Incident reporting – a difficult balancing act
The purpose of reporting adverse incidents is not to point to scapegoats, but to increase patient safety. Nevertheless, many professionals fail to report unwanted incidents, a study shows.
Background: Although health authorities expect patient safety incidents to be reported, research shows that such incidents are underreported, and the reasons for this are currently being debated. Knowledge is needed on the factors that promote and inhibit incident reporting in the health services.
Objectives: To describe factors that influence midwives’ and mental health nurses’ decisions on whether or not to report adverse incidents.
Method: The study has a quantitative design. Data were collected using a self-administered written questionnaire. The respondents were midwives and mental health nurses (n = 133).
Main results: The majority of informants were familiar with the procedures for reporting adverse incidents, but had more knowledge of the procedures for reporting clinical errors than unethical practice. The main motivation for reporting such incidents was to avoid harm to patients. However, the informants’ own interests or the interests of their work colleagues affected the decision of whether or not to report.
Conclusion: The midwives and mental health nurses highly prioritised the patients’ rights. Still, reporting adverse incidents is complicated and is influenced by cultural and organisational factors.
Health authorities work, nationally as well as internationally, to lower the frequency of adverse incidents in the health services (1 – 3). One measure is the establishment of systems for reporting such incidents. The reports will be used to prevent the repetition of unwanted incidents, and the emphasis is on the reports’ contribution to learning. A precondition for learning from adverse incidents is awareness of the existing incidents.
Research shows that such incidents are underreported, and that the health services lack knowledge on why health professionals fail to report incidents as they happen. Nurses are central actors in the health services. Knowledge of their attitudes to, and experiences of, reporting incidents is thus important when the health services shall meet government expectations to a system and culture for learning from errors (4).
Attention to patient safety
The Norwegian Specialist Health Service Act § 3 – 3, § 3-3a and §4 (5), and The Internal Control Regulations (6) require that the specialist health services have a reporting system and routines for following up incidents. They are also required to give the supervisory authorities (The Knowledge Centre and Norwegian Board of Health Supervision) information on events that have or may have endangered patient safety (5, 6). In line with this nurses are motivated by education and professional ethical guidelines to pay close attention to patient safety. Point 5.4 in the Code of Ethics for Nurses states: “The nurse reports or gives notification of any situation where patients are exposed to blameworthy or unjustifiable conditions. Loyalty to the workplace shall not prevent this” (7).
Although patient safety has been a priority for several decades, the research field is relatively new. Proper concepts and definitions are being developed. This is one definition of patient safety: “Patients shall not be subjected to unnecessary harm or risk as a result of the health services’ efforts or lack of such” (8, p 6).
It is difficult to report adverse incidents caused by a colleague.
The concepts of “unwanted incident”, “adverse event”, “error”, “reprehensible actions” and “negligent” or “irresponsible” practice are used for incidents in which the patient is in danger or being harmed or is harmed (8). Words like “whistle blowing”, “report” and “incident-reporting” are used about actions that lead to the uncovering of such incidents.
In this article, we use the concept “incident” in such a way that it encompasses harm and danger for harming the patient. We use the concept “reporting incidents” about reporting such incidents to someone with the authority to do something about it.
Prior research
Research shows that nurses are continuously and actively involved in patient safety work. They expect, from themselves and from others, to be the patient’s advocate and report adverse incidents (9-11). However, reporting such incidents appears to result in formal and/or informal sanctions such as retribution, workplace ostracism, silencing and loss of advancement possibilities or change in employment terms (12 – 18). There are reports that both formal and informal sanctions have led to physical, psychological and /or social stress, with subsequent reduction in health and work capacity (14 – 18).
The choice between reporting and not reporting is influenced by conditions at both the individual and system level. There may for instance be a lack of familiarity with reporting routines, low consensus on what to report, experience that reporting does not result in anything being done, and a lack of support from the work environment (14 – 17, 19). Research on the psychosocial consequences for those that cause incidents and conditions that encourage and discourage reporting (16-19) is wanted. The purpose of this project was to describe factors that influence midwives’ and mental health nurses’ reporting of adverse incidents.
Method
This study is part of a research project carried out in collaboration with nursing researchers at the Molde University College and James Cook University in Australia. We used both quantitative and qualitative methods (20). We here present the result from the Norwegian quantitative questionnaire.
Sample and recruitment
The inclusion criteria were valid authorisation or accreditation as mental health nurse or midwife. These two groups were specialist nurses the research team had knowledge about. We also assessed the two groups as having comparable professional functions and independence in their professional work in both Norway and Australia.
