The home care services carry out extensive laboratory activity
A study shows that most home care services in Nordland, Sogn og Fjordane and Østfold counties perform a wide range of laboratory services.
Background: Little is known within the health service about the types of laboratory services that are performed for the roughly 145 000 Norwegian users of the home care services who receive home-based nursing care.
Purpose: To compile an overview of the laboratory activity carried out in the home care services in Nordland, Sogn og Fjordane and Østfold counties.
Method: Data was collected on laboratory activity in the home care services by sending out a web-based survey to 165 home care services units and 220 GP surgeries in the three counties in 2014. The response rate was 89 per cent and 84 per cent, respectively.
Results: A total of 95 per cent of the units perform laboratory services. Of these, 99 per cent analyse capillary samples, 96 per cent perform urine strip tests, and 89 per cent perform venous sampling. Of those units that take capillary samples, 99 per cent analyse glucose, 56 per cent C-reactive protein (CRP), 46 per cent haemoglobin, and 32 per cent analyse prothrombin time/international normalised ratio (PT/INR). It is the GPs who usually order venous sampling and capillary INR, glucose and haemoglobin, while the home care services often order urine strip tests and CRP tests. The GP surgeries think that they order a higher percentage of CRP tests than they actually do.
Conclusion: The home care services units conduct extensive laboratory activity with an analysis repertoire rather similar to that of nursing homes. Given the wide range of laboratory services performed by the home care services and the large number of employees involved in these activities, it is crucial to have quality assurance systems in combination with adequate professional expertise.
The home care services are a statutory primary healthcare service which seeks to ensure that residents have access to the necessary health and care services (1). The users of home care services comprise part of the GP’s patient list and must be given the same priority as other listed patients (2). About 145 000 users of home care services received home-based nursing care in 2015 (3).
Employees of the home care services also perform certain laboratory services, but there is little systematic knowledge about the extent and content of these types of services. For example, it is not known which point-of-care tests (POCT) are analysed in the user’s home. There is also reason to believe that the Coordination Reform (4), which calls for more patients to receive treatment in their homes, will increase the amount of laboratory activity carried out by the home care services.
There is relatively sound knowledge about what analyses are performed in the laboratory activity at GP surgeries and in nursing homes. For example, data from 2014 show that 95 per cent of nursing homes perform analyses of C-reactive protein (CRP) and urine strips, 98 per cent analyse glucose, 79 per cent analyse haemoglobin, and 40 per cent analyse prothrombin time/international normalised ratio (PT/INR) (5).
Laboratory services performed by the home care services
Alternatives to the home care services performing laboratory services are 1) that healthcare personnel (mobile laboratory personnel from hospitals or private laboratories or employees of GP surgeries) travel to the users, or 2) that the users are transported to the closest testing point (6).
The distance a user must travel to the closest testing point and the distance from the home care services to laboratories in nursing homes or GP surgeries can be significant for how the home care services units are organised and for which services are performed. For example, home care services co-located with nursing homes can improve cooperation on laboratory activity.
If the home care services offer laboratory services, the potential advantages are that the users avoid tiring journeys and get their test results more quickly. A potential disadvantage is that the quality of the laboratory services performed is not satisfactory due to inadequate expertise of the personnel.
Laboratory services, like other health services, have consequences for treatment and require resources. Thus, it is critical that these services are carried out properly and at the correct level. A survey of the extent and structure of the laboratory activity in the home care services is therefore important in order to assess how the organisation and quality assurance of such services can be optimised in the future.
Study of laboratory activity
In this article, we present the results of a study of laboratory activity in three Norwegian counties. The study was part of a pilot project in 2014–2015 conducted under the auspices of the organisation known as Norwegian Quality Improvement of Laboratory Examinations (Noklus). The study is included in the Care Plan 2015 (7) and is intended to comprise part of the basis for future recommendations on how laboratory activity in the home care services should be organised (8).
Noklus is a national, not-for-profit organisation that works to ensure that laboratory analyses are ordered, carried out and interpreted correctly in accordance with the patient’s need for examination, treatment and follow-up. Almost all GP surgeries and nursing homes in Norway are affiliated with Noklus. To the best of our knowledge, no other studies, national or international, have surveyed laboratory activity in the home care services.
