Do the scales at child health clinics show the correct weight?
Weight measurement provides an indication of the well-being, nutrition and health of children and adolescents. It is therefore important that the scale that is used provides precise measurements.
Background: Weight measurement is a basic indicator of child and adolescent well-being, nutrition and health. For a public health nurse to take the appropriate action based on a child's weight, it is essential that the scales used are accurate.
Objective: To find out whether the scales at child health clinics measure correct weight, if there are differences in accuracy between medically approved and non-medically approved scales, and if current control routines correspond with evidence-based recommendations.
Method: Clinical auditing was used for mapping the scales and the routines at 27 child health clinics. In total 152 scales were tested: 102 baby scales and 50 flat scales.
Results: 16 of 152 scales showed a 100 per cent correct weight in all tests. 82 of the scales were medically approved and these were significantly more accurate than those scales which were not medically approved. Three of 27 child health clinics had good procedures where the baby scales were tested according to set criteria. None of the child health clinics had procedures for testing flat scales.
Conclusion: The audit shows that few scales are 100 per cent accurate and that there is a discrepancy between practice and evidence-based recommendations. Ensuring strict controls and introducing a standard to mandate the use of medically approved scales at all child health clinics will result in more accurate data collection in public health nursing services.
Weight measurement is one of the basic indicators of child and adolescent well-being, nutrition and health. Norwegian authorities follow the World Health Organization (WHO)’s recommendations for close follow-up of a child's weight. The authorities’ main goal with weighing and measuring by child health clinics and school health services is to help identify children and adolescents with weight deviations at an early point in time. Another goal is to reduce the negative consequences that deviant weight can have for the individual child (1).
Measuring weight is an important part of the work of a public health nurse, whose duties are guided by a preventive and health promotion perspective. Measuring weight is a primary preventive action whereby all children are routinely weighed from birth to adolescence (2). In order to enable public health nurses to implement appropriate actions, it is essential that the scales that are used provide precise measurements. Earlier studies show that many scales used to measure body weight are imprecise (3, 4). Among other things, inaccurate scales can yield Body Mass Index values (BMIs) that can result in an incorrect assessment of a child's weight status (5, 6).
Recommended tests
To ensure accurate measurements, the national professional guidelines for weighing and measuring by the child health clinic and school health services recommend that scales be tested twice annually, and more often if they are moved around (1). No specifics are given for how the scales are to be tested, nor are there any requirements to use medically approved scales. According to Júlíusson et al. (7) it is important to test a scale with the weight the scale is meant to measure, i.e. baby scales should be tested with weights corresponding to the weight of children under the age of two. Flat scales at child health clinics should be tested with weights corresponding to the weight of children over the age of two.
The tests should be performed with certified weights to ensure accurate measurements (4). Placement of the scale, the surface underneath and type of scale are also significant (3). Norway has a requirement to use medically approved scales for monitoring, diagnosing and medical treatment in medical practice (8). Public health nurses perform health monitoring by following the growth development of the child and adolescent population, which can provide a good basis for preparing targeted preventive measures and evaluating the local and national effect of the measures (1).
Measuring weight is a primary preventive action whereby all children are routinely weighed from birth to adolescence.
Evaluating the extent to which the child health clinics follow evidence-based recommendations necessitates a survey of actual practice compared with what is standard. In this way, any need for improvements can be discovered (9).
Survey current practice
Clinical audits set criteria and standards for surveying practice. The purpose of this audit was to ascertain whether the scales used at child health clinics and during home visits to newborns measure correctly. We also wanted to map whether current practice is consistent with evidence-based recommendations (1). According to the National Strategy for Quality Improvement in Social and Health Services, a prerequisite for good quality is the probability of reducing errors to a minimum (11). The following questions were the starting point for undertaking a clinical audit:
- Do the scales used at the child health clinics and during home visits measure the correct weight?
- Are there differences in accuracy between medically approved and non-medically approved scales?
- Do the child health clinics follow the recommendations for testing scales a minimum of twice a year with a weight the scale is meant to measure?