We recruited the informants from the specialist health services, from maternity/neonatal units and psychiatric units at ten hospitals widely distributed in Norway. The leader of the organisations informed employees of the study and handed out information and questionnaires. The employees were free to choose to respond to the questionnaire online through a web address or on a paper version with an addressed and stamped response envelope enclosed. For reasons of practicability in carrying out the survey, we did not collect data on the number of nurses who were invited to participate. We have therefore not calculated response percentage.
Data collection
The researchers from Norway and Australia collaborated on developing the questionnaire. We also gained permission to use parts of a questionnaire we had used earlier, developed by Firth-Cozens, Firth and Booth (20-21). Through discussion, researchers with long clinical experience arrived at themes important to explore, and agreed on the questions’ central concepts and content. The questions were worded in parallel in Australian English and Norwegian. We used the concepts of “clinical practice” and “unethical practice” to distinguish between incidents related to clinical treatment, such as errors in medication, and incidents related to unethical actions.
Before reporting, one fourth would consider the risk of losing the job.
We first tried out the questionnaire in a pilot study before modifying it for use in the main study. The questionnaire had 31 questions with a total 62 variables and several types of response alternatives. Ten questions were answerable by “yes”, “no” or “don’t know”. One had a Likert scale with the response alternatives “very difficult”, “difficult”, “neutral”, “easy” and “very easy”. Two questions had the response alternatives “very important”, “important”, “unimportant” or “very unimportant”. For one question the respondents were to range the response alternatives from first to fifth priority. Missing data did not exceed 8 per cent on any question.
Ethical considerations
The researchers recognise the potentially sensitive character of the data, and confidentiality and anonymity became ruling principles in the study. We used an anonymous questionnaire with no coding and no reminder possibilities. The raw data did not contain names of participants or workplace. We assumed that no participant would get into trouble as a result of participation in the study, but should this happen, the participants were given names of members of the research group who would be available. The researchers were not employed and did not have work colleagues in the hospitals from which the participants were recruited. The information pamphlet emphasised that participation in the study was voluntary. Those choosing to participate consented by returning the completed questionnaire. The study is approved by The Norwegian Centre for Research Data.
Data analysis
Data were analysed using IBM SPSS Statistics version 22 (Boston, USA). We used descriptive statistics with frequency analyses, cross tabulation and comparisons of mean, central tendency and data spread to gain an overview and describe sociodemographic data. Inferential statistics with chi-square test were used to study relationships between midwives and mental health nurses, and between those who reported incidents and those who did not. Independent variables were made dichotomous. We set the significance level at p < 0.05.
Result
53 per cent (70) mental health nurses and 47 per cent (63) midwives responded. All respondents worked in the specialist health services and were 23 years of age or older (n=133). The midwives had from two to 34 years of work experience (median 12.8 years), and the mental health nurses from one to 40 years (median 10.6 years). There was no significant relationship between profession and years of work experience. As only 18 men participated, we do not distinguish between genders in the presentation of the results. We use the collective designation “specialist nurse “ for midwives and mental health nurses.
Experience with incident reporting
11.9 per cent (15) of respondents stated that they had given the wrong medication at least once during the past 12 months, while 4.0 per cent (5) responded that they had given a wrong treatment to a patient during the same time period (n=126). Of those who had given the wrong medication, 20.0 per cent (3) stated that they had not reported the incident. All who had given a wrong treatment had reported the incident.
65.4 per cent (87) of the respondents had at least once witnessed an adverse unwanted incident caused by others. There was no significant relationship between experience with such incidents and profession. 50.6 per cent (44) reported the incident, and 44.8 per cent (39) did not. Of the ones that did not report the incident, 76.9 per cent (30) stated that they should have done so, while 11.4 per cent (5) of those who had reported the incident would not have done so again. Significantly more mental health nurses, 37.3 per cent (31), than midwives, 15.7 per cent (13), had reported incidents (p=0.003) (n=83).
Awareness of procedures for reporting incidents
With regard to awareness of reporting routines for clinical errors, 13.1 per cent (17) stated that the workplace did not have, or that they were unaware whether the workplace had, procedures for this. There was no significant relationship between awareness of such procedures and profession. There was, however, a significant difference between the professions with regard to awareness of procedure for reporting unethical practice. Of those that answered that they were not aware of any such procedures, 37.0 per cent (48) were midwives and 25.4 per cent (33) were mental health nurses (p=0.001) (n=130).
The reporting process
The respondents stated that it was difficult to report an incident caused by a colleague. As many as 67.7 per cent (90) found it difficult to report an incident when the colleague in question is a nurse. 63.2 per cent (84) stated that it was difficult to report an incident when the colleague is not a nurse.