However, some studies have investigated the competence of employees in the home care services. In a study of 1016 employees in nursing homes and the home care services, Bing-Jonsson et al. (9) found inadequate expertise in certain areas, such as nursing measures, advanced procedures and documentation. They also found a lower level of competence in the home care services than in nursing homes.
In a study of 209 employees in the home care services in six Norwegian municipalities, Bing-Jonsson and Tønnessen (10) found a need to increase competence in identifying symptoms of urinary tract infections and the use of urine strips.
Materials and method
We conducted the survey by sending out a web-based questionnaire to all home care services units in Nordland, Sogn og Fjordane and Østfold counties. We contacted a total of 165 units, of which 79 were located in Nordland, 46 in Sogn og Fjordane and 40 in Østfold.
The home care services units were identified from a list created by Statistics Norway. Then we quality assured the list by contacting the development centres for nursing homes and home care services (11) and by gathering information from the websites of the individual municipalities.
Various terms such as zones, main facilities and wards are used about the units in the various municipalities. We therefore decided in the questionnaire to define a ‘home care services unit’ as the physical space where the employees are co-located. Thereafter we use the term ‘unit’.
Preparation of the questionnaire
We prepared the questionnaire in consultation with employees of Noklus and Noklus’ advisory group for the home care services. A revised version was circulated for review to two or three different units in each of the three counties.
In spring 2014, we sent out a final version of the questionnaire with a three-week response deadline. We attached a letter from the Norwegian Director of Health encouraging the units to respond to the questionnaire. A reminder was emailed two weeks after the questionnaire was sent out initially, and in the final week we phoned those who had not responded.
We asked about organisation of the services, the analytical repertoire and cooperation with GP surgeries and nursing homes. To assess the appropriateness of a given form of organisation, we asked about 1) the users’ travel time to the closest GP surgery and 2) the travel time from the units to the closest GP surgery and nursing home.
Response to the questionnaire
Altogether, 146 of a total of 165 units (89 per cent response rate) responded to the questionnaire, of which 70 were from Nordland, 40 from Sogn og Fjordane and 36 from Østfold. We registered responses from units in all municipalities in the three counties.
The alternative travel times in the questionnaire were as follows: 0 (co-located), 1–5, 6–15, 16–30, 30–60, 60–120 and more than 120. Few respondents reported a travel time of more than 30 minutes, and three of the categories were therefore consolidated into the category ‘> 30 minutes’.
Some of the respondents failed to answer all the questions, and therefore the response rates vary. We used chi-square tests to test differences between the counties. We used Microsoft Excel for the analyses.
At the same time as we sent out the questionnaire to the home care services, we sent out the questionnaire to all GP surgeries in the counties. We asked about the type and degree of cooperation with the home care services on laboratory activity. GPs in the three counties reviewed the questionnaire in advance. Then we sent it to 220 GP surgeries. This resulted in a response rate of 83.6 per cent.
To avoid having too many tables in the results section, we decided to report some of our results in written form only. We also chose not to present the percentages with decimals due to the relatively low number of observations.