Methodology
In the period January to May 2015 we carried out a clinical audit of baby and flat scales used at child health clinics and during home visits.
Criteria and standards
Clinical auditing is a method for systematic evaluation and quality improvement consisting of five steps. First, the area of improvement must be identified, after which criteria and standards are set. Practice is surveyed before practice is compared with criteria and standards. Finally, measures are implemented, and new surveying can be carried out. Criteria are set based on best practice, and shall be predicated on evidence-based recommendations (10).
A standard must be defined if criteria are to be useful. A standard describes the quality level of what one desires to achieve, and is presented as a percentage (12). The criteria set for our project prescribed that baby and flat scales used at child health clinics and during home visits must show the correct weight. They shall also be tested a minimum of twice a year with a weight the scale is meant to measure. To gain an overview of how many of the scales are accurate, we set an ideal standard of 100 per cent correct weight.
Preparation and execution
The reference standard that was used was certified weights loaned by the Outpatient Obesity Clinic at Haukeland University Hospital (HUS) and Teck-Ho Service. The weights were calibrated in advance at Kiwa Teknologisk Institutt. We tested stationary baby scales, portable baby scales for use during home visits, and stationary flat scales. The weights represented the weights the scales were meant to measure. Baby scales are used to weigh children from birth to age two, and these were tested with 2 kg, 5 kg, 7 kg, 10 kg and 15 kg weights. Flat scales used at child health clinics weigh children from age two until they start school. These scales were tested with 10 kg, 15 kg, 20 kg, 30 kg and 40 kg weights. In advance, we received an introduction to and briefing on the calibration of scales at Kiwa Teknologisk Institutt.
The tests should be performed with certified weights to ensure accurate measurements.
We performed all of the tests at the child health clinics on a flat, hard and stable surface, such as a suitable table, or on the floor. In order to check that the scales measured correctly, we tested the scales’ accuracy, repeatability and stability. We measured accuracy by placing certified weights on the scale. We tested repeatability by repeating the procedure three times. Stability was checked by performing the corner test on the scales. This was done by placing a 10 kg weight on the various points (the middle and all four corners) of the scale. The scales were re-set to zero between each test. We recorded the results of the measurements, information about the scales and the control routines at the child health clinic.
Collection of data
Data were collected from March to May 2015. We included one large city municipality and four rural municipalities in the same hospital trust, with altogether 27 child health clinics. Because midwives from the “Midwife Home Visitor” service at the hospital visit the homes in the city municipality during the first week of a child’s life, we also tested five of their baby scales. The hospital requires the scales to be medically approved and has routines for testing them. In all, we tested 152 scales, of which 102 were baby scales and 50 were flat scales. Prior to collection of the data, we informed senior public health nurses at the various child health clinics about the study by e-mail, and we received approval to come to the clinics at agreed times. We asked the available public health nurse about the control routines at the child health clinic.
Data analysis
We analysed data with the aid of SPSS 22. Coding and entry of data were quality assured by a duplicating check. We used descriptive statistics and average deviation to evaluate the accuracy and average standard deviation per scale to assess repeatability. The chi-square test was performed to examine differences between accuracy on medically approved and non-medically approved scales. The level of significance was set at p <0.05 (13).