The question on why it is important to report adverse incidents did not distinguish between incidents caused by the respondent and incidents caused by others. “Improve practice/minimise harm” scored the highest on the ranking of reasons for reporting incidents, but more mental health nurses, 7.8 per cent (10), than midwives, 1.6 per cent (2), ranked this as less important (table 1).
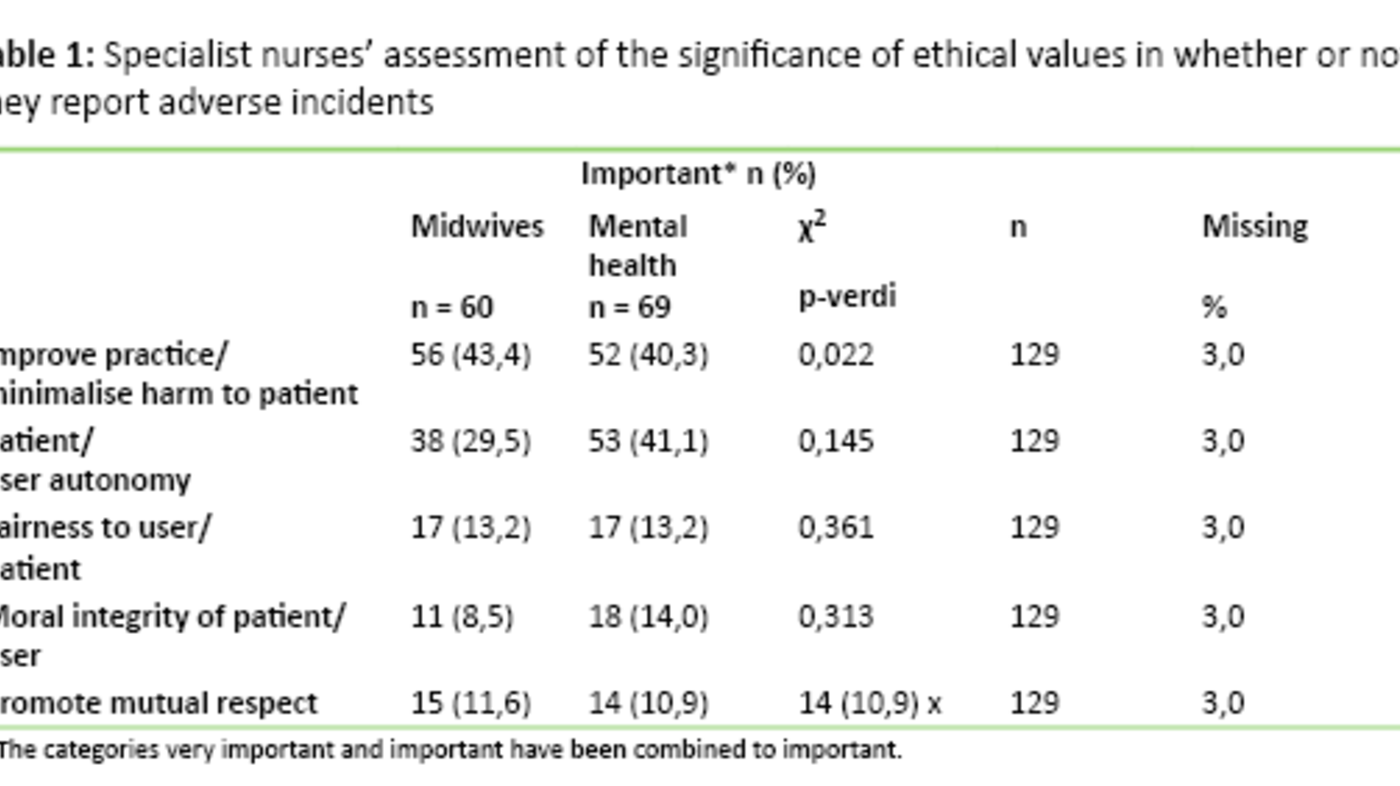
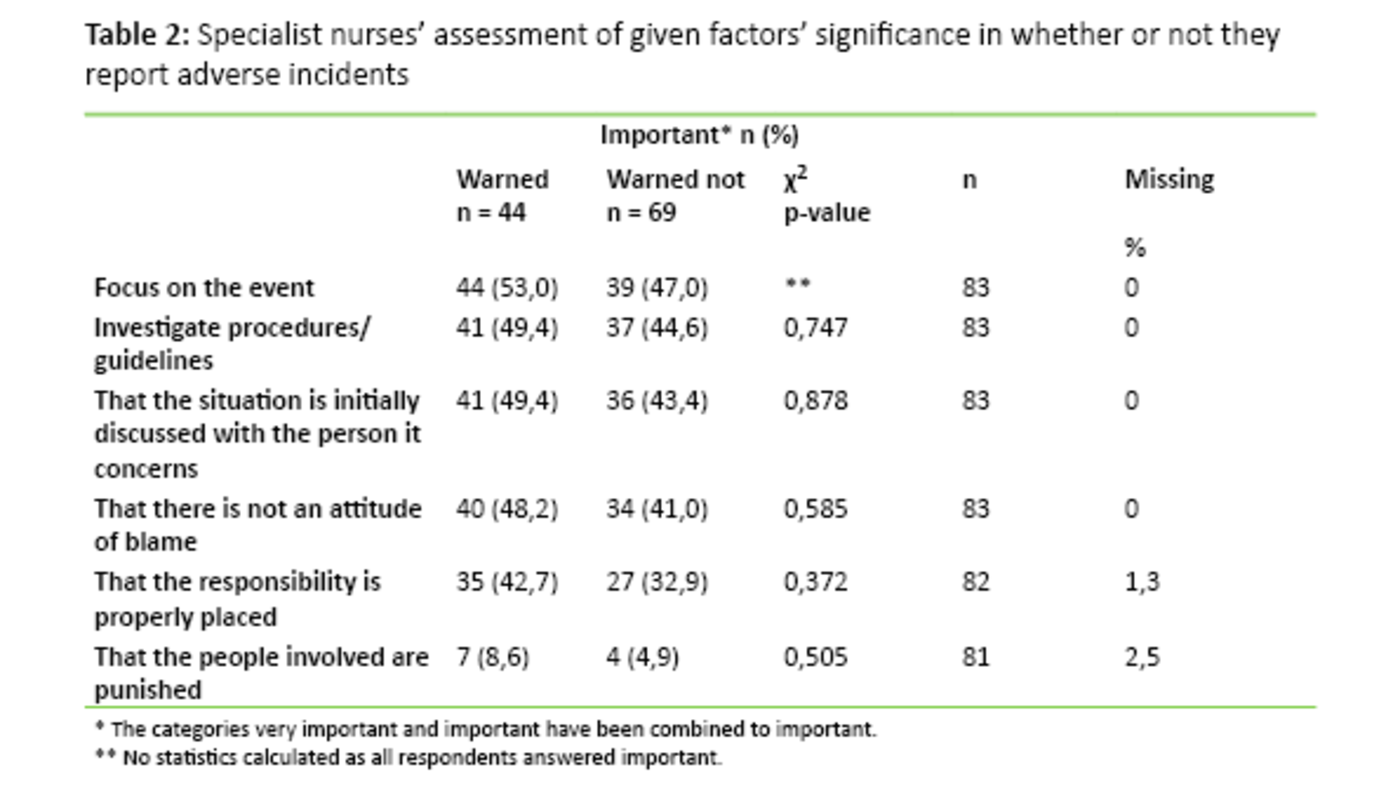
The informants ranked five factors in response to what matters should be attended to for reporting to be an option (table 2). All respondents, 100 per cent (130), said it was important to “focus on what had happened”. 94.6 per cent (123) responded that it was important that the “guidelines be investigated”. 93.8 per cent (122) responded that “the situation first be discussed with the person it concerns” and 93.1 per cent (121) that it was important “ to not assume an attitude of blame”. The lowest score was related to placing the blame for the incident: 81.4 per cent (105) stated it was important to place responsibility, while 18.0 per cent (23) responded that it was important that “those involved be punished”. There was no significant relationship between the professions and the given factors (n=130). Table 2 shows the distribution of those who reported, and those who had considered reporting, but did not.