Results
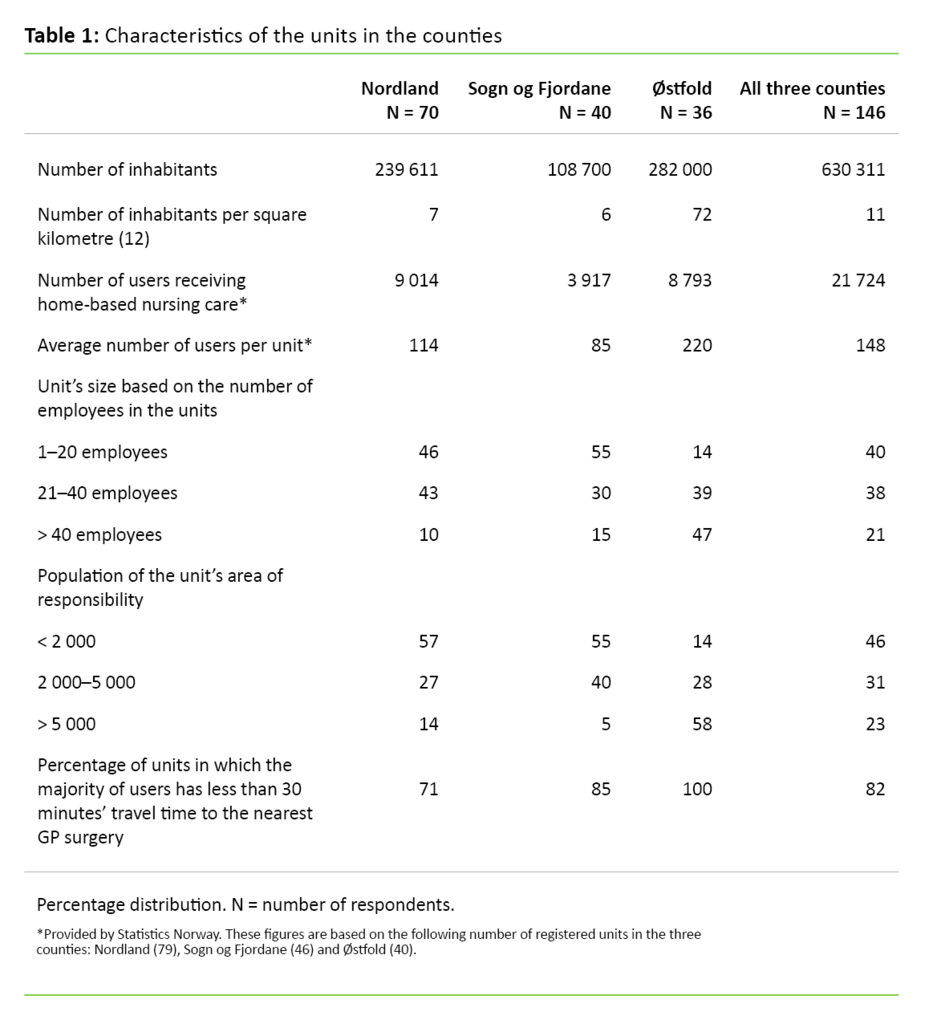
Table 1, characteristics of the units in the counties, shows that Sogn og Fjordane county has far fewer users who receive home-based nursing care than Nordland and Østfold counties. Each unit in Østfold county has almost three times as many users as the units in Sogn og Fjordane county and nearly twice as many as the units in Nordland county.
Eighty-two per cent of the units stated that the travel time to the nearest GP surgery was less than 30 minutes for most of their users. This percentage is highest for Østfold county (100 per cent).
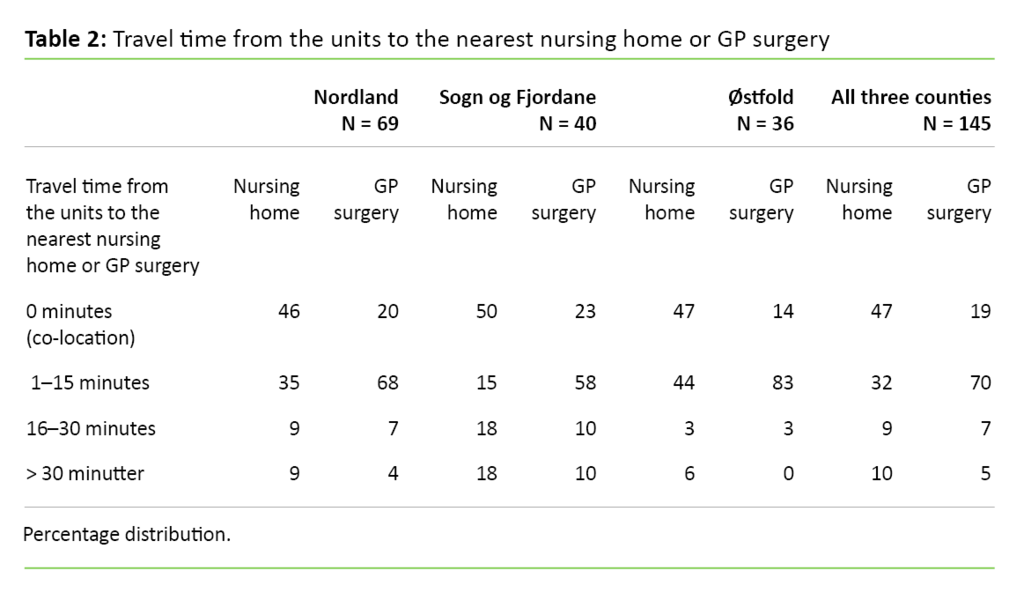
Table 2 shows the travel time from the units to the nearest nursing home and the nearest GP surgery, measured in minutes. Altogether, 47 per cent of the home care services units were co-located with a nursing home, while 19 per cent were co-located with a GP surgery (Table 2).
