo: Universitetsforlaget; 2011.
14. Kvale S, Brinkmann S. Det kvalitative forskningsintervju. 3. ed. Oslo: Gyldendal Akademisk; 2015.
15. NESH. Forskningsetiske retningslinjer for samfunnsvitenskap, humaniora, juss og teknologi. Oslo: De nasjonale forskningsetiske komiteer; 2016.
16. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004;24:105–12.
17. Raphael-Leff J. Psychological processes of childbearing. 4. ed. London: Chapman and Hall; 2005.
18. Erlandsson K, Häiggström-Nordin E. Prenatal parental education from the perspective of fathers with experience as caregiver immediately following birth; a phenomenographic study. Journal of Perinatal Education. 2010;19(1):19–28.
19. Chin R, Daiches A, Hall P. A qualitative exploration of first-time fathers' experiences of becoming a father. Community Practitioner. 2011;84(7):19–23.
20. Fägerskiöld A. Support of fathers of infants by the child health nurse. Scandinavian Journal of Caring Sciences. 2006(20):79–85.
21. St.meld. nr. 8 (2008–2009): Om menn, mannsroller og likestilling. Oslo: Barne- og likestillingsdepartementet.
22. Rege M, Solli I. The impact of paternity leave on long-term father invovement. CESifo Working Paper Series nr. 3130; 2010.
23. Lindberg A, Hvatum I. Møtet med helsestasjonen – foreldre som aktive deltakere. In: Holme H, Valla L, Hansen MB, Olavesen ES, eds. Helsestasjonstjenesten. Oslo: Gyldendal Akademisk; 2016.
24. Carlson J, Edleson J, Kimball E. First-time fathers’ experiences of and desires for formal support: A multiple lens perspective. Fathering. 2014;12(3):242–61.










Comments