The challenges associated with implementing new practice
Normalisation Process Theory can be used to assess the prerequisites for ensuring that a new intervention becomes established practice.
Background: A great many initiatives that have proved to be effective have nevertheless failed to be implemented as part of everyday practice. We need knowledge about how to facilitate new initiatives to ensure that their potential for assimilation into established practice is optimised. Increasing numbers of practitioners highlight the need to evaluate the process.
Purpose: Presentation of Normalisation Process Theory (NPT) as a process evaluation tool for use in association with the implementation of new practice. The main principles of the theory are presented and explained in detail through a pilot study, using NPT in the evaluation.
Method: As part of a larger study (EU-WISE), 16 patients diagnosed with type 2 diabetes were enrolled in a pilot study. Nurses introduced an intervention which encourages enhanced use of local networks to help patients cope with their illness. Qualitative in-depth interviews of nurse and patients were conducted by employing a reflection form based on normalisation process theory.
Results: The evaluation process uncovered a number of intervention factors – some obstructing and others facilitating the implementation of network support for patients who struggle with the self-management of chronic disease.
Conclusion: NPT provided a framework for the evaluation that focused not only on the intervention, but also on the specific and practical challenges involved with implementing the initiative.
In the words of Socrates, ‘who knows what is right, will do what is right’, but regrettably this is not always the case. In the literature, we identify two challenges associated with the introduction of new knowledge into nursing practice. In an early phase of nursing research, inadequate access (comprehensibility, applicability etc.) to research findings was given attention. This inadequacy was described as a gap between science and practice (1, 2). Today, researchers are keen to highlight specific, practical implications when research findings are presented, and nurses are trained to read and consider research results. However, the attention has now moved to another challenge: Even if new research is made accessible to practitioners in the field, this does not necessarily result in the implementation of new practice.
Research shows that many effective initiatives are never put into practice, and that health professionals continue to use measures that have little or no impact (2). Even initiatives whose effectiveness is well documented, have taken between one and two decades to be implemented (3). The international literature refers to this challenge as ‘the second translational gap’ (2) or ‘the knowledge-action gap’ (3). The demand for research-based nursing has been accompanied by an increasing interest in the development and evaluation of new initiatives. Research shows that the ‘translational gap’ (4) is particularly prevalent in the primary health service. Despite documented positive results, many research and development projects end up as so-called one-off projects. Why is it that initiatives with documented good efficacy never become part of new practice? The answer to this question suggests that we need tools to help us identify the ‘survival potential’ of interventions.
The purpose of this article is to present such a process evaluation tool: Normalisation Process Theory (NPT) (4–6). We will present the theory and provide examples of its application by describing our experience of testing a new intervention in the primary health service.
Normalisation Process Theory as an evaluation toolkit
The literature suggests that process evaluation is important (4). While evaluation of the intervention focuses on its efficacy, process evaluations focus on what factors are important for the intervention to be implemented as new practice. Theories that focus on the process are therefore important, and a number of different process theories have been developed (4, 5).
NPT is based on recognition that the implementation of complex interventions requires attention to the social processes that are needed for the initiative to be established as part of everyday practice (7). All individuals will act in accordance with their own context. Action is understood as a social process in which the people involved accept the new initiative depending on how well it fits in with their perceptions. Furthermore, a new practice must be capable of adjustment to and implementation within an existing framework and daily schedule (table 1). According to May et al., NPT focuses on:
‘… the work that actors do as they engage with some ensemble of activities (that may include new or changed ways of thinking, acting, and organising) and by which means it becomes routinely embedded in the matrices of already existing, socially patterned, knowledge and practices’ (7).
Intervention toolkit
Based on Normalisation Process Theory, British scholars have developed a toolkit (8) for investigating aspects of new interventions. In particular, the toolkit focuses on how new practice may be ‘normalised’ within an organisation or within a profession, and not least accepted by the target group (the patients). NPT is thus an appropriate model for complex interventions which involve several actors (and organisations).
The core questions in NPT are associated with the actors (nurses as well as patients, as service users), the intervention itself, and the organisation. The model is prospective and helps us look ahead, towards factors that may obstruct or facilitate the implementation of new practice. The theory focuses on four elements that have proved key to either facilitating or obstructing the implementation of new practice (4, 6):
- Relational integrationis associated with the actors’ perception of the new intervention and establishes by means of questions whether all actors share an understanding of the intervention and what is to be done.
- Interactional workabilityfocuses on how much the new practice is considered to differ from former practice. Attention is directed to the scope of the change, and whether the change represents an entirely new way to look at something or perceive something.