The percentage of units co-located with a nursing home was rather evenly distributed among the counties, while Østfold county had the lowest percentage of units co-located with a GP surgery. However, Table 2 shows that Østfold county has the shortest travel time, both to the nearest nursing home and to the nearest GP surgery.
The units were asked to respond ‘yes’ or ‘no’ to the question of whether they perform sampling and/or analysis of blood or urine. Henceforth, those units that responded ‘yes’ to this question are considered to conduct laboratory activity, and the subsequent tables contain data from this group only.
A total of 139 of these units responded ‘yes’ (95 per cent) to this question – 96 per cent in Nordland, 98 per cent in Sogn og Fjordane and 92 per cent in Østfold. The units were also asked to state whether they perform venous sampling. The percentage of units that performed venous sampling was high for Nordland (97 per cent) and Sogn og Fjordane (92 per cent) and significantly lower (p-value < 0.05) for Østfold (69 per cent).
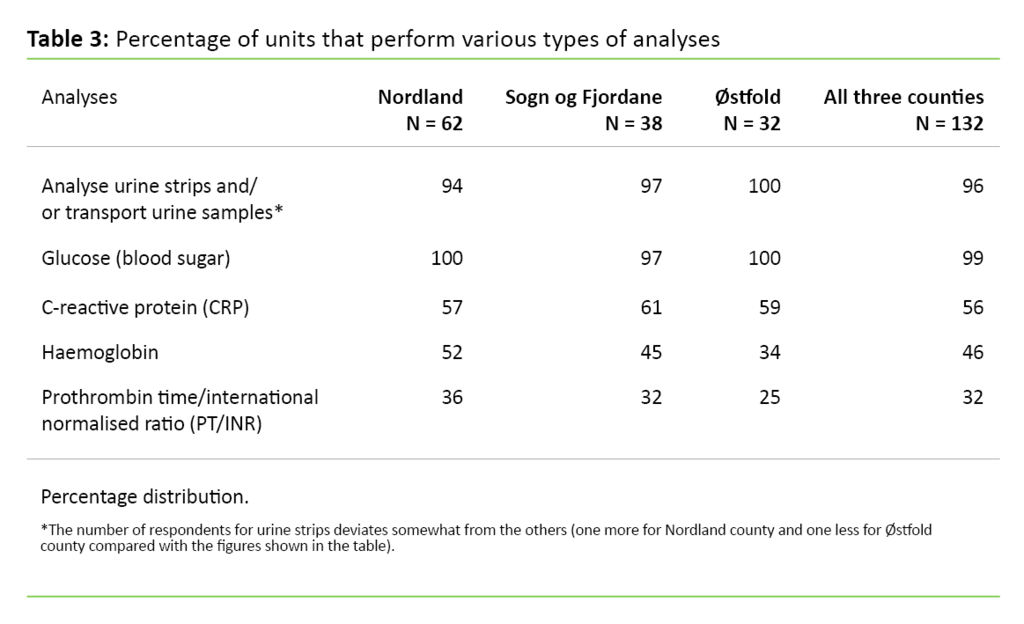
Table 3 shows that almost all the units take capillary samples and analyse urine strips and/or transport urine samples. Glucose is analysed most frequently (96 per cent); about half of the units analyse CRP (56 per cent) and haemoglobin (46 per cent), while one-third analyse PT/INR (32 per cent). No units stated that they conducted other analyses than those mentioned above.