Results
Accuracy, repeatability and stability
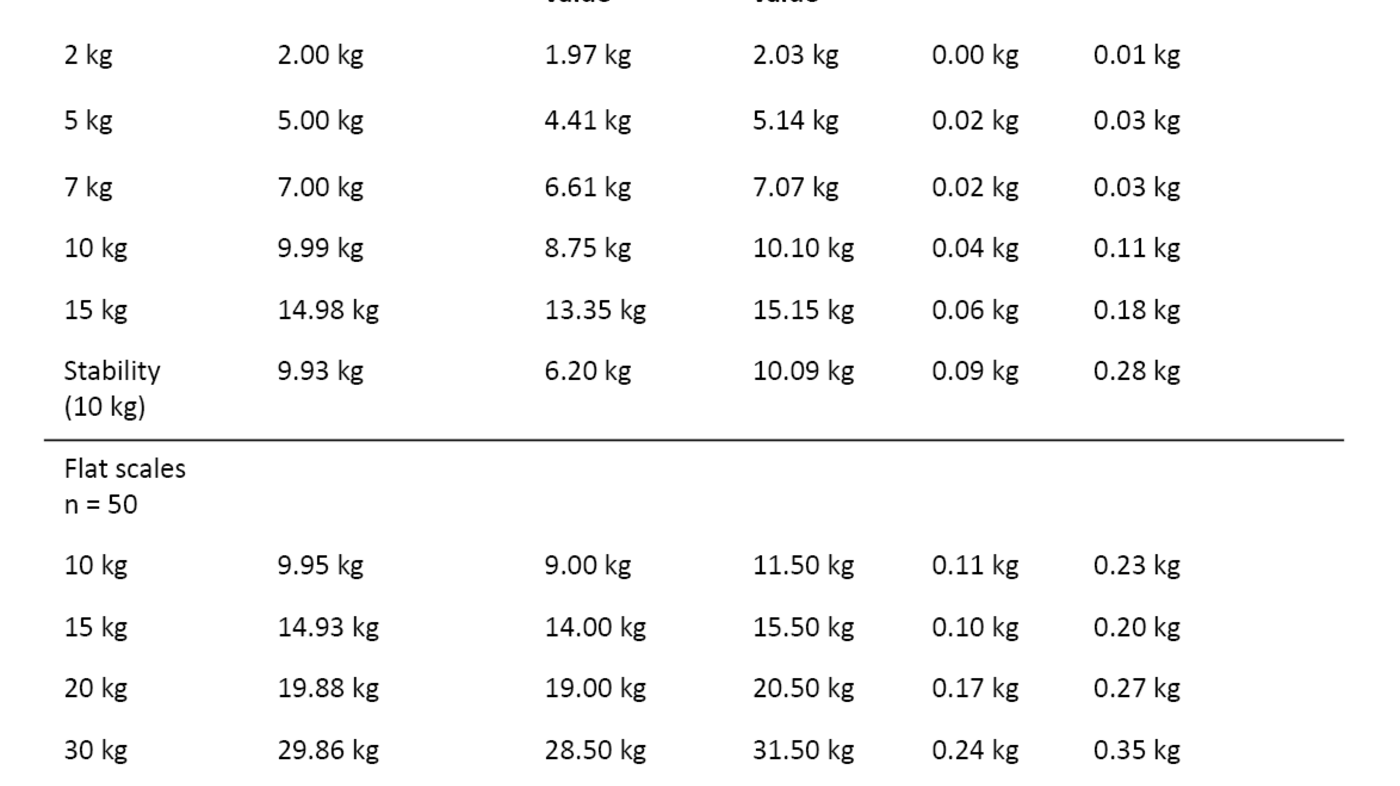
Of 152 scales, 16 showed 100 per cent correct weight during all control measurements; of these nine were baby scales (n = 102) and seven were flat scales (n = 50). The baby scales that were not correct had deviations ranging from 0.01 kg to 1.65 kg, while the deviations on the flat scales varied from 0.05 kg to 2.00 kg. Accuracy and repeatability declined with increasing weight (Table 1). Scales with stability deviations also had accuracy and repeatability deviations.