- Skill-set workabilityis associated with the question of whether the new intervention requires new knowledge and/or who is responsible for what needs to be done.
- Contextual integrationinvestigates the workability of the change within its intended setting. Is everything in place for the new practice to be implemented in the current context, or will it require major organisational and/or resource-related change?
It is important to note that NPT can, and should, be applied in connection with the development of a new intervention as well as in the evaluation of this intervention when tested (9).
Evaluation of interventions
The following presents an evaluation of an intervention which used NPT as a framework for obtaining the respondents’ experiences. The study presents findings from a pilot study of patients’ experiences with a network-centred practice designed to facilitate self-management of type 2 diabetes. The pilot study forms part of a major international project: EU-WISE, funded under EU’s seventh framework programme. The project is a four-year collaborative programme involving six European countries and is intended to develop good community initiatives for helping patients to cope with chronic or long-term disease. The number of patients with type 2 diabetes is large and rising (10), and the disease puts great demands on the patient’s self-management skills (11, 12). This is why these patients were chosen as the target group for the EU-WISE project.
Intervention developed as a supplement
Existing initiatives to stimulate self-management of type 2 diabetes are intended to stimulate the behaviour of individuals through knowledge and motivation (13). This is helpful for some (14), while other patients drop out for various reasons (15, 16), which suggests a need for a range of different approaches. There is clear connection between a limited social network and poor self-management of chronic disease (17, 18). In this context, ‘social network’ refers to family, friends, colleagues, interest organisations etc. with which a person is associated.
Patients who never considered the diagnosis to be serious, were not interested in the initiative.
Based on trials (19) and literature compilations (11, 20, 21) the EU-WISE project has developed the European Generating Engagement in Networks Involvement (EUGENIE) intervention. The EUGENIE intervention was tested as a supplement to existing programmes in a pilot study conducted in the period from August to November 2014 in a Norwegian municipality. The purpose of the pilot study was to contribute to the development of the intervention with a view to assessing its suitability for further use on a larger scale in Norway. We chose NPT because we wanted our approach to allow us to assess whether this intervention might be implemented as part of normal practice, and what might need to be adjusted before testing the intervention on a larger scale.
The objective of this part study is thus to investigate whether the use of NPT gives us a good insight into how service users, in this case the patients and nurses, assess the quality of the EUGENIE toolkit and therefore its viability.
Method
Recruitment and sample
A nursing clinic run by the municipal health service agreed to test the EUGENIE intervention. The nursing clinic is part of a recently established medical centre located in Eastern Norway. The municipality provides out-patient training programmes, follow-up and self-management support for patients with chronic or long-term afflictions. The nurses at the nursing clinic and the doctors at the regional hospital’s out-patients’ clinic gave eligible patients verbal information about the EUGENIE study and invited them to take part in the pilot study. A total of 16 patients took part, which complies with the protocol established for the main project.
The inclusion criteria for participation were type 2 diabetes diagnosis in patients aged 18 or above, and sufficient fluency in Norwegian to be able to take part in a qualitative interview without an interpreter. Exclusion criteria were patients with a combination of type 2 and type 1 diabetes, and pregnancy-related diabetes. We also interviewed one of the two nurses who conducted the intervention.
We started by informing the patient about the background and purpose of the intervention. We also obtained the patient’s written informed consent to take part in the study. The study was approved by the Regional Committees for Medical and Health Research Ethics (REK South-East). Furthermore, we obtained the consent of the institution’s management.
The intervention
The EUGENIE intervention focuses on strengthening the personal networks of people with chronic diseases like type 2 diabetes. The intervention involves a conversation between a nurse and a patient within the framework provided by the EUGENIE toolkit. Figure 1 shows the four stages of EUGENIE.

The nurses who took part in the intervention received training which introduced them to the background for the intervention and taught them how to use the EUGENIE toolkit. The nurses already had an overview of activities available within the local community, such as local walking groups, diet and nutrition courses, senior dancing groups etc.
Material and data collection
The researcher asked the patients’ permission to observe their session with the nurse, and it was agreed that the researcher would then conduct an interview with the patient immediately following the intervention. The interview was conducted in a different room to where the intervention took place. The research interviews started by inviting the patients to share their thoughts about their conversation with the nurse, what it had felt like to answer the EUGENIE toolkit questions, and what they thought about the invitation to increase their involvement with various networks. In addition to the open-ended introductory questions, we followed up the interview with more structured questions based on NPT (table 1) and earlier evaluations of similar interventions (22).