All types of employees perform glucose measurements and urine strip tests, and transport urine samples, while nurses are by far the most important group regarding venous sampling. In our study, 99 per cent of the units state that nurses perform venous sampling, while the corresponding figure for auxiliary nurses (health workers), social educators and unskilled personnel is 14 per cent, 11 per cent and 4 per cent, respectively.
Twenty-eight per cent of the units also performed analyses at night. In this regard, there was a relatively large variation between the counties: Nordland 22 per cent, Sogn og Fjordane 15 per cent and Østfold 55 per cent.
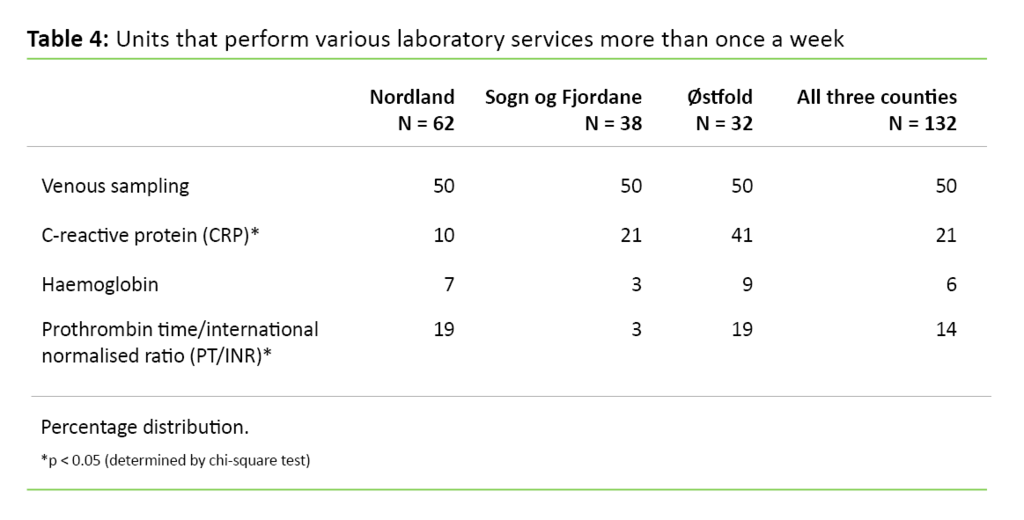
Table 4 shows that half the units in all the counties perform venous sampling more than once a week, while the percentages are much lower and vary for the remaining three types of analysis; between 6 and 21 per cent. The percentage that analysed CRP differs significantly between the counties.
In addition, Table 4 shows that the percentage of units that analysed CRP more than once a week is highest for Østfold county. The percentage that performed PT/INR more than once a week is significantly lower in Sogn og Fjordane county.
The units were also asked which types of analyses they performed. Almost 46 per cent of the units conducted at least four of the five analyses we asked about: glucose, CRP, haemoglobin, PT/INR and urine strip testing. One-quarter of the units performed all five.
The respondents stated that glucose, PT/INR and haemoglobin were usually analysed in the home of the user. CRP was analysed both in the user’s home and at the unit’s main facility. Urine strip testing was performed most often in the patient’s home, then at the unit’s main facility and then at the GP surgery.