Medically approved and non-medically approved scales
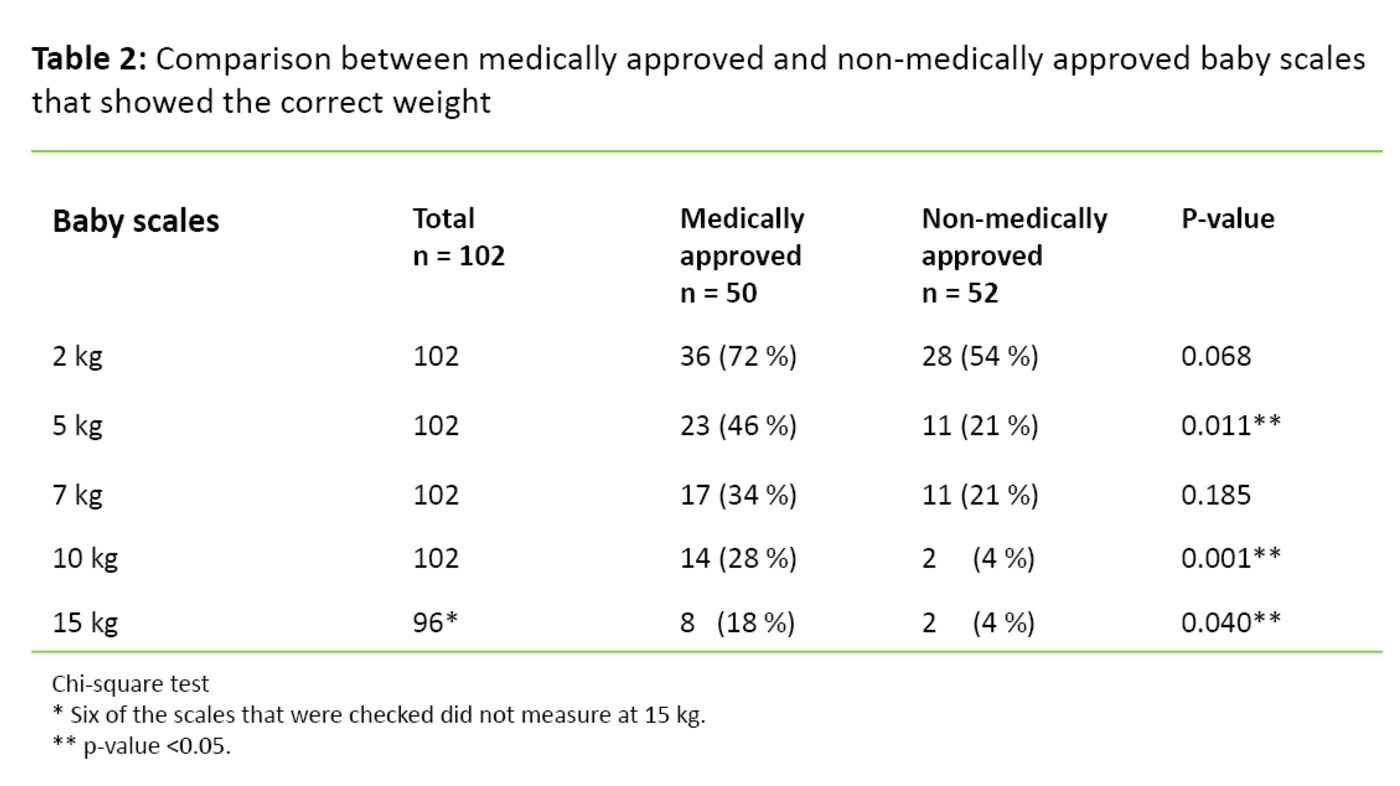
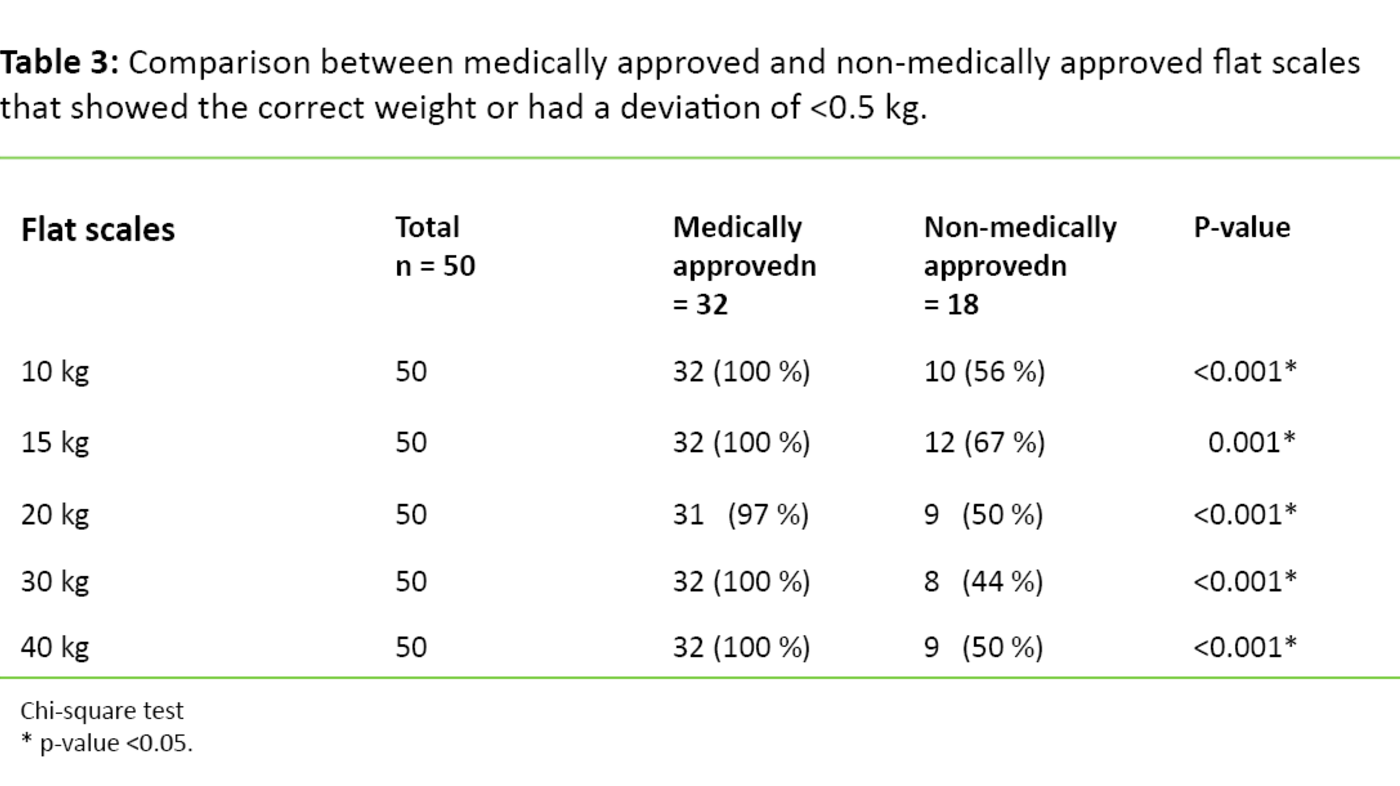
Eighty-two of the scales were medically approved, of which 50 were baby scales (n = 102) and 32 were flat scales (n = 50). All of the stationary baby scales were medically approved. Many of the portable baby scales used during home visits were non-medically approved. The medically approved scales were significantly more accurate during most measurements than the non-medically approved scales (Table 2 and Table 3). Half of the non-medically approved flat scales had a deviation of 0.5 kg or more, while only one of the medically approved flat scales had a deviation of 0.5 kg (Table 3). The medically approved scales also did better with regard to repeatability and stability.
Control routines
Three of 27 child health clinics had good routines in accordance with the recommendations, where the baby scales were tested a minimum of twice a year with a 5 kg weight. The “Midwife Home Visitor” service also had good routines, where the scales were regularly checked when serviced. Five child health clinics had routines where they regularly tested the baby scales with weights under 5 kg. For instance, they used weights of 0.5 to 1 kg, toys, large liquid soap containers, loose-leaf binders and packages of butter. The other child health clinics had no regular control routines for baby scales, and none of the child health clinics had routines for testing flat scales. The child health clinics that had good routines and the “Midwife Home Visitor” service had more accurate scales than the child health clinics that had no routines, or had routines where they tested the scales with weights under 5 kg.
Discussion
Our results showed that even though many scales are highly accurate, a scale that is not tested can in principle show any reading. Only 16 of 152 scales showed 100 per cent correct weight. Schlegel-Pratt and Heizer (4) believe that established standards are important for accurate scales. It is conceivable that a standard of 100 per cent correct weight is somewhat strict, but it is difficult to judge acceptable deviations. Two different scales used at the same child health clinic can be imprecise in either direction, and can thus yield a wider discrepancy. This can result in weight loss at one visit and weight gain at another visit, and vice versa. Such weight variations can potentially affect decisions with respect to interventions. A deviation of only 20 grams on a baby scale can produce a discrepancy of 40 grams, and the larger the deviation, the greater the potential consequences.