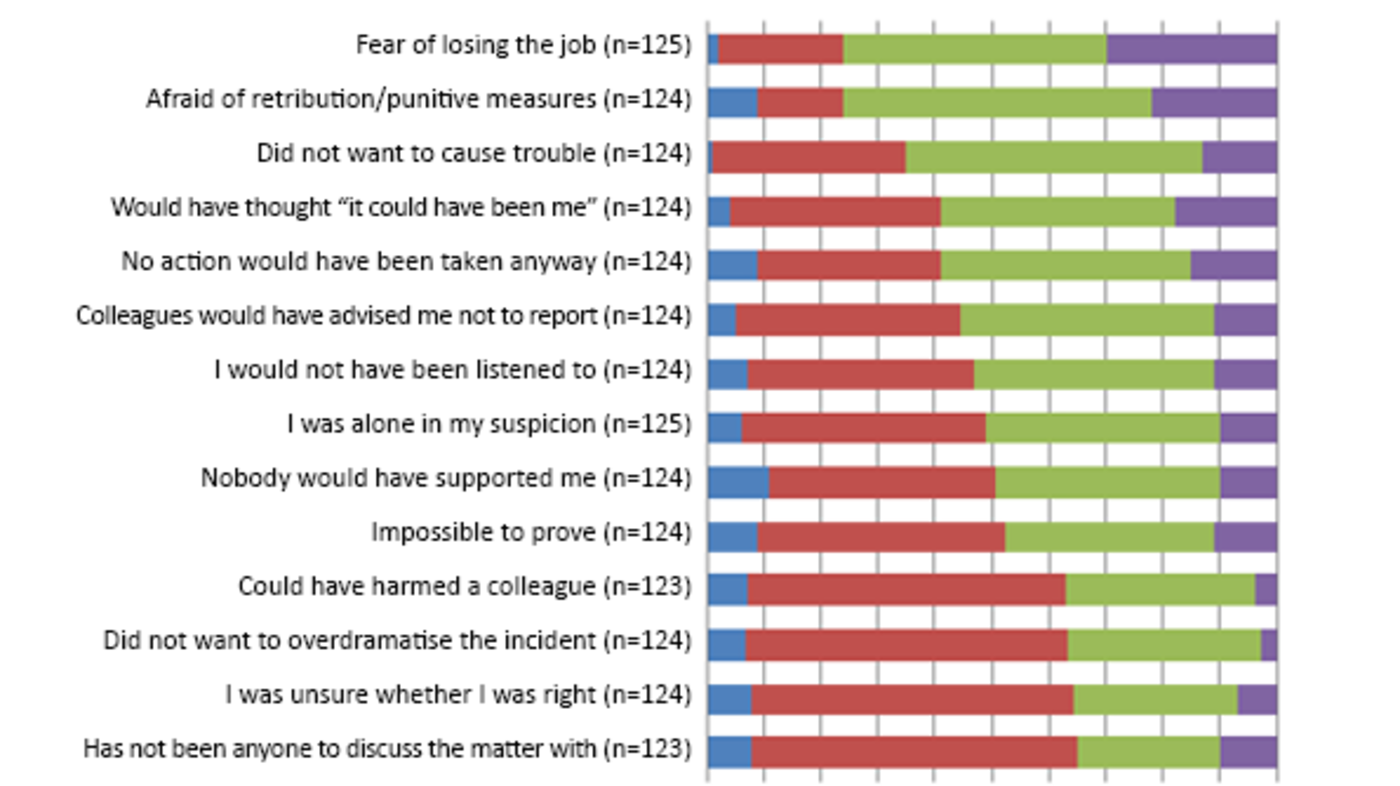
The informants considered 14 statements and responded to their level of importance in whether they reported incidents or not. Figure 1 shows the distribution of the total number of informants. There were no significant relationships between profession and the individual statement. When we compared answers from those who reported incidents with those who did not we found two significant relationships. 23.5 per cent (19) assessed “did not want to cause any trouble” as important and did not report, and 13.6 per cent (11) assessed the statement as important and did report (p=0.023)(n=81). The other significant relationship was the following: Of those considering “not having anyone to discuss the matter with” as important, 32.1 per cent (26) had reported and 39.5 per cent (32) had not reported (p=0.018)(n=81).
Discussion
The purpose of the study was to illuminate factors that influence the midwives’ and mental health nurses’ reporting of incidents. The result shows that many informants have been in situations where they had considered reporting incidents, but that they on some occasions had chosen not to. The informants responded that it was first and foremost important to avoid harm to patients, but that they also considered their own and colleagues’ situation as well as issues in their work environment before reporting incidents.
Clinical errors in patient safety work
“Improve practice/minimise harm to patient” was the most important ethical justification for reporting incidents – this is seen as in line with national patient safety work, regulations and professional ethical guidelines for nurses (4,5,7). At the same time one may ask whether events that result in obvious harm have highest priority in the patient safety effort. More than half of the informants were unfamiliar with guidelines for reporting unethical practice. That suggests that reporting clinical errors is considered as superior to reporting unethical practice. This is supported by the qualitative part of the study, where the informants expressed a wish for more attention to ethical issues and reporting of unethical practice (17).
There were more mental health nurses than midwives who reported incidents they had witnessed, and knew procedures for reporting unethical practice. More mental health nurses than midwives also ranked “improve practice/minimise harm to patient” lowest. A possible explanation to this is different attitudes in the two professional groups. Attitude is one factor that influences action (23). On the other hand, the decision to report an incident is influenced by more issues than attitude (15, 22 – 26).