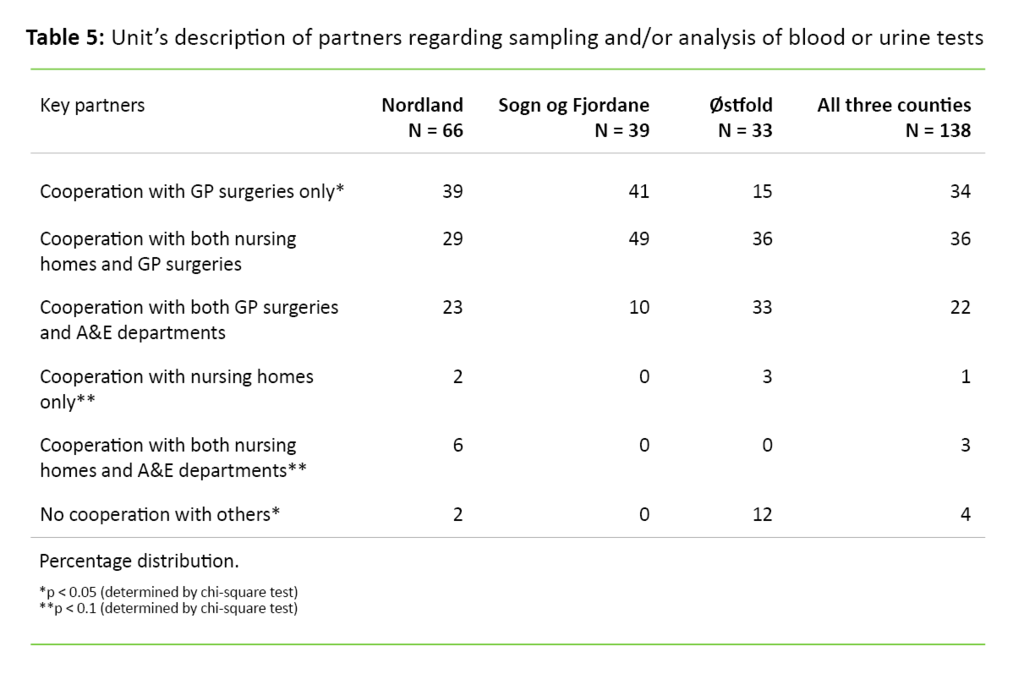
Table 5 shows that GP surgeries are the units’ most important partners. Sogn og Fjordane county, and Nordland county to some extent, cooperated for the most part solely with GP surgeries or with GP surgeries and nursing homes. Østfold county had the highest percentage of units which stated that they cooperate with both GP surgeries and A&E departments.
The units stated that they often chose to order specific services based solely on their own experience: 44 per cent said that they almost always order urine samples on this basis, and 31 per cent said that they often order urine samples for CRP. This occurred far less often for venous sampling, haemoglobin and PT/INR. Except for urine samples, in which Nordland county has a higher percentage than the other counties, there were no significant variations among the counties.
When we compared our findings for the units and GP surgeries regarding requisitions, we found that the GP surgeries thought that they ordered a higher percentage of all CRP tests than was actually the case. We also found that 54 per cent of the units almost always, based on the test results, assessed whether it was necessary to contact a doctor, while only 23 per cent of the GP surgeries believed that the units did this.
Altogether, 117 of 135 units stated that they ‘almost always’ entered the test results in a journal, while 7 units stated that they ‘did this in more than half the cases’. Only 7 per cent of the GP surgeries reported having signed a written agreement with the home care services on the type and extent of cooperation.
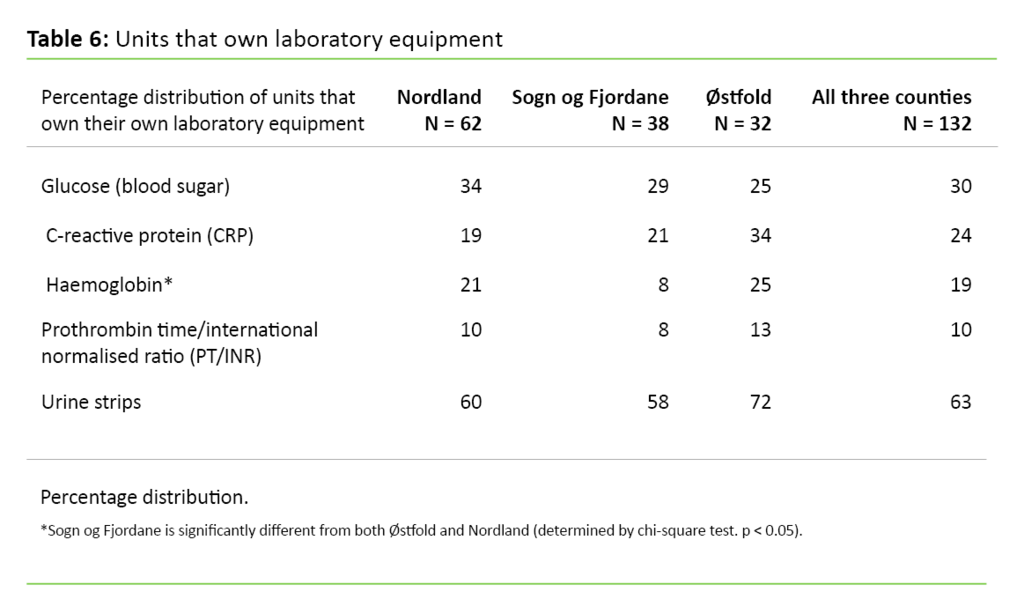
Table 6 shows that 63 per cent of the units used their own urine strips, while the percentage of units that owned their own equipment for measuring glucose, CRP, haemoglobin and PT/INR was lower – between 10 and 30 per cent. Moreover, the table shows that the units in Østfold county generally owned more equipment than the units in Nordland and Sogn og Fjordane counties.