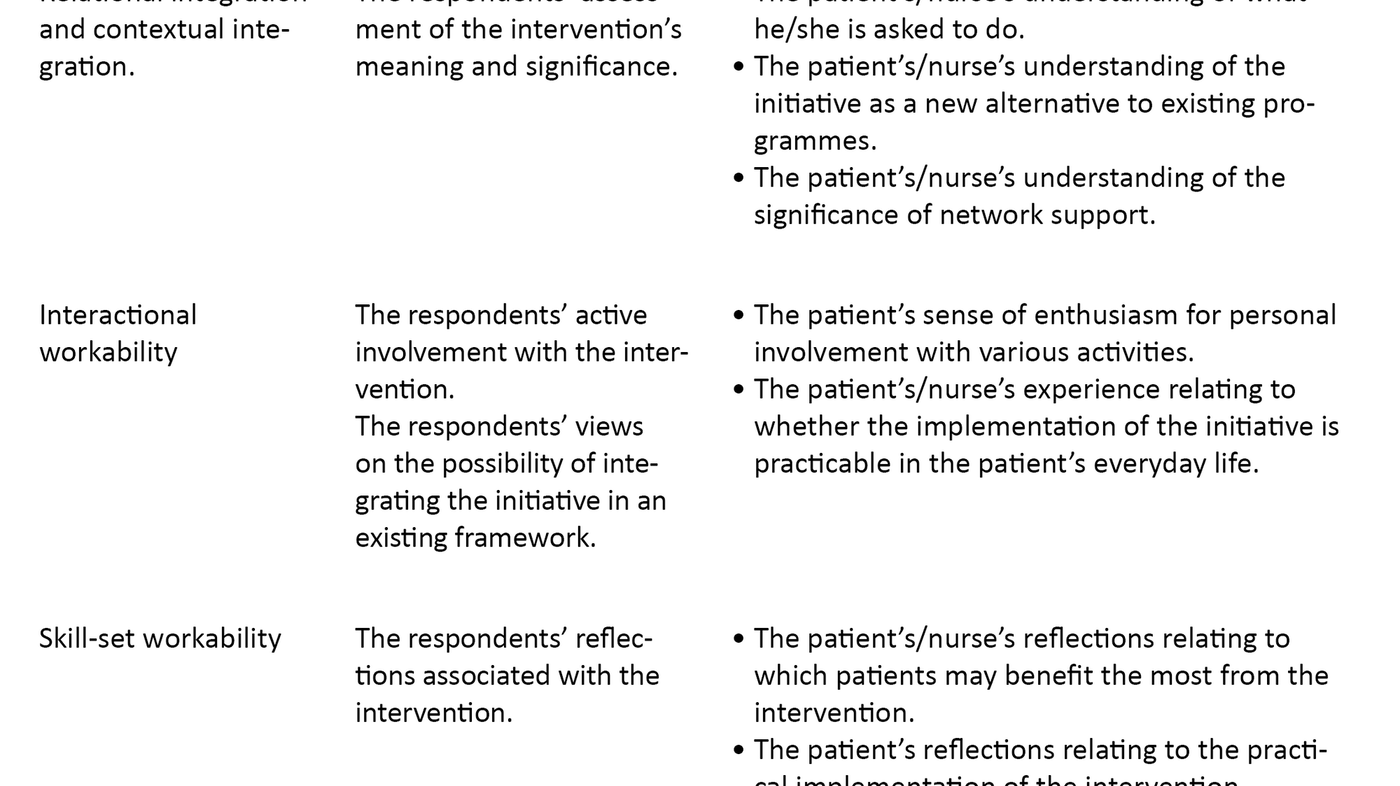
The nurses who took part in the intervention discussed their experiences between themselves and found that they were very similar. One of the two nurses who had taken part in the intervention was interviewed after the project had ended. This interview was also structured in accordance with the NPT elements (table 1).
The duration of the interviews varied between ten and 28 minutes, and they were recorded on a digital sound recorder. We transcribed all the interviews consecutively; the nurse was interviewed after the project had been completed. This interview lasted longer (50 minutes) and was open-ended, but the interviewer ensured that all parts of the intervention were discussed.
Data analysis
Our content analysis is inspired by Kvale and Brinkmann’s (23) description of theoretically driven analysis of interviews. First, we close-read the complete interviews. In this phase, we put emphasis on the respondents’ answers to the first open-ended question of the interview because we assumed that this would reflect the respondents’ immediate thoughts about what was important to them. At the same time, the application of normalisation process theory remained at the heart of the analysis process throughout, as we made use of a reflection form. The NPT-based reflection form (table 1) worked as a tool for the analysis in that overarching themes as well as the associated questions helped to direct attention to the elements that are key to NPT.