Unclear guidelines lead to less reporting
A Dutch study found that awareness raising training in patient safety work led to increased attention to adverse incidents and greater competence in identifying and reporting such incidents. This was, however, not enough to fill the gap between intending to report and in fact doing so (26). Another explanation may be that the mental health nurses have clearer guidelines and more attention to reporting unethical actions, for instance in relation to the use of coercion. This supposition is supported by studies that show that unclear guidelines may lead to less reporting (22, 24, 25).
Perceived risk of sanctions may influence the decision to report incidents.
Patient autonomy – self-determination - was given high priority. One may ask why autonomy is emphasised and given priority, while preserving patient integrity and mutual respect, possibly a consequence of autonomy, has lower priority. The reason may partly be that the nurses had to rank several response alternatives, but it is nevertheless interesting that this was given such low priority. Being met with respect is important in clinical treatment. Official reports point out that the users to a greater extent shall be involved and have influence when receiving health services. An absence of respect and co-determination may threaten the right to participation (27).
Consider consequences before reporting
Despite high priority of “improving practice/minimising harm to patient” the specialist nurses assess the work environment situation before reporting adverse incidents. Almost all respondents stated that it is difficult to report incidents caused by a colleague and that they before such reporting will assess conditions that concern the relationship with work colleagues (Table 2). They made a priority of following recognised procedures such as “talking to those involved” and ensuring that “an attitude of blame was not assumed” to those involved. The informants are in line with the health authorities on these issues. The purpose of reporting incidents is not to point to scapegoats and place blame, but to increase patient safety (4, 17, 28).
We do, however, see a tendency that the specialist nurses are not quite convinced that the attention to patient safety and learning from errors is sustained in practice. Before reporting, nearly all informants would consider issues that concern any colleagues involved, whereas one fourth would consider “the risk of retribution” and “the risk of losing one’s job” (Figure 1). That this risk is real is supported by other research (12, 13, 18).
Placing the responsibility with the individual
A study carried out by The Norwegian Nurses Organisation found that 19 per cent of the nurses knew of negative consequences of reporting adverse incidents in own workplace, and that 13 per cent had experienced negative reactions from management or colleagues following an incident report (30). This is in line with the tendency in this study. Perceived risk of sanctions may influence the decision to report incidents. Based on this finding one may ask whether the responsibility for adverse incidents and reporting such incidents to a too great extent is placed with the individual nurse, while less attention is paid to complicated causal relations and problems caused by system failure. If this is the case, this may help explain why the specialist nurses so strongly emphasised concern for the individuals involved, and that they expressed empathy with their colleagues and pointed out that “it could have been me”. This may also help explain why three fourths of those that did not report incidents, responded that they ought to have done so, and that one in ten of those who had reported, would not do so again.
Do not want to be overly dramatic
The tendency is supported by studies that show that nurses, who have been involved in adverse incidents, have experienced a lack of support from their work environment. The studies also found that the nurses were alone in deciding whether or not to report adverse incidents. Nurses also reported having been subjected to formal or informal sanctions from management or work environment (24, 26, 28). It seems as if the informants were caught in a conflict of loyalties if concerns for the patient, the colleagues and the nurse conflicted.
Prioritising between the various concerns seemed to be a difficult balancing act. This supposition is strengthened by the finding that more nurses who had not reported, than nurses who had reported, responded that they “did not want to cause any trouble”. The supposition is also strengthened by that three fourths of the informants answered that it is important “not to overdramatise the incident”. The statement that scored the highest as a factor that may hinder reporting was “having no one to discuss the case with” (Figure 1). This suggests that the decision to report an adverse incident is based on complex deliberations and that the choice is difficult. One may ask whether there is too little talk about experiences of incident reporting, and whether there is a lack of openness to and acceptance of the fact that incidents do occur.
The decision to report an adverse incident is based on complex deliberations.
Despite increased attention to the development of patient safety cultures (1 ,4) the results from this study are still relevant. There are a limited number of studies from a Norwegian context in which the researchers try to understand why health personnel do not report adverse incidents. It is important to explore what kind of influence psychosocial aspects have on such reporting, what influence reporting systems and guidelines have on the reporting frequency, and what types of incidents that are reported. These factors may all contribute to increased understanding of how such reporting is related to individual concerns, work environment contexts, adverse incident reporting systems and management.
Methodology critique
The questionnaire was partly self-developed and not pre-validated, and questions may have been misunderstood or responses misinterpreted. One strength of the study is that several questions were tried out in a pilot study, and that the questionnaire was modified based on this pilot study. We tried to avoid ambiguities around concepts through the information that accompanied the questionnaire, and an explanatory paragraph to introduce the questions. Small spread in the material and few missing data may indicate that the informants have comprehended the questions and that the issues questioned were familiar.