Discussion
It is surprising that more than 95 per cent of the home care services units in Nordland, Sogn og Fjordane and Østfold counties conduct laboratory activity and that a large percentage of them perform many different types of laboratory services. All the units perform capillary sampling and analysis in the user’s home, while 90 per cent of the units in Nordland and Sogn og Fjordane counties perform venous sampling. The percentage is somewhat lower in Østfold county. A disadvantage of performing analyses in a location other than the patient’s home is that the test results are received at a later time.
Analytical repertoire
There are no significant differences between the counties regarding analysis repertoire. This finding is rather surprising in light of the variation between counties in terms of travel distance.
When we processed the results, we did not account for the variation in the units’ size and travel distances (Tables 1 and 2). Since the users in Østfold county have the shortest travel distance to alternative laboratories where samples are taken, such as the A&E department, we anticipated a narrower analysis repertoire for this county. One possible explanation is that Østfold county has larger units with more users and employee full-time equivalents, and therefore has a greater need for easily accessible laboratory equipment.
Another interesting observation was that the units’ analysis repertoire corresponded somewhat with the repertoire of Norwegian nursing homes (5). The percentage of nursing homes and units that performed urine strip tests, glucose and PT/INR was relatively equal, while it varied for haemoglobin and CRP: 79 and 95 per cent for nursing homes, and 45 and 56 per cent for the units respectively.
Cooperation with GP surgeries and A&E departments
We also found that the units in Østfold county cooperated more with A&E departments and less with GP surgeries than the two other counties. This is probably because the users in Østfold county have a shorter travel distance to alternative laboratories. When we compared the lists of the analysis repertoire and the percentage of equipment owned by the home care services, we found that 42 per cent of the units that perform CRP analysis own the instruments themselves.
The percentage was highest for Østfold county, which could be because Østfold county has larger units and therefore a greater need for easily accessible laboratory equipment. A previous study found that increased accessibility of an analysis instrument at the GP surgery resulted in more frequent use of the relevant analysis (13). This finding confirms that accessibility of the analysis equipment alone affects the frequency of analysis.
The units carry out more laboratory activity than the GP surgeries are aware of, which may be because not all the test results are reported to GP surgeries.
The failure of units to report test results and record information in patient journals may be due to an absence of written agreements that clarify the tasks of the home care services. In addition, Bing-Jonsson et al. have confirmed that there is a lack of documentation activity in the home care services (9).
Representative sample for the three counties
With a response rate of 89 and 84 per cent from the home care services units and the GP surgeries respectively, there is reason to believe that the respondents are representative of the three sample counties. It is likely that our findings also provide relevant information about the situation in other counties. However, this study does not include any of Norway’s five largest cities, which means that we must be cautious when generalising.
In densely populated areas, for example, it is much easier to dispatch healthcare personnel to the users in order to perform planned analyses, while at the same time the user’s travel time and distance to the closest GP surgery is shorter. Any future expansions of our project should include more counties and larger cities. Studies may be carried out both to include more counties and to choose other units of observation, e.g. to distinguish between large and small units.
There is also some difference between the units as to who responded to the questionnaire. In Sogn og Fjordane county, 82 per cent of the respondents were heads of units, while this percentage was somewhat lower in the other two counties. Such differences could have impacted on our findings.
In our study, we do not know the number of samples that were analysed in the individual units and by the individual employees. We decided not to ask about such conditions since we thought it was unlikely to find respondents who had such an overview. Instead we asked about the number of tests the units had available and whether the units analyse the samples more than once a week.