Consequences for practice
It is very important to assess weight development during the neonatal period because weight reflects nutrition and well-being. Difficulty with breastfeeding is the main reason for large weight loss after birth (14). In newborns, a 10 per cent weight loss limit has been established for implementing interventions (1). We saw scales used for home visits that showed up to 590 grams too little at 5 kg (Table 1), a deviation of more than 10 per cent. It is conceivable that inaccurate scales can trigger interventions on a completely erroneous basis. Such instances require public health nurses to invest time and resources and can also have negative consequences for the family concerned. For example, already well-established breastfeeding may be disrupted if the mother loses confidence in her ability to breastfeed.
A scale that is not tested can in principle show any reading.
We also saw scales that showed up to 140 grams too much at 5 kg (Table 1). Such a deviation can cause serious consequences in cases where a mother is assured that her newborn has gained the normal amount of weight, when in reality this may not be the case. Collection of reliable weight measurements is usually not an isolated act, but must be viewed in the context of an overall assessment of the child (15). The clinical eye must therefore never be underestimated. Looking at clinical signs in conjunction with assessing the child's general condition provides valuable additional information (1). It can be the most important background for the decisions that are taken in cases where the scales do not measure correctly.
After babyhood, the child will be weighed at ages two and four. The measuring point at age four is particularly important for being able to determine early development of child overweight/obesity (1). Public health nurses have a particular responsibility for tracking a child's weight and recognising risk factors for overweight/obesity and metabolic disorders (16). Earlier studies have shown that inaccurate scales can lead to miscalculations of a child's BMI (5, 6). It is essential that the scales measure correctly if public health nurses are to prevent overweight/obesity and implement individual interventions.
Control routines and standards for use
According to the weighing and measuring guidelines for the child health clinic and school health services, growth measurements are the surest method for assessing whether children are growing satisfactorily (1). In view of this we question why the same requirements are not made of the scales used in the public health nurse service, as are made at GP surgeries and hospitals (8). Today, it may appear that random circumstances and finances determine the type of scale that is used. While public health nurses do not diagnose and provide medical treatment, they perform health monitoring at the individual and population level by weighing (1).
Since the results show significant differences in accuracy when medically approved and non-medically approved scales are compared, is it far from sufficient to perform health examinations with scales that are not subject to requirements. A standard should therefore also be introduced for the use of medically approved scales in the child health clinic and school health services. WHO recommends that bathroom scales should not be used in assessing a child's growth since they have often proven to be unreliable (17). This bolsters our recommendations to use medically approved scales.
It is conceivable that inaccurate scales can trigger interventions on a completely erroneous basis.
Control routines at child health clinics vary considerably. Few child health clinics tested the scales in accordance with the guidelines, and no child health clinics had routines for testing flat scales. Minor deviations were found while testing 2 kg, but at 5 kg and above the deviations were considerable. Our results showed reduced precision with increasing weight, particularly for non-medically approved scales. These findings are in line with Stein et al. (3), who also report that the scales show reduced precision with increasing weight, and that control routines are important for accuracy. Testing the scales with, for instance, 0.5 kg will give a false sense of security that the scales are accurate.
Schlegel-Pratt and Heizer (4) recommend regular tests with certified weights. For this reason the child health clinics should at least have 5 and 10 kg weights. In this way, systematic tests of both baby and flat scales can be performed with 5, 10 and 15 kg, and more deviations can be discovered. While procurement of weights may be a question of finances, such an investment is a one-off expense that will contribute to greater quality assurance in the public health nurse service.