Self-reporting of a phenomenon does not necessarily make the whole picture emerge. The respondent may have “forgotten” situations or does not wish to reveal certain things. For instance, the desire for a positive presentation of own profession may influence the informants to respond in accordance with recognised attitudes. Adverse incidents and reporting thereof are sensitive subjects and although the demand for anonymity was upheld, some may nevertheless have refrained from responding to some questions. In order for the study to be practically possible to carry out, we did the study on a selective sample. We did not collect data on how many were invited to participate.
The sample consists of informants from ten different health service institutions, and there are similarities between the sample and the professions in the way they are composed in professional life. There are more women than men, more mental health nurses than midwives, and more male mental health nurses than male midwives. It is possible that the responding specialist nurses have a greater interest in, or more experience from, reporting adverse incidents.
The findings must be interpreted as saying something about these specialist nurses’ priorities and not necessarily as valid for all nurses in general, or for the groups of specialist nurses in the sample.
Conclusion
The study shows that the participants gave the patient’s right not to be harmed high priority when deliberating whether to report an adverse incident. They based the decision of reporting or not reporting on complex considerations and were to a great extent influenced by cultural and organisational issues. A culture of openness to adverse incidents and reporting is important, as is support for those involved without placing blame or risking sanctions. In working with increasing the reporting frequency, the management’s task is to promote a work culture that accepts that errors are made, that welcomes reports, and that focuses on complex causal factors. More knowledge on what encourages and what discourages reporting is needed. Discussing the direction of the patient safety effort and establishing consensus as to what to report and what should be solved in other ways, are important. Those who report incidents should find that the report is useful and leads to changes and improvement for the patients.
We thank professor Øyvind Kirkevold for good ideas and help with the statistical analyses.
References
1. Skjellanger AG, Deilkås ET, Sørensen R, Advocaat-Vedvik J, Brudvik M, Schreiner M, Fredheim N, Longva KW, Austdal C, Lemser M, Nikolaisen J. Sluttrapport for pasientsikkerhetskampanjen «I trygge hender 24-7» 2011–2013. 2015. Available at: http://www.kunnskapssenteret.no/publikasjoner/sluttrapport-for-pasients…;(Downloaded 01.10.2015).
2. Donaldson L. World Alliance for Patient Safety. WHO 2005 France: WHO. Available at: http://www.who.int/patientsafety/en/brochure_final.pdf(Downloaded 26.09.2016).
3. Vincent C, Aylin P, Franklin BD, Holmes A, Iskander S, Jacklin A, Moorthy K. Is health care getting safer? Bmj 2008;337:a2426. Doi: 10.1136/bmj.a2426.
4. Meld. St. nr 10 (2012–2013). God kvalitet – trygge tjenester. Kvalitet og pasientsikkerhet i helse- og omsorgstjenesten. Oslo: Helse- og omsorgsdepartementet. 2012.
5. Lovdata. Lov om spesialisthelsetjenesten. 2 juli 1999; nr. 61. (Spesialisthelsetjenesteloven). Available at: https://lovdata.no/dokument/NL/lov/1999-07-02-61 (Downloaded 01.10.2015).
6. Lovdata. Forskrift om systematisk helse-, miljø- og sikkerhetsarbeid i virksomheter. 6. desember 1996; nr. 1127. (Internkontrollforskriften). Available at: https://lovdata.no/dokument/SF/forskrift/1996-12-06-1127 (Downloaded 01.10.2105).
7. Norsk Sykepleierforbund. Yrkesetiske retningslinjer for sykepleiere. 2014. Available at: https://www.nsf.no/Content/1378906/Yyrkesetiske%20retningslinjer.pdf(Downloaded 10.01.2015).
8. Saunes IS, Svendsby PO, Mølstad K, Thesen J. Kartlegging av begrepet pasientsikkerhet (notat). Oslo: Nasjonalt kunnskapssenter for helsetjenesten. 2010. ISBN 978-82-8121-999-1.
9. Ahern K, McDonald A. The beliefs of nurses who were involved in a whistleblowing event. J Adv Nurs 2002;38:303–9.
10. Jackson D, Peters K, Andrew S, Edenborough M, Halcomb E, Luck L, Salamonson Y, Wilkes L. Understanding whistleblowing: qualitative insights from nurse whistleblowers. Journal of Advanced Nursing 2010;66:2194–201. Doi: 10.1111/j.1365-2648.2010.05365.x.
11. Vaartio H, Leino-Kilpi H, Salantera S, Suominen T. Nursing advocacy: how is it defined by patients and nurses, what does it involve and how is it experienced? Scand J Caring Sci 2006;20:282–92. Doi: 10.1111/j.1471-6712.2006.00406.x.