After reviewing the data material several times, we organised the themes according to their corresponding reflection form components. This suggests a relatively theory-led analysis, even if the material was analysed ‘both ways’: open-ended based on the introductory questions and theory-driven via the reflection form. During the analysis process, we reviewed the data material in its entirety on several occasions in order to check that no meaningful items were missed.
Findings
Because patients were recruited via the specialist out-patient service, many of our respondents were suffering late complications and struggled a great deal with their diabetes. Despite the fact that the respondents were positively inclined to take part in the interview, many of them gave relatively brief answers. In the following, we will present the intervention experiences as recounted by respondents and nurses. The presentation is structured according to the main elements of NPT. However, skill-set workability and the potential for contextual integration have been merged to form a single item because responses appeared to be overlapping.
Relational and contextual integration
The respondents’ immediate reflections on the intervention varied. Some patients understood the purpose of the first part of the intervention, the mapping, within the framework of a medical survey-finding mission, and thus saw the exercise as a requirement to meet the needs of the health service. Consequently, in these instances the patient and the nurse do not have a shared understanding of the purpose served by the mapping of networks. Other patients quickly grasped ‘the idea’ and expressed enthusiasm for the focus on networks. Like many of the patients, the nurses reflected that the focus on networks was unfamiliar, but very rewarding.
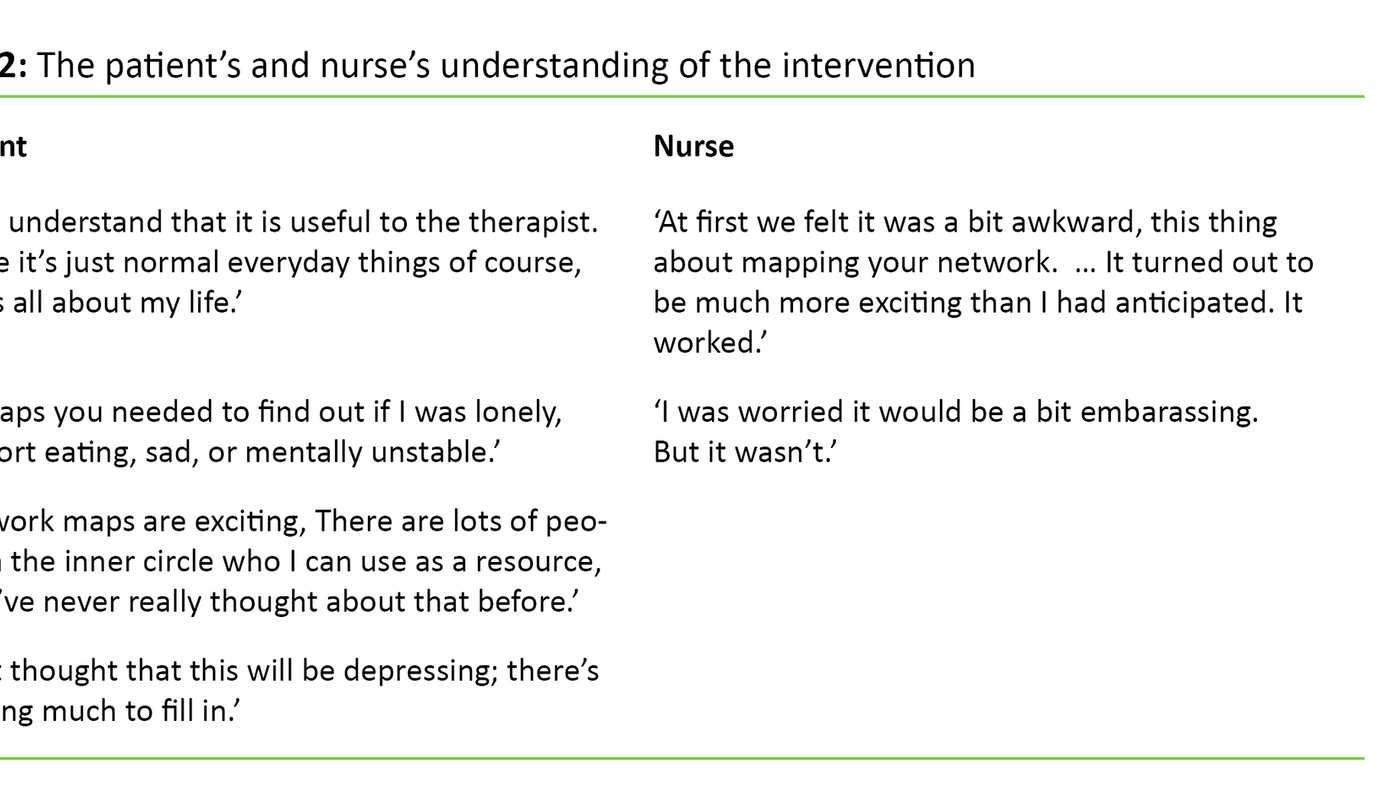
It may seem that both nurse and patients considered the mapping of networks to be potentially difficult. Having a small network may be considered to carry a stigma, and some patients expressed embarrassment.