Transferability to the school health services
In this clinical audit we tested the scales at child health clinics, but we believe that the results can also be transferred to the school health services. The study conducted by Biehl et al. (5), which was performed on scales at various schools, points out that failure to test the scales will likely lead to miscalculations of overweight and obesity. This finding is supported by Gerner et al. (6), who state that inaccurate scales can lead to miscalculations of children’s BMI. In the school health services, children are weighed in the first, third and eighth grade (2). During 40 kg tests, the maximum weight we tested, there was a discrepancy of three and a half kilograms between the lowest and highest measured weight (Table 1). It is conceivable that the deviation will increase with higher weight. An eighth grader can weigh more than 40 kg. Scales in the school health services should therefore be tested with heavier weights, which can be a challenge in terms of procurement and storage. One possibility is to consider a service agreement with a calibration firm.
Strengths and weaknesses
One advantage of the audit was that all data were collected directly at the child health clinics, with no use of intermediaries. Accuracy was thoroughly tested by checking several weights. We also tested repeatability and stability. We recorded the type of scales that were used and could therefore compare results from medically approved and non-medically approved scales. We found few studies about the accuracy of scales through systematic searches for scientific articles and no studies concerning the accuracy of baby scales. Not recording the year in which the various scales were put into service may constitute a weakness, but it was difficult to obtain this information.
Public health nurses have a particular responsibility for tracking a child's weight and recognising risk factors for overweight/obesity and metabolic disorders.
According to Biehl et al. (5), newly procured scales usually measure the correct weight. However, heavy use, incorrect use, general wear and tear, and wear and tear due to frequent transport affect accuracy. A common misunderstanding is that when a scale has been installed and calibrated, instrument error is insignificant (4). The scales at child health clinics are frequently used and are moved in connection with home visits. Combined with the lack of control routines, these factors entail a risk that the scales used at child health clinics measure inaccurately. The study conducted by Stein et al. (3) showed a level of inaccuracy that was three times higher with worn scales than with scales in perfect condition.
Going forward
The final step in a clinical audit process involves implementing measures in practice and conducting a new survey. Data collection per se has no impact unless it is followed up (18). All of the child health clinics received verbal or written feedback about the results of their scales. Conducting this clinical audit heightened awareness of the necessity of testing the scales at child health clinics. Routines must be improved before a new survey can be conducted. A good start would be for all child health clinics to begin following the weighing and measuring guidelines for the child health clinic and school health services by testing the scales a minimum of twice a year. Furthermore, the tests must be conducted with a weight the scale is meant to measure.
Conclusion
This audit, which was conducted on scales in use at child health clinics and during home visits, showed that only nine of 102 (8.8 per cent) baby scales and seven of 50 (14 per cent) flat scales were 100 per cent correct. There were also significant differences in accuracy between medically approved and non-medically approved scales. Only three of 27 (11.1 per cent) child health clinics had good control routines for their scales. Our results thus show that there is a discrepancy between practice and evidence-based recommendations.
Measuring weight is a cost-effective and simple way of gathering data about the population, but the validity of the measurements must be critically assessed. Although the importance of weight measurements is well documented, it appears that there may be a lack of awareness about checking whether the scales actually measure accurately. Ensuring good control routines and introducing standards to use medically approved scales can help to quality assure a valid collection of data in the child health clinic and school health services.
Many thanks to all who made it possible to conduct the study: Jörg Aßmus for helpful guidance in statistics, Evelyn Kvamme for briefing us on weight calibration, and Petur Júlíusson and Jan Larsen for lending certified weights.
References
1. Helsedirektoratet. Nasjonale faglige retningslinjer for veiing og måling i helsestasjons- og skolehelsetjenesten. Oslo: Helsedirektoratet. 2011. Available at: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/236/Nasjonal-faglig-retningslinje-for-veiing-ogmaling-IS-1736.pdf (downloaded 20.04. 2016)
2. Sosial- og helsedirektoratet. Kommunens helsefremmende og forebyggende arbeid i helsestasjons- og skolehelsetjenesten. Oslo: Sosial- og helsedirektoratet. 2004. Available at: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/388/veileder-til-forskrift-kommunens-helsefremmende-og-forebyggende-arbeid-i-helsestasjons--og-skolehelsetj-.pdf (downloaded 20.04. 2016).