12. Kirkehei IA, Lindahl K, og Tinnå M. Helsepersonell som har vært involvert i uønskede hendelser. Oslo: Nasjonalt kunnskapssenter for helsetjenesten (notat). Oslo: Kunnskapssenteret. 2012.
13. Mesel T. Når noe går galt: fortellinger om skyld, skam og ansvar i helsetjenesten. Oslo: Cappelen Damm Akademisk. 2014.
14. Sirriyeh R, Lawton R, Gardner P, Armitage G. Coping with medical error: a systematic review of papers to assess the effects of involvement in medical errors on healthcare professionals’ psychological well-being. Qual Saf Health Care 2010;19:43:8. Doi:10.1136/qshc.2009.035253.
15. Black LM. Tragedy into policy: a quantitative study of nurses’ attitudes toward patient advocacy activities. Am J Nurs 2011;111(6):26–35. Doi:10.1097/01.NAJ.0000398537.06542.c0.
16. Peters K, Luck L, Hutchinson M, Wilkes L, Andrew S, Jackson D. The emotional sequelae of whistleblowing: findings from a qualitative study. J Clin Nurs 2011;20:2907–14. Doi:10.1111/j.1365-2702.2011.03718.x.
17. Ulvund I, Dale KY, Ødegård, A. Skal – skal ikke. Jordmødre og psykiatriske sykepleieres erfaringer med varsling av avvik. Tidsskrift for Nordisk Helseforskning. 2015;11(2):86–96. Doi:http://dx.doi.org/10.7557/14.3714.
18. Sanghera IS, Franklin BD, Dhillon S. The attitudes and beliefs of healthcare professionals on the causes and reporting of medication errors in a UK Intensive care unit. Anesthesia 2007;62(1):53–61. Doi:10.1111/j.1365-2044.2006.04858.x.
19. Joolaee S, Hajibabaee F, Peyrovi H, Haghani H, Bahrani N. The relationship between incidence and report of medication errors and working conditions. International Nursing Review 2011;58:37–44. Doi: 10.1111/j.1466-7657.2010.00872.x.
20. Ulvund I, Vatne S. Varsling og mangel på varsling av kliniske feil og uetisk praksis (rapport). Molde: Møreforsking 2015. In press.
21. Firth-Cozens J, Firth, RA, Booth S. Attitudes to and experiences of reporting poor care. Clinical Governance: An International Journal 2001:8(4):331–6. Doi: 10.1108/14777270310499423.
22. Gifford ML, Anderson JE. Barriers and motivating factors in reporting incidents of assault in mental health care. J Am Psychiatr Nurses Assoc. 2010;5:288–98. Doi: 10.1177/1078390310384862.
23. Ajzen I. Attitudes, personality and behaviour (2. utg.). Berkshire, Storbritannia: McGraw-Hill Education. 2005.
24. Evans SM, Berry JG, Smith BJ, Esterman A, Selim P, O’Shaughnessy J, DeWit M. Attitudes and barriers to incident reporting: a collaborative hospital study. Qual Saf Health Care 2006;15:39–43. Doi:10.1136/qshc.2004.012559.
25. Prang IW, Jelsness-Jørgensen LP. Should I report? A qualitative study of barriers to incident reporting among nurses working in nursing homes. Geriatr Nurs 2014;35:441–7. Doi:10.1016/j.gerinurse.2014.07.003.
26. Jansma JD, Wagner C, Kate RW, Bijnen AB. Effects on incident reporting after educating residents in patient safety: a controlled study. BMC Health Serv Res 2011;335. Doi: 10.1186/1472-6963-11-335.
27. Helse- og omsorgsdepartementet. Og bedre skal det bli – Nasjonal strategi for kvalitetsforbedring i sosial- og helsetjenesten 2005–2015. Oslo: Sosial- og helsedirektoratet. 2005.
28. Jackson D, Peters K, Andrew S, Edenborough M, Halcomb L, Luck Y, Salamonson Y, Wilkes L. Understanding whistleblowing: qualitative insights from nurse whistleblowers. Journal of Advanced Nursing 2010;66:2194–201. Doi:10.1111/j.1365-2648.2010.05365.x.
29. Peters K, Luck L, Hutchinson M, Wilkes L, Andrew S, Jackson D. The emotional sequelae of whistleblowing: findings from a qualitative study. J Clin Nurs 2011;19–20:2907–14. Doi:10.1111/j.1365-2702.2011.03718.x.
30. Hofstad E. Avvik stoppes og avvises. Sykepleien 2015;3:30–9. Available at: https://sykepleien.no/2015/03/1-av-2-ser-ikke-nytten-av-melde (Downloaded 12.09.2016).









Comments