Interactional workability
All patients completed the EUGENIE instrument used during their session with the nurse and made arrangements for a further appointment. Most of the patients were actively involved with identifying activities that would be appropriate for themselves. Some patients asked for particular activities, while others awaited suggestions from the nurse. Several patients felt that the intervention could contribute to a more active lifestyle.
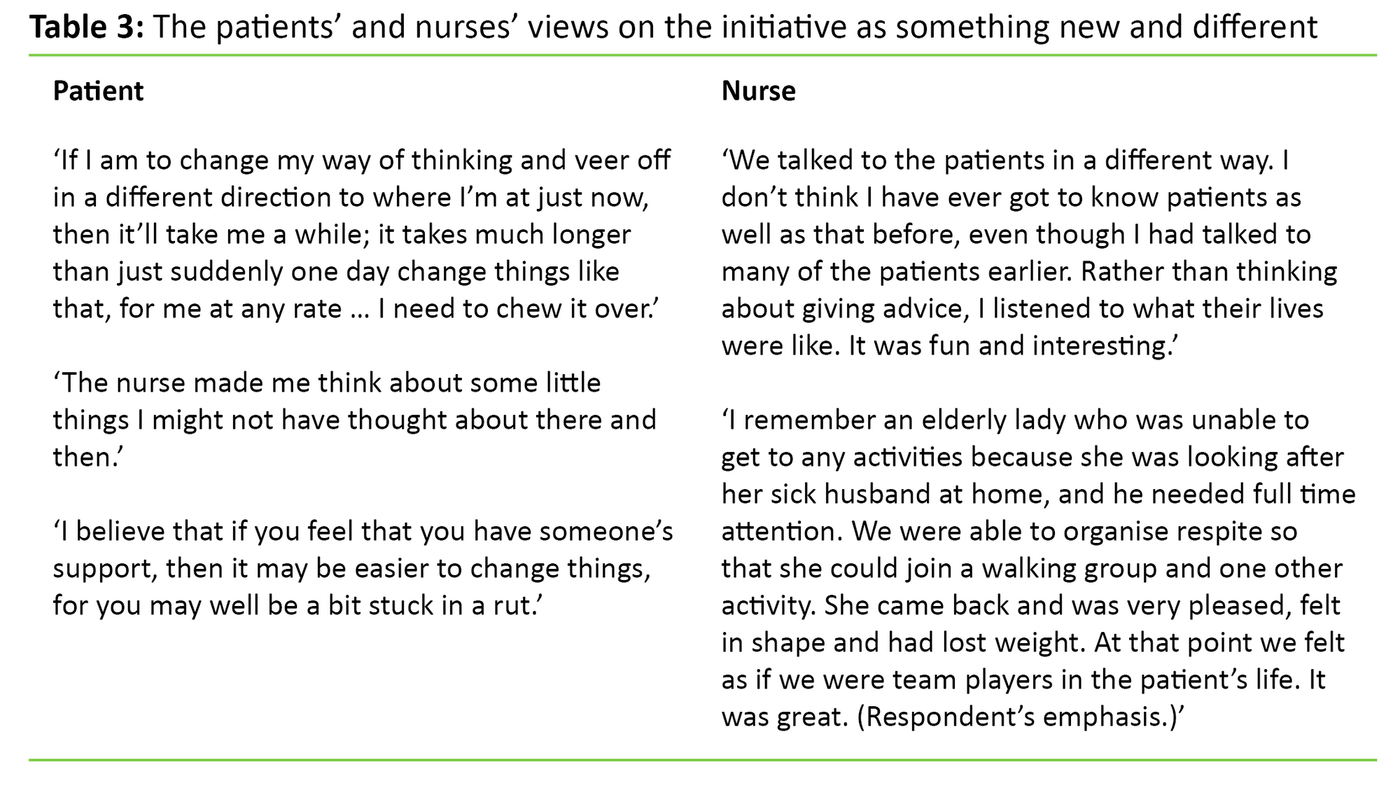
Any change that differs significantly from earlier practice will put great demands on the people involved. The patients as well as the nurse considered the intervention’s focus on networks to be a novel idea. Some patients said that they started to reflect on their own network in a new way and thereby discovered resources they had previously not been aware of. The nurse also pointed out that the approach gave new access to initiatives that could be integrated into the patient’s everyday life in a positive way. The patients as well as the nurse were of the opinion that time is needed for reflection and adjustment before the network approach can be integrated as a natural part of the nurse’s appraisal of the patient, or the patient’s self-understanding.