3. Stein RJ, Haddock CK, Poston WS, Catanese D, Spertus JA. Precision in weigting: a comparison of scales found in physician offices, fitness centers, and weight loss centers. Public Health Rep. 2005;120:266–70. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1497726/pdf/16134566.pdf (downloaded 20.04.2016).
4. Schlegel-Pratt K, Heizer WD. The accuracy of scales used to weigh patients. Nutr Clin Pract. 1990 Des 5(6):254–7.
5. Biehl, A, Hovengen R, Meyer HE, Hjelmesæth J, Meisfjord J, Grøholt EK et al. Impact of instrument error on the estimated prevalence of overweight and obesity in population-based surveys. BMC Public Health 2013;13:146. Available at: http://www.biomedcentral.com/1471-2458/13/146 (downloaded 20.04.2016).
6. Gerner B, Maccallum Z, Sheehan J, Harris C, Wake M. Are general practitioners equipped to detect child overweight/obesity? Survey and audit. J Pediatr Child Health. 2006;42(4):206–11.
7. Júlíusson PB, Vinsjansen S, Nilsen B, Sælensminde H, Vågset R, Eide GE et al. Måling av vekst og vekt: En oversikt over anbefalte teknikker. Pediatrisk Endokrinologi 2005;19:23–9.
8. Lovdata. Forskrift om krav til ikke-automatiske vekter. 21. desember 2007 nr. 1527. Available at: https://lovdata.no/dokument/SF/forskrift/2007-12-21-1735 (downloaded 20.04.2016).
9. Kunnskapsbasert praksis. Oslo: Nasjonalt kunnskapssenter for helsetjenesten. 2004. Available at: http://www.kunnskapssenteret.no/kunnskapsbasert-helsetjeneste/kunnskapsbasert-helsetjeneste (downloaded 19.05.2015).
10. Nortvedt MW, Jamtvedt G, Graverholt B, Nordheim LV, Reinar LM. Jobb kunnskapsbasert! En arbeidsbok. 2 ed. Oslo: Akribe. 2012.
11. Helsedirektoratet. Nasjonal strategi for kvalitetsforbedring i sosial- og helsetjenesten … Og bedre skal det bli (2005–2015). Oslo: Helsedirektoratet. 2005. Available at: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/233/Og-bedre-skal-det-bli-nasjonal-strategi-for-kvalitetsforbedring-i-sosial-og-helsetjenesten-2005-2015-IS-1162-bokmal.pdf (downloaded 20.04. 2016).
12. Anderson DG. ABC of audit. Tees Valley: Vocational Training Scheme. 2012. Available at: http://www.gp-training.net/training/tutorials/management/audit/audabc.htm (downloaded 19.05.2015).
13. Polit DF, Beck CT. Nursing research: generating and assessing evidence for nursing practice. 8. ed. Philadelphia: Wolters Kluwer Health. 2014.
14. Dewey KG, Nommsen-Rivers LA, Heinig MJ, Cohen RJ. Risk factors for suboptimal infant breastfeeding behavior, delayed onset of lactation, and excess neonatal weight loss. Pediatrics 2003;112(3 Pt 1):607–19.
15. Royal college of nursing. Standards for the weighing of infants, children and young people in the acute health care setting. London: The Royal College of Nursing. 2013. Available at: https://www2.rcn.org.uk/__data/assets/pdf_file/0009/351972/003828.pdf (downloaded 20.04.2016).
16. Helsedirektoratet. Nasjonale faglige retningslinjer for forebygging, utredning og behandling av overvekt og fedme hos barn og unge. Oslo: Helsedirektoratet. 2010. Available at: https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/389/nasjonal-faglig-retningslinje-for-forebygging-utredning-og-behandling-av-overvekt-og-fedme-hos-barn-og-unge.pdf (downloaded 20.04.2016).
17. World Health Organization. Training Course on Child Growth Assessment. Geneve: WHO. 2008. Available at: http://www.who.int/childgrowth/training/en (downloaded 20.04.2016).
18. Benjamin A. Audit: how to do it in practice. BMJ 2008;336:1241–5.









Comments