It is likely that the individual employee in the home care services carries out laboratory activity less often than employees in GP surgeries, and just as seldom as employees in nursing homes. Therefore, it is especially important to have good training and quality assurance systems.
Conclusion
Our study shows that most of the units conduct laboratory activity and that this activity is relatively extensive and more extensive than the GP surgeries are aware of. This means that there are many employees in the home care services who, in one way or another, are involved in laboratory activity.
The units have multiple partners that they must engage with. It is therefore crucial that those involved in laboratory activity have adequate professional expertise, while at the same time they develop tailored quality assurance systems to ensure that cooperation between the GP surgery, nursing home and home care services is satisfactory.
Nurses carry out a considerable amount of laboratory activity. Therefore, an important measure to ensure that nurses have adequate expertise could be to include laboratory activity in their basic nursing education.
We wish to thank the laboratory advisor and project coordinator Marit Steinsund in Noklus for data collection and helpful suggestions during the preparation of this article.
References
1. Lov 24. juni 2011 nr. 30 om kommunale helse- og omsorgstjenester m.m. (helse- og omsorgstjenesteloven) § 3.1–3.2. Available at: https://lovdata.no/dokument/NL/lov/2011-06-24-30(downloaded 08.01.2018).
2. Forskrift 28. august 2012 nr. 842 om fastlegeordning i kommunene. Available at: https://lovdata.no/dokument/SF/forskrift/2012-08-29-842?q=Forskrift om fastlegeordning i kommunene(downloaded 08.01.2018).
3. Statistisk sentralbyrå. Omsorgstenester. 2017. Available at: https://www.ssb.no/helse/statistikker/pleie(downloaded 13.02.2017).
4. St.meld. nr. 47 (2008–2009). Samhandlingsreformen. Rett behandling– på rett sted – til rett tid. Oslo: Helse- og omsorgsdepartementet; 2009.
5. Laboratorietilbud i sykehjem; Veileder for utvidelse og vurdering av laboratorietilbud i sykehjem. Available at: http://www.noklus.no/Portals/2/Kurs%20og%20veiledning/R%E5d%20om%20analyserepertoar/2014-10-21%20Laboratorietilbud%20i%20sykehjem%20med%20dato%20-%20Veileder%20fra%20Noklus.pdf(downloaded 19.10.2016).
6. Helserådet. Skal hjemmesykepleien ta blodprøver. 2013;2:6–7. Helsebiblioteket.no. Available at: http://www.helsebiblioteket.no/samfunnsmedisin-og-folkehelse/helseradet/?index=100(downloaded 19.10.2016).
7. Omsorg 2020. Regjeringens plan for omsorgsfeltet 2015–2020. Oslo: Helse- og omsorgsdepartementet. Available at: https://www.regjeringen.no/contentassets/af2a24858c8340edaf78a77e2fbe9cb7/omsorg_2020.pdf(downloaded 15.02.2017).
8. Fauli S. Hvilken laboratorievirksomhet bør hjemmetjenesten ha? Tidsskr Nor Legeforen 2014;134:487.
9. Bing-Jonsson PC, Hofoss D, Kirkevold M, Bjørk IT, Foss C. Sufficient competence in community elderly care? Results from a competence measurement of nursing staff. BMC Nursing 2016;15:5.
10. Bing-Jonsson PC, Tønnessen S. Urinveisinfeksjon blant eldre i hjemmesykepleien. Sykepleien Forskning. Available at: https://sykepleien.no/forskning/2016/11/urinveisinfeksjon-blant-eldre-pasienter-i-hjemmesykepleien(downloaded 08.01.2018).
11. Senter for fagutvikling og forskning, Utviklingssenter for sykehjem og hjemmetjenester i Oslo. Available at: http://www.utviklingssenter.no/index.php?cat=176135(downloaded 17.01.2018).
12. Statistisk sentralbyrå. Folkemengde og areal, etter fylke og kommune. Available at: http://www.ssb.no/a/aarbok/tab/tab-057.html(downloaded 17.01.2018).
13. Fauli S, Thue G. Decision making in general practice: the availability and use of a specific laboratory analysis. International Journal of Technology Assessment in Health Care. 2005;21(3):386–92.










Comments