Skill-sets and the potential for contextual integration
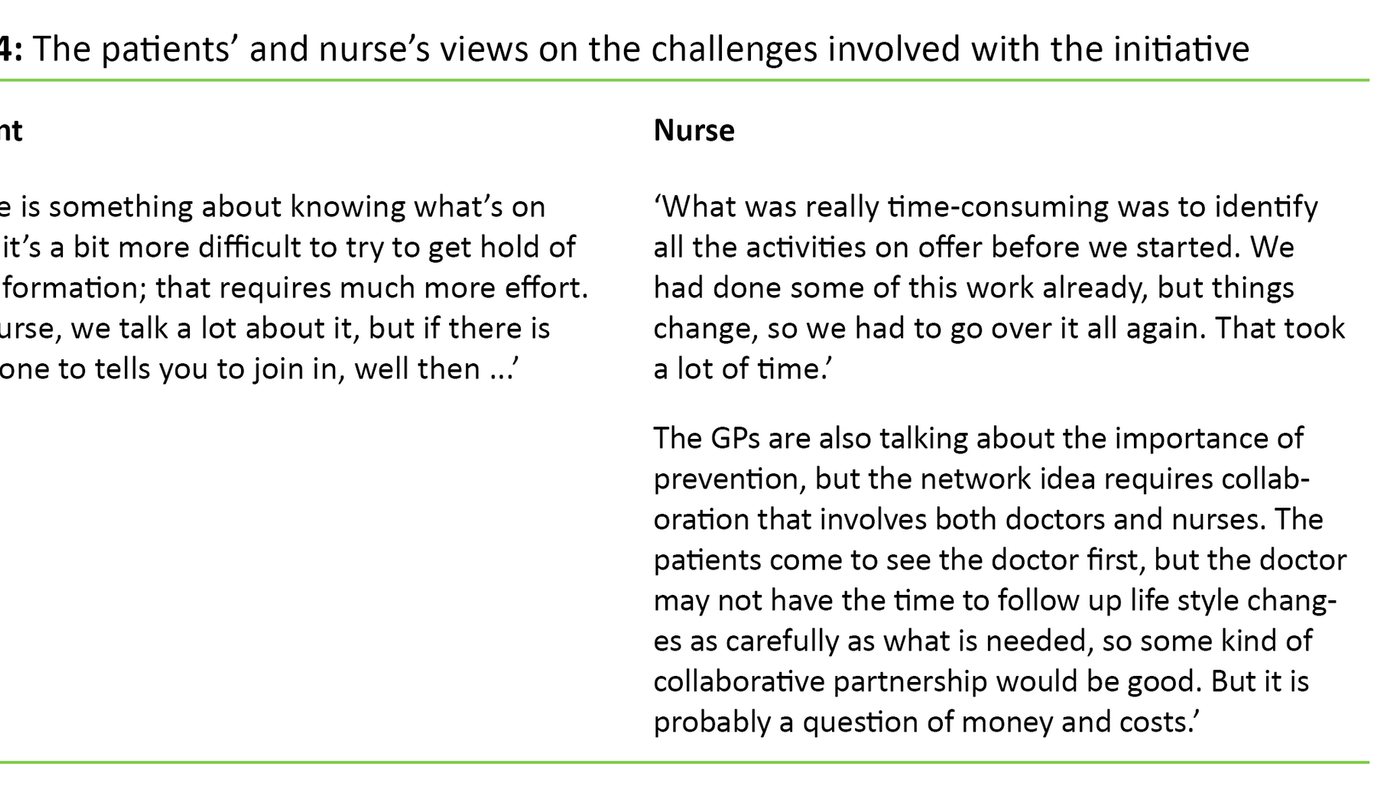
Many patients pointed out that it is important to partner up with someone to get active. A number of patients wanted the nurse to contact the organisers of the activities on their behalf to agree when and where to attend. The nurses pointed out that the new intervention required significant effort in order to obtain and maintain an overview of all the community programmes on offer at any given time.
Several patients wished to recommend the intervention to others. The pilot study suggested that it was the elderly patients who were the keenest to talk about possible resources within their network. They also talked about what they could do to make better use of these resources or to expand their networks. Several elderly women also talked about care responsibilities which made it difficult for them to take part in activities. For these women, practical facilitation was an important initiative.
Discussion
We made use of NPT as an approach by which to explore whether the EUGENIE intervention is acceptable and workable in the eyes of our sample of patients with type 2 diabetes and their nurse. The pilot study is small and the participants are monitored over a very short period of time. Our findings will therefore have to be considered in the light of the study’s limitations.
Most respondents were open to a network-style approach. The mapping of patient networks is a sensitive topic which will require a considerate approach by health personnel who wish to make use of network mapping as a tool. A large proportion of the patients became more aware of resources within their own networks and wanted to take part in new activities. Like other initiatives that aim to stimulate the behaviour of individuals through knowledge and motivation, a network-oriented approach will not help the self-management of every patient. Patients who did not consider their diagnosis to be serious, were not interested in the initiative. This experience is supported by earlier research (19) and indicates that the EUGENIE intervention, like other interventions, will not appeal to all patients diagnosed with type 2 diabetes.
Any change that differs significantly from earlier practice will put great demands on the people involved.
Most respondents felt it was challenging to cope with the demands of their disease. The nurse as well as the patients expressed the view that the network approach was new and unfamiliar to them. The fact that the respondents saw the intervention as a new idea, did not generally appear to engender scepticism towards the intervention, as described in earlier research (24, 25). Although most of the respondents were active and interested in finding appropriate activities, their statements suggest that new concepts need time and perhaps repeated sessions to become established.
Given the above reservations, we draw some tentative conclusions. The intervention appeared to potentially provide an important supplement to existing practice. A pre-existing plan of all activity programmes on offer is a prerequisite, to ensure that health professionals need not spend time on compiling and maintaining such listings. Patients as well as health personnel consider it important that enough time and preferably more than one session, is set aside to ensure that patients are able to assimilate the new way of thinking. The nurse also needs time and training to conduct the intervention. It is important to ensure that such training of health personnel gives due attention to the ethical sensitivity required in connection with the mapping of patients’ network.
Some patients considered the network mapping exercise to form part of the data collection procedure required for the health professionals to satisfy the need for patient information. This perception suggests that the relational integration of the intervention was not always successful, and this may have had an obstructive effect. However, the nurse and patients appeared to take a positive attitude to the changes involved with the new approach, and they considered them to be workable within the context of the patient’s day-to-day life as well as within the nursing framework. If the local authorities have no comprehensive schedule of existing activity programmes, the intervention becomes more demanding since a listing of all existing programmes needs to be compiled first.
Conclusion
The purpose of health care interventions is to make people better. In order to meet this objective, researchers need to ensure that the interventions they develop can be implemented. NPT provides a toolkit to this end. It is rare for anyone to examine the prerequisites for a new intervention to be implemented as new practice, and this may well form part of the reason for the ‘translational gap’ that we described in the introduction.
This article has presented a tried and tested conceptual model as a tool to evaluate the process of implementing a clinical intervention. We have wanted to clarify the theory by allowing its various elements to structure our analysis as well as our presentation of findings and discussion. We have demonstrated how the model may be used by presenting, by way of an example, an intervention involving adult patients diagnosed with type 2 diabetes. It is important to point out that the process evaluation must be pre-planned and form part of the intervention from the very beginning of the project.
The EUGENIE intervention appeared to be a new and engaging approach to the self-management of disease, from the patient’s as well as the nurses’ perspective. The study’s findings are important for the continued development of the intervention. By using NPT as a framework, we were able to focus not only on values and thought processes, but also on specific and practical every-day challenges in the lives of patients and nurses. We were able to expose obstructing as well as facilitating factors that may affect the degree to which a network approach can be established as one of the support programmes offered to patients with chronic illness so that they can cope with everyday life.
References
1. Kirkevold M. Vitenskap for praksis? 4. ed. Oslo: Gyldendal Akademisk. 2004.
2. Lau R, Stevenson F, Ong B, Dziedzic K, Elridge S, Everitt H et al. Addressing the evidence to practice gap for complex interventions in primary care: a systematic review of reviews protocol. BMJ Open 2014;4.
3. Hakim A. Vascular disease. The tsunami of health care. Stroke 2007;38:3296–301.
4. May C, Finch T, Mair F, Ballini L, Dowrick C, Eccles M. Understanding the implementation of complex interventions in health care: the normalization process model. BMC Health Services Research 2007;7(1):148–55.
5. May C, Finch TL, Ballini L, MacFarlane A, Mair FS, Murray E et al. Evaluating complex interventions and health technologies using normalization process theory: development of a simplified approach and web-enabled toolkit. BMJ Health Services Research 2011;11.
6. May C. A rational model for assessing and evaluating complex interventions in health care. BMC Health Services Research 2006;6.
7. May C, Mair FS, Finch TL, MacFarlane A, Dowrick C, Treweek S et al. Development of a theory of implementation and integration: Normalization Process Theory. Implementation Science 2009;4(29).
8. May C, Mair F, Dowrick CF, Finch T. Process evaluation for complex interventions in primary care: understanding trials using the normalization process model. BMC Family Practice 2007;8.
9. Murray E, Treweek S, Pope C, MacFarlaine A, Ballini L, Dowrick C et al. Normalication process theory: a framework for developing, evaluating and implementing complex interventions. BMJ Medicine 2010;8.
10. Helsedirektoratet. Diabetes – forebygging, diagnostikk og behandling. Nasjonale faglige retningslinjer. 2009. Available from: https://helsedirektoratet.no/retningslinjer/diabetes. (Downloaded14.11.2016).
11. Foss C, Knutsen I, Kennedy A, Todorova E, Wensing M, Lionis C et al. Connectivity, contest and the ties of self-management support for type 2 diabetes: a meta-synthesis of qualitative literature Health and Social Care in the Community 2015; 24(6):672-686. doi: 10.1111/hsc.12272
12. Knutsen IAR, Foss C, Todorova E, Roukova P, Kennedy A, Portillo MC et al. Negotiating diet in networks: A cross-European study of the experiences of managing type-2 diabetes. Qualitative Health Research 2015.
13. Ong BN, Rogers A, Kennedy A, Bower P, Sanders T, Morden A et al. Behaviour change and social blinkers? The role of sociology in trials of self-management behaviour in chronic conditions. Sociology of Health and Illness 2014;36(2):226–38.
14. Austvoll-Dahlgren A, Nøstberg AM, Steinsbekk A, Vist GE. Effekt av gruppeundervisning i pasient- og pårørendeopplæring: en oppsummering av systematiske oversikter [The effects of group education on patients and their next of kin]. Oslo: Nasjonalt kunnskapssenter for helsetjenesten. 2011. Available from: http://www.kunnskapssenteret.no/publikasjoner. (Downloaded 14.11.2016).
15. Sandaunet A. The challenge of fitting in: non-participation and withdrawal from an online self-help group for breast cancer patients. Sociology of Health & Illness. 2008;30:131–44.
16. Bury M, Pink D. The HSJ debate. Self-management of chronic disease doesn't work. Health Services Research 2005;115(5947):18–9.
17. Blickem C, Kennedy A, Vessilev I, Morris I, Jarlwala P, Rogers A. Linking people with long-term health conditions to healthy community activities: development of Patient-Led Assessment for Network Support (PLANS). Health Expectations 2013;16(3):48–9.
18. Morris RL, Saunders C, Kennedy AP, Rogers A. Shifting priorities in multimorbidity: a longitudinal qualitative study of patients' prioritization of multiple conditions. Chronic Illness 2011;7:147–61.
19. Blickem C, Kennedy A, Jariwala P, Morris R, Bowen R, Vassilev I et al. Aligning everyday life priorities with people's self-management support networks: an exploration of the work and implementation of a needs-led telephone support system. BMC Health Services Research 2014;14.
20. Vassilev I, Rogers A, Kenned A, Koetsenruijter J. The influence of social networks on self-management support: a metasynthesis. BMC Public Health 2014;14:719–30.
21. Kousoulis A, Patelarou E, Shea S, Foss C, Ruud Knutsen I, Todorova E et al. Diabetes self-management arrangements in Europe: a realist review to facilitate a project implemented in six countries. BMC Health Care Services Research 2014;14:453.
22. Vassilev I, Rogers A, Blickem C, Brooks H, Kapadia D et al. Social Networks, the 'Work' and Work Force of Chronic Illness Self-Management: A Survey Analysis of Personal Communities. Plus One 2013;8(4). doi:http://dx.doi.org/10.1371/journal.pone.0059723
23. Kvale S, Brinkmann S. Det kvalitative forskningsintervju. 2. ed. Oslo: Gyldendal Akademisk. 2009.
24. Lamas K, Graneheim UH, Jacobsson C. Experiences of abdominal massage for constipation. J Clin Nurs 2012;21(5-6):757–65.
25. Jacobsen ET, Rasmussen SR, Christensen M, Engberg M, Lauritzen T. Perspectives on lifestyle intervention: the views of general practitioners who have taken part in a health promotion study. Scand J Public Health 2005;33(1):4–10.









